Abstract
Background
Human cystic echinococcosis continues to be a public health problem worldwide. The standard treatment of hydatidosis in children is open surgical intervention for removal of the cyst completely without spillage. The limited use of minimal invasive surgery (MIS) in hydatidosis has been due to the concern of inadequate removal and spillage, leading to recurrence or dissemination of the disease. Recently, a few authors have reported the successful use of minimal invasive surgery (MIS) for management of hydatid disease in children. We present our experience with successful use of MIS in the management of hydatid disease involving lung and liver in children.
Methods
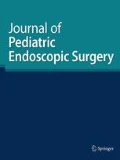
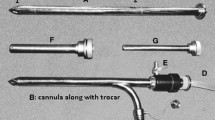
Between 2006 and 2017, data of 22 children treated for hydatid disease in our institute were reviewed. The diagnosis was made radiologically with Computerised Tomography scan of chest and abdomen. All children received albendazole therapy prior to and after the surgery. Thoracoscopic/laparoscopic procedures were undertaken sequentially in all children. Children with synchronous disease involving lung and liver had an interval of 2 weeks between procedures. The techniques of puncture, aspiration, injection and re-aspiration (PAIR) and also our modifications of cyst removal are described.
Results
There were a total of 22 children with liver and or lung involvement. Four children had synchronous lung and liver involvement and four children had bilateral lung involvement. The duration of the procedure ranged from 60 to 90 min. There were 3 (18) conversions in the thoracic group and 1 (12) in the laparoscopic group. PAIR technique with our modification of cyst extraction was used in all except in one child. Capitonnage of the cyst wall in lung hydatidosis was not done. There were no postoperative events. Recurrence of the lesion at original site was seen in two children, one each in laparoscopic and thoracoscopic group. Occurrence of new lesion or dissemination of the disease was not identified on a mean follow-up of 7 years.
Conclusion
Our series demonstrates the safe and effective utility of MIS in management of pulmonary and liver hydatid in children. Use of MIS does not lead to dissemination of the disease. Albendazole therapy is an useful adjunct prior to surgery. Single lung ventilation with isolation of uninvolved lung is useful during surgery for lung hydatid.



Similar content being viewed by others
References
Matossian RM, Rickard MD, Smyth JD (1977) Hydatidosis: a global problem of increasing importance. Bull World Health Org 55(4):499–507
Kayal A, Hussain A (2014) A comprehensive prospective clinical study of hydatid disease. ISRN Gastroenterol. 2014:514757
WHO Fact Sheets (2016) Meeting of the WHO informal working group on echinococcosis (WHO-IWGE) WHO Headquarters, Geneva, Switzerland
Celik M, Senol C, Keles M, Halezeroglu S, Urek S, Haciibrahimoglu G et al (2000) Surgical treatment of pulmonary hydatid disease in children: report of 122 cases. J Pediatr Surg 35:1710–1713
Nepalia S, Joshi A, Shende A, Sharma SS (2006) Management of echinococcosis. J Assoc Phys India 54(6):458–462
Mirshemirani A, Khaleghnejad A, Kouranloo J, Sadeghian N, Rouzrokh M, Hasas-Yeganeh S (2011) Liver hydatid cyst in children (a 14-year review). Iran J Pediatr 21(3):385–389
Smego RA Jr, Bhatti S, Khaliq AA, Beg MA et al (2003) Percutaneous aspiration–injection–reaspiration drainage plus albendazole or mebendazole for hepatic cystic echinococcosis: a meta-analysis. Clin Infect Dis. 37:1073–1083
Filice C, Bruneti E, Bruno R, Crippa FG (2000) Percutaneous drainage of echinococcal cysts (PAIR- puncture, aspiration, injection, reaspiration): results of a worldwide survey for assessment of its safety and efficacy. WHO-Informal Working Group on Echinococcosis-PAIR Network. Gut 47(1):156–157
Becmeur F, Chaouachi B, Dhaoui R, Kaabar N, Popperova N, Bientz J, Sauvage P (1994) Video-assisted thoracic surgery of hydatid cysts of the lung in children. J Chir (Paris) 131(12):541–543
Parelkar SV, Gupta RK, Shah H, Sanghvi B, Gupta A, Jadhav V et al (2009) Experience with video-assisted thoracoscopic removal of pulmonary hydatid cysts in children. J Pediatr Surg 44(4):836–841
Maazoun K, Mekki M, Chioukh FZ, Sahnoun L, Ksia A, Jouini R et al (2007) Laparoscopic treatment of hydatid cyst of the liver in children. A report on 34 cases. J Pediatr Surg 42(10):1683–1686
Ma J, Wang X, Mamatimin X, Ahan N, Chen K, Peng C et al (2016) Therapeutic evaluation of video-assisted thoracoscopic surgery versus open thoracotomy for pediatric pulmonary hydatid disease. J Cardiothorac Surg. 11(1):129
Kanojia RP (2012) Laparoscopic port-in-cyst technique for retrieval of hepatic hydatid and review of other techniques used in literature. J Pediatr Surg 47(9):1772–1774
Turna A, Yilmaz MA, Haciibrahimoğlu G, Kutlu CA, Bedirhan MA (2002) Surgical treatment of pulmonary hydatid cysts: is capitonnage necessary? Ann Thorac Surg 74(1):191–195
Mentes A (1994) Hydatid liver disease: a perspective in treatment. Dig Dis 12:150–160
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Shankar, G., Ramesh, S. & Srimurthy, K.R. Long-term outcome of minimal access surgery for hydatidosis in children: a single institutional experience. J Ped Endosc Surg 1, 113–117 (2019). https://doi.org/10.1007/s42804-019-00022-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42804-019-00022-z