Abstract
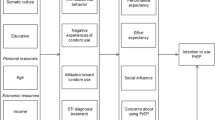
Men who have sex with men (MSM) account for most new HIV infections in the United States. Despite representing a fraction of the population, MSM make up an estimated 65% of new infections. To address this epidemic, pre-exposure prophylaxis (PrEP) is recommended to supplement condom use. Despite its effectiveness, PrEP uptake among MSM is low. Few studies have employed theoretical approaches to understand PrEP use intention. Incorporating factors like safe sex fatigue, expectation of better sexual experiences, and perceived risk are proposed in this dual motivational path model of PrEP use intention. This model hypothesized that PrEP use intention is influenced by two key pathways: (1) protection motivation pathway, and (2) sexual expectancy pathway. Data were collected using social networking applications from 402 MSM. The model was tested using structural equation modeling. We elaborate the complex decision-making process proposed by this novel theoretical model and discuss its practical implications.



Similar content being viewed by others
References
Linley L, An Q, Song R, Valverde E, Oster AM, Qian X, et al. HIV testing experience before HIV diagnosis among men who have sex with men—21 Jurisdictions, United States, 2007-2013. MMWR Morb Mortal Wkly Rep. 2016;65(37):999–1003.
Wolitski RJ, Valdiserri RO, Denning PH, Levine WC. Are we headed for a resurgence of the HIV epidemic among men who have sex with men? Am J of Public Health. 2001;91(6):883–8.
Kalichman SC. Post-exposure prophylaxis for HIV infection in gay and bisexual men: implications for the future of HIV prevention. Am J Prev Med. 1998;15(2):120–7.
Chesney MA, Chambers DB, Kahn JO. Risk behavior for HIV infection in participants in preventive HIV vaccine trials: a cautionary note. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;16(4):266–71.
CDC. HIV testing and risk behaviors among gay, bisexual, and other men who have sex with men—United States. MMWR Morb Mortal Wkly Rep. 2013;62(47):958–62.
Paz-Bailey G, Mendoza MCB, Finlayson T, Wejnert C, Le B, Rose C, et al. Trends in condom use among MSM in the United States: the role of antiretroviral therapy and seroadaptive strategies. AIDS. 2016;30(12):1985–90.
Smith DK, Grant RM, Weidle PJ, Lansky A, Mermin J, Fenton KA. Interim guidance: pre-exposure prophylaxis for the prevention of HIV infection in men who have sex with men. CDC, 2011.
Donnell D, Baeten JM, Bumpus NN, Brantley J, Bangsberg DR, Haberer JE, et al. HIV protective efficacy and correlates of tenofovir blood concentrations in a clinical trial of PrEP for HIV prevention. J Acquir Immune Defic Syndr Hum Retrovirol. 2014;66(3):340–8.
Spinner CD, Boesecke C, Zink A, Jessen H, Stellbrink HJ, Rockstroh JK, et al. HIV pre-exposure prophylaxis (PrEP): a review of current knowledge of oral systemic HIV PrEP in humans. Infection. 2016;44(2):151–8.
Vissers DCJ, Voeten HACM, Nagelkerke NJD, Habbema JDF, de Vlas SJ. The impact of pre-exposure prophylaxis (PrEP) on HIV epidemics in Africa and India: a simulation study. PLoS ONE. 2008;3(5):e2077.
Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90.
Hanscom B, Janes HE, Guarino PD, Huang Y, Brown ER, Chen YQ, et al. Brief report: preventing HIV-1 infection in women using oral preexposure prophylaxis: a meta-analysis of current evidence. J Acquir Immune Defic Syndr. 2016;73(5):606–8.
Deutsch MB, Glidden DV, Sevelius J, Keatley J, McMahan V, Guanira J, et al. HIV pre-exposure prophylaxis in transgender women: a subgroup analysis of the iPrEx trial. Lancet HIV. 2015;2(12):e512–9.
Krakower DS, Mimiaga MJ, Rosenberger JG, Novak DS, Mitty JA, White JM, et al. Limited awareness and low immediate uptake of pre-exposure prophylaxis among men who have sex with men using an internet social networking site. PLoS ONE. 2012;7(3):e33119.
Hood JE, Buskin SE, Dombrowski JC, Kern DA, Barash EA, Katzi DA, et al. Dramatic increase in preexposure prophylaxis use among MSM in Washington state. AIDS. 2016;30(3):515–9.
Holloway I, Dougherty R, Gildner J, Beougher SC, Pulsipher C, Montoya JA, et al. PrEP Uptake, adherence, and discontinuation among California YMSM using geosocial networking applications. J Acquir Immune Defic Syndr (1999). 2017;74(1):15–20.
Gomez GB, Borquez A, Caceres CF, Segura ER, Grant RM, Garnett GP, et al. The potential impact of pre-exposure prophylaxis for HIV prevention among men who have sex with men and Transwomen in Lima, Peru: a mathematical modelling study. PLoS Med. 2012;9(10):e1001323.
Mayer KH, Oldenburg CE, Novak DS, Elsesser SA, Krakower DS, Mimiaga MJ. Early adopters: correlates of HIV chemoprophylaxis use in recent online samples of US men who have sex with men. AIDS Behav. 2016;20(7):1489–98.
Golub SA, Gamarel KE, Rendina HJ, Surace A, Lelutiu-Weinberger CL. From efficacy to effectiveness: facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Patient Care STDS. 2013;27(4):248–54.
Hoff CC, Chakravarty D, Bircher AE, Campbell CK, Grisham K, Neilands TB, et al. Attitudes towards PrEP and anticipated condom use among concordant HIV-negative and HIV-discordant male couples. AIDS Patient Care STDS. 2015;29(7):408–17.
Golub SA, Kowalczyk W, Weinberger CL, Parsons JT. Preexposure prophylaxis and predicted condom use among high-risk men who have sex with men. J Acquir Immune Defic Syndr. (1999). 2010;54(5):548–55.
Carlo Hojilla J, Koester KA, Cohen SE, Buchbinder S, Ladzekpo D, Matheson T, et al. Sexual behavior, risk compensation, and HIV prevention strategies among participants in the San Francisco PrEP demonstration project: a qualitative analysis of counseling notes. AIDS Behav. 2016;20(7):1461–9.
Cain M. Sex without fear: my experience with the HIV-prevention drug PrEP. The Guardian. 2017 June 22.
Hogben M, Liddon N. Disinhibition and risk compensation: scope, definitions, and perspective. Sex Transm Dis. 2008;35(12):1009.
Rudy BJ, Kapogiannis BG, Lally MA, Gray GE, Bekker LG, Krogstad P, et al. Youth-specific considerations in the development of preexposure prophylaxis, microbicide, and vaccine research trials. J Acquir Immune Defic Syndr. 2010;54(Suppl 1):S31–42.
Guest G, Shattuck D, Johnson L, Akumatey B, Clarke EE, Chen PL, et al. Changes in sexual risk behavior among participants in a PrEP HIV prevention trial. Sex Transm Dis. 2008;35(12):1002–8.
Eaton LA, Kalichman SC. Risk compensation in HIV prevention: implications for vaccines, microbicides, and other biomedical HIV prevention technologies. Current HIV/AIDS Rep. 2007;4(4):165–72.
Kalichman SC, Rompa D. Sexual sensation seeking and Sexual Compulsivity Scales: reliability, validity, and predicting HIV risk behavior. J Pers Assess. 1995;65(3):586–601.
Marcus JL, Glidden DV, Mayer KH, Liu AY, Buchbinder SP, Amico KR, et al. No evidence of sexual risk compensation in the iPrEx trial of daily oral HIV preexposure prophylaxis. PLoS ONE. 2013;8(12):e81997.
Chesney MA, Chambers DB, Kahn JO. Risk behavior for HIV infection in participants in preventive HIV vaccine trials: a cautionary note. J Acquir Immune Defic Syndr. 1997;16(4):266–71.
Martin JN, Roland ME, Neilands TB, Krone MR, Bamberger JD, Kohn RP, et al. Use of postexposure prophylaxis against HIV infection following sexual exposure does not lead to increases in high-risk behavior. AIDS. 2004;18(5):787–92.
Ostergren JE, Rosser BRS, Horvath KJ. Reasons for non-use of condoms among men-who-have-sex-with-men: a comparison of receptive and insertive role-in-sex and online and offline meeting venue. Cult Health Sex. 2011;13(2):123–40.
Sarkar NN. Barriers to condom use. Eur J Contracept Reprod Health Care. 2008;13(2):114–22.
Carballo-Diéguez A, Dolezal C. HIV risk behaviors and obstacles to condom use among Puerto Rican men in New York City who have sex with men. Am J Public Health. 1996;86(11):1619–22.
Ho DD. Therapy of HIV infections: problems and prospects. Bull N Y Acad Med. 1996;73(1):37–45.
Wolitski RJ. The emergence of barebacking Among Gay and bisexual men in the United States: a public health perspective. J Gay Lesbian Psychother. 2005;9(3/4):9–34.
Gamarel K, Golub S. Intimacy motivations and pre-exposure prophylaxis (PrEP) adoption intentions among HIV-negative men who have sex with men (MSM) in romantic relationships. Ann Behav Med. 2015;49(2):177–86.
Golub SA, Starks TJ, Payton G, Parsons JT. The critical role of intimacy in the sexual risk behaviors of gay and bisexual men. AIDS Behav. 2012;16(3):626–32.
Rowniak S. Safe sex fatigue, treatment optimism, and serosorting: new challenges to HIV prevention among men who have sex with men. J Assoc Nurses AIDS Care. 2009;20(1):31–8.
Blackwell CW. Men who have sex with men and recruit bareback sex partners on the internet: implications for STI and HIV prevention and client education. Am J Mens Health. 2008;2(4):306–13.
Stolte IG, de Wit JBF, Kolader M, Fennema H, Coutinho RA, Dukers NHTM. Association between ‘safer sex fatigue’ and rectal gonorrhea is mediated by unsafe sex with casual partners among HIV-positive homosexual men. Sex Transm Dis. 2006;33(4):201–8.
Kellogg AP. ‘Safe sex fatigue’ grows among gay students. Chronicle High Educ. 2002;48(19):A37.
Ostrow DG, Silverberg MJ, Cook RL, Chmiel JS, Johnson L, Li X, et al. Prospective study of attitudinal and relationship predictors of sexual risk in the multicenter AIDS cohort study. AIDS Behav. 2007;12(1):127.
Coleman CL, Ball K. Determinants of perceived barriers to condom use among HIV-infected middle-aged and older African-American men. J Adv Nurs. 2007;60(4):368–76.
Balán IC, Carballo-Diéguez A, Ventuneac A, Remien RH, Dolezal C, Ford J. HIV-negative men-who-have-sex-with-men who bareback are concerned about HIV infection: implications for HIV risk reduction interventions. Arch Sex Behav. 2013;42(2):279–89.
Aghaizu A, Mercey D, Copas A, Johnson AM, Hart G, Nardone A. Who would use PrEP? Factors associated with intention to use among MSM in London: a community survey. Sex Transm Infect. 2013;89(3):207–11.
Mimiaga MJ, Case P, Johnson CV, Safren SA, Mayer KH. Preexposure antiretroviral prophylaxis attitudes in high-risk Boston area men who report having sex with men: limited knowledge and experience but potential for increased utilization after education. J Acquir Immune Defic Syndr. 2009;50(1):77–83.
Grov C, Rendina HJ, Jimenez R, Parsons JT. Using online settings to identify gay and bisexual men willing to take or with experience taking PrEP: implications for researchers and providers. AIDS Educ Prev. 2016;28(5):378–92.
Wade Taylor S, Mayer KH, Elsesser SM, Mimiaga MJ, O’Cleirigh C, Safren SA. Optimizing content for pre-exposure prophylaxis (PrEP) counseling for men who have sex with men: perspectives of PrEP users and high-risk PrEP Naïve men. AIDS Behav. 2014;18(5):871–9.
Rendina HJ, Whitfield THF, Grov C, Starks TJ, Parsons JT. Distinguishing hypothetical willingness from behavioral intentions to initiate HIV pre-exposure prophylaxis (PrEP): findings from a large cohort of gay and bisexual men in the U.S. Soc Sci Med. 2017;172:115–23.
Jackson T, Huang A, Chen H, Gao X, Zhong X, Zhang Y. Cognitive, psychosocial, and sociodemographic predictors of willingness to use HIV pre-exposure prophylaxis among Chinese men who have sex with men. AIDS Behav. 2012;16(7):1853–61.
Shrestha R, Altice FL, Huedo-Medina TB, Karki P, Copenhaver M. Willingness to use pre-exposure prophylaxis (PrEP): an empirical test of the information-motivation-behavioral skills (IMB) model among high-risk drug users in treatment. AIDS Behav. 2017;21(5):1299–308.
Helweg-Larsen M, Collins BE. The UCLA multidimensional condom attitudes scale: documenting the complex determinants of condom use in college students. Health Psychol. 1994;13(3):224–37.
Ostrow DE, Fox KJ, Chmiel JS, Silvestre A, Visscher BR, Vanable PA, et al. Attitudes towards highly active antiretroviral therapy are associated with sexual risk taking among HIV-infected and uninfected homosexual men. AIDS. 2002;16(5):775.
Dermen KH, Cooper ML. Sex-related alcohol expectancies among adolescents: I. Scale development. Psychol Addict Behav. 1994;8(3):152–60.
Napper L, Fisher D, Reynolds G. Development of the perceived risk of HIV Scale. AIDS Behav. 2012;16(4):1075–83.
Chin WW. Commentary: issues and opinion on structural equation modeling. MIS Q. 1998;22(1):vii–xvi.
Bollen KA, Long JS. Tests for structural equation models: introduction. Sociol Methods Res. 1992;21(2):123–31.
Arbuckle JL. Amos. 24th ed. Chicago: IBM; 2014.
Barrett P. Structural equation modelling: adjudging model fit. Pers Individ Dif. 2007;42(5):815–24.
Fairchild A, MacKinnon D. A general model for testing mediation and moderation effects. Prev Sci. 2009;10(2):87–99.
Adam BD, Husbands W, Murray J, Maxwell J. AIDS optimism, condom fatigue, or self-esteem? Explaining unsafe sex among gay and bisexual men. J Sex Res. 2005;42(3):238–48.
Hall HI, Frazier EL, Rhodes P, Holtgrave DR, Furlow-Parmley C, Tang T, et al. Differences in human immunodeficiency virus care and treatment among subpopulations in the United States. JAMA Intern Med. 2013;173(14):1337–44.
Brodie M, Flournoy RE, Altman DE, Blendon RJ, Benson JM, Rosenbaum MD. Health information, the internet, and the digital divide. Health Aff. 2000;19(6):255–65.
Funding
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, part of the National Institutes of Health, under Award Number AR060231-06 (Fraenkel). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors do not have any conflicts of interest related to the content of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yerina S. Ranjit, Alex Dubov, Maxim Polonksy, Liana Fraenkel, Adedotun Ogunbajo, Kenneth Mayer, and Frederick L. Altice declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ranjit, Y.S., Dubov, A., Polonsky, M. et al. Pre-exposure Prophylaxis Among Men Who have Sex with Men: Dual Motivational Model of Intention to Use Pre-exposure Prophylaxis. AIDS Behav 23, 534–543 (2019). https://doi.org/10.1007/s10461-018-2214-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2214-2