Abstract
Aim
The purpose of this study was to investigate the diagnostic performance of 68Ga-PSMA-11 PET/CT in the evaluation of bone metastases in metastatic prostate cancer (PC) patients scheduled for radionuclide therapy in comparison to [18F]sodium fluoride (18F-NaF) PET/CT.
Methods
Sixteen metastatic PC patients with known skeletal metastases, who underwent both 68Ga-PSMA-11 PET/CT and 18F-NaF PET/CT for assessment of metastatic burden prior to radionuclide therapy, were analysed retrospectively. The performance of both tracers was calculated on a lesion-based comparison. Intensity of tracer accumulation of pathologic bone lesions on 18F-NaF PET and 68Ga-PSMA-11 PET was measured with maximum standardized uptake values (SUVmax) and compared to background activity of normal bone. In addition, SUVmax values of PET-positive bone lesions were analysed with respect to morphologic characteristics on CT. Bone metastases were either confirmed by CT or follow-up PET scan.
Results
In contrast to 468 PET-positive lesions suggestive of bone metastases on 18F-NaF PET, only 351 of the lesions were also judged positive on 68Ga-PSMA-11 PET (75.0%). Intensity of tracer accumulation of pathologic skeletal lesions was significantly higher on 18F-NaF PET compared to 68Ga-PSMA-11 PET, showing a median SUVmax of 27.0 and 6.0, respectively (p < 0.001). Background activity of normal bone was lower on 68Ga-PSMA-11 PET, with a median SUVmax of 1.0 in comparison to 2.7 on 18F-NaF PET; however, tumour to background ratio was significantly higher on 18F-NaF PET (9.8 versus 5.9 on 68Ga-PSMA-11 PET; p = 0.042). Based on morphologic lesion characterisation on CT, 18F-NaF PET revealed median SUVmax values of 23.6 for osteosclerotic, 35.0 for osteolytic, and 19.0 for lesions not visible on CT, whereas on 68Ga-PSMA-11 PET median SUVmax values of 5.0 in osteosclerotic, 29.5 in osteolytic, and 7.5 in lesions not seen on CT were measured. Intensity of tracer accumulation between18F-NaF PET and 68Ga-PSMA-11 PET was significantly higher in osteosclerotic (p < 0.001) and lesions not visible on CT (p = 0.012).
Conclusion
In comparison to 68Ga-PSMA-11 PET/CT, 18F-NaF PET/CT detects a higher number of pathologic bone lesions in advanced stage PC patients scheduled for radionuclide therapy. Our data suggest that 68Ga-PSMA-11 PET should be combined with 18F-NaF PET in PC patients with skeletal metastases for restaging prior to initiation or modification of therapy.
Similar content being viewed by others

Introduction
Prostate cancer (PC) is the most frequent solid cancer among males and the third leading cause of cancer-related death in men in Europe [1, 2]. Bone is the most common site of hematogeneous metastases in PC [3]. Approximately 65–75% of patients with advanced disease show malignant skeletal involvement [4]. Presence and number of bone metastases has an important impact on prognosis and quality of life in PC patients [5,6,7]. Different therapeutic options are available in the management of bone metastases in PC patients, including also targeted radionuclide therapies with beta-emitting radionuclides such as [89Sr]strontium and [153Sm]samarium lexidronam [8]. Recently, prostate specific membrane antigen (PSMA)-directed 177Lu-labelled PSMA ligands or the alpha-emitter [223Ra]radium dichloride (223Ra) have gained much interest, and are increasingly applied in metastatic PC patients [9,10,11,12]. Knowledge of the exact burden of malignant bone involvement is crucial for therapy decision, and a prerequisite for a reliable evaluation of response to therapy.
Various morphologic and metabolic imaging modalities are applied for the assessment of skeletal metastases in PC patients [13]. In particular, computed tomography (CT), magnetic resonance imaging (MRI), and bone scintigraphy (BS) with 99mTc-labelled bisphosphonates are used in the diagnostic work-up of PC patients with suspected or known bone metastases at different phases of the disease [9, 14]. Currently, international guidelines still recommend conventional BS as imaging modality for the assessment of bone metastases in PC patients [9, 14]. However, it is well established that PET using the bone-seeking agent [18F]sodium fluoride (18F-NaF) is superior to BS in detecting skeletal metastases [15,16,17,18,19].
With respect to other PET tracers, 11C- or 18F-labelled choline has been proven to detect bone metastases in PC patients at a very early phase of bone metastases formation [15, 20]. In recent years, PET radiopharmaceuticals targeting PSMA, overexpressed on the majority of PC cells, were successfully introduced into clinical practice [21,22,23]. Currently, most data are available on the PSMA-inhibitor 68Ga-PSMA-11 (“68Ga-HBED-CC“), which seems to outperform choline, at least in PC patients with biochemical recurrence [24,25,26]. 68Ga-PSMA-11 has the potential to visualize bone metastases in PC patients [22, 27,28,29], but little is known on its accuracy concerning assessment of bone metastases. Recent publications suggest a higher sensitivity of 68Ga-PSMA-11 PET in the detection of bone metastases in PC patients in comparison with BS [30, 31].
Nevertheless, due to limited data the role of 68Ga-PSMA-11 PET/CT in the evaluation of the status of malignant skeletal involvement and monitoring of therapy response remains to be elucidated. In particular, except for one case report, no original article on the direct comparison of 68Ga-PSMA-11 and 18F-NaF in PC is available in the literature at the time of paper submission [32].
Therefore, the primary aim of this study was to investigate the diagnostic performance of 68Ga-PSMA-11 PET/CT in comparison with 18F-NaF PET/CT, performed as baseline study in metastatic PC patients prior to radionuclide therapy with 177Lu-PSMA-617 and 223Ra.
Materials and methods
Patient characteristics
The data presented in this retrospective study were obtained from patients treated with 177 Lu-PSMA-617 or 223Ra (Xofigo®) at our department between November 2013 and April 2017. The inclusion criteria for analysis were: patients with confirmed metastatic PC and known bone metastases, who were considered for targeted nuclear medicine therapy (either with 177Lu-PSMA-617 or 223Ra) and received combined pre-therapeutic staging with 18F-NaF PET/CT and 68Ga-PSMA PET/CT, that were performed within 30 days; a follow-up period of at least 6 months after baseline PET/CT-scan (for confirmation of PET-positive lesions on follow-up PET scans, conducted for therapy response assessment as part of the first visit after completion of therapy).
A total of 79 patients were extracted from our database who received a radionuclide therapy in that period. All patients presented with suspected progressive disease following conventional treatment of PC (e.g., hormone therapy, chemotherapy, radiation therapy and/or surgery). Sixteen patients met all inclusion criteria, receiving 223Ra therapy in 13 cases after baseline PET imaging, whereas three patients were scheduled for 177Lu-PSMA-617 therapy.
Patients showed a median PSA-value of 15.97 ng/ml (range: 0.35–885.0 ng/ml), measured at the time of the 68Ga-PSMA-11 PET/CT exam. Detailed patient characteristics including information on ongoing and previous treatment are summarized in Table 1.
Radiopharmaceuticals
PSMA-11 (Glu-NH-CO-NH-Lys(Ahx)-HBED-CC; HBED-CC=N,N′-bis[2-hydroxy-5-(carboxyethyl)benzyl]ethylenediamine-N, N′-diacetic acid) was obtained from ABX advanced biochemical compounds (Radeberg, Germany) in GMP quality. 68Ga-PSMA-11 was prepared on an automated synthesis module (Modular-Lab PharmTracer; Eckert & Ziegler, Berlin) using a procedure previously described [33]. The radiochemical purity of the final product was > 91% as analysed by reversed-phase high-performance liquid chromatography and thin-layer chromatography.
The injected median activity of 68Ga-PSMA-11 was 150 MBq (range: 121–169 MBq). Variation of injected activities of 68Ga-PSMA-11 are caused by the short half-life of 68Ga as well as the variable output of the 68Ge/68Ga generator.
For 18F-NaF PET-imaging, [18F]sodium fluoride provided by IASON GmbH, Austria was applied (IASOFLU®). A median activity of 152 MBq (range: 92–157 MBq) was administered.
Variation in activities of 18F-NaF are due to time of tracer delivery and tight patient schedule in our PET center, with a high number of PET scans on daily routine.
However, in our experience with both 68Ga-PSMA-11 PET/CT and 18F-NaF PET/CT, injected activities are considered sufficient for achieving adequate image quality.
Imaging protocol
PET/CT scans were performed on a dedicated PET/CT system (Discovery 690; GE Healthcare, Milwaukee, WI, USA). All patients were first scheduled for 68Ga-PSMA-11 PET/CT which was followed by 18F-NaF PET/CT within 30 days.
68Ga-PSMA-11 PET/CT imaging
The acquisition protocol for 68Ga-PSMA-11 PET/CT included a whole-body scan (skull base to upper thighs) in three-dimensional mode, emission time: 2 min per bed position, axial field of view: 15.6 cm per bed position. Image acquisition started after a median uptake time of 77 min. PET reconstructions were performed with an ordered subset expectation maximization algorithm (OSEM) with four iterations and eight subsets. A low-dose CT scan was performed for attenuation correction of the PET emission data. The low-dose CT scan parameters using BGE smart mA dose modulation were: 100 kVp, 15–150 mA, noise index 60, 0.8 s per tube rotation, slice thickness 3.75 mm and pitch 1.375. In seven patients a diagnostic, contrast-enhanced CT (ceCT) was acquired, whereas nine patients received only a low-dose CT. The ceCT scan parameters using BGE smart mA dose modulation were: 100–120 kVp, 80–450 mA, noise index 24, 0.8 s per tube rotation, slice thickness 3.75 mm and pitch 0.984. A CT scan of the thorax, abdomen and pelvis (shallow breathing) was acquired 40–70 s after injection of contrast agent (60 to 120 ml of Iomeron 400 mg/l, depending on patient body weight), followed by a CT scan of the thorax in deep inhalation.
18F-NaF PET/CT imaging
Acquisition protocol of 18F-NaF PET/CT followed the guidelines of the Society of Nuclear Medicine [34]. Image acquisition was started after a median uptake time of 126 min post-injection, with an acquisition time of 2 min per bed position. In all patients, a low-dose CT from the skull vertex to mid-thigh was obtained first, using the same parameters as described for 68Ga-PSMA-11 PET. Low-dose CT was used for attenuation correction and anatomical correlation of lesions with increased tracer uptake on PET images. Immediately after the low-dose CT, the PET scan was performed covering the same regions. For reconstruction of PET images, the same parameters as for 68Ga-PSMA-11 PET were used.
Image analysis
All 68Ga-PSMA-11 PET/CT and 18F-NaF PET/CT images were analysed with a dedicated commercially available workstation (Advance Workstation, Version AW4.5 02, GE Healthcare), which allowed the review of PET, CT, and fused imaging data in axial, coronal, and sagittal slices. The software enabled simultanous cursor placement on corresponding structures of PET and CT images, allowing anatomic localisation of increased tracer accumulation.
PET images were interpreted independently by two board-approved nuclear medicine physicians with 6 and 14 years of clinical experience respectively, who read all data sets independently and resolved any disagreements by consensus.
In order to minimize a bias, 18F-NaF PET/CT and 68Ga-PSMA-11 PET/CT images were not read simultaneously. First, 18F-NaF PET/CT images of all patients were analysed, followed by 68Ga-PSMA-11 PET/CT image analysis at a later time point. Visual interpretation of PET images was the main criteria for reaching the final diagnosis.
With regard to assessment of malignant bone involvement on 68Ga-PSMA-11 PET images, any focal skeletal uptake higher than surrounding background activity of normal bone was considered pathological, and suspicious for bone metastasis.
With 18F-NaF PET, foci of increased tracer uptake were classified as malignant after exclusion of a benign etiology of the increased uptake on CT, e.g., degenerative disease or posttraumatic alterations. In particular lesions with pathologic 18F-NaF accumulation were interpreted as benign when they were located at joints or at the edges of vertebral bodies.
PET-positive lesions that were classified as malignant on 18F-NaF PET and 68Ga-PSMA-11 PET were categorized as osteoblastic, osteolytic, and non-visible, depending on the finding of the corresponding area of low-dose CT or ceCT images. PET-positive lesions with no changes in the bone structure on CT were regarded as bone-marrow metastases.
In addition, intensity of tracer uptake of lesions considered malignant was measured applying maximum standardized uptake value (SUVmax). For SUVmax calculation, volumes of interest were drawn automatically with a manually adapted isocontour threshold centered on pathologic foci. SUVmax was chosen due to its higher reproducibility [21] between different investigators when compared to mean standardized uptake value. The latter is always dependent on the volume drawn by the investigator, whereas SUVmax is size-independent.
For calculation of tumour to background ratio (T/B ratio) SUVmax-value of each PET-positive lesion was compared to the SUVmax-value of normal bone. For 68Ga-PSMA-11 PET, the left femur was selected for background measurements, whereas in 18F-NaF PET the shaft of the left humerus was chosen as reference for normal skeletal tracer-uptake. Furthermore, PET-positive bone lesions were classified as osteosclerotic, osteolytic, or not visible according to the underlying morphologic appearance on CT.
Data analysis
All PET-positive bone lesions judged as malignant on PET/CT scans were included for analysis. In order to assess the performance of both tracers, 18F-NaF-PET and 68Ga-PSMA-11 PET were compared on a lesion basis. For that purpose, all lesions suggestive of bone metastases on 18F-NaF PET and 68Ga-PSMA-11 PET were analysed in a second step by a side-by-side comparison of 18F-NaF-PET and 68Ga-PSMA-11 images.
Statistical analysis
Since lesions were spread among only 16 patients, statistical methods accounting for clustering within patients were used. Comparison of lesion number between 18F-NaF PET and 68Ga-PSMA-11 PET was performed with the McNemar test for clustered binary paired data as proposed by Durkalski et al. [35]. Paired clustered Wilcoxon signed-rank tests using the Rosner–Glynn–Lee method [36] were applied for the following analyses: (1) comparison of SUVmax values of bone metastases and T/B ratios on 18F-NaF PET and 68Ga-PSMA-11 PET, (2) comparison of SUVmax values in osteosclerotic, osteolytic, and CT-negative lesions on 18F-NaF PET and 68Ga-PSMA-11 PET. Unpaired clustered Wilcoxon signed-rank tests using the Rosner–Glynn–Lee method were applied for the comparison of SUVmax values between osteosclerotic, osteolytic, and CT-negative lesions. The influence of lesion size on SUVmax values was assessed using a mixed model for clustered data with random intercept and slope. A significance level of a = 0.05 (two-tailed) was applied for all p-values. Statistical analyses were performed using SPSS, version 22.0 (IBM Corp., Armonk, NY, USA) and R, version 3.3.0.
Results
In the 16 patients included in the analysis, a total of 468 lesions consistent with bone metastases were detected on 18F-NaF PET. In contrast, 68Ga-PSMA-11 PET only revealed 351 bone lesions judged positive for bone metastases (75.0% of 18F-NaF-positive lesions). The difference in lesion number between 18F-NaF PET and 68Ga-PSMA-11 PET was statistically significant (p < 0.001). A histologic confirmation of the lesions classified as metastases was not performed, mainly due to ethical and practical reasons. However, lesions suggestive of bone metastases on 18F-NaF PET either showed a morphologic correlate on low-dose or contrast-enhanced diagnostic CT (n = 365; 78.0%) or were confirmed on follow-up 18F-NaF PET-scans (n = 103; 22.0%). All 68Ga-PSMA-positive bone lesions also showed a pathologic tracer uptake on 18F-NaF PET. No additional pathologic bone lesion could be revealed with 68Ga-PSMA-11 PET that was not visible on 18F-NaF PET. Bone metastases not detectable on 68Ga-PSMA-11 PET were mainly osteosclerotic lesions (n = 66) or not visible on CT (n = 49), and in only two cases correlated with an osteolytic lesion on CT.
As to 18F-NaF PET, 365 of all 18F-NaF-positive bone lesions revealed a morphologic correlate on CT (78%). In the remaining 103 lesions (22.0%) no clear morphologic alteration could be detected on CT. Of all bone lesions visible on CT, in 347 lesions an osteosclerotic alteration was found on CT, whereas 18 lesions corresponded to an osteolysis. Detailed information on morphologic characterisation of PET-positive bone lesions is listed in Table 2.
In order to ensure a statistically correct comparison of 18F-NaF PET and 68Ga-PSMA-11 PET the main data analysis was performed including only lesions that were positive with both tracers (n = 351). Regarding the intensity of tracer accumulation of these lesions, irrespective of its underlying morphology on CT, the median SUVmax was significantly higher in 18F-NaF PET compared to 68Ga-PSMA-11 PET (27.0 vs 6.0; range: 4.0–122.0 vs 0.9–54.0; p < 0.001). Although background activity of normal bone was lower in 68Ga-PSMA-11 PET than in 18F-NaF PET (median SUVmax: 1.0 vs 2.7), T/B ratio of pathologic bone lesions was higher in 18F-NaF PET compared to 68Ga-PSMA-11 PET with a median T/B ratio of 9.8 vs 5.9 (range 1.1–90.6 vs 1.0–114.3), reaching also a statistically significant difference (p = 0.042). An overview of SUVmax values and T/B ratio of pathologic lesions and normal bone tissue is given in Table 3.
Comparing intensity of tracer accumulation in pathologic lesions between 18F-NaF PET and 68Ga-PSMA-11 PET stratified by morphologic classification on CT, a statistically significant difference in median SUVmax between both tracers was revealed in osteosclerotic (26.0 vs 5.0; p < 0.001) and lesions not visible on CT (26.5 vs 7.5; p = 0.012) respectively. In contrast, median SUVmax of osteolytic lesions did not differ significantly between 18F-NaF PET and 68Ga-PSMA-11 PET (median SUVmax: 37.0 vs 29.5; p = 0.963). A summary of SUVmax values of different types of metastases is given in Table 4.
With respect to T/B ratio of lesions visible with both tracers (n = 351), a significant higher T/B ratio of 18F-NaF compared to 68Ga-PSMA-11 was found in osteosclerotic metastases (median T/B ratio: 9.7 vs 4.7 p = 0.013). T/B ratio of lesions not visible on CT was also higher in 18F-NaF, but did not differ significantly from T/B ratio with 68Ga-PSMA-11 (median T/B ratio: 8.4 vs 7.7; p = 0.597). In contrast, T/B ratio was higher in osteolytic metastases on 68Ga-PSMA-11 PET than on 18F-NaF PET (70.2 vs 57.8); however, this did not reach statistical significance (p = 0.308). For more details regarding T/B ratios of different types of bone metastases between 18F-NaF and 68Ga-PSMA-11, see also Table 4.
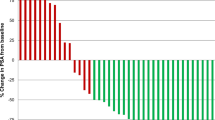
In a subgroup analysis intensity of tracer accumulation in osteosclerotic, osteolytic, and CT negative lesions was compared on 18F-NaF PET and on 68Ga-PSMA-11 PET separately. Of all lesions judged positive on 18F-NaF PET (n = 468), osteolytic metastases showed a higher median SUVmax than osteosclerotic and lesions not visible on CT (median SUVmax: 35.0 vs 23.6 vs 19.0). A statistically significant difference was only reached in the subgroup of osteosclerotic vs non visible lesions (p = 0.043), whereas the difference between osteolytic vs osteosclerotic (p = 0.285) and osteolytic vs CT-negative lesions (p = 0.206) did not show a statistical relevance. Statistical analysis of all 68Ga-PSMA-11 PET-positive lesions (n = 351) did not reveal a statistically significant difference in median SUVmax values in the subgroups osteosclerotic vs osteolytic (p = 0.355), osteosclerotic vs CT-negative (0.436) and osteolytic vs CT-negative lesions (p not available, due to low patient number). Corresponding SUVmax values of 68Ga-PSMA-11 are listed in Table 4.
We also investigated a possible correlation of lesion size measured on CT images and intensity of tracer accumulation in pathologic bone lesions on 18F-NaF PET and 68Ga-PSMA-11 PET. Among the lesions visible on CT (n = 365), tracer uptake of bone metastases was higher in lesions > 10 mm (n = 286) compared with lesions < 10 mm (n = 79) on both 18F-NaF PET (median SUVmax: 26.0 vs 17.0) and 68Ga-PSMA-11 PET (median SUVmax: 6.0 vs 3.5). See also Table 3. Statistical analysis, applying a mixed model with random intercept and slope, revealed a significant influence of size on metastasis-related tracer-uptake. An increase of 1.0 mm in size correlated positively with a rise of SUVmax of 0.425 in 18F-NaF PET and of 0.099 in 68Ga-PSMA-11 PET (p = 0.017 and p = 0.031). A significantly higher number of lesions with a size < 10 mm was detected on 18F-NaF PET (n = 79) compared to 68Ga-PSMA-11 PET (n = 52). In lesions > 10 mm the number was also higher on 18F-NaF PET than on 68Ga-PSMA-11 PET (n = 286 vs n = 245), however, the difference was not so strong (see Table 2).
Although it was not the aim of the study, we also added some preliminary data on treatment outcome of the patients included in this analysis, assessed at the first follow-up visit, that was usually performed 2 to3 months after termination of therapy (see supplement 1a, 1b).
Discussion
Knowledge of the burden of bone metastases in metastatic PC patients before starting or modifying therapy is essential for proper evaluation of therapy response.
68Ga-PSMA-11 PET/CT has been shown to establish a very sensitive method in detecting PC lesions [22, 27, 28, 37]. In particular, with respect to assessment of malignant bone involvement, a detection rate of 68Ga-PSMA-11-positive bone metastases in up to 35.9% of PC patients with biochemical recurrence has been described [22, 27, 28]. Recently published studies could demonstrate a higher sensitivity of 68Ga-PSMA-11 PET in the detection of bone metastases in PC patients in comparison to conventional bone scintigraphy including SPECT acquisition [30, 31]. However, 18F-NaF is considered the “gold standard” of available nuclear medicine bone-seeking tracers [16,17,18]. This is due to improved spatial resolution of the PET technique, but also partly due to the fact that 18F-NaF also allows the detection of non-sclerotic bone metastases [19, 38, 39]. In addition, total tumour burden of skeletal metastases measured on baseline 18F-NaF PET has been proven to have a prognostic impact on PC patients treated with 223Ra [40].
Therefore, we decided to use 18F-NaF PET as a reference to evaluate the performance of 68Ga-PSMA-11 PET for the assessment of skeletal metastases in patients with known metastatic PC, scheduled for radionuclide therapy. To date, only one case report describing a direct comparison of 18F-NaF PET and 68Ga-PSMA-11 PET in the evaluation of bone metastases in a single PC patient has been published [32]. To the best of our knowledge, this is the first original article that compares 68Ga-PSMA-11 PET and 18F-NaF PET in a cohort of metastatic PC patients.
The most important result of our study is that 18F-NaF PET showed a significant higher number of bone lesions suggestive of metastases compared with 68Ga-PSMA-11 PET (468 vs 351 skeletal metastases; p < 0.001). One possible explanation could be the fact that bone metastases in PC are predominantly osteosclerotic [41]. Bone metastases that are purely sclerotic might be missed on 68Ga-PSMA-11 PET, probably due to low tumour cell volume in this type of bone metastases, as could be already demonstrated in some PC patients by Eiber et al. [27]. In fact, in our study the majority of pathologic bone lesions were osteosclerotic on CT (n = 347; 74.2%), of which only 281 (81%) could be diagnosed on 68Ga-PSMA-11 PET. The association of the sclerotic reaction in bone metastases and intensity of tracer accumulation of 68Ga-PSMA-11 was also underlined by the finding that osteosclerotic lesions showed a significantly lower median SUVmax on 68Ga-PSMA-11 PET in comparison with 18F-NaF PET (26.0 vs 5.0; p < 0.001; see also Table 4). This is in line with a study by Janssen et al., who described a relatively low uptake of 68Ga-PSMA-11 in osteoblastic–osteosclerotic metastases compared to osteolytic metastases [42]. They also found a negative correlation of the intensity of 68Ga-PSMA-11 accumulation and the density of osteosclerotic metastases, measured with Hounsfield units on CT [42]. An example of a PC patient with predominantly osteosclerotic bone lesions showing high uptake on 18F-NaF PET and only faint tracer accumulation on 68Ga-PSMA-11 PET is given in Fig. 1.
18F-NaF PET/CT and 68Ga-PSMA-11 PET/CT performed as baseline study prior to 223Ra therapy in a 81-year-old metastatic prostate cancer patient with no therapy at time of PET (PSA: 5.74 ng/ml), revealing multiple bone metastases on maximum intensity projection (MIP) of 18F-NaF PET (a) and 68Ga-PSMA-11 PET (b). The majority of predominantly osteosclerotic lesions show a markedly increased tracer uptake on 18F-NaF PET, whereas tracer uptake of lesions on 68Ga-PSMA-11 is much lower, as demonstrated on a metastasis in the spine, marked with a red arrow on MIP images (a, b). The lesion shows a SUVmax of 51.9 on axial fused 18F-NaF PET/low-dose CT image (c, red arrow) in comparison with a SUVmax of 8.3 on axial fused 68Ga-PSMA-11 PET/low-dose CT slice (d, red arrow), appearing as purely sclerotic on axial CT images (e, red arrow)
Surprisingly, 18F-NaF PET also revealed a higher number of malignant bone lesions, which did not show a sclerotic reaction on CT, classified as either osteolytic or not visible on CT (n = 121 with 18F-NaF vs n = 70 on 68Ga-PSMA-11). It has been proven that non-sclerotic bone metastases can be visualised with both 18F-NaF PET [39] and 68Ga-PSMA-11 PET [29, 42]. This was confirmed in our study with respect to detection of osteolytic metastases, as PET-positive bone lesions with a clear osteolytic correlate on CT did show a high uptake on 18F-NaF PET (n = 18) as well as on 68Ga-PSMA-11 PET (n = 16), with a median SUVmax value of 37.0 and 29.5 respectively (see Table 4). Furthermore, both 18F-NaF and 68Ga-PSMA-11 PET also revealed PET-positive bone lesions that were not clearly visible on CT. It should be noted that the number of lesions not visible on CT was significantly higher on 18F-NaF PET compared to 68Ga-PSMA-11 PET (n = 103 vs n = 54), revealing also a significantly higher tracer accumulation on 18F-NaF PET, with a median SUVmax of 26.5 in comparison with a median SUVmax of 7.5 on 68Ga-PSMA-11 (see Table 4). However, the reason for the significant higher number of bone lesions considered as metastases without CT-correlate on 18F-NaF PET compared to 68Ga-PSMA-11 PET in our study is rather unclear. A possible explanation may be the fact that in seven patients only low-dose CT was available for morphologic characterisation. Although the quality of low-dose CT for evaluation of bone lesions seems sufficient in most of the cases [30], distinct bone alterations might be missed with low-dose CT alone. On the other hand, it is well known that malignant bone-marrow infiltration usually cannot be depicted with CT, even when high-dose, contrast-enhanced CT is applied [43]. Therefore, in our study PET-positive lesions that did not show a morphologic correlate on CT may indeed reflect bone-marrow infiltration of tumour cells, which is considered to be the first step in the development of bone metastases in PC patients [44, 45]. An example of a patient with PET-positive lesions suggestive of metastases on 18F-NaF PET with absent tracer uptake on 68Ga-PSMA-11 PET and no clear correlate on CT is shown in Fig. 2.
18F-NaF PET/CT and 68Ga-PSMA-11 PET/CT in a 82-year-old metastatic prostate cancer patient under androgen deprivation therapy (PSA: 40.56 ng/ml) scheduled for 223Ra therapy with multiple bone metastases, depicted on maximum intensity projection (MIP) of 18F-NaF PET (a) and 68Ga-PSMA-11 PET (b). The total number of lesions suggestive of bone metastases on 18F-NaF PET is higher in comparison with68Ga-PSMA-PET. Two lesions of the left iliac bone, clearly positive on MIP of 18F-NaF PET (a, red arrows) are not visible on MIP of 68Ga-PSMA-11 PET, showing a high uptake on fused axial PET/CT images of 18F-NaF PET/CT (c, red arrows). On fused axial 68Ga-PSMA-11 PET/CT no pathologic focal tracer uptake at that site can be detected (d, red arrows) with no clear morphologic correlate on axial CT (e, red arrows). In addition, a small osteosclerotic lesion of the left iliac bone (4.9 mm) on CT (e, yellow arrow) reveals an increased uptake on 18F-NaF PET (c, yellow arrow), showing no pathologic tracer uptake on 68Ga-PSMA-11 PET (d, yellow arrow)
Another interesting observation of our study was that the intensity of tracer uptake of both 18F-NaF PET and 68Ga-PSMA-11 PET positively correlates with lesion size. An increase in size of 1.0 mm is expected to result in a SUVmax value which is 0.425 units higher on 18F-NaF PET and 0.099 units higher on 68Ga-PSMA-11 PET. This can be probably explained by the well-established, size-dependent partial volume effect occuring in PET imaging [46]. The measured tracer uptake in small tumour lesions does not reflect the true amount of metabolic activity. Furthermore, the spatial resolution limit of the PET system plays a significant role in the detectabilty of lesions [47]. Lesions that are only a few millimeters in size usually cannot be visualised. This is even more pronounced in lesions with low metabolic activity and/or low tracer uptake. These two inherent problems of PET acquisition might be a possible explanation of our findings. In our study, we were able to demonstrate that lesions smaller than 10.0 mm in size revealed a lower tracer accumulation on 18F-NaF PET and 68Ga-PSMA-11 PET compared to lesions larger than 10.0 mm (median SUVmax: 17.0 vs 26.0 for 18F-NaF PET and 3.5 vs 6.0 for 68Ga-PSMA-11 PET respectively). It is especially noteworthy that median SUVmax in lesions smaller then 10 mm was markedly higher on 18F-NaF PET than on 68Ga-PSMA-11 PET (17.0 vs 3.5). In contrast to 79 lesions smaller than 10 mm positive on 18NaF PET, only 52 of these lesions could be detected on 68Ga-PSMA-11 PET (65.8%). These data indicate that small osteosclerotic metastases could be missed on 68Ga-PSMA-11 PET, but can be visualised by 18F-NaF PET, due to higher tracer accumulation. An example of a patient with a small osteosclerotic lesion which is positive on 18F-NaF PET and negative on 68Ga-PSMA-11 PET is shown in Fig. 2.
Different physical decay characteristics of 18F and 68Ga might also have an influence on lesion detectability. Due to higher positron energy of 68Ga with a longer positron range in comparison with 18F, 68Ga-based imaging is expected to have a lower spatial resolution than PET scans using 18F labelled radiopharmaceuticals [48]. In contrast, a negative impact of the different half-life of 68Ga and 18F on lesion detectability in our patient cohort is unlikely, as deviation of median uptake time of 68Ga-PSMA-11 and 18F-NaF from the half-life of the corresponding isotope was comparable (77 min and 126 min respectively).
One limitation of our study is that all patients included were not naive to therapy. In particular, 13 patients were under androgen deprivation therapy or Denosumab at the time of the PET scans. We are aware of the fact that a therapy-induced flare phenomenon might have been present on 18F-NaF PET. This phenomenon, considered as a healing response, could be a possible cause for the high number of pathologic bone lesions in 18F-NaF PET that were not visible on 68Ga-PSMA-11 PET [49,50,51]. However, flare phenomenon on bone scintigraphy is usually present in the first months after inititation of systemic therapy, with decreasing tracer uptake thereafter [51]. This is also documented in PC patients on androgen deprivation [52,53,54]. A flare reaction on bone scintigraphy has been described as unusual 3 months after onset of therapy [52,53,54]. In fact, in our study in all patients who were investigated under medication, therapy was started more than 3 months before the 18F-NaF PET scan. Furthermore, in those patients who received a PET/CT control study, pathologic bone lesions were confirmed on follow-up, rendering the diagnosis of “vital” bone metastases at baseline 18F-NaF PET plausible. Nevertheless, the results of our study have to be interpreted with caution, as an influence of therapy on the findings of the PET scans cannot be ruled out. As 18F-NaF is more sensitive than bone scintigraphy, it seems at least possible that bone remodeling is detectable on 18F-NaF PET for a longer time than generally assumed. Based on our data, the question whether 18F-NaF PET overestimates the extent of metastatic disease and 68Ga-PSMA-11 reflects the true amount of vital tumour lesions, or whether 68Ga-PSMA-11 is less sensitive than 18F-NaF PET, cannot be answered with absolute certainty. In general, this question reflects an unsolved clinical problem in PC patients with known bone metastases before modification of therapy, in whom a baseline exam usually is performed in order to monitor therapy response. It is still under debate which imaging modality, including CT and whole-body magnetic resonance imaging, constitutes the most appropriate technique to evaluate effectiveness of therapy in bone metastases [16].
In this context, another shortcoming of our study is the lack of histologic confirmation of the malignant nature of the lesions regarded as metastases. This was not possible due to ethical and practical reasons. False-positive or false-negative results can only be ruled out reliably with histology as reference standard. Even so, all lesions judged positive for metastases on both PET scans did either show a correlate on CT or were confirmed on follow-up imaging.
A major limitation of the study is the relatively low number of patients included. At the same time, the total number of tumour lesions was high, and we tried to address this issue with the application of statistical tests that account for the limited number of patients.
There is also an apparent bias in patient selection, with only three patients treated with 177Lu-PSMA-617 in comparison to 13 patients who received therapy with 223Ra. As patients treated with 223Ra tend to have a relatively high burden of bone metastases, patients with a low number of skeletal metastases might be underrepresented in this cohort. This selection bias is due to a different pretherapeutic diagnostic work-up of metastatic PC patients considered for radionuclide therapy at our department. In PC patients referred for 223Ra therapy, both a 18F-NaF scan to confirm high bone turn-over in bone metastases and a 68Ga-PSMA-11 PET, in order to exclude visceral/lymphnode metastases are performed. In contrast, in patients who are scheduled for PSMA therapy, in the majority of cases only a 68Ga-PSMA-11 PET is made.
In summary, we acknowledge the need for prospective trials with a larger patient population and histologic verification of PET-positive bone lesions in order to verify the results of our study. In particular, a head-to-head analysis of a similar number of patients treated with 223Ra (usually presenting with a high volume of bone metastases) and patients scheduled for 177Lu-PSMA-617 therapy (with a tendentially lower burden of skeletal involvement) would be of interest.
Conclusion
18F-NaF PET revealed a significantly higher number of pathologic bone lesions suggestive of metastases compared with 68Ga-PSMA-11 PET in metastatic PC patients, referred for restaging prior to initiation of radionuclide therapy. Our data suggest that 18F-NaF-PET might deliver complementary information to 68Ga-PSMA-11 PET, especially in small osteosclerotic metastases. As the determination of the true extent of skeletal tumour burden in PC patients with known metastatic disease before modification of therapy is crucial for the evaluation of therapy response, we recommend combining 18F-NaF PET with 68Ga-PSMA-11 PET for baseline assessment in PC patients considered for targeted radionuclide therapy.
References
Arnold M, Karim-Kos HE, Coebergh JW, Byrnes G, Antilla A, Ferlay J, et al. Recent trends in incidence of five common cancers in 26 European countries since 1988: Analysis of the European Cancer Observatory. Recent trends in incidence of five common cancers in 26 European countries since 1988: Analysis of the European Cancer Observatory. Eur J Cancer. 2015;51(9):1164–87.
Center MM, Jemal A, Lortet-Tieulent J, Ward E, Ferlay J, Brawley O, et al. International variation in prostate cancer incidence and mortality rates. Eur Urol. 2012;61(6):1079–92.
Bubendorf L, Schöpfer A, Wagner U, Sauter G, Moch H, Willi N, et al. Metastatic patterns of prostate cancer: an autopsy study of 1,589 patients. Hum Pathol. 2000;31(5):578–83.
Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev. 2001;27(3):165–76.
Nørgaard M, Jensen AØ, Jacobsen JB, Cetin K, Fryzek JP, Sørensen HT. Skeletal related events, bone metastasis and survival of prostate cancer: a population based cohort study in Denmark (1999 to 2007). J Urol. 2010;184(1):162–7.
Saad F, Clarke N, Colombel M. Natural history and treatment of bone complications in prostate cancer. Eur Urol. 2006;49(3):429–40.
Tait C, Moore D, Hodgson C, Brown M, Morris T, Growcott J, et al. Quantification of skeletal metastases in castrate-resistant prostate cancer predicts progression-free and overall survival. BJU Int. 2014;114(6b):E70–3.
Handkiewicz-Junak D, Poeppel TD, Bodei L, Aktolun C, Ezziddin S, Giammarile F, et al. EANM guidelines for radionuclide therapy of bone metastases with beta-emitting radionuclides. Eur J Nucl Med Mol Imaging. 2018;45(5):846–59.
Cornford P, Bellmunt J, Bolla M, Briers E, De Santis M, Gross T, et al. EAU-ESTRO-SIOG Guidelines on prostate cancer. part II: treatment of relapsing, metastatic, and castration-resistant prostate cancer. Eur Urol. 2017;71(4):630–42.
Virgolini I, Decristoforo C, Haug A, Fanti S, Uprimny C. Current status of theranostics in prostate cancer. Eur J Nucl Med Mol Imaging. 2017.
von Eyben FE, Roviello G, Kiljunen T, Uprimny C, Virgolini I, Kairemo K, et al. Third-line treatment and 177Lu-PSMA radioligand therapy of metastatic castration-resistant prostate cancer: a systematic review. Eur J Nucl Med Mol Imaging. 2017.
Poeppel TD, Handkiewicz-Junak D, Andreeff M, Becherer A, Bockisch A, Fricke E, et al. EANM guideline for radionuclide therapy with radium-223 of metastatic castration-resistant prostate cancer. Eur J Nucl Med Mol Imaging. 2017.
Evangelista L, Bertoldo F, Boccardo F, Conti G, Menchi I, Mungai F, et al. Diagnostic imaging to detect and evaluate response to therapy in bone metastases from prostate cancer: current modalities and new horizons. Eur J Nucl Med Mol Imaging. 2016;43:1546–62.
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017;71(4):618–29.
Beheshti M, Rezaee A, Geinitz H, Loidl W, Pirich C, Langsteger W. Evaluation of prostate cancer bone metastases with 18F-NaF and 18F-Fluorocholine PET/CT. J Nucl Med. 2016;57:55S–60S.
Cook GJ, Azad G, Padhani AR. Bone imaging in prostate cancer: the evolving roles of nuclear medicine and radiology. Can J Urol. 2016;23(6):8564–7.
Langsteger W, Rezaee A, Pirich C, Beheshti M. 18F-NaF-PET/CT and 99mTc-MDP bone scintigraphy in the detection of bone metastases in prostate cancer. Semin Nucl Med. 2016;46(6):491–501.
Schirrmeister H, Glatting G, Hetzel J, Nüssle K, Arslandemir C, Buck AK, et al. Prospective evaluation of the clinical value of planar bone scans, SPECT, and (18)F-labeled NaF PET in newly diagnosed lung cancer. J Nucl Med. 2001;42(12):1800–4.
Schirrmeister H, Guhlmann A, Elsner K, Kotzerke J, Glatting G, Rentschler M, et al. Sensitivity in detecting osseous lesions depends on anatomic localization: planar bone scintigraphy versus 18F PET. J Nucl Med. 1999;40(10):1623–9.
Beheshti M, Vali R, Waldenberger P, Fitz F, Nader M, Hammer J, et al. The use of F-18 choline PET in the assessment of bone metastases in prostate cancer: correlation with morphological changes on CT. Mol Imaging Biol. 2010;12(1):98–107.
Afshar-Oromieh A, Malcher A, Eder M, Eisenhut M, Linhart HG, Hadaschik BA, et al. PET imaging with a [68Ga]gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging. 2013;40(6):971–2.
Afshar-Oromieh A, Holland-Letz T, Giesel FL, Kratochwil C, Mier W, Haufe S, et al. Diagnostic performance of 68Ga-PSMA-11 (HBED-CC) PET/CT in patients with recurrent prostate cancer: evaluation in 1007 patients. Eur J Nucl Med Mol Imaging. 2017;44(8):1258–68.
Schwarzenbock SM, Rauscher I, Bluemel C, Fendler WP, Rowe SP, Pomper MG, et al. PSMA ligands for PET-imaging of prostate cancer. J Nucl Med. 2017;58(10):1545–1552 https://doi.org/10.2967/jnumed.117.191031.
Schwenck J, Rempp H, Reischl G, Kruck S, Stenzl A, Nikolaou K, et al. Comparison of 68Ga-labelled PSMA-11 and 11C-choline in the detection of prostate cancer metastases by PET/CT. Eur J Nucl Med Mol Imaging 2017;44(1):92–101.
Morigi JJ, Stricker PD, van Leeuwen PJ, Tang R, Ho B, Nguyen Q, et al. Prospective comparison of 18F-Fluoromethylcholine versus 68Ga-PSMA PET/CT in prostate cancer patients who have rising PSA after curative treatment and are being considered for targeted therapy. J Nucl Med. 2015;56(8):1185–90.
Afshar-Oromieh A, Zechmann CM, Malcher A, Eder M, Eisenhut M, Linhart HG, et al. Comparison of PET imaging with a (68)Ga-labelled PSMA ligand and (18)F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2014;41(1):11–20.
Eiber M, Maurer T, Souvatzoglou M, Beer AJ, Ruffani A, Haller B, et al. Evaluation of hybrid 68Ga-PSMA ligand PET/CT in 248 patients with biochemical recurrence after radical prostatectomy. J Nucl Med. 2015;56(5):668–74.
Ceci F, Uprimny C, Nilica B, Geraldo L, Kendler D, Kroiss A, et al. (68)Ga-PSMA PET/CT for restaging recurrent prostate cancer: which factors are associated with PET/CT detection rate? Eur J Nucl Med Mol Imaging. 2015;42(8):1284–94.
Uprimny C, Kroiss AS, Decristoforo C, Fritz J, von Guggenberg E, Kendler D, et al. 68Ga-PSMA-11 PET/CT in primary staging of prostate cancer: PSA and Gleason score predict the intensity of tracer accumulation in the primary tumour. Eur J Nucl Med Mol Imaging. 2017;44(6):941-949
Janssen JC, Meißner S, Woythal N, Prasad V, Brenner W, Diederichs G, et al. Comparison of hybrid 68Ga-PSMA-PET/CT and 99mTc-DPD-SPECT/CT for the detection of bone metastases in prostate cancer patients: additional value of morphologic information from low dose CT. Eur Radiol. 2018;28(2):610-619. https://doi.org/10.1007/s00330-017-4994-6.
Pyka T, Okamoto S, Dahlbender M, Tauber R, Retz M, Heck M, et al. Comparison of bone scintigraphy and 68Ga-PSMA PET for skeletal staging in prostate cancer. Eur J Nucl Med Mol Imaging. 2016 Nov;43(12):2114–21.
Uprimny C, Kroiss A, Nilica B, Buxbaum S, Decristoforo C, Horninger W, et al. (68)Ga-PSMA ligand PET versus (18)F-NaF PET: evaluation of response to (223)Ra therapy in a prostate cancer patient. Eur J Nucl Med Mol Imaging. 2015;42(2):362–3.
Uprimny C, Kroiss AS, Decristoforo C, Fritz J, Warwitz B, Scarpa L, et al. Early dynamic imaging in 68Ga- PSMA-11 PET/CT allows discrimination of urinary bladder activity and prostate cancer lesions. Eur J Nucl Med Mol Imaging. 2017;44(5):765–75.
Segall G, Delbeke D, Stabin MG, Even-Sapir E, Fair J, Sajdak R, et al. SNM. SNM practice guideline for sodium 18F-fluoride PET/CT bone scans 1.0. J Nucl Med. 2010;51(11):1813–20.
Durkalski VL, Palesch YY, Lipsitz SR, Rust PF. Analysis of clustered matched-pair data. Stat Med. 2003;22(15):2417–28.
Rosner B, Glynn RJ, Lee ML. The Wilcoxon signed rank test for paired comparisons of clustered data. Biometrics. 2006;62(1):185–92.
Perera M, Papa N, Christidis D, Wetherell D, Hofman MS, Murphy DG, et al. Sensitivity, specificity, and predictors of positive 68Ga-Prostate-specific membrane antigen positron emission tomography in advanced prostate cancer: a systematic review and meta-analysis. Eur Urol. 2016;70(6):926–37.
Araz M, Aras G, Küçük ÖN. The role of 18F-NaF PET/CT in metastatic bone disease. J Bone Oncol. 2015;4(3):92–7.
Even-Sapir E, Mishani E, Flusser G, Metser U. 18F-fluoride positron emission tomography and positron emission tomography/computed tomography. Semin Nucl Med. 2007 Nov;37(6):462–9.
Etchebehere EC, Araujo JC, Fox PS, Swanston NM, Macapinlac HA, Rohren EM. Prognostic factors in patients treated with 223Ra: the role of skeletal tumor burden on baseline 18F-fluoride PET/CT in predicting overall survival. J Nucl Med. 2015;56(8):1177–84.
Ibrahim T, Flamini E, Mercatali L, Sacanna E, Serra P, Amadori D. Pathogenesis of osteoblastic bone metastases from prostate cancer. Cancer. 2010;116(6):1406–18.
Janssen JC, Woythal N, Meißner S, Prasad V, Brenner W, Diederichs G, et al. [68Ga]PSMA-HBED-CC uptake in osteolytic, osteoblastic, and bone marrow metastases of prostate cancer patients. Mol Imaging Biol. 2017;19(6):933–43.
Yang HL, Liu T, Wang XM, Xu Y, Deng SM. Diagnosis of bone metastases: a meta-analysis comparing 18FDG PET, CT, MRI and bone scintigraphy. Eur Radiol. 2011;21(12):2604–17.
Jin JK, Dayyani F, Gallick GE. Steps in prostate cancer progression that lead to bone metastasis. Int J Cancer. 2011;128(11):2545–61.
Keller ET, Brown J. Prostate cancer bone metastases promote both osteolytic and osteoblastic activity. J Cell Biochem. 2004;91(4):718–29. Review
Soret M, Bacharach SL, Buvat I. Partial-volume effect in PET tumor imaging. J Nucl Med. 2007 Jun;48(6):932–45.
Moses WW. Fundamental Limits of spatial resolution in PET. Nucl Instrum Methods Phys Res A. 2011;648(Supplement 1):S236–40.
Sánchez-Crespo A, Andreo P, Larsson SA. Positron flight in human tissues and its influence on PET image spatial resolution. Eur J Nucl Med Mol Imaging. 2004;31(1):44–51.
van Schelven WD, Pauwels EK. The flare phenomenon: far from fair and square. Eur J Nucl Med. 1994;21(5):377–80.
Rossleigh MA, Lovegrove FT, Reynolds PM, Byrne MJ. Serial bone scans in the assessment of response to therapy in advanced breast carcinoma. Clin Nucl Med. 1982;7(9):397–402.
Coleman RE, Mashiter G, Whitaker KB, Moss DW, Rubens RD, Fogelman I. Bone scan flare predicts successful systemic therapy for bone metastases. J Nucl Med. 1988;29(8):1354–9.
Pollen JJ, Witztum KF, Ashburn WL. The flare phenomenon on radionuclide bone scan in metastatic prostate cancer. AJR Am J Roentgenol. 1984;142(4):773–6.
Sundkvist GM, Ahlgren L, Lilja B, Mattsson S, Abrahamsson PA, Wadström LB. Repeated quantitative bone scintigraphy in patients with prostatic carcinoma treated with orchiectomy. Eur J Nucl Med. 1988;14(4):203–6.
Sundkvist GM, Björk T, Kjellström H, Lilja B. Quantitative bone scintigraphy in patients with prostatic carcinoma treated with LH-RH analogues. Scand J Urol Nephrol. 1996;30(1):29–32.
World Medical Association. Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2000;284:3043–5.
Acknowledgements
We want to express our gratitude to all the members of our PET staff for their contribution in performing this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the principles of the 1964 Declaration of Helsinki and its subsequent amendments [55]. All patients published in this manuscript signed a written informed consent to the PET studies.
Electronic supplementary material
ESM 1
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Uprimny, C., Svirydenka, A., Fritz, J. et al. Comparison of [68Ga]Ga-PSMA-11 PET/CT with [18F]NaF PET/CT in the evaluation of bone metastases in metastatic prostate cancer patients prior to radionuclide therapy. Eur J Nucl Med Mol Imaging 45, 1873–1883 (2018). https://doi.org/10.1007/s00259-018-4048-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4048-6