Abstract
Background
Nowadays, neoadjuvant chemotherapy (nCT) in breast cancer is more and more standardized, not only in advanced tumours but also in those for which there is an attempt to achieve breast-conserving surgery. In literature, we can find evidences of the relationship between several types of tumours and systemic inflammatory response. Our objective is to analyse the prognostic value of blood parameters (lymphocytes, neutrophils, monocytes, lymphocyte-to-monocyte ratio (LMR), neutrophil-to-monocyte ratio (NMR) and neutrophil-to-lymphocyte ratio (NLR) in breast cancer (BC) patients treated with nCT.
Methods
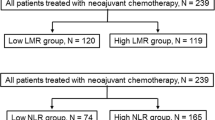
A retrospective cohort of 150 breast cancer patients treated with nCT and subsequently with surgery was analysed. Data about the patients, histology, response to chemotherapy and peripheral blood values of lymphocytes, monocytes and neutrophils was collected, and used to calculate the LMR, NMR and NLR. Univariate and multivariate analyses were performed for the variables to see the relationship of the ratios to disease-free survival (DFS) and overall survival (OS).
Results
Patients with high LMR (≥5.46) and low NLR (<3.33) were associated with a lower percentage of relapse (P = 0.048 and P = 0.015, respectively) and, above all, NLR was associated with a better survival (P = 0.024), being those factors that predict a good progress.
Conclusion
High LMR and low NLR can be considered as favourable prognostic factors in BC patients treated with nCT.

Similar content being viewed by others
References
Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66(4):271–89.
Mieog JS, Van der Hage JA, Van de Velde CJ. Preoperative chemotherapy for women with operable breast cancer. Cochrane Database Syst Rev. 2007;18;(2):CD005002 (review).
Prabhudesai SR, Malini AV, Raghavendra RM, Ashwini NR, Geetha VP, Patil S, et al. Pathologic complete response rates following neoadjuvant chemotherapy in the treatment of locally advanced breast cancer. In: ASCO annual meeting proceedings, vol 29, no. 15 suppl. 2011.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–99.
Roxburgh CS, McMillan DC. Review role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010;6(1):149–63.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–7.
Krenn-Pilko S, Langsenlehner U, Thurner EM, Stojakovic T, Pichler M, Gerger A, et al. The elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis in breast cancer patients. Br J Cancer. 2014;110(10):2524–30.
Engin H, Bilir C, Tekin IO. Prognostic significance of peripheral blood flow cytometry parameters in patients with non-metastatic breast cancer. Asian Pac J Cancer Prev. 2013;14:7645–9.
Tang X. Tumor-associated macrophages as potential diagnostic and prognostic biomarkers in breast cancer. Cancer Lett. 2013;332:3–10.
Kwon HC, Kim SH, Oh SY, Lee S, Lee JH, Choi HJ, et al. Clinical significance of preoperative neutrophil-lymphocyte versus platelet-lymphocyte ratio in patients with operable colorectal cancer. Biomarkers. 2012;17(3):216–22.
Domagala-Kulawik J. The role of the immune system in non-small cell lung carcinoma and potential for therapeutic intervention. Transl Lung Cancer Res. 2015;4:177–90.
Sun D, Elson P, Liedtke M, Medeiros BC, Earl M, Alizadeh A, et al. Absolute lymphocyte count at day 28 independently predicts event-free and overall survival in adults with newly diagnosed acute lymphoblastic leukemia. Am J Hematol. 2012;87:957–60.
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ, et al. Strategies for subtypes—dealing with the diversity of breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22(8):1736–47.
Ogston KN, Miller ID, Payne S, Hutcheon AW, Sarkar TK, Smith I. A new histological grading system to assess response of breast cancers to primary chemotherapy: prognostic significance and survival. Breast. 2003;12:320–7.
Cortazar P, Zhang L, Untch M, Mehta K, Constantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–72.
Boughey JC, McCall LM, Ballman KV, Mittendorf EA, Ahrendt GM, Wilke LG, et al. Tumor biology correlates with rates of breast-conserving surgery and pathologic complete response after neoadjuvant chemotherapy for breast cancer: findings from the ACOSOG Z1071 (Alliance) prospective multicenter clinical trial. Ann Surg. 2014;260:608–14.
Malyguine AM, Strobl SL, Shurin MR. Immunological monitoring of the tumor immunoenvironment for clinical trials Cancer Immunology. Immunotherapy. 2012;61(2):239–47.
Donskov F. Immunomonitoring and prognostic relevance of neutrophils in clinical trials. Semin Cancer Biol. 2013;23:200–7.
Aggarwal B, Gehlot P. Inflammation and cancer: how friendly is the relationship for cancer patients? Curr Opin Pharmacol. 2009;9:351–69.
Pierce BL, Ballard-Barbash R, Berstein L, Baumgartner RN, Ml Neuhouser, Wener MH, et al. Elevated biomarkers of inflammation are associated with reduced survival among breast cancer patients. J Clin Oncol. 2009;21:3437–44.
Proctor M, Morrison D, Talwar D, Balmer SM, Fletcher CD, O´Reilly DJ, et al. A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow inflammation outcome study. Eur J Cancer. 2011;47:2633–41.
Xiao-Jian N, Xiao-Lan Z, Qian-Wen OY, Guo-Wei Q, Lei W, Sheng C, et al. An elevated peripheral blood lymphocyte-to-monocyte ratio predicts favorable response and prognosis in locally advanced breast cancer following neoadjuvant chemotherapy. PLoS One. 2014;9(11):e111886.
Zhang GM, Zhu Y, Luo L, Wan FN, Zhu YP, Sun LJ, et al. Preoperative lymphocyte-monocyte and platelet-lymphocyte ratios as predictors of overall survival in patients with bladder cancer undergoing radical cystectomy. Tumor Biol. 2015;36(11):8537–43.
Azab B, Shah N, Radbel J, Tan P, Bhatt V, Vonfrolio S, et al. Pretreatment neutrophil/lymphocyte ratio is superior to platelet/lymphocyte ratio as a predictor of long-term mortality in breast cancer patients. Med Oncol. 2013;30:432.
Pusztai L, Mendoza TR, Reuben JM, Martinez MM, Willey JS, Lara J, et al. Changes in plasma levels of inflammatory cytokines in response to paclitaxel chemotherapy. Cytokine. 2004;2004(25):94–102.
Gorelik E, Landsittel DP, Marrangoni AM, Modugno F, Velikokhatnaya L, Matthew T, et al. Multiplexed immunobead-based cytokine profiling for early detection of ovarian cancer. Cancer Epidemiol Biomark Prev. 2005;14:981–7.
Yao M, Liu Y, Jin H, Liu X, Lv K, Wei H, et al. Prognostic value of preoperative inflammatory markers in Chinese patients with breast cancer. OncoTargets Ther. 2014;7:1743–52.
Retsky M, Rogers R, Demicheli R, Hrushesky JM, Gukas I, Vaidya JS, et al. NSAID analgesic ketorolac used perioperatively may suppress early breast cancer relapse: particular relevance to triple negative subgroup. Breast Cancer Res Treat. 2012;134:881.
Bergamaschi A, Tagliabue E, Sørlie T, Naume B, Triulzi T, Orlandi R, et al. extracellular matrix signature identifies breast cancer subgroups with different clinical outcome. J Pathol. 2008;214(3):357–67.
Andre F, Berrada N, Desmedt C. implication of tumor microenvironment in the resistance to chemotherapy in breast cancer patients. Curr Opin Oncol. 2010;22(6):547–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
All patients signed informed consent prior to treatment. All of them were informed and in accordance with medical practise.
Rights and permissions
About this article
Cite this article
Marín Hernández, C., Piñero Madrona, A., Gil Vázquez, P.J. et al. Usefulness of lymphocyte-to-monocyte, neutrophil-to-monocyte and neutrophil-to-lymphocyte ratios as prognostic markers in breast cancer patients treated with neoadjuvant chemotherapy. Clin Transl Oncol 20, 476–483 (2018). https://doi.org/10.1007/s12094-017-1732-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-017-1732-0