Abstract
Purpose
Doctor–patient communication is the primary way for women diagnosed with breast cancer to learn about their risk of distant recurrence. Yet little is known about how doctors approach these discussions.
Methods
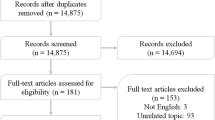
A weighted random sample of newly diagnosed early-stage breast cancer patients identified through SEER registries of Los Angeles and Georgia (2013–2015) was sent surveys about ~2 months after surgery (Phase 2, N = 3930, RR 68%). We assessed patient perceptions of doctor communication of risk of recurrence (i.e., amount, approach, inquiry about worry). Clinically determined 10-year risk of distant recurrence was established for low and intermediate invasive cancer patients. Women’s perceived risk of distant recurrence (0–100%) was categorized into subgroups: overestimation, reasonably accurate, and zero risk. Understanding of risk and patient factors (e.g. health literacy, numeracy, and anxiety/worry) on physician communication outcomes was evaluated in multivariable regression models (analytic sample for substudy = 1295).
Results
About 33% of women reported that doctors discussed risk of recurrence as “quite a bit” or “a lot,” while 14% said “not at all.” Over half of women reported that doctors used words and numbers to describe risk, while 24% used only words. Overestimators (OR .50, CI 0.31–0.81) or those who perceived zero risk (OR .46, CI 0.29–0.72) more often said that their doctor did not discuss risk. Patients with low numeracy reported less discussion. Over 60% reported that their doctor almost never inquired about worry.
Conclusions
Effective doctor–patient communication is critical to patient understanding of risk of recurrence. Efforts to enhance physicians’ ability to engage in individualized communication around risk are needed.




Similar content being viewed by others
References
Liu Y, Perez M, Aft RL, Massman K, Robinson E, Myles S, Schootman M, Gillanders WE, Jeffe DB (2010) Accuracy of perceived risk of recurrence among patients with early-stage breast cancer. Cancer Epidem Biomark Prev 19(3):675–680. doi:10.1158/1055-9965.epi-09-1051
Hawley ST, Jagsi R, Morrow M, Janz NK, Hamilton A, Graff JJ, Katz SJ (2014) Social and clinical determinants of contralateral prophylactic mastectomy. JAMA Surg 149(6):582–589. doi:10.1001/jamasurg.2013.5689
Liu Y, Perez M, Schootman M, Aft RL, Gillanders WE, Jeffe DB (2011) Correlates of fear of cancer recurrence in women with ductal carcinoma in situ and early invasive breast cancer. Breast Cancer Res Treat 130(1):165–173. doi:10.1007/s10549-011-1551-x
Freeman-Gibb LA, Janz NK, Katapodi MC, Zikmund-Fisher BJ, Northouse L (2016) The relationship between illness representations, risk perception and fear of cancer recurrence in breast cancer survivors. Psycho-Oncology. doi:10.1002/pon.4143
Lee-Jones C, Humphris G, Dixon R, Hatcher MB (1997) Fear of cancer recurrence—a literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psycho-Oncology 6(2):95–105. doi:10.1002/(sici)1099-1611(199706)6:2<95:aid-pon250>3.0.co;2-b
Waters EA, Kiviniemi MT, Orom H, Hay JL (2016) “I don’t know” my cancer risk: implications for health behavior engagement. Ann Behav Med 50(5):784–788. doi:10.1007/s12160-016-9789-5
Katapodi MC, Lee KA, Facione NC, Dodd MJ (2004) Predictors of perceived breast cancer risk and the relation between perceived risk and breast cancer screening: a meta-analytic review. Prev Med 38(4):388–402. doi:10.1016/j.ypmed.2003.11.012
Schapira MM, McAuliffe TL, Nattinger AB (2000) Underutilization of mammography in older breast cancer survivors. Med Care 38(3):281–289
Fink AK, Gurwitz J, Rakowski W, Guadagnoli E, Silliman RA (2004) Patient beliefs and tamoxifen discontinuance in older women with estrogen receptor—positive breast cancer. J Clin Oncol 22(16):3309–3315. doi:10.1200/jco.2004.11.064
Kelly KM, Ajmera M, Bhattacharjee S, Vohra R, Hobbs G, Chaudhary L, Abraham J, Agnese D (2013) Perception of cancer recurrence risk: more information is better. Patient Educ Couns 90(3):361–366. doi:10.1016/j.pec.2011.12.003
Janz NK, Li Y, Beesley LJ, Wallner LP, Hamilton AS, Morrison RA, Hawley ST (2016) Worry about recurrence in a multi-ethnic population of breast cancer survivors and their partners. Support Car Cancer 24(11):4669–4678. doi:10.1007/s00520-016-3314-z
Janz NK, Leinberger RL, Zikmund-Fisher BJ, Hawley ST, Griffith K, Jagsi R (2015) Provider perspectives on presenting risk information and managing worry about recurrence among breast cancer survivors. Psycho-Oncology 24(5):592–600. doi:10.1002/pon.3625
Tan AS, Nagler RH, Hornik RC, DeMichele A (2015) Evolving information needs among colon, breast, and prostate cancer survivors: results from a longitudinal mixed-effects analysis. Cancer Epidem Biomark Prev 24(7):1071–1078. doi:10.1158/1055-9965.epi-15-0041
Edwards AG, Naik G, Ahmed H, Elwyn GJ, Pickles T, Hood K, Playle R (2013) Personalised risk communication for informed decision making about taking screening tests. Cochrane Database Syst Rev 2:Cd001865. doi:10.1002/14651858.CD001865.pub3
Brewer NT, Richman AR, DeFrank JT, Reyna VF, Carey LA (2012) Improving communication of breast cancer recurrence risk. Breast Cancer Res Treat 133(2):553–561. doi:10.1007/s10549-011-1791-9
Zikmund-Fisher BJ, Janz NK, Hawley ST, Griffith KA, Sabolch A, Jagsi R (2016) Communication of recurrence risk estimates to patients diagnosed with breast cancer. JAMA Oncol. doi:10.1001/jamaoncol.2015.6416
Lipkus IM (2007) Numeric, verbal, and visual formats of conveying health risks: suggested best practices and future recommendations. Med Decis Mak 27(5):696–713. doi:10.1177/0272989x07307271
Gurmankin AD, Baron J, Armstrong K (2004) The effect of numerical statements of risk on trust and comfort with hypothetical physician risk communication. Med Decis Mak 24(3):265–271. doi:10.1177/0272989x04265482
Barnes AJ, Hanoch Y, Miron-Shatz T, Ozanne EM (2016) Tailoring risk communication to improve comprehension: do patient preferences help or hurt? Health Psychol 35(9):1007–1016. doi:10.1037/hea0000367
Zikmund-Fisher BJ, Fagerlin A, Ubel PA (2008) Improving understanding of adjuvant therapy options by using simpler risk graphics. Cancer 113(12):3382–3390. doi:10.1002/cncr.23959
Rosenberg SM, Tracy MS, Meyer ME, Sepucha K, Gelber S, Hirshfield-Bartek J, Troyan S, Morrow M, Schapira L, Come SE, Winer EP, Partridge AH (2013) Perceptions, knowledge, and satisfaction with contralateral prophylactic mastectomy among young women with breast cancer: a cross-sectional survey. Ann Intern Med 159(6):373–381. doi:10.7326/0003-4819-159-6-201309170-00003
Halbach SM, Ernstmann N, Kowalski C, Pfaff H, Pfortner TK, Wesselmann S, Enders A (2016) Unmet information needs and limited health literacy in newly diagnosed breast cancer patients over the course of cancer treatment. Patient Educ Couns 99(9):1511–1518. doi:10.1016/j.pec.2016.06.028
Katz MG, Jacobson TA, Veledar E, Kripalani S (2007) Patient literacy and question-asking behavior during the medical encounter: a mixed-methods analysis. J Gen Intern Med 22(6):782–786. doi:10.1007/s11606-007-0184-6
Hamstra DA, Johnson SB, Daignault S, Zikmund-Fisher BJ, Taylor JM, Larkin K, Wood A, Fagerlin A (2015) The impact of numeracy on verbatim knowledge of the longitudinal risk for prostate cancer recurrence following radiation therapy. Med Decis Mak 35(1):27–36. doi:10.1177/0272989x14551639
Galsky MD, Domingo-Domenech J (2013) Advances in the management of muscle-invasive bladder cancer through risk prediction, risk communication, and novel treatment approaches. Clin Adv Hematol Oncol 11(2):86–92
Kripalani S, Bengtzen R, Henderson LE, Jacobson TA (2008) Clinical research in low-literacy populations: using teach-back to assess comprehension of informed consent and privacy information. IRB 30(2):13–19
Ferguson B, Lowman SG, DeWalt DA (2011) Assessing literacy in clinical and community settings: the patient perspective. J Health Commun 16(2):124–134. doi:10.1080/10810730.2010.535113
Partridge A, Adloff K, Blood E, Dees EC, Kaelin C, Golshan M, Ligibel J, de Moor JS, Weeks J, Emmons K, Winer E (2008) Risk perceptions and psychosocial outcomes of women with ductal carcinoma in situ: longitudinal results from a cohort study. J Natl Cancer Inst 100(4):243–251. doi:10.1093/jnci/djn010
Hamilton AS, Hofer TP, Hawley ST, Morrell D, Leventhal M, Deapen D, Salem B, Katz SJ (2009) Latinas and breast cancer outcomes: population-based sampling, ethnic identity, and acculturation assessment. Cancer Epidem Biomark Prev 18(7):2022–2029. doi:10.1158/1055-9965.epi-09-0238
Dillman D, Smyth J, Christian L (2009) Internet, mail, and mixed-mode surveys: the tailored design method, 3rd edn. Wiley, Hoboken
Jagsi R, Griffith KA, Kurian AW, Morrow M, Hamilton AS, Graff JJ, Katz SJ, Hawley ST (2015) Concerns about cancer risk and experiences with genetic testing in a diverse population of patients with breast cancer. J Clin Oncol 33(14):1584–1591. doi:10.1200/jco.2014.58.5885
Janz NK, Hawley ST, Mujahid MS, Griggs JJ, Alderman A, Hamilton AS, Graff JJ, Jagsi R, Katz SJ (2011) Correlates of worry about recurrence in a multiethnic population-based sample of women with breast cancer. Cancer 117(9):1827–1836. doi:10.1002/cncr.25740
Hawley ST, Griggs JJ, Hamilton AS, Graff JJ, Janz NK, Morrow M, Jagsi R, Salem B, Katz SJ (2009) Decision involvement and receipt of mastectomy among racially and ethnically diverse breast cancer patients. J Natl Cancer Inst 101(19):1337–1347. doi:10.1093/jnci/djp271
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, Geyer CE Jr, Dees EC, Perez EA, Olson JA Jr, Zujewski J, Lively T, Badve SS, Saphner TJ, Wagner LI, Whelan TJ, Ellis MJ, Paik S, Wood WC, Ravdin P, Keane MM, Gomez Moreno HL, Reddy PS, Goggins TF, Mayer IA, Brufsky AM, Toppmeyer DL, Kaklamani VG, Atkins JN, Berenberg JL, Sledge GW (2015) Prospective validation of a 21-gene expression assay in breast cancer. N Engl J Med 373(21):2005–2014. doi:10.1056/NEJMoa1510764
Vaz-Luis I, Ottesen RA, Hughes ME, Mamet R, Burstein HJ, Edge SB, Gonzalez-Angulo AM, Moy B, Rugo HS, Theriault RL, Weeks JC, Winer EP, Lin NU (2014) Outcomes by tumor subtype and treatment pattern in women with small, node-negative breast cancer: a multi-institutional study. J Clin Oncol 32(20):2142–2150. doi:10.1200/jco.2013.53.1608
Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM (2007) Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Mak 27(5):672–680. doi:10.1177/0272989x07304449
Zikmund-Fisher BJ, Smith DM, Ubel PA, Fagerlin A (2007) Validation of the subjective numeracy scale: effects of low numeracy on comprehension of risk communications and utility elicitations. Med Deci Mak 27(5):663–671. doi:10.1177/0272989x07303824
Chew LD, Bradley KA, Boyko EJ (2004) Brief questions to identify patients with inadequate health literacy. Fam Med 36(8):588–594
Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, Bradley KA, Nugent SM, Baines AD, Vanryn M (2008) Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med 23(5):561–566. doi:10.1007/s11606-008-0520-5
Waters EA, Klein WM, Moser RP, Yu M, Waldron WR, McNeel TS, Freedman AN (2011) Correlates of unrealistic risk beliefs in a nationally representative sample. J Behav Med 34(3):225–235. doi:10.1007/s10865-010-9303-7
Lipkus IM, Samsa G, Rimer BK (2001) General performance on a numeracy scale among highly educated samples. Med Decis Mak 21(1):37–44
Peters E, Dieckmann N, Dixon A, Hibbard JH, Mertz CK (2007) Less is more in presenting quality information to consumers. Med Car Res Rev 64(2):169–190. doi:10.1177/10775587070640020301
Peters E (2008) Numeracy and the perception and communication of risk. Ann NY Acad Sci 1128:1–7. doi:10.1196/annals.1399.001
Peters E, Hart PS, Fraenkel L (2011) Informing patients: the influence of numeracy, framing, and format of side effect information on risk perceptions. Med Decis Mak 31(3):432–436. doi:10.1177/0272989x10391672
Trevena LJ, Zikmund-Fisher BJ, Edwards A, Gaissmaier W, Galesic M, Han PK, King J, Lawson ML, Linder SK, Lipkus I, Ozanne E, Peters E, Timmermans D, Woloshin S (2013) Presenting quantitative information about decision outcomes: a risk communication primer for patient decision aid developers. BMC Med Inform Decis Mak 13(Suppl 2):S7. doi:10.1186/1472-6947-13-s2-s7
Brooks C, Ballinger C, Nutbeam D, Adams J (2016) The importance of building trust and tailoring interactions when meeting older adults’ health literacy needs. Disabil Rehabil 7:1–8
Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, Leong-Grotz K, Castro C, Bindman AB (2003) Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med 163(1):83–90
Koh HK, Rudd RE (2015) The arc of health literacy. JAMA 314(12):1225–1226. doi:10.1001/jama.2015.9978
Rosenberg SM, Partridge AH (2014) Contralateral prophylactic mastectomy: an opportunity for shared decision making. JAMA Surg 149(6):589–590. doi:10.1001/jamasurg.2013.5713
Ahmed H, Naik G, Willoughby H, Edwards AG (2012) Communicating risk. BMJ 344:e3996. doi:10.1136/bmj.e3996
Janz NK, Friese CR, Li Y, Graff JJ, Hamilton AS, Hawley ST (2014) Emotional well-being years post-treatment for breast cancer: prospective, multi-ethnic, and population-based analysis. J Cancer Surviv 8(1):131–142. doi:10.1007/s11764-013-0309-3
Spellman E, Sulayman N, Eggly S, Peshkin BN, Isaacs C, Schwartz MD, O’Neill SC (2013) Conveying genomic recurrence risk estimates to patients with early-stage breast cancer: oncologist perspectives. Psycho-Oncology 22(9):2110–2116. doi:10.1002/pon.3264
Engelhardt EG, Pieterse AH, van Duijn-Bakker N, Kroep JR, de Haes HC, Smets EM, Stiggelbout AM (2015) Breast cancer specialists’ views on and use of risk prediction models in clinical practice: a mixed methods approach. Acta Oncol 54(3):361–367. doi:10.3109/0284186x.2014.964810
Acknowledgements
We acknowledge the work of our project staff (Mackenzie Crawford, M.P.H. and Kiyana Perrino, M.P.H. from the Georgia Cancer Registry; Jennifer Zelaya, Pamela Lee, Maria Gaeta, Virginia Parker, B.A. and Renee Bickerstaff-Magee from USC; Rebecca Morrison, M.P.H., Alexandra Jeanpierre, M.P.H., Stefanie Goodell, B.S., and Rose Juhasz, Ph.D. from the University of Michigan). We acknowledge with gratitude the breast cancer patients who responded to our survey.
Funding
This study was funded by Grant P01 CA163233 to the University of Michigan from the National Cancer Institute. The collection of Los Angeles County cancer incidence data used in this study was supported by the California Department of Public Health pursuant to California Health and Safety Code Section 103885; Centers for Disease Control and Prevention’s (CDC) National Program of Cancer Registries, under cooperative agreement 5NU58DP003862-04/DP003862; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health, the National Cancer Institute, and the CDC or their contractors and subcontractors is not intended nor should be inferred. The collection of cancer incidence data in Georgia was supported by contract HHSN261201300015I, Task Order HHSN26100006 from the NCI and cooperative agreement 5NU58DP003875-04-00 from the CDC. The ideas and opinions expressed herein are those of the author(s) and endorsement by the States of California and Georgia, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their contractors and subcontractors is not intended nor should be inferred.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Allison Kurian has received research funding for work performed outside of the current study from MyriadGenetics, Invitae, Ambry Genetics, GenDx, and Genomic Health. No other authors have conflicts of interests to report.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study through their return of a completed survey.
Additional information
Sarah T. Hawley is the senior author.
Rights and permissions
About this article
Cite this article
Janz, N.K., Li, Y., Zikmund-Fisher, B.J. et al. The impact of doctor–patient communication on patients’ perceptions of their risk of breast cancer recurrence. Breast Cancer Res Treat 161, 525–535 (2017). https://doi.org/10.1007/s10549-016-4076-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-016-4076-5