Abstract
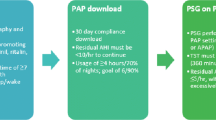
Excessive daytime sleepiness (EDS) is a complaint affecting half of patients with obstructive sleep apnea (OSA) and can persist in some patients despite normalization of breathing, oxygenation, and sleep quality with primary OSA therapy, such as continuous positive airway pressure (CPAP). EDS is often overlooked and underdiscussed in the primary care setting and in the follow-up of CPAP-treated patients due to difficult assessment of such a multidimensional symptom. This review aims to provide suggestions for procedures that can be implemented into routine clinical practice to identify, evaluate, and manage EDS in patients with OSA, including how to appropriately use various self-report and objective assessments along the clinical pathway. In addition, examples of when it is appropriate for a healthcare provider to refer a patient to a sleep specialist for evaluation are discussed. Despite certain limitations of this method, healthcare professionals (HCPs) should screen all patients diagnosed with OSA for EDS with the Epworth Sleepiness Scale. If a patient is suspected of having EDS, it needs to be confirmed that the underlying airway obstruction is being optimally treated with CPAP or another OSA primary treatment. If the patient continues to experience EDS despite adherence to primary OSA therapy, the treating clinician should review the patient in clinic and, when appropriate, using questionnaires, physical exams, laboratory tests, or objective assessments to rule out other potential causes of EDS. After a differential diagnosis of residual EDS has been established, the clinician may consider pharmacologic treatment which may include a wake-promoting agent.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–5.
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–14.
Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7(8):687–98.
American Academy of Sleep Medicine. Obstructive sleep apnea, adult. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. p. 53–62.
Bailly S, Destors M, Grillet Y, et al. Obstructive sleep apnea: a cluster analysis at time of diagnosis. PLoS One. 2016;11(6):e0157318.
Koutsourelakis I, Perraki E, Economou NT, et al. Predictors of residual sleepiness in adequately treated obstructive sleep apnoea patients. Eur Respir J. 2009;34(3):687–93.
Kapur VK, Baldwin CM, Resnick HE, Gottlieb DJ, Nieto FJ. Sleepiness in patients with moderate to severe sleep-disordered breathing. Sleep. 2005;28(4):472–7.
Macey PM, Woo MA, Kumar R, Cross RL, Harper RM. Relationship between obstructive sleep apnea severity and sleep, depression and anxiety symptoms in newly-diagnosed patients. PLoS One. 2010;5(4):e10211.
Lipford MC, Wahner-Roedler DL, Welsh GA, Mandrekar J, Thapa P, Olson EJ. Correlation of the Epworth sleepiness scale and sleep-disordered breathing in men and women. J Clin Sleep Med. 2019;15(1):33–8.
Gabryelska A, Białasiewicz P. Association between excessive daytime sleepiness, REM phenotype and severity of obstructive sleep apnea. Sci Rep. 2020;10(1):34.
Kendzerska TB, Smith PM, Brignardello-Petersen R, Leung RS, Tomlinson GA. Evaluation of the measurement properties of the Epworth Sleepiness Scale: a systematic review. Sleep Med Rev. 2014;18(4):321–31.
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of sleep medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med. 2019;15(2):335–43.
Epstein LJ, Kristo D, Strollo PJ Jr, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263–76.
Gasa M, Tamisier R, Launois SH, et al. Residual sleepiness in sleep apnea patients treated by continuous positive airway pressure. J Sleep Res. 2013;22(4):389–97.
Pepin JL, Viot-Blanc V, Escourrou P, et al. Prevalence of residual excessive sleepiness in CPAP-treated sleep apnoea patients: the French multicentre study. Eur Respir J. 2009;33(5):1062–7.
Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34(1):111–9.
Weaver TE, Maislin G, Dinges DF, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007;30(6):711–9.
Budhiraja R, Kushida CA, Nichols DA, et al. Predictors of sleepiness in obstructive sleep apnoea at baseline and after 6 months of continuous positive airway pressure therapy. Eur Respir J. 2017;50(5):1700348.
Stepnowsky C, Sarmiento KF, Bujanover S, Villa KF, Li VW, Flores NM. Comorbidities, health-related quality of life, and work productivity among people with obstructive sleep apnea with excessive sleepiness: findings from the 2016 US National Health and Wellness Survey. J Clin Sleep Med. 2019;15(2):235–43.
Lal C, Strange C, Bachman D. Neurocognitive impairment in obstructive sleep apnea. Chest. 2012;141(6):1601–10.
Werli KS, Otuyama LJ, Bertolucci PH, et al. Neurocognitive function in patients with residual excessive sleepiness from obstructive sleep apnea: a prospective, controlled study. Sleep Med. 2016;26:6–11.
Mulgrew AT, Ryan CF, Fleetham JA, et al. The impact of obstructive sleep apnea and daytime sleepiness on work limitation. Sleep Med. 2007;9(1):42–53.
Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med. 2009;5(6):573–81.
Garbarino S, Guglielmi O, Sanna A, Mancardi GL, Magnavita N. Risk of occupational accidents in workers with obstructive sleep apnea: systematic review and meta-analysis. Sleep. 2016;39(6):1211–8.
Gottlieb DJ, Ellenbogen JM, Bianchi MT, Czeisler CA. Sleep deficiency and motor vehicle crash risk in the general population: a prospective cohort study. BMC Med. 2018;16(1):44.
Won CH, Bogan RK, Doghramji K, et al. Assessing communication between physicians and patients with excessive daytime sleepiness associated with treated obstructive sleep apnea: insights from an ethnographic study of in-office visits [abstract]. Am J Respir Crit Care Med. 2019;199:A1390.
Pépin JL, Tamisier R, Hwang D, Mereddy S, Parthasarathy S. Does remote monitoring change OSA management and CPAP adherence? Respirology. 2017;22(8):1508–17.
He K, Kapur VK. Sleep-disordered breathing and excessive daytime sleepiness. Sleep Med Clin. 2017;12(3):369–82.
Javaheri S, Javaheri S. Update on persistent excessive daytime sleepiness in obstructive sleep apnea. Chest. 2020;158:776–86.
Chervin RD. Sleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apnea. Chest. 2000;118(2):372–9.
Vernet C, Redolfi S, Attali V, et al. Residual sleepiness in obstructive sleep apnoea: phenotype and related symptoms. Eur Respir J. 2011;38(1):98–105.
Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14(6):540–5.
Johns M, Hocking B. Daytime sleepiness and sleep habits of Australian workers. Sleep. 1997;20(10):844–9.
About the Epworth Sleepiness Scale. 2020. Available at: https://epworthsleepinessscale.com/about-the-ess/. Accessed 16 Oct 2020.
Lapin BR, Bena JF, Walia HK, Moul DE. The Epworth Sleepiness Scale: validation of one-dimensional factor structure in a large clinical sample. J Clin Sleep Med. 2018;14(8):1293–301.
Rosenberg R, Babson K, Menno D, et al. Epworth Sleepiness Scale Test-Retest reliability analysis in solriamfetol studies [abstract]. Sleep. 2020;43(Suppl 1):A285–6.
Taylor E, Zeng I, O’Dochartaigh C. The reliability of the Epworth Sleepiness Score in a sleep clinic population. J Sleep Res. 2019;28(2):e12687.
Campbell AJ, Neill AM, Scott DAR. Clinical reproducibility of the Epworth Sleepiness Scale for patients with suspected sleep apnea. J Clin Sleep Med. 2018;14(5):791–5.
Nguyen AT, Baltzan MA, Small D, Wolkove N, Guillon S, Palayew M. Clinical reproducibility of the Epworth Sleepiness Scale. J Clin Sleep Med. 2006;2(2):170–4.
Hoddes E, Dement W, Zarcone V. The development and use of the Stanford sleepiness scale (SSS) [abstract]. Psychophysiology. 1972;9:150.
Hoddes E, Zarcone V, Smythe H, Phillips R, Dement WC. Quantification of sleepiness: a new approach. Psychophysiology. 1973;10(4):431–6.
Carskadon MA, Dement WC. Cumulative effects of sleep restriction on daytime sleepiness. Psychophysiology. 1981;18(2):107–13.
Herscovitch J, Broughton R. Sensitivity of the Stanford sleepiness scale to the effects of cumulative partial sleep deprivation and recovery oversleeping. Sleep. 1981;4(1):83–91.
Akerstedt T, Gillberg M. Subjective and objective sleepiness in the active individual. Int J Neurosci. 1990;52(1–2):29–37.
Shahid A, Wilkinson K, Marcu S, Shapiro CM, Karolinska Sleepiness Scale (KSS). STOP, THAT and one hundred other sleep scales. New York: Springer; 2012. p. 209–10.
Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg. 2016;45(1):43.
Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245–58.
Weaver TE. Novel aspects of CPAP treatment and interventions to improve CPAP adherence. J Clin Med. 2019;8(12):2220.
Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173–8.
Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15(6):343–56.
Pengo MF, Czaban M, Berry MP, et al. The effect of positive and negative message framing on short term continuous positive airway pressure compliance in patients with obstructive sleep apnea. J Thorac Dis. 2018;10(Suppl 1):S160–s169.
Parthasarathy S, Haynes PL, Budhiraja R, Habib MP, Quan SF. A national survey of the effect of sleep medicine specialists and American Academy of Sleep Medicine Accreditation on management of obstructive sleep apnea. J Clin Sleep Med. 2006;2(2):133–42.
Parthasarathy S, Subramanian S, Quan SF. A multicenter prospective comparative effectiveness study of the effect of physician certification and center accreditation on patient-centered outcomes in obstructive sleep apnea. J Clin Sleep Med. 2014;10(3):243–9.
Sleep and sleep disorders data and statistics. 2017. Available at: https://www.cdc.gov/sleep/data_statistics.html. Accessed 16 Oct 2020.
Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843–4.
Ejaz SM, Khawaja IS, Bhatia S, Hurwitz TD. Obstructive sleep apnea and depression: a review. Innov Clin Neurosci. 2011;8(8):17–25.
American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014.
Littner MR, Kushida C, Wise M, et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep. 2005;28(1):113–21.
Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387–94.
Doghramji K, Mitler MM, Sangal RB, et al. A normative study of the maintenance of wakefulness test (MWT). Electroencephalogr Clin Neurophysiol. 1997;103(5):554–62.
Bennett LS, Stradling JR, Davies RJ. A behavioural test to assess daytime sleepiness in obstructive sleep apnoea. J Sleep Res. 1997;6(2):142–5.
Priest B, Brichard C, Aubert G, Liistro G, Rodenstein DO. Microsleep during a simplified maintenance of wakefulness test. A validation study of the OSLER test. Am J Respir Crit Care Med. 2001;163(7):1619–25.
Dinges DF, Powell JW. Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav Res Methods Instrum Comput. 1985;17(6):652–5.
Naito E, Kinomura S, Geyer S, Kawashima R, Roland PE, Zilles K. Fast reaction to different sensory modalities activates common fields in the motor areas, but the anterior cingulate cortex is involved in the speed of reaction. J Neurophysiol. 2000;83(3):1701–9.
Jung CM, Ronda JM, Czeisler CA, Wright KP Jr. Comparison of sustained attention assessed by auditory and visual psychomotor vigilance tasks prior to and during sleep deprivation. J Sleep Res. 2011;20(2):348–55.
D'Rozario AL, Field CJ, Hoyos CM, et al. Impaired neurobehavioural performance in untreated obstructive sleep apnea patients using a novel standardised test battery. Front Surg. 2018;5:35.
Batool-Anwar S, Kales SN, Patel SR, Varvarigou V, DeYoung PN, Malhotra A. Obstructive sleep apnea and psychomotor vigilance task performance. Nat Sci Sleep. 2014;6:65–71.
Thomann J, Baumann CR, Landolt HP, Werth E. Psychomotor vigilance task demonstrates impaired vigilance in disorders with excessive daytime sleepiness. J Clin Sleep Med. 2014;10(9):1019–24.
Deering S, Amdur A, Borelli J, Headapohl W, Stepnowsky CJ. A three-minute mobile version of the psychomotor vigilance task [abstract 1053]. Sleep. 2018;41(Suppl 1):A391–2.
Smith MT, McCrae CS, Cheung J, et al. Use of actigraphy for the evaluation of sleep disorders and circadian rhythm sleep-wake disorders: an American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med. 2018;14(7):1209–30.
Martin JL, Hakim AD. Wrist actigraphy. Chest. 2011;139(6):1514–27.
Li Y, Zhang J, Lei F, Liu H, Li Z, Tang X. Self-evaluated and close relative- evaluated Epworth Sleepiness Scale vs. multiple sleep latency test in patients with obstructive sleep apnea. J Clin Sleep Med. 2014;10(2):171–6.
Li Y, Vgontzas A, Kritikou I, et al. Psychomotor vigilance test and its association with daytime sleepiness and inflammation in sleep apnea: clinical implications. J Clin Sleep Med. 2017;13(9):1049–56.
Provigil [package insert]. North Wales, PA: Teva Pharmaceuticals; 2018.
Nuvigil [package insert]. North Wales, PA: Teva Pharmaceuticals; 2018.
Pack AI, Black JE, Schwartz JR, Matheson JK. Modafinil as adjunct therapy for daytime sleepiness in obstructive sleep apnea. Am J Respir Crit Care Med. 2001;164(9):1675–81.
Black JE, Hirshkowitz M. Modafinil for treatment of residual excessive sleepiness in nasal continuous positive airway pressure-treated obstructive sleep apnea/hypopnea syndrome. Sleep. 2005;28(4):464–71.
Hirshkowitz M, Black JE, Wesnes K, Niebler G, Arora S, Roth T. Adjunct armodafinil improves wakefulness and memory in obstructive sleep apnea/hypopnea syndrome. Respir Med. 2007;101(3):616–27.
Roth T, White D, Schmidt-Nowara W, et al. Effects of armodafinil in the treatment of residual excessive sleepiness associated with obstructive sleep apnea/hypopnea syndrome: a 12-week, multicenter, double-blind, randomized, placebo-controlled study in nCPAP-adherent adults. Clin Ther. 2006;28(5):689–706.
Hirshkowitz M, Black J. Effect of adjunctive modafinil on wakefulness and quality of life in patients with excessive sleepiness-associated obstructive sleep apnoea/hypopnoea syndrome: a 12-month, open-label extension study. CNS Drugs. 2007;21(5):407–16.
Black JE, Hull SG, Tiller J, Yang R, Harsh JR. The long-term tolerability and efficacy of armodafinil in patients with excessive sleepiness associated with treated obstructive sleep apnea, shift work disorder, or narcolepsy: an open-label extension study. J Clin Sleep Med. 2010;6(5):458–66.
Chapman JL, Vakulin A, Hedner J, Yee BJ, Marshall NS. Modafinil/armodafinil in obstructive sleep apnoea: a systematic review and meta-analysis. Eur Respir J. 2016;47(5):1420–8.
European Medicines Agency. Modafinil - Article 31 referral - Annex I, II, III, IV. 2011. Available at: https://www.ema.europa.eu/documents/referral/modafinil-article-31-referral-annex-i-ii-iii-iv_en.pdf. Accessed 24 Jan 2019.
Sukhal S, Khalid M, Tulaimat A. Effect of wakefulness-promoting agents on sleepiness in patients with sleep apnea treated with CPAP: a meta-analysis. J Clin Sleep Med. 2015;11(10):1179–86.
Sunosi® (solriamfetol) tablets Prescribing Information. Palo Alto, CA: Jazz Pharmaceuticals, Inc; 2019.
Sunosi® (solriamfetol) tablets summary of product characteristics. Dublin, Ireland: Jazz Pharmaceuticals Ireland Ltd; 2020.
Schweitzer PK, Rosenberg R, Zammit GK, et al. Solriamfetol for excessive sleepiness in obstructive sleep apnea (TONES 3): a randomized controlled trial. Am J Respir Crit Care Med. 2019;199(11):1421–31.
Strollo PJ Jr, Hedner J, Collop N, et al. Solriamfetol for the treatment of excessive sleepiness in OSA: a placebo-controlled randomized withdrawal study. Chest. 2019;155(2):364–74.
Malhotra A, Shapiro C, Pepin JL, et al. Long-term study of the safety and maintenance of efficacy of solriamfetol (JZP-110) in the treatment of excessive sleepiness in participants with narcolepsy or obstructive sleep apnea. Sleep. 2020;43(2):zsz220.
Wakix [package insert]. Plymouth Meeting, PA: Harmony Biosciences; 2019.
Dauvilliers Y, Verbraecken J, Partinen M, et al. Pitolisant for daytime sleepiness in obstructive sleep apnea patients refusing CPAP: a randomized trial. Am J Respir Crit Care Med. 2020;201(9):1135–45.
Rosenberg R, Baladi M, Menno D, Bron M. Clinically relevant effects of solriamfetol on excessive daytime sleepiness: a post-hoc analysis of the magnitude of change in clinical trials in adults with narcolepsy or obstructive sleep apnoea [abstract]. Sleep Med. 2019;64(suppl):S325.
Scrima L, Emsellem HA, Becker PM, et al. Identifying clinically important difference on the Epworth Sleepiness Scale: results from a narcolepsy clinical trial of JZP-110. Sleep Med. 2017;38:108–12.
Lammers GJ, Bogan R, Schweitzer PK, et al. Thresholds for clinically meaningful changes on the Epworth sleepiness scale and maintenance of wakefulness test sleep latency [abstract]. Presented at: Biennial World Sleep Congress; September 20–25, 2019; Vancouver, BC, Canada.
Rosenberg R, Schweitzer PK, Malhotra A, et al. Incidence and duration of common adverse events in a solriamfetol (JZP-110) phase 3 study for treatment of excessive daytime sleepiness in obstructive sleep apnea [abstract 0569]. Sleep. 2019;42(suppl 1):A226–7.
Ritalin [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2019.
Adderall [package insert]. Horsham, PA: Teva Pharmaceuticals; 2017.
Dextroamphetamine sulfate [package insert]. North Wales, PA: Teva Pharmaceuticals; 2016.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rosenberg, R. (2022). Utilization of Wake-Promoting Drugs in Patients on CPAP Therapy. In: Shapiro, C.M., Gupta, M., Zalai, D. (eds) CPAP Adherence. Springer, Cham. https://doi.org/10.1007/978-3-030-93146-9_30
Download citation
DOI: https://doi.org/10.1007/978-3-030-93146-9_30
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-93144-5
Online ISBN: 978-3-030-93146-9
eBook Packages: MedicineMedicine (R0)