Abstract
Objective
Protein sparing, the major goal of nutritional support, may be affected by the glucose/lipid ratio. This study in critically ill patients compared the efficacy and tolerance of two isocaloric isonitrogenous total parenteral nutritions (TPN) having different glucose/lipid ratios.
Design
Multicentric prospective randomized study.
Patients
47 patients with SAPS I score higher than 8 and requiring exclusive TPN.
Interventions
Patients received glucose/lipid ratios of 50/50 or 80/20. For 7 days all patients received 32 glucidolipidic kcal/kg and 0.27 g/kg nitrogen daily. All-in-one bags were prepared using industrial mixtures and a fat emulsion.
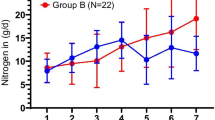
Measurements and results
We determined TPN efficacy by nitrogen balance, urinary 3-methylhistidine/creatinine ratio, transthyretin and tolerance by glycemia, and liver enzymes. After controlling for five variables with significant effects, patients receiving the 50/50 ratio during TPN had significantly higher nitrogen balance than those receiving the 80/20 ratio. The daily difference in mean nitrogen sparing effect in favor of the latter group was 1.367 g (95% CI 0.0686–2.048). Glycemia on day 4 and γ-glutamyltranspeptidase on day 8 were higher in group receiving the the 80/20 ratio.
Conclusions
In critically ill patients TPN at a glucose/lipid ratio of 80/20 ratio induces a small nitrogen sparing effect compared to the ratio of 50/50, at the expense of poorer glycemic control. The clinical significance is unclear.

Similar content being viewed by others
References
Brennan MF, Fitzpatrick GF, Cohen KH, Moore FD (1975) Glycerol: major contributor to the short-term protein sparing effect of fat emulsions in normal mal. Ann Surg 182:386–394
Jeejeebhoy KN, Andersson GH, Nakooda AF, Greenberg GR, Sanderson I, Marliss EB (1976) Metabolic studies in total parenteral nutrition with lipid in man. Comparison with glucose. J Clin Lab Invest 57:25–136
Van Itallie TB, Moore FD, Geyer RP (1954) Will fat emulsions given intravenously promote protein synthesis? Metabolic studies on normal subjects and surgical patients. Surgery 36:720–731
Wilmore DW, Moylan JA, Helmkamp GM, Pruitt BA (1973) Clinical evaluation of a 10% intravenous fat emulsion for parenteral nutrition in thermally injury patients. Ann Surg 178:503–513
Iapichino G, Radrizzani D, Solca M, Pesenti A, Gattinoni L, Ferro A, Leoni L, Langar M, Vesconi S, Damia G (1994) The main determinants of nitrogen balance during parenteral nutrition in critically ill injured patients. Intensive Care Med 10:251–254
Battistella FD, Wildergren JT, Anderson JT, Siepler JK, Weber JC, MacColl K (1997) A prospective, randomized trial of intravenous fat emulsion administration in trauma victims requiring total parenteral nutrition. J Trauma 43:52–58
Hart DW, Wolf SE, Zhang XJ, Chinkes DL, Buffalo MC, Matin SI, DebRoy MA, Wolfe RR, Herndon DN (2001) Efficacy of a high-carbohydrate diet in catabolic illness. Crit Care Med 29:318–1324
Tappy L, Schwarz JM, Schneitez P, Cayeux C, Revelly JP, Fagerquist CK, Jequier E, Chiolero R (1998) Effects of isoenergetic glucose-based or lipid-based parenteral nutrition on glucose metabolism, de novo lipogenesis, and respiratory gas exchanges in critically ill patients. Crit Care Med 26:860–867
Garrel DR, Razi M, Larivière F, Jobin N, Naman N, Emptoz-Bonneton A, Pugeat MM (1995) Improved clinical status and length of ware with low-fat nutrition support in burn patients. JPEN J Parenter Enteral Nutr 19 482–491
Gogos CA, Kalfarentzos FE, Zoumbos NC (1990) Effect of different types of total parenteral nutrition on T-lymphocyte subpopulations and NK cells 1:2. Am J Clin Nutr 51:119–122
Gore DC, Chinkes DL, Hart DW, Wolf SE, Herndon DN, Sanford AP (2002) Hyperglycemia exacerbates muscle protein catabolism in burn-injured patients. Crit Care Med 30:2438–2442
Jensen GL, Mascioli EA, Seidner DL, Istfan NW, Donitch AM, Selleck K, Babayan VK, Blackburn GL, Bistrian BR (1990) Parenteral nutrition of long- and medium-chain triglycerides and reticuloendothelial system function in man. JPEN J Parenter Enteral Nutr 14:467–471
Van Den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R (2001) Intensive insulin therapy in critically ill patients. N Engl J Med 345:1359–1367
Cardenas D, Blonde-Cynober F, Ziegler F, Cano N, Cynober L (2001) Should a single centre for the assay of biochemical markers of nutritional status be mandatory in multicentric trial? Clin Nutr 20:553–558
Cerra F, Blackburn G, Hirsch J (1987) The effect of stress level, amino acid formula and nitrogen dose on nitrogen retention in traumatic and septic stress. Ann Surg 205:282–287
Cerra FB (1987) Hypermetabolism, organ failure and metabolic support. Surgery 101:1–14
Clowes GHA, Heideman M, Lindberg B, Randall HD, Hirsch HF, Cha CJ, Martin H (1980) Effect of parenteral alimentation on amino acid metabolism in septic patient. Surgery 88:531–543
Frankenfield DC, Smith JS, Cooney RN (1997) Accelerated nitrogen loss after traumatic injury is not attenuated by achievement of energy balance. JPEN J Parenter Enteral Nutr 21:324–329
Greig PD, Elwyn DH, Askanazi J, Kinney JM (1987) Parenteral nutrition in septic patients: effects of increasing nitrogen intake. Am J Clin Nutr 46:1040–1047
Long JM III, Wilmore DW, Mason AD Jr, Pruitt BA Jr (1977) Effect of carbohydrate and fat intake on nitrogen excretion during total intravenous feeding. Ann Surg 185:417–422
Woolfson AM, Heatley RV, Allison SP (1979) Insulin to inhibit protein catabolism after injury. N Engl J Med 300:14–17
Baker JP, Detsky AS, Stewart S, Whitwell J, Marlisss EB, Jeejeebhoy KN (1984) Randomized trial of total parenteral nutrition in critically ill patients: metabolic effects of varying glucose-lipid ratios as the energy source. Gastroenterology 87:53–59
De Chalain TM, Michell WL, O’Keefe SJ, Ogden JM (1992) The effect of fuel source on amino acid metabolism in critically ill patients. J Surg Res 52:167–176
Nordenstrom J, Askanazi J, Elwyn DH, Martin P, Carpentier YA, Robin AP, Kinney JM (1983) Nitrogen balance during total parenteral nutrition: glucose vs. fat. Ann Surg 197:27–33
Paluzzi M, Meguid MM (1987) A prospective randomized study of the optimal source of nonprotein calories in total parenteral nutrition. Surgery 102:711–717
Shaw JH, Holdaway CM (1988) Protein-sparing effect of substrate infusion in surgical patients is governed by the clinical state, and not by the individual substrate infused. JPEN J Parenter Enteral Nutr 12:433–440
Chambrier C, Laville M, Rhzioul Berrada K, Odeon M, Boulétreau P, Beylot M (2000) Insulin sensitivity of glucose and fat metabolism in severe sepsis. Clin Sci (Lond) 99:321–328
Pierre EJ, Barrow RE, Harvkins HK, Nguyen TT, Sajurai Y, Desai M, Wolfe RR, Herdon DN (1998) Effects of insulin on wound healing. J Trauma 44:342-
Ferrando AA, Chinkes DL, Wolf SE, Matin S, Herndon DN, Wolfe RR (1999) A submaximal dose of insulin promotes net skeletal muscle protein synthesis in patients with severe burns. Ann Surg 229:11–18
Hinton P, Allison SP, Littlejohn S, Lloyd J (1971) Insulin and glucose to reduce catabolic response to injury in burned patients. Lancet 1:767–769
Sakurai Y, Aarsland A, Herndon DN, Chinkes DL, Pierre E, Nguyen TT, Patterson BW, Wolfe RR (1995) Stimulation of muscle protein synthesis by long-term insulin infusion in severely burned patients. Ann Surg 222:283–297
Gelfand RA, Barrett EJ (1987) Effect of physiologic hyperinsulinemia on skeletal muscle protein synthesis and breakdown in man. J Clin Invest 80:1–6
Jahoor F, Shangraw RE, Miyoshi H, Wallfish H, Herndon DN, Wolfe RR (1989) Role of insulin and glucose oxidation in mediating protein catabolism of burns and sepsis. Am J Physiol 275:E323–E331
Zang XJ, Kunkel KR, Jahoor F, Wolfe RR (1991) Role of basal insulin in the regulation of protein kinetics and energy metabolism in septic patients. JPEN J Parenter Enteral Nutr 15:394–349
Burke JF, Wolfe RR, Mullany CJ, Mathews DE, Bier DM (1980) Glucose requirements folowing burn injury. Ann Surg 190:274–285
Clarke PJ, Ball MJ, Kettlewell (1991) Liver function tests in patients receiving parenteral nutrition. JPEN J Parenter Enteral Nutr 15:54–59
Quigley EMM, Marsh MN, Shaffer JL, Markin RS (1993) Hepatobiliary complications of total parenteral nutrition. Gastroenterology 104:286–301
Buchmiller CE, Kleiman Wexler RL, Ephgrave KS, Booth B, Hensley II CE (1993) Liver dysfunction and energy source: results of a randomized clinical trial. JPEN J Parenter Enteral Nutr 17:301–306
Messing B, Bitoun A, Galian A, Mary JY, Goll A, Bernier JJ (1977) La stéatose hépatique au cours de la nutrition parentérale dépend-elle de l’apport calorique glucidique? Gastroenterol Clin Biol 1:1015–1025
Author information
Authors and Affiliations
Corresponding author
Additional information
This research was supported by a grant from Fresenius Laboratories
Rights and permissions
About this article
Cite this article
Boulétreau, P., Chassard, D., Allaouchiche, B. et al. Glucose-lipid ratio is a determinant of nitrogen balance during total parenteral nutrition in critically ill patients: a prospective, randomized, multicenter blind trial with an intention-to-treat analysis. Intensive Care Med 31, 1394–1400 (2005). https://doi.org/10.1007/s00134-005-2771-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2771-5