Abstract
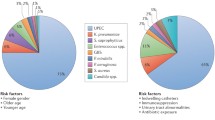
Urinary tract infections (UTIs) are one of the most common infectious diseases among humans and account for over one million hospitalizations and $1.6 billion in medical costs per year in the United States. Bacterial etiologies are the most common cause of UTI, with uropathogenic Escherichia coli (UPEC) accounting for over 80% of all infections. The development of UTIs can be influenced by urinary tract anatomy, congenital anomalies, and bacterial pathogenic proteins.
Cystitis, urethritis, and pyelonephritis represent common UTIs that remain prevalent globally with symptoms including dysuria, frequency, urgency, suprapubic or flank pain, hematuria, and fever. Events that must occur between the host and the microbes for bacteria to colonize include adhesion to host cells, colonization of tissues, cellular invasion, and intracellular multiplication and dissemination. Current antibiotic guidelines to treat these infections depend on various comorbidities or infection etiology.
Treatment of UTIs caused by E. coli with standard antibiotics is becoming increasingly difficult due to antibiotic resistance. Alternative therapies in the treatment of UTIs caused by UPEC include anti-adhesion agents to disrupt biofilms, phage therapy, phytochemicals, nanomedicine, and natural remedies such as cranberry juice and probiotics. Creation of a vaccine may have the largest potential for protection, and there are several in development and in clinical trials around the world. The abundance of antigens as targets for vaccines makes the hope for an effective vaccine in the future seem possible.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Ulett GC, Totsika M, Schaale K, Carey AJ, Sweet MJ, Schembri MA. Uropathogenic Escherichia coli virulence and innate immune responses during urinary tract infection. Curr Opin Microbiol. 2013;16(1):100–7.
CDC. Suffering from a urinary tract infection? [Internet]. Centers for Disease Control and Prevention. 2022 [cited 2022 May 28]. Available from: https://www.cdc.gov/antibiotic-use/uti.html
Iacovelli V, Gaziev G, Topazio L, Bove P, Vespasiani G, Finazzi AE. Nosocomial urinary tract infections: a review. Urologia. 2014;81(4):222–7.
Anatomy of the Urinary System | Johns Hopkins Medicine [Internet]. [cited 2022 May 28]. Available from: https://www.hopkinsmedicine.org/health/wellness-and-prevention/anatomy-of-the-urinary-system
Croxen MA, Finlay BB. Molecular mechanisms of Escherichia coli pathogenicity. Nat Rev Microbiol. 2010;8(1):26–38.
Lüthje P, Brauner A. Virulence factors of uropathogenic E. coli and their interaction with the host. Adv Microb Physiol. 2014;65:337–72.
Thumbikat P, Berry RE, Zhou G, Billips BK, Yaggie RE, Zaichuk T, et al. Bacteria-induced uroplakin signaling mediates bladder response to infection. PLoS Pathog. 2009;5(5):e1000415.
Eto DS, Jones TA, Sundsbak JL, Mulvey MA. Integrin-mediated host cell invasion by type 1–piliated uropathogenic Escherichia coli. PLoS Pathog. 2007;3(7):e100.
Dhakal BK, Mulvey MA. Uropathogenic Escherichia coli invades host cells via an HDAC6-modulated microtubule-dependent pathway. J Biol Chem. 2009;284(1):446–54.
Anderson GG, Palermo JJ, Schilling JD, Roth R, Heuser J, Hultgren SJ. Intracellular bacterial biofilm-like pods in urinary tract infections. Science. 2003;301(5629):105–7.
Wiles TJ, Dhakal BK, Eto DS, Mulvey MA. Inactivation of host Akt/protein kinase B signaling by bacterial pore-forming toxins. Mol Biol Cell. 2008;19(4):1427–38.
Lane MC, Simms AN, Mobley HLT. Complex interplay between type 1 fimbrial expression and flagellum-mediated motility of uropathogenic Escherichia coli. J Bacteriol. 2007;189(15):5523–33.
Kaper JB, Nataro JP, Mobley HLT. Pathogenic Escherichia coli. Nat Rev Microbiol. 2004;2(2):123–40.
Mulvey MA, Schilling JD, Hultgren SJ. Establishment of a persistent Escherichia coli reservoir during the acute phase of a bladder infection. Infect Immun. 2001;69(7):4572–9.
Foxman B, Brown P. Epidemiology of urinary tract infections: transmission and risk factors, incidence, and costs. Infect Dis Clin N Am. 2003;17(2):227–41.
Bien J, Sokolova O, Bozko P. Role of uropathogenic Escherichia coli virulence factors in development of urinary tract infection and kidney damage. Int J Nephrol. 2012;2012:681473.
Tittel AP, Heuser C, Ohliger C, Knolle PA, Engel DR, Kurts C. Kidney dendritic cells induce innate immunity against bacterial pyelonephritis. J Am Soc Nephrol. 2011;22(8):1435–41.
Chassin C, Goujon JM, Darche S, du Merle L, Bens M, Cluzeaud F, et al. Renal collecting duct epithelial cells react to pyelonephritis-associated Escherichia coli by activating distinct TLR4-dependent and -independent inflammatory pathways. J Immunol. 2006;177(7):4773–84.
Ingersoll MA, Kline KA, Nielsen HV, Hultgren SJ. G-CSF induction early in uropathogenic Escherichia coli infection of the urinary tract modulates host immunity. Cell Microbiol. 2008;10(12):2568–78.
Samuelsson P, Hang L, Wullt B, Irjala H, Svanborg C. Toll-like receptor 4 expression and cytokine responses in the human urinary tract mucosa. Infect Immun. 2004;72(6):3179–86.
Weisheit CK, Engel DR, Kurts C. Dendritic cells and macrophages: sentinels in the kidney. Clin J Am Soc Nephrol CJASN. 2015;10(10):1841–51.
Mobley HL, Island MD, Massad G. Virulence determinants of uropathogenic Escherichia coli and Proteus mirabilis. Kidney Int Suppl. 1994;47:S129–36.
Uropathogenic Escherichia Coli – an overview | ScienceDirect Topics [Internet]. [cited 2022 May 26]. Available from: https://www.sciencedirect.com/topics/medicine-and-dentistry/uropathogenic-escherichia-coli.
Choong FX, Antypas H, Richter-Dahlfors A. Integrated pathophysiology of pyelonephritis. Mulvey MA, Stapleton AE, Klumpp DJ, editors. Microbiol Spectr. 2015;3(5):3.5.09.
Li X, Hassoun HT, Santora R, Rabb H. Organ crosstalk: the role of the kidney. Curr Opin Crit Care. 2009;15(6):481–7.
Boekel J, Källskog O, Rydén-Aulin M, Rhen M, Richter-Dahlfors A. Comparative tissue transcriptomics reveal prompt inter-organ communication in response to local bacterial kidney infection. BMC Genomics. 2011;12:123.
Jackson GG. Pathogenesis of renal infection. Arch Intern Med. 1957;100(5):692.
Finer G, Landau D. Pathogenesis of urinary tract infections with normal female anatomy. Lancet Infect Dis. 2004;4(10):631–5.
Bent S, Nallamothu BK, Simel DL, Fihn SD, Saint S. Does this woman have an acute uncomplicated urinary tract infection? JAMA. 2002;287(20):2701–10.
Fall M, Baranowski AP, Elneil S, Engeler D, Hughes J, Messelink EJ, et al. EAU guidelines on chronic pelvic pain. Eur Urol. 2010;57(1):35–48.
Lovick TA. Central control of visceral pain and urinary tract function. Auton Neurosci Basic Clin. 2016;200:35–42.
Kanter G, Komesu YM, Qaedan F, Jeppson PC, Dunivan GC, Cichowski SB, et al. Mindfulness-based stress reduction as a novel treatment for interstitial cystitis/bladder pain syndrome: a randomized controlled trial. Int Urogynecol J. 2016;27(11):1705–11.
Charrua A, Pinto R, Taylor A, Canelas A, Ribeiro-da-Silva A, Cruz CD, et al. Can the adrenergic system be implicated in the pathophysiology of bladder pain syndrome/interstitial cystitis? A clinical and experimental study. Neurourol Urodyn. 2015;34(5):489–96.
Birder L, Andersson KE. Urothelial signaling. Physiol Rev. 2013;93(2):653–80.
Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T Peer-Rev J Formul Manag. 2015;40(4):277–83.
Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, et al. International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and Pyelonephritis in Women: A 2010 Update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011;52(5):e103–20.
Huang ES, Stafford RS. National patterns in the treatment of urinary tract infections in women by ambulatory care physicians. Arch Intern Med. 2002;162(1):41–7.
Stamm W. Evaluating guidelines. Clin Infect Dis. 2007;44:775–6.
Uncomplicated Cystitis and Pyelonephritis (UTI) [Internet]. [cited 2022 May 28]. Available from: https://www.idsociety.org/practice-guideline/uncomplicated-cystitis-and-pyelonephritis-uti/.
Colgan R, Williams M. Diagnosis and treatment of acute uncomplicated cystitis. Am Fam Physician. 2011;84(7):771–6.
den Heijer CDJ, Donker GA, Maes J, Stobberingh EE. Antibiotic susceptibility of unselected uropathogenic Escherichia coli from female Dutch general practice patients: a comparison of two surveys with a 5 year interval. J Antimicrob Chemother. 2010;65(10):2128–33.
Sannes MR, Kuskowski MA, Johnson JR. Geographical distribution of antimicrobial resistance among Escherichia coli causing acute uncomplicated pyelonephritis in the United States. FEMS Immunol Med Microbiol. 2004;42(2):213–8.
Harbarth S, Albrich W, Brun-Buisson C. Outpatient antibiotic use and prevalence of antibiotic-resistant pneumococci in France and Germany: a sociocultural perspective. Emerg Infect Dis. 2002;8(12):1460–7.
Lob SH, Nicolle LE, Hoban DJ, Kazmierczak KM, Badal RE, Sahm DF. Susceptibility patterns and ESBL rates of Escherichia coli from urinary tract infections in Canada and the United States, SMART 2010–2014. Diagn Microbiol Infect Dis. 2016;85(4):459–65.
Seifert H, Blondeau J, Dowzicky MJ. In vitro activity of tigecycline and comparators (2014–2016) among key WHO “priority pathogens” and longitudinal assessment (2004–2016) of antimicrobial resistance: a report from the T.E.S.T. study. Int J Antimicrob Agents. 2018;52(4):474–84.
Jean SS, Coombs G, Ling T, Balaji V, Rodrigues C, Mikamo H, et al. Epidemiology and antimicrobial susceptibility profiles of pathogens causing urinary tract infections in the Asia-Pacific region: results from the Study for Monitoring Antimicrobial Resistance Trends (SMART), 2010–2013. Int J Antimicrob Agents. 2016;47(4):328–34.
Kwon KT, Kim B, Yeol RS, Wie SH, Kim J, Uk JH, et al. Changes in clinical characteristics of community-acquired acute pyelonephritis and antimicrobial resistance of uropathogenic Escherichia coli in South Korea in the past decade. Antibiotics. 2020;9(9):617.
Spellberg B, Guidos R, Gilbert D, Bradley J, Boucher HW, Scheld WM, et al. The epidemic of antibiotic-resistant infections: a call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 2008;46(2):155–64.
Ejrnæs K. Bacterial characteristics of importance for recurrent urinary tract infections caused by Escherichia coli. Dan Med Bull. 2011;58(4):B4187.
Walker E, Lyman A, Gupta K, Mahoney MV, Snyder GM, Hirsch EB. Clinical management of an increasing threat: outpatient urinary tract infections due to multidrug-resistant uropathogens. Clin Infect Dis. 2016;63(7):960–5.
Lee DS, Lee SJ, Choe HS. Community-acquired urinary tract infection by Escherichia coli in the era of antibiotic resistance. Biomed Res Int. 2018;(2018):1–14.
Hayami H, Takahashi S, Ishikawa K, Yasuda M, Yamamoto S, Uehara S, et al. Nationwide surveillance of bacterial pathogens from patients with acute uncomplicated cystitis conducted by the Japanese surveillance committee during 2009 and 2010: antimicrobial susceptibility of Escherichia coli and Staphylococcus saprophyticus. J Infect Chemother. 2013;19(3):393–403.
Seo MR, Kim SJ, Kim Y, Kim J, Choi TY, Kang JO, et al. Susceptibility of Escherichia coli from community-acquired urinary tract infection to fosfomycin, nitrofurantoin, and temocillin in Korea. J Korean Med Sci. 2014;29(8):1178.
Yang B, Yang F, Wang S, Wang Q, Liu Z, Feng W, et al. Analysis of the spectrum and antibiotic resistance of uropathogens in outpatients at a tertiary hospital. J Chemother. 2018;30(3):145–9.
Treviño M, Losada I, Fernández-Pérez B, Coira A, Peña-Rodríguez MF, Hervada X, et al. [Surveillance of antimicrobial susceptibility of Escherichia coli producing urinary tract infections in Galicia (Spain)]. Rev Espanola Quimioter Publicacion Of Soc Espanola Quimioter. 2016;29(2):86–90.
Chervet D, Lortholary O, Zahar JR, Dufougeray A, Pilmis B, Partouche H. Antimicrobial resistance in community-acquired urinary tract infections in Paris in 2015. Médecine Mal Infect. 2018;48(3):188–92.
Sanchez M. Short-term effectiveness of ceftriaxone single dose in the initial treatment of acute uncomplicated pyelonephritis in women. A randomised controlled trial. Emerg Med J. 2002;19(1):19–22.
Yilmaz N, Agus N, Bayram A, Samlioglu P, Sirin MC, Karaca Derici Y, et al. Antimicrobial susceptibilities of Escherichia coli isolates as agents of community-acquired urinary tract infection (2008–2014). Türk Ürol Dergisi (Turkish J Urol). 2016;42(1):32–6.
Lee YR, Yeo S. Cefiderocol, a new siderophore cephalosporin for the treatment of complicated urinary tract infections caused by multidrug-resistant pathogens: preclinical and clinical pharmacokinetics, pharmacodynamics, efficacy and safety. Clin Drug Investig. 2020;40(10):901–13.
El-Lababidi RM, Rizk JG. Cefiderocol: a siderophore cephalosporin. Ann Pharmacother. 2020;54(12):1215–31.
Wu JY, Srinivas P, Pogue JM. Cefiderocol: a novel agent for the management of multidrug-resistant gram-negative organisms. Infect Dis Ther. 2020;9(1):17–40.
Birder LA. Pathophysiology of interstitial cystitis. Int J Urol. 2019;26(S1):12–5.
Asadi Karam MR, Habibi M, Bouzari S. Urinary tract infection: pathogenicity, antibiotic resistance and development of effective vaccines against uropathogenic Escherichia coli. Mol Immunol. 2019;(108):56–67.
Dashti AA, West P, Paton R, Amyes SGB. Characterization of extended-spectrum β-lactamase (ESBL)-producing Kuwait and UK strains identified by the Vitek system, and subsequent comparison of the Vitek system with other commercial ESBL-testing systems using these strains. J Med Microbiol. 2006;55(4):417–21.
Hawkey PM, Munday CJ. Multiple resistance in Gram-negative bacteria. Rev Res Med Microbiol. 2004;15(2):51–61.
Barguigua A, El Otmani F, Talmi M, Bourjilat F, Haouzane F, Zerouali K, et al. Characterization of extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae isolates from the community in Morocco. J Med Microbiol. 2011;60(9):1344–52.
Fusté E, López-Jiménez L, Segura C, Gainza E, Vinuesa T, Viñas M. Carbapenem-resistance mechanisms of multidrug-resistant Pseudomonas aeruginosa. J Med Microbiol. 2013;62(9):1317–25.
Patel G, Bonomo R. “Stormy waters ahead”: global emergence of carbapenemases. Front Microbiol [Internet]. 2013 [cited 2022 May 28];4. Available from: https://www.frontiersin.org/article/10.3389/fmicb.2013.00048
Strahilevitz J. Plasmid-mediated quinolone resistance: a multifaceted threat [Internet]. [cited 2022 May 28]. Available from: https://journals.asm.org/doi/epub/10.1128/CMR.00016-09
Zurfluh K, Abgottspon H, Hächler H, Nüesch-Inderbinen M, Stephan R. Quinolone resistance mechanisms among Extended-Spectrum Beta-Lactamase (ESBL) producing Escherichia coli isolated from rivers and lakes in Switzerland. Khan AU, editor. PLoS ONE. 2014;9(4):e95864.
Robicsek A, Jacoby GA, Hooper DC. The worldwide emergence of plasmid-mediated quinolone resistance. Lancet Infect Dis. 2006;6(10):629–40.
Sharma G, Sharma S, Sharma P, Chandola D, Dang S, Gupta S, et al. Escherichia coli biofilm: development and therapeutic strategies. J Appl Microbiol. 2016;121(2):309–19.
Sturbelle RT, da C de Avila LF, Roos TB, Borchardt JL, de Cássia dos Santos da Conceição R, Dellagostin OA, et al. The role of quorum sensing in Escherichia coli (ETEC) virulence factors. Vet Microbiol. 2015;180(3):245–52.
Lo AWH, Van de Water K, Gane PJ, Chan AWE, Steadman D, Stevens K, et al. Suppression of type 1 pilus assembly in uropathogenic Escherichia coli by chemical inhibition of subunit polymerization. J Antimicrob Chemother. 2014;69(4):1017–26.
Han Z, Pinkner JS, Ford B, Obermann R, Nolan W, Wildman SA, et al. Structure-based drug design and optimization of mannoside bacterial FimH antagonists. J Med Chem. 2010;53(12):4779–92.
Kostakioti M, Hadjifrangiskou M, Hultgren SJ. Bacterial biofilms: development, dispersal, and therapeutic strategies in the dawn of the postantibiotic era. Cold Spring Harb Perspect Med. 2013;3(4):a010306.
Guiton PS, Cusumano CK, Kline KA, Dodson KW, Han Z, Janetka JW, et al. Combinatorial small-molecule therapy prevents uropathogenic Escherichia coli catheter-associated urinary tract infections in mice. Antimicrob Agents Chemother. 2012;56(9):4738–45.
Pei R, Lamas-Samanamud GR. Inhibition of biofilm formation by T7 bacteriophages producing quorum-quenching enzymes. Appl Environ Microbiol. 2014;80(17):5340–8.
Chibeu A, Lingohr EJ, Masson L, Manges A, Harel J, Ackermann HW, et al. Bacteriophages with the ability to degrade uropathogenic Escherichia Coli biofilms. Viruses. 2012;4(4):471–87.
Coulter LB, McLean RJC, Rohde RE, Aron GM. Effect of bacteriophage infection in combination with tobramycin on the emergence of resistance in Escherichia coli and Pseudomonas aeruginosa biofilms. Viruses. 2014;6(10):3778–86.
Monte J, Abreu AC, Borges A, Simões LC, Simões M. Antimicrobial activity of selected phytochemicals against Escherichia coli and Staphylococcus aureus and their biofilms. Pathogens. 2014;3(2):473–98.
Maisuria VB, Hosseinidoust Z, Tufenkji N. Polyphenolic extract from maple syrup potentiates antibiotic susceptibility and reduces biofilm formation of pathogenic bacteria. Appl Environ Microbiol. 2015;81(11):3782–92.
Lellouche J, Kahana E, Elias S, Gedanken A, Banin E. Antibiofilm activity of nanosized magnesium fluoride. Biomaterials. 2009;30(30):5969–78.
Johnson JR, Delavari P, Azar M. Activities of a nitrofurazone-containing urinary catheter and a silver hydrogel catheter against multidrug-resistant bacteria characteristic of catheter-associated urinary tract infection. Antimicrob Agents Chemother. 1999;43(12):2990–5.
Lellouche J, Friedman A, Gedanken A, Banin E. Antibacterial and antibiofilm properties of yttrium fluoride nanoparticles. Int J Nanomedicine. 2012;8(7):5611–24.
He W, Wang D, Ye Z, Qian W, Tao Y, Shi X, et al. Application of a nanotechnology antimicrobial spray to prevent lower urinary tract infection: a multicenter urology trial. J Transl Med. 2012;10(1):S14.
Emerich DF, Thanos CG. The pinpoint promise of nanoparticle-based drug delivery and molecular diagnosis. Biomol Eng. 2006;23(4):171–84.
Allen TM, Cullis PR. Drug delivery systems: entering the mainstream. Science. 2004;303(5665):1818–22.
Chang LC, Wu SC, Tsai JW, Yu TJ, Tsai TR. Optimization of epirubicin nanoparticles using experimental design for enhanced intravesical drug delivery. Int J Pharm. 2009;376(1):195–203.
Abed N, Couvreur P. Nanocarriers for antibiotics: a promising solution to treat intracellular bacterial infections. Int J Antimicrob Agents. 2014;43(6):485–96.
Das S. Natural therapeutics for urinary tract infections—a review. Future J Pharm Sci. 2020;6(1):64.
González de Llano D, Moreno-Arribas MV, Bartolomé B. Cranberry polyphenols and prevention against urinary tract infections: relevant considerations. Molecules. 2020;25(15):3523.
Mantzorou M. Cranberry consumption against urinary tract infections: clinical state of- the-art and future perspectives | Bentham Science. 2018 [cited 2022 May 28];19(13). Available from: http://www.eurekaselect.com/article/95063
Reid G, Bruce AW, Fraser N, Heinemann C, Owen J, Henning B. Oral probiotics can resolve urogenital infections. FEMS Immunol Med Microbiol. 2001;30(1):49–52.
Inhibitory Effect of Lactic Acid Bacteria on Uropathogenic Escherichia coli-Induced Urinary Tract Infections [Internet]. [cited 2022 May 28]. Available from: https://www.longdom.org/open-access/inhibitory-effect-of-lactic-acid-bacteria-on-uropathogenic-escherichia-coliinduced-urinary-tract-infections-35463.html
Montorsi F, Gandaglia G, Salonia A, Briganti A, Mirone V. Effectiveness of a combination of Cranberries, Lactobacillus rhamnosus, and vitamin C for the management of recurrent urinary tract infections in women: results of a pilot study. Eur Urol. 2016;70(6):912–5.
Nickel JC, Saz-Leal P, Doiron RC. Could sublingual vaccination be a viable option for the prevention of recurrent urinary tract infection in Canada? A systematic review of the current literature and plans for the future. Can Urol Assoc J. 2020;14(8):281–7.
Aziminia N, Hadjipavlou M, Philippou Y, Pandian SS, Malde S, Hammadeh MY. Vaccines for the prevention of recurrent urinary tract infections: a systematic review. BJU Int. 2019;123(5):753–68.
Garcia EC, Brumbaugh AR, Mobley HLT. Redundancy and specificity of Escherichia coli iron acquisition systems during urinary tract infection. Payne SM, editor. Infect Immun. 2011;79(3):1225–35.
Habibi M, Asadi Karam MR, Bouzari S. Evaluation of prevalence, immunogenicity and efficacy of FyuA iron receptor in uropathogenic Escherichia coli isolates as a vaccine target against urinary tract infection. Microb Pathog. 2017;110:477–83.
Mike LA, Smith SN, Sumner CA, Eaton KA, Mobley HLT. Siderophore vaccine conjugates protect against uropathogenic Escherichia coli urinary tract infection. Proc Natl Acad Sci. 2016;113(47):13468–73.
Starks CM, Miller MM, Broglie PM, Cubbison J, Martin SM, Eldridge GR. Optimization and qualification of an assay that demonstrates that a FimH vaccine induces functional antibody responses in women with histories of urinary tract infections. Hum Vaccines Immunother. 2021;17(1):283–92.
Durant L, Metais A, Soulama-Mouze C, Genevard JM, Nassif X, Escaich S. Identification of candidates for a subunit vaccine against extraintestinal pathogenic Escherichia coli. Infect Immun. 2007;75(4):1916–25.
Valle J, Mabbett AN, Ulett GC, Toledo-Arana A, Wecker K, Totsika M, et al. UpaG, a new member of the trimeric autotransporter family of adhesins in uropathogenic Escherichia coli. J Bacteriol. 2008;190(12):4147–61.
Alteri CJ, Hagan EC, Sivick KE, Smith SN, Mobley HLT. Mucosal immunization with iron receptor antigens protects against urinary tract infection. PLoS Pathog. 2009;5(9):e1000586.
Wieser A, Romann E, Magistro G, Hoffmann C, Nörenberg D, Weinert K, et al. A multiepitope subunit vaccine conveys protection against extraintestinal pathogenic Escherichia coli in mice. Infect Immun. 2010;78(8):3432–42.
Searle LJ, Méric G, Porcelli I, Sheppard SK, Lucchini S. Variation in siderophore biosynthetic gene distribution and production across environmental and faecal populations of Escherichia coli. PLoS One. 2015;10(3):e0117906.
Shields J, Maxwell AP. Acute pyelonephritis can have serious complications. Practitioner. 2010;254(1728):19. 21, 23–4, 2
Ki M. The epidemiology of acute pyelonephritis in South Korea, 1997–1999. Am J Epidemiol. 2004;160(10):985–93.
Brogden RN, Ward A. Ceftriaxone. A reappraisal of its antibacterial activity and pharmacokinetic properties, and an update on its therapeutic use with particular reference to once-daily administration. Drugs. 1988;35(6):604–45.
Rodman DP, McKnight JT, Anderson RL. A critical review of the new oral cephalosporins. Considerations and place in therapy. Arch Fam Med. 1994;3(11):975–80.
Hong MT, Seifert CF. Clinical impact of discordant prescribing of fluoroquinolones and alternative treatments in Escherichia coli pyelonephritis. J Pharm Pract. 2016;29(5):467–71.
Wells WG, Woods GL, Jiang Q, Gesser RM. Treatment of complicated urinary tract infection in adults: combined analysis of two randomized, double-blind, multicentre trials comparing ertapenem and ceftriaxone followed by appropriate oral therapy. J Antimicrob Chemother. 2004;53 Suppl 2:ii67–74.
Sharara SL, Amoah J, Pana ZD, Simner PJ, Cosgrove SE, Tamma PD. Is piperacillin-tazobactam effective for the treatment of pyelonephritis caused by extended-spectrum β-lactamase–producing organisms? Clin Infect Dis. 2020;71(8):e331–7.
Jansåker F, Frimodt-Møller N, Benfield TL, Knudsen JD. Mecillinam for the treatment of acute pyelonephritis and bacteremia caused by Enterobacteriaceae: a literature review. Infect Drug Resist. 2018;(11):761–71.
Pedersen G, Schønheyder HC, Sørensen HT. Antibiotic therapy and outcome of monomicrobial gram-negative bacteraemia: a 3-year population-based study. Scand J Infect Dis. 1997;29(6):601–6.
Neu HC. Synergy of mecillinam, a beta-amidinopenicillanic acid derivative, combined with beta-lactam antibiotics. Antimicrob Agents Chemother. 1976;10(3):535–42.
Zhanel GG, Chung P, Adam H, Zelenitsky S, Denisuik A, Schweizer F, et al. Ceftolozane/tazobactam: a novel cephalosporin/β-lactamase inhibitor combination with activity against multidrug-resistant gram-negative bacilli. Drugs. 2014;74(1):31–51.
Wagenlehner FM, Umeh O, Steenbergen J, Yuan G, Darouiche RO. Ceftolozane-tazobactam compared with levofloxacin in the treatment of complicated urinary-tract infections, including pyelonephritis: a randomised, double-blind, phase 3 trial (ASPECT-cUTI). Lancet. 2015;385(9981):1949–56.
Perrotta C, Aznar M, Mejia R, Albert X, Ng CW. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database Syst Rev [Internet] 2008 [cited 2022 May 26];(2). Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD005131.pub2/abstract
Kolman KB. Cystitis and pyelonephritis. Prim Care Clin. 2019;46(2):191–202.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kelmis, C., Stephan, K., Varadhan, A., Brown, J.B., Preuss, C. (2023). Recent Developments in the Treatment of Bacterial Urinary Tract Infections. In: Shegokar, R., Pathak, Y. (eds) Infectious Diseases Drug Delivery Systems. Springer, Cham. https://doi.org/10.1007/978-3-031-20521-7_17
Download citation
DOI: https://doi.org/10.1007/978-3-031-20521-7_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-20520-0
Online ISBN: 978-3-031-20521-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)