Abstract
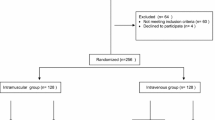
Childbirth consists of a three-stage period beginning with uterine, contractions, and ending in the expulsion of the placenta. The aim of this study was the effect of intramuscular hyoscine and hyoscine-promethazine on the duration of labor in nulliparous pregnant women. This study was a triple-blind clinical trial on 213 nulliparous pregnant women who had referred to Amiralmomenin hospital in Zanjan, Iran. Selection of samples was random and done with using 3, 6(1:1:1) of blocking ratio. This study had three groups. The first group received 20 mg hyoscine (group A), the second group 3 cc sterile water (group B), and the third group 20 mg hyoscine and 25 mg promethazine (group C). Data collection tools included a demographic questionnaire, checklist of data, and partograph chart. The mean of the first stage of labor in hyoscine group was 88.95 ± 51.07 min, hyoscine-promethazine 100.05 ± 65.88 min, and control group 170.37 ± 106.87 min. There was significant correlation between A and C and B and C groups (P < 0.001). The mean of the second stage in group A was 46.37 ± 44.60, group B 32.25 ± 17.74, and control group 55.05 ± 44.44 min and a significant relationship was between B and C groups (P = 0.03). The results showed that hyoscine and hyoscine-promethazine can be used to reduce the duration of labor.
Similar content being viewed by others
Change history
21 May 2019
The article listed above was initially published with incorrect copyright information. Upon publication of this Correction, the copyright of this article changed to ���The Author(s)���. The original article has been corrected.
21 May 2019
The article listed above was initially published with incorrect copyright information. Upon publication of this Correction, the copyright of this article changed to ���The Author(s)���. The original article has been corrected.
References
Cunningham F, Leveno K, Bloom S, Spong CY, Dashe JS, Hoffman BL, et al. Williams obstetrics. 24th ed. New York: McGraw Hill Education Medical; 2014.
Zhang J, Troendle J, Mikolajczyk R, Sundaram R, Beaver J, Fraser W. The natural history of the normal first stage of labor. Obstet Gynecol. 2010;115(4):705–10.
Rohwer Anke C, Khondowe O, Young T. Antispasmodics for labour. Cochrane Database of Systematic Reviews. 2013. https://doi.org/10.1002/14651858.CD009243.pub3.
Cheng YW, Hopkins LM, Caughey AB. How long is too long: does a prolonged second stage of labor in nulliparous women affect maternal and neonatal outcomes? Am J Obstet Gynecol. 2004;191(3):933–8.
Li W-h, Zhang H-y, Ling Y, Jin S. Effect of prolonged second stage of labor on maternal and neonatal outcomes. Asian Pac J Trop Med. 2011;4(5):409–11.
Sandström A, Altman M, Cnattingius S, Johansson S, Ahlberg M, Stephansson O. Durations of second stage of labor and pushing, and adverse neonatal outcomes: a population-based cohort study. J Perinatol. 2017;37(3):236–42.
Mayanja R, Chakura A, Mubiru M, Masembe S, Nkonwa I, Njagi J, et al. Association between duration of second stage of labour and perinatal outcomes among mothers admitted in labour at Mbarara Regional Referral Hospital, Uganda. ASRJETS. 2016;25(1):112–30.
Myles TD, Santolaya J. Maternal and neonatal outcomes in patients with a prolonged second stage of labor. Obstet Gynecol. 2003;102(1):52–8.
Cohen WR. Influence of the duration of second stage labor on perinatal outcome and puerperal morbidity. Obstet Gynecol. 1977;49(3):266–7.
Rouse DJ, Weiner SJ, Bloom SL, Varner MW, Spong CY, Ramin SM, et al. Second-stage labor duration in nulliparous women: relationship to maternal and perinatal outcomes. Am J Obstet Gynecol. 2009;201(4):357. e1–7.
Laughon SK, Berghella V, Reddy UM, Sundaram R, Lu Z, Hoffman MK. Neonatal and maternal outcomes with prolonged second stage of labor. Obstet Gynecol. 2014;124(1):57–67.
Hunt JC, Menticoglou SM. Perinatal outcome in 1515 cases of prolonged second stage of labour in nulliparous women. J Obstet Gynaecol Can. 2015;37(6):508–16.
Vahratian A, Zhang J, Troendle JF, Sciscione AC, Hoffman MK. Labor progression and risk of cesarean delivery in electively induced nulliparas. Obstet Gynecol. 2005;105(4):698–704.
Dehgani R, Tayebi N. Associate effect of IV atropine on the Fridman in the nulliparous women in active phase of labor. FEYZ Kashan. 2008;11(2):12–6.
Kausar U, Siddiqui N. To compare the efficacy of drotaverine hydrochloride with hyoscine butylbroumide for increasing the rate of cervical dilatation. IJRCOG. 2017;6(4). https://doi.org/10.18203/2320-1770.ijrcog20171438.
Cromi A, Ghezzi F, Agosti M, Uccella S, Piazza N, Serati M, et al. Use of an antispasmodic (rociverine) to shorten the length of labor: a randomized, placebo-controlled trial. Acta Obstet Gynecol Scand. 2011;90(12):1371–8.
Dahal P, Banerjee B, Uprety D, Das B, Thakur A, Agrawal A. Comparative study of efficacy of drotaverine hydrochloride and valethamate bromide with control in first stage of labour. Health Renaissance. 2013;11(1):38–42.
Gupta B, Nellore V, Mittal S. Drotaverine hydrochloride versus hyoscine-N-butylbromide in augmentation of labor. Int J Gynecol Obstet. 2008;100(3):244–7.
Madhu C, Mahavarkar S, Bhave S. A randomised controlled study comparing Drotaverine hydrochloride and Valethamate bromide in the augmentation of labour. Arch Gynecol Obstet. 2010;282(1):11–5.
Samuels L, Christie L, Roberts-Gittens B, Fletcher H, Frederick J. The effect of hyoscine butylbromide on the first stage of labour in term pregnancies. BJOG Int J Obstet Gynaecol. 2007;114(12):1542–6.
Sharma J, Pundir P, Kumar A, Murthy N. Drotaverine hydrochloride vs. valethamate bromide in acceleration of labor. Int J Gynecol Obstet. 2001;74(3):255–60.
Singh K, Jain P, Goel N, Saxena A. Drotaverine hydrochloride for augmentation of labor. Int J Gynecol Obstet. 2004;84(1):17–22.
Warke H, Chauhan A, Raut V, Ingle K. The efficacy of Camylofin dihydrochloride in acceleration of labour: a randomised double blind trial. Bombay Hosp J. 2003;45(3):420–4.
Yilmaz B, Kart C, Kelekci S, Gokturk U, Sut N, Tarlan N, et al. Meperidine versus valethamate bromide in shortening the duration of active labor. Int J Gynecol Obstet. 2009;107(2):126–9.
Mayadeo N, Gangadhar A, Das S. Camylofin in the management of prolonged labor: a review of evidence. IJRCOG. 2017;6(3):776–80.
Martindale W, Parfitt K, Britain RPSoG. Martindale: the complete drug reference. 38th ed. London: Pharmaceutical Press; 2014.
Vella L, Francis D, Houlton P, Reynolds F. Comparison of the antiemetics metoclopramide and promethazine in labour. Br Med J (Clin Res Ed). 1985;290(6476):1173–5.
Hall PF. Use of promethazine (Phenergan) in labour. CMAJ. 1987;136(7):690–1.
Znoozi M, Hashemijam MS. A comparative study of transcutaneous electrical nerve stimulation and pethidine - promethazine for pain relief in active phase of labor. Razi of Medical Science J. 2009;15(61–60):93–87.
Hobbs FS, Carroll JJ. The use of promethazine (phenergan) as a sedative during labour. Can Med Assoc J. 1958;79(10):822–5.
Makvandi S, Tadayon M, Abbaspour MR, Zaker Hoseini V, Sepandi M. Study on the effect of hyoscine-N-butylbromide suppository on pain and process of labor. Jondi Shapur Medical J. 2011;10(3):335–44.
Fardiazar Z, Niknami F, Mashayekhi S, Ghojazadeh M. Hyoscine-N-butylbromide versus atropine as labour accelerant and analgesic: a randomized clinical trial. Pak J Biol Sci. 2013;16(9):443–5.
Suki Z, Sedighpur N, Ershadi A, Karbaschi MH. Effect mixed promethazine- atropine on the active phase of labor. FEYZ Kashan. 1999;3(2):7–10.
Mortazavi F, Rakhshani M. Effects of atropine, hyoscine, promethazine on the duration phases and progress rate delivery in multiparus women. J Gorgan Univ Med Sci. 2006;14(6):92–4.
Saatsaz S, Hajiahmadi M, Basirat Z, Beheshti Z, Nazari R. Comparative effect atropine-promethazine and pethidine on the active phase of labor. JBUMS. 2009;3(9):39–42.
Irvani M, Bekhradnasab H. Effect of IV hyoscine on the labor process. Shahid Sadughi University of Medical Sciences. 2006;5(13):59–64.
Mardi A, Azari M, Nasiri E, Molud S, Manavi M, Azizzade R. Associate effect of IV Atropin and Hyoscin on the phazes of labor in nulliparus women on the Alavi hospital of Ardabil. 8th international congress obstetric and Gynecology Nov; Iran 2013. p. 110–1.
Acknowledgments
This article is an approved project of the Tabriz University of Medical Sciences (11/03/2015). Finally, we would like to thank the president, personnel, and the staff of the Amiralmomenin Hospital of Khodabandeh.
Funding
This project was funded by the Tabriz University of Medical Sciences Deputy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Shafaie, F.S., Shahmohammadi, F., Jafarabadi, M.A. et al. The Effect of Intramuscular Hyoscine and Hyoscine-Promethazine on the Duration of Labor in Nulliparous Pregnant Women (Triple-Blind Randomized Controlled Trial). SN Compr. Clin. Med. 1, 60–66 (2019). https://doi.org/10.1007/s42399-018-0013-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-018-0013-8