Abstract
The chapter focuses on three crucial elements of social and behavior change (SBC) preparedness within the realm of risk communication. The first section of the chapter describes how to implement a systematic first response to a new epidemic or outbreak. The World Health Organization (WHO)/The Global Outbreak Alert and Response Network (GOARN) framework provides a comprehensive structure to operationalize the immediate national level response for SBC. Ethiopia’s first response was well coordinated and planned, and importantly, started before the detection of the first COVID-19 case in the country. The second section of the chapter provides pooled estimates of COVID-19 prevention behaviors in the country which show a pattern of uneven adoption. The need to develop strategic SBC approaches for both behavior change and behavior maintenance is highlighted. Finally, the third section of the chapter deals with the mental health context during the pandemic in Ethiopia. We propose an integration of community-based mental health support with SBC preparedness activities.
The chapter conducts a meta-analysis of peer reviewed literature on three COVID-19 preventive behaviors and on the huge mental burden borne by Ethiopians during the COVID-19 pandemic. The guidelines for practice provided in the chapter are globally applicable. We hope that Ethiopia’s collective experience results in better success in the global fight against COVID-19.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Introduction
Ethiopia is Africa’s second most populous country, with an estimated population of 115 million [1]. Yet the country had recorded only 470,760 COVID-19 infections and 7,510 deaths as of May 11, 2022 [2]. Several theories exist to explain the lower rates of infection and fatality in African countries including younger age of the population, cross immunity from other infectious diseases, and limited testing and surveillance [3]. The Ethiopian government’s early response to the pandemic may be another contributor. Ethiopia ranks third in terms of COVID-19 preparedness among 9 African countries that had testing and Ready Score data available [4].
The first section of this chapter provides a case study of how the Ethiopia government acted quickly to mitigate the impact of the COVID-19 pandemic through mobilization of the local and international emergency response community and implementation of a coordinated risk communication and community engagement (RCCE) strategy. We describe the nation’s application of the RCCE prevention framework to enable the adoption of a systematic response during March 2020–October 2020. We also assess how COVID-19 prevention activities were monitored and used for adaptive management during this time period.
The second section provides an analysis of behavioral and mental health trends in Ethiopia from March 2020 to April 2022 and identifies lessons learned for the nation’s ongoing COVID-19 risk communication strategy. Using published peer-reviewed literature, we assess the pooled prevalence estimates of COVID-19 preventive behaviors and of mental health disorders in healthcare workers and the general population. Pooled estimates provide more stable estimates which take into consideration regional and within region variations. This analysis, as well as lessons learned from the Johns Hopkins University Center for Communication Programs (CCP), highlights the need to develop both short-term and long-term objectives to mitigate not only the immediate health impacts of the COVID-19 pandemic, but also mental health indicators.
The objectives of the chapter are as follows:
-
1.
To share Ethiopia’s early SBC emergency response process during the COVID-19 pandemic that can inform risk communication preparedness guidelines for future epidemics.
-
2.
To identify gaps in COVID-19 prevention efforts by examining peer-reviewed literature from 2020 to 2022 on adoption of COVID-19 prevention behaviors.
-
3.
To understand the context of mental distress in healthcare workers and the general population by assessing the magnitude of the problem and factors associated with mental disorders, and to offer insights on how to address mental health challenges through the risk communication and community engagement (RCCE) prevention framework.
The COVID-19 Pandemic in Ethiopia
Ethiopia’s first COVID-19 case occurred on March 13, 2020. The country experienced four subsequent waves of COVID-19 [2]. The four waves are shown in Fig. 1. The second wave saw the highest share of COVID cases. However, a sharp uptick of confirmed cases was also observed in the fourth wave. The highest death rate was observed in the third wave, and the lowest death rate was recorded in the fourth wave.
Understanding how the pandemic is unfolding, with periods of less transmission punctuated by severe outbreaks, is central to SBC communication planning, as described later in this chapter.
Emergency Preparedness in Ethiopia
Under the revised International Health Regulations (IHR–2005), countries are required to develop core capacities for responding to public health emergencies that may have international implications [5]. Emergency preparedness spans a number of core capacities including risk communication. States are assessed on emergency preparedness through the WHO Joint External Evaluation (JEE) [6]. Data from the JEE is used to create an aggregated ReadyScore for each country that is published on the Resolve to Save Lives: Prevent Epidemics website. Of 31 countries in Africa with a ReadyScore, Ethiopia ranks fifth highest with a score of 52 based on the JEE conducted in the country in 2016 [4, 7]. There are indications that the nation’s emergency preparedness improved based on the self-assessed “all capacities average” of 72% as of May 2022, which compares favorably with the regional average of 48% and a global average of 64% [4].
Using the self-assessment tool, the country has consistently scored 80% for core capacity of risk communication since 2018 and above average regional scores of less than 64% annually [4]. A well-developed SBC preparedness structure is an important component of the health system’s readiness to mount an effective and early emergency response [8]. The Ethiopian government was therefore prepared to commit to a prevention framework that prioritized risk communication in the very early days of the pandemic, prior to cases being recorded in the nation. CCP, which has a long-standing presence in the country, collaborated with the government along with the WHO, the United Nations International Children's Emergency Fund (UNICEF), the Centers for Disease Control and Prevention (CDC), and the United States Agency for International Development (USAID) implementing partners, and other major stakeholders to support RCCE activities for the prevention and management of early cases. These efforts were supported by USAID through Breakthrough ACTION, the agency’s flagship global SBC project.
As a technical SBCC partner to governments in the management of disease outbreaks, CCP identified key elements of SBC preparedness during the Ebola outbreak in Guinea in February 2021, noting that it is both “….a short- and long-term process where preparedness is focused on public communication, counseling, stigma reduction, immediate prevention response that includes promoting prevention behaviors, transmission of accurate information, and transmission of epidemic related information that builds trust within communities and which reduces fear” [9]. As we continue to expand our understanding of SBCC preparedness, there was a need to develop both short- and long-term communication objectives for the prolonged COVID-19 pandemic.
COVID-19 Risk Communication in Ethiopia
The WHO JEE focuses on five indicators to assess risk communication preparedness among members states. These five indicators provided the structure for the Emergency Operations Center (EOC)’s risk communication efforts in Ethiopia [6].
-
Risk communication systems: Formal and clearly recognized systems that will guide the development and implementation of a risk communication strategy “during times of emergency”, determine who will make decisions; and how decisions will be made.
-
Partner and internal coordination: Ensure that all key partners (external partners and government agencies) participate in the risk communication system and coordinate activities and messaging to ensure optimal timing, reach, and consistency of important information.
-
Public communication: Use of media and public channels to communicate information about COVID-19 quickly and effectively.
-
Community engagement: Focuses on reaching out to vulnerable communities to engage them in identifying and addressing communication needs and creating channels of engagement that acknowledge contextual factors and preferences.
-
Addressing uncertainty and perceptions and managing misinformation: This is a priority for all risk communication and includes efforts to track rumors and misinformation and provide a rapid and clear response.
With USAID support, Breakthrough ACTION worked alongside the Ethiopian government and non-governmental partners to improve core competencies across all five areas and ensure a comprehensive, coordinated response to COVID-19. A key aspect of risk communication was reaching out to a large number of people through public communication to accurately describe risk and motivate behavior change without creating fear and panic among the population. SBCC campaigns can be defined as purposive attempts to inform or influence behaviors in large audiences within a specified time period using an organized set of communication activities and featuring an array of mediated messages in multiple channels generally to produce non-commercial benefits to individuals and society [8, 9, 10]. SBCC approaches in Ethiopia during the first months of the pandemic included mass media; social mobilization campaigns using audio mounted vans; and community engagement activities including facilitating community discussions and COVID-19 education in public places such as marketplaces, religious institutions, and community meetings. The Ethiopia government launched a highly effective text messaging campaign via mobile phones and inserted prevention messages into telephone answering systems. All of these interventions formed the cornerstone of an effective COVID-19 prevention strategy during that time period.
The next section of this chapter describes the RCCE’s activities from March 2020 to October 2020. We present data from Breakthrough ACTION’s continuous monitoring that captured major achievements across the five pillars of the WHO/Global Outbreak Alert and Response Network (GOARN) framework. Figure 2 presents the WHO/GOARN indicators that form the framework for the risk communication approach.
Risk Communication Systems
The Ethiopian Public Health Institute (EPHI), which is responsible for responding to public health emergencies in the country, activated its EOC after the first COVID-19 case was reported in China on December 31, 2019, well before COVID-19 was declared a pandemic. The EOC was overseen by a national technical advisory team created by the Minister of Health, with the EPHI Director serving as Secretary. The EPHI Deputy Director served as the Chairperson of the EOC. The RCCE unit was established under the national EOC. Breakthrough ACTION project, as an active member of the communication technical working group in Ethiopia, provided technical support to EPHI to create the RCCE committee and its terms of reference based on WHO guidelines. The unit is composed of relevant departments from the Ministry of Health (MOH) including the Directorates of Public Relations and Communication, Health Promotion, and the Health Extension as well as multilateral and implementing partners. Overall, there were about 15 full-time experts from various implementing partner institutions that served on the RCCE committee. All implementing partners, including CCP, provided at least one dedicated full-time expert to the national RCCE team. The team held weekly virtual meetings and reviewed progress of the response activities. This level of effort across the government directorates and implementing partners enabled a highly coordinated RCCE response in the country.
The national EOC addressed several key functions of the emergency response: case management, logistics and supply, public risk communication and community engagement, and laboratory and diagnostic services. Public health institutes at the regional level established EOCs in 11 regions including in various city administrations, in a similar manner.
Breakthrough ACTION supported the national and regional RCCEs to regularly review and update the risk communication plan. The project participated in daily reviews of new developments regarding the status of the outbreak in Ethiopia and subsequent preparations/revisions of the response plan with RCCEs at both the national and regional level.
Partner and Internal Coordination
As an active member of the RCCE, Breakthrough ACTION helped develop the first strategic communication plan to respond to COVID-19 at both national and regional levels. The project adapted its global synthesized guidance for COVID-19 message development to the Ethiopia context. The guide served as a reference for partners and national and regional RCCEs to design risk communication materials on COVID-19.
In the early stages of the pandemic when countries were trying to prevent COVID-19 from entering their borders, Ethiopia focused on the transportation corridors, especially the Bole International Airport, Ethiopian Airlines, and Addis Ababa international hotels. Breakthrough ACTION supported the RCCE to provide orientation for 3,000 Ethiopian Airlines flight crew members and airport personnel that included the COVID-19 case definition guidelines for managing and reporting and development of a universal precaution kit.
In collaboration with other partners, Breakthrough ACTION developed multisectoral engagement guidelines for interventions involving religious leaders, hotels, and media professionals. The project supported the national RCCE committee to develop and provide orientation to hotel managers in Addis Ababa and other tourist destination towns. Managers were equipped with quick guidelines on how to orient the rest of the hotel staff. The project supported the RCCE committee in developing training programs for all regional and zonal focal persons on harmonized action plans and helped to identify and reach out to vulnerable groups (e.g., nursing home residents, senior citizens, and people with chronic diseases).
The project provided technical support to regional RCCEs in conducting supportive supervision (SS) in collaboration with other departments in the regional health bureaus (RHBs) to woredas (districts), primary health care units, and health posts at the ground level. The SS aimed to enhance performance of the COVID-19 response activities and to mitigate the effect of COVID-19 on routine health services uptake behavior of the community. The SS team provided on-the-spot technical assistance to the visited woredas (districts) and health facilities based on identified gaps.
To facilitate learnings and knowledge sharing among partners, Breakthrough ACTION designed an online COVID-19 knowledge management platform. The platform helped partners to easily access resources related to COVID 19 prevention. It was launched in July 2020 with more than 90 risk communication tools uploaded and disseminated to the partners (Fig. 3).
Public Communications
After the first COVID-19 case was reported in Ethiopia, the RCCE committee’s strategy shifted from preparedness to response mode. A mechanism for daily press releases was established with a fixed time and place that was communicated to all media in advance. The RCCE team was responsible for compiling all new COVID cases, deaths, and recovery data coming through case management teams from all the regions and city administrations. The Minister of Health was identified as the official spokesperson who communicated with the press each day, after which the press release was also posted on social media.
In collaboration with national and regional RCCEs, Breakthrough ACTION designed and disseminated 39 radio spots and six television (TV) spots for dissemination through national and regional media (both public and private), and 53 unique print materials including banners, posters, leaflets, and stickers for distribution to the regions. These materials contained key messages on routes of transmission and prevention methods including handwashing, masking, and distancing. The radio and TV spots were disseminated through national and regional radio and TV channels, both public and private. The messages across all media reached an estimated 25 million people, excluding repeated counts (Fig. 4). In addition, the project created social media content to communicate accurate information to the public and tapped into existing and new platforms such as websites, Facebook, and Twitter pages of the MOH, EPHI, and Regional Health Bureaus to post daily COVID-19 updates.
Breakthrough ACTION supported the staff of the existing 952 call centers with orientation and training on how to respond to calls and questions about COVID-19. In addition, the project helped to establish a new national 8,335 call center and regional call centers in 11 regions. Breakthrough action provided basic counseling training for the counselors, developed a Q and A that served as a reference for counselors, and oriented all the call center staff to respond to queries from the public.
A guide to engaging the Ministry of Transportation included messages that could be transmitted at transport stations through long distance buses and city buses. Posters, banners, and stickers were developed to create awareness for travelers and the public transportation team. A directive to reduce the number of people who travel in each bus was released.
To assess message reach to the audiences and level of recall, Breakthrough ACTION Ethiopia conducted a phone-based assessment of a randomly sampled group of 1,000 individuals. Findings of the assessment were used by the project and partners to identify focus areas for COVID-19 SBC.
Community Engagement
In order to engage various communities and influential groups, Breakthrough ACTION provided technical and financial support for the development of engagement guides for religious leaders, IDIRs (informal community support groups in Ethiopia), volunteers, nursing homes, schools, and industrial parks. The project supported the national and regional RCCE team to organize advocacy and orientation workshops for these different groups.
Local community groups played a significant role in raising public awareness on COVID-19 and promoting preventive behaviors. The project provided orientation to health extension workers (HEWs) and religious leaders focusing on social mobilization for COVID-19. The orientation was given to a total of 424 HEWs and 58 religious leaders (Fig. 5).
Addressing Uncertainties and Managing Misperceptions
In the early phase of the pandemic, the project messaging focused on raising public awareness of transmission and prevention methods. As the pandemic quickly progressed, misconceptions relating COVID 19 with that of “666 bad spirit” were identified as a barrier for preventive practices. The project designed messages addressing this misconception and focused on identifying and responding to rumors and misconceptions. The project supported the national and regional RCCEs to develop tools to help identify, evaluate, and respond to rumors. This effort included development of a misinformation management guide; establishment of a rumor and misinformation management team at national level; online and community level platforms to collect, analyze, and prioritize rumors and misinformation; and a system to quickly respond to them. All the above critical steps facilitated the creation of timely knowledge on COVID-19 among the public and helped to address misinformation and misconceptions.
In collaboration with the national and regional RCCEs, the project provided risk communication training to 186 regional media professionals. The training covered topics including facts about COVID 19 and the role of media in promoting COVID-19 preventive behaviors (Fig. 6). An information sheet for media outlets and a pocket guide for government spokespersons were also designed and distributed to media professionals to frame their role on risk communication about COVID-19.
Timeline for RCCE Activities and Pivotal Events
The following timeline describes the major steps taken during the first phase of the pandemic in Ethiopia to support the five core competencies of risk communication systems, coordination, public communication, community engagement, and management of misperceptions, along with important external events that changed the direction or nature of the outbreak. As described under previous sections, the strategy initially focused on the transportation sector to prevent the virus from entering the country. Once the first case was documented, the strategy quickly shifted to emphasizing prevention.
Factors that Contributed to the Success of the RCCE
High-level political and administrative leadership and commitment to coordinate the COVID-19 pandemic response in the country, capacity strengthening efforts of various stakeholders, and a unified communication campaign were all key factors in the success of the RCCE’s efforts in Ethiopia. Strong partnerships with WHO, UNICEF, USAID, and CDC, who were all willing and committed to bring financial and technical resources to Ethiopia; an active EOC; and active engagement of leadership at the highest level, especially the Minister of Health and the EPHI all contributed to an effective and well-coordinated RCCE platform. This heightened level of coordination and collaboration was necessary to implement response activities and interventions.
When the COVID pandemic challenged the world, there was an enormous strain on the existing health systems and structures of many developing countries. Countries needed full-time engagement of the RCCE to manage the situation. Experts from various organizations, who served full-time on the RCCE, played a critical role in multi-stakeholder coordination. Harmonizing messages, daily press releases, branded communication materials development, and active engagement of different stakeholders were made possible with systems strengthening and coordination efforts.
Breakthrough ACTION provided capacity building training to national and local media professionals, regional and zonal RCCE, health promotion focal persons, and hotline counselors. To accelerate the response mechanism at the community level, a mobile-based training module was developed. This resulted in training of all HEWs in larger regions.
Breakthrough ACTION designed and used a monitoring system to assess the performance of the risk communication activities and used the results for adaptive management. The project provided technical support to regional RCCEs in conducting SS in collaboration with other departments in the regional health bureaus to woredas (districts), primary healthcare units, and health posts at the ground. The SS aimed to enhance performance of the COVID-19 response activities and to mitigate the effect of COVID-19 on routine health services uptake behavior of the community. The SS team provided on-the-spot technical assistance to the visited woredas and health facilities based on identified gaps.
Adoption of COVID-19 Prevention Behaviors and Adverse Mental Health Outcomes in Ethiopia
In this section of the chapter, we present evidence of the adoption of three COVID-19 prevention behaviors in Ethiopia: (a) wearing a face mask, (b) handwashing with soap, and (c) social distancing of two meters. In addition, the evidence on enormous mental distress experienced by almost every segment of the population is presented, as mitigating stress is a crucial aspect for reducing the negative impacts of the COVID-19 pandemic. We opted for a literature review and meta-analysis of COVID-19 behaviors and mental health outcomes to provide more stable estimates of prevalence ratios calculated through pooled estimates.
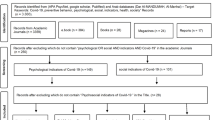
A systematic search was performed using the PubMed and Google Scholar databases. The peer-reviewed literature search included papers published from March 9, 2020 to April 25, 2022. The search was done using the following search terms: “COVID-19” and “Ethiopia” or “social distancing” or “wearing a mask” or “hand washing” or “mental disorder.” The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guided the literature review. We identified a total of 8,674 articles (8,509 from PubMed and 165 from Google Scholar databases, of which 16 studies measured COVID 19 preventive measures and 20 studies measured mental disorders. The analysis consisted of overall and subgroup pooled analysis by regional states and different population segments. The results are presented through forest plots. The diamond in the forest plot indicates the summary measure, the square boxes provide the prevalence ratio, and the size of the box determines how significant the prevalence ratio of a single study is in comparison to the pooled estimate. The horizontal line running through the box is indicative of the 95% confidence interval around the prevalence, with the length of the line representing the width of the confidence interval. The vertical line represents the pooled prevalence estimate. Weights are assigned to each study based on sample size.
Heterogeneity implies the extent to which individual prevalence estimates are different from each other. Heterogeneity across individual studies was assessed by I-squared statistic with percentage values ranging from 0 to 100%. A value of 0% indicated no observed heterogeneity, and larger values showed increasing heterogeneity. Heterogeneity among the included studies was tested using the chi-square (χ2) test statistic (Cochran’s Q statistic). The P values were obtained by comparing the statistic with a chi-square test distribution with k − 1 degrees of freedom where k is the number of studies.
Table 1 presents a list of all the peer-reviewed papers in the literature by the three COVID-19 preventive behaviors and by mental disorders. It also provides the regions where the studies were conducted, the population group that was surveyed, and the sample size for each study. Additionally, the prevalence of the preventive behaviors or mental disorders appears along with 95% confidence intervals.
COVID-19 Prevention Behaviors in Ethiopia
Face Mask Use
Across 15 quantitative studies, the sample size varied from 384 to 12,056, covering a range of respondents from household members to healthcare workers to non-health-related employees. The overall pooled estimates of face mask use in Ethiopia was 67% (95% CI 60.0–76, Fig. 1). A regional analysis of mask use indicated a wide variation within and between the four major regions of Ethiopia (Fig. 2). The highest face mask use was in Addis Ababa (81%) and Oromia (83.1%) while Southern Nations, Nationalities, and Peoples’ Region (SNNPR) (58%) and Amhara (61%) had much lower rates of mask use. The annual trend analysis from 2020 to 2021 indicates that mask use peaked in 2020 followed by a downward trend in 2021. A high level of heterogeneity (I2 > 99.64%, p = 0.001) is evident for all four regions indicating local level variations within the district. These findings are of importance as public communication campaigns should be supported with strong audience segmentation.
The sub-group analysis among different population groups (Fig. 3) indicates that mask use was significantly high among healthcare workers (81%), employees other than healthcare workers (61%), and health facility visitors (70%), followed by household heads and members (64%). Medical students and taxi drivers had lower mask use (50%). And the lowest mask use was in pregnant women (6.6%), prisoners (25.5%), and youth (26.9%). Some of the reasons provided for low mask use were unemployment, livelihood disruptions, and political context. In a study in Dessie city, Amhara, about half the respondents stated they felt discomfort while wearing a mask (Figs. 8, 9 and 10).
Handwashing with Soap
The overall pooled estimates of proper handwashing practice in Ethiopia during the COVID-19 pandemic was 79% (95% CI 73–86, Fig. 4) with highly significant heterogeneity between studies (I2 = 99.48%, p = 0.001). About five studies reported low prevalence of handwashing with soap, from 9 to 45%. One of the barriers to handwashing with soap was lack of availability of water and soap. The pooled estimates of proper handwashing in Addis Ababa (90%) were higher than the handwashing practices in other regional states (Fig. 5). The highest proper handwashing practice is seen in Oromia (84%) followed by Amhara (76%). Handwashing in SNNP was 65%. Handwashing with soap was highest among healthcare workers (91%) followed by health facility visitors (86%). The lowest handwashing practice was reported by pregnant women (9.6%), health facility visitors (30.5%), youth (33.3%), and prisoners (45.5%). Proper handwashing practice was high among healthcare workers (91%) (Figs. 11, 12 and 13).
Social Distancing
The practice of maintaining a distance of two meters between people seemed to be among the most difficult COVID-19 prevention behaviors to adopt in Ethiopia. The overall pooled prevalence estimate of social distancing was 60% (95% CI 39 - 80, Fig. 7) with substantial heterogeneity between studies (I2 = 99.91%, p = 0.001), which was lower than the pooled estimates of mask wearing and handwashing with soap. Social distancing in SNNP was lowest (41%), and the highest was reported in Addis Ababa (73%, Fig. 8). Social distancing was highly practiced among healthcare workers (89%) followed by employees outside the health sector (82%). The pooled estimates of social distancing practice were lower than the national average, among household members (25%), medical and health science students (32.4%), and health facility visitors (35.5%). The practice of social distancing was lowest in prisoners (2.1%, Fig. 8).
Among the 11 studies reviewed, eight presented data collected during the initial phase of the pandemic from April 2020 to November 2020. A study of 6,007 high-risk persons in Addis Ababa in April [20] found that respondents who had used the 8335 free call center were 1.3 times more likely to report knowledge of COVD-19 transmission routes. High levels of protective behaviors practiced by government workers point toward the effectiveness of the RCCE’s early communication efforts, with 89.5% reporting proper social distancing and higher percentages reporting mask wearing (95.9%) and handwashing (94.5%) [21]. However, social distancing as a primary prevention practice was practiced less consistently than mask wearing due to the impracticalities of distancing in markets, restaurants, and public transport transit points [24] (Fig. 14, 15 and 16).
The Mental Health Burden During COVID-19
We examined 15 peer-reviewed papers on mental distress in different sub-groups of the population. The data indicated that a parallel mental health pandemic afflicted Ethiopians, even as people are coming to terms with disruptions caused by the pandemic. The need to adequately address mental health in future waves or newer epidemics has become the most critical coping strategy to strengthen peoples’ abilities to manage COVID-19 waves and their consequences.
Studies on healthcare workers in different parts of Ethiopia show that the extent and severity of the stress experienced by healthcare workers was significantly higher than in pre-pandemic times [32,33,34,35]. Levels of depression in healthcare workers ranged from 21 to 59%, and anxiety was equally high. The studies recommended a continuous assessment of healthcare workers during the pandemic to identify healthcare workers with mental distress. Women healthcare workers were significantly more likely to experience mental distress than male workers according to a study conducted in Oromia and Addis Ababa (N = 816) [51].
The general population has not been spared the anxiety, depression, insomnia, and stress of the COVID-19 pandemic. Mental discomfort experienced due to the COVID-19 pandemic impacted people at all levels from loss of livelihood, lockdowns, loss of loved ones to COVID-19, closure of schools and universities, and managing chronic and infectious diseases in the face of severe impacts on the availability of health services. One study on the general population (N = 660) showed that 32% of the respondents had depression symptoms, 25% experienced anxiety, and 14% felt stressed [31]. The Depression, Anxiety, Stress, and Insomnia (DASS 21) scale was used by several studies to measure mental health outcomes. Risk factors associated with mental disorders in the general population included being female, having comorbidities, having a history of medical illness, and smoking.
Patients with chronic illnesses (N = 423) also showed a high level of depression symptoms (55%) and anxiety (61%) which indicated that being female, widowed, or having poor social support were strongly associated with mental disorders [40]. A study conducted in the Tigray region with COVID-19 patients in quarantine (N = 371) showed that 18% suffered from depression. Those who were female, unemployed, and felt stigmatized were significantly more likely to be depressed [37]. Persons with disabilities also showed very high levels of depression (46%) [40]. Policemen were not spared mental distress during COVID times with 29% reporting symptoms of depression and 30% showing feelings of anxiety (N = 385) according to a study from Dessie town, Amhara [42].
Pooled estimates of prevalence ratios for depression, stress, anxiety, and insomnia are provided below through forest plots (Fig. 17, 18, 19, and 20).
Figure 9 The pooled prevalence estimate of depression was 37% (95% confidence interval, 29–45) with high heterogeneity between studies (I2 = 98.16%, p = 0.0001).
Figure 10 The pooled prevalence estimate of stress was 49% (95% confidence interval, 38–60) with significant heterogeneity between studies (I2 = 98.37%, p = 0.0001).
Figure 11 The overall pooled estimates of anxiety during COVID were 46% (95% CI 37–55%) with high heterogeneity between studies (I2 = 98.6%, p = 0.0001).
Figure 12 The pooled prevalence estimate of insomnia (sleep disorder) was 38% (95% confidence interval: 15–61) with significant heterogeneity between studies (I2 = 99.3%, p = 0.0001).
Discussion and Guidelines for SBC Preparedness
We focused on immediate emergency SBC preparedness in the first part of the chapter, which began even before the first case of COVID-19 was detected in Ethiopia. We outline complex implementation processes related to coordination and planning that led to a synchronized response of government agencies with many stakeholders. Some of the key factors that ensured the functioning of the risk communication efforts included: (1) the Ethiopian government’s early mobilization of resources and establishment of the EOC to serve as a coordination hub; (2) inclusion of all major directorates and international partners in the RCCE, including the government’s decision to work with a specialized agency with expertise in strategic communications and public health; (3) application of the WHO/GOARN framework to guide RCCE strategy and activities; and (4) activation of regional EOCs, which further supported harmonization and implementation of RCCE activities throughout the country. SBC preparedness relies on bringing together key partners and establishing clear roles and contributions of each to implementing a consistent and cohesive RCCE strategy [8].
The chapter discusses the processes of establishing a real-time SBC response to a new emergency that threatened lives, economies, and the very fabric of society. The WHO/GOARN framework provided the structure for establishing a quick and responsive SBC program to tackle the early stages of the pandemic. The analysis of mental health needs in the country only serves to underscore the need for an ongoing effective SBC response with both short- and long-term objectives, given the pandemic’s devastating impact across all domains of life. The advent of new variants complicates the scenario as the virus can mutate to unleash newer and more potent waves of COVID-19. The lessons learned from the detailed description of the early response to the pandemic can be applied to emergency response for emerging infectious diseases beyond COVID-19. Using the implementation narrative of the risk communication program in the early preparedness and response stages, other countries and states can emulate the Ethiopian effort in the face of new waves of COVID-19 or emerging diseases.
Lessons learned from the Ethiopia experience include:
-
(a)
Ensure that the country/state has well established RCCE systems which can assume a leadership role in formulating an SBC preparedness strategy.
-
(b)
The WHO/GOARN framework structure should be used in formulating the response.
-
(c)
Select a public communication partner capable of creating persuasively powerful campaigns that provide accurate, focused, and relevant information.
-
(d)
The early days of immediate response should include trusted sources of information that can allay fears of the community.
-
(e)
Establish a system that can activate youth volunteers and community health workers to lead some of the community engagement efforts.
-
(f)
Coordination mechanisms should be set up at the level of the central ministries.
Evidence Related to Mask Use, Handwashing with Soap, and Social Distancing
Our chapter is limited to the role of preventive behaviors and mental health outcomes. It does not address the role of vaccines in the COVID-19 pandemic. There is evidence to indicate that after the early systematic response to the pandemic, the adoption of COVID-19 prevention behaviors remained uneven with several ups and downs between waves. The challenge of consistent adoption of mask use, handwashing with soap, and social distancing is riddled with all the barriers surrounding long-term behavior change, in addition to the enormous stress that the pandemic unleashed on unsuspecting populations. These barriers include difficulty of converting behaviors into habit behaviors, the lack of social norms and social approval around these behaviors, and living conditions within Ethiopia that prevent many people from adhering to social distancing. Therefore, as the COVID-19 behavioral literature review from studies in Ethiopia suggests, adherence to the core prevention strategies needed to break the cycle of COVID-19 infections was at best uneven.
Our behavioral analysis of peer-reviewed literature revealed that people adopt behaviors inconsistently and start and stop at will, irrespective of government guidelines. This gap can be articulated as one where behavior maintenance is not consciously promoted or achieved. COVID-19 messages themselves often give the impression that these are short-term measures. However, with the pandemic entering the third year, it is necessary to develop a cogent long-term behavioral strategy that is acceptable to people.
The approach of SBC preparedness entails the development of a long-term strategic plan for all pillars of risk communication. This plan should be developed such that campaigns address the immediate needs of calming populations as well as promoting planned approaches to behavior change and behavior maintenance. SBC preparedness will require each country/state to have databases of creative agencies, public health experts, and community-based organizations (CBOs) in addition to the available government resources. These agencies, public health experts in health behavior change, and CBOs need to be engaged in collectively developing SBC strategic plans.
Campaigns and community engagement efforts need to be infused with ‘shared compassion’, increasing people’s trust and soothing their fears. By shared compassion, we mean arousing feelings of empathy within both the provider and the receiver. It is an equitable partnership when the receiver can also strengthen the provider. The provider can be a healthcare worker or a CBO or a neighbor and the receiver can be any member of the community. A positive emotional element needs to be promoted which can lead to increasing feelings of wellbeing and reducing mental distress. Community champions have successfully addressed common mental disorders in a rural area of Maharashtra, India [52]. A recent needs assessment by CCP Ethiopia found that young people want to be involved in helping others [53]. A database of adolescent youth groups can also be prepared and tapped.
Going digital is essential to make public communication campaigns and community engagement activities work in real time and to amplify the reach of media campaigns. Simple tools such as the digital relay, which works offline, can be used. The digital relay can reach the last mile of the population and can be triggered to saturate populations with accurate and motivating content [54]. Digital orientation and counseling packages can be prepared for volunteers. In addition, the SBC preparedness strategy needs to include a separate social media preparedness approach. In the past two and a half years of the pandemic, our dependence on electronic media, social media, and virtual communications has increased exponentially. We need to plan a social media strategy that promotes shared compassion, reduces posts which spew hate, and provides a platform where people can seek succor from the pandemic.
Habit-level behavior change takes a long time and if we expect to achieve this sustainable behavior change at a population level, the challenge is even greater [55]. In order to achieve this level of behavior change, we need policy-makers, behavioral science experts, and public communication professionals to work together. Unfortunately, in the crisis of the pandemic, even public communication was handled by medical experts instead of behavioral science professionals. The goal of long-term SBC preparedness is to achieve sustainable change of key COVID-19 preventive behaviors. Behaviors are adopted with a short-term time frame, not as permanent change. The adoption of COVID-19 behaviors ebbs and flows with the pandemic.
As more behavioral data becomes available, looking at deeper audience segments will be essential. For example, pregnant women in Ethiopia reported only 6% mask use. Vulnerable groups need to be defined, identified, and reached since we know that COVID-19 has impacted them adversely. Similarly, campaigns should aim to reach out to people with comorbidities and chronic diseases.
Evidence from the literature review indicates that there was message fatigue during the COVID-19 pandemic. We recommend short- and long-term public communication and community engagement planning to address this issue. Tools like a rapid literature review can identify the barriers to COVID-19 behaviors. For example, discomfort in mask use and lack of social norms around preventive behaviors and other barriers can be incorporated into campaigns to address immediate contextual issues. Creative planning will be necessary to address message fatigue and maintain a campaign environment that builds confidence and trust.
The following are guidelines for SBC preparedness for sustainable behavior change in COVID-19 behaviors:
-
(a)
SBC preparedness includes short-term and long-term behavior change strategic plans.
-
(b)
Information that identifies barriers to COVID-19 prevention behaviors should be gathered from peer-reviewed papers and used in campaigns.
-
(c)
Public communication campaigns should be designed to soothe and calm people rather than scare them with fear related content.
-
(d)
Determinants of behaviors should be mapped prior to campaign design.
-
(e)
Digital approaches that use innovations such as the digital relay need to be prioritized for amplifying program reach.
-
(f)
A separate strategy for social media is required.
-
(g)
Message fatigue needs to be combated with creative, engaging, and innovative campaigns.
The Magnitude of the Mental Health Burden in COVID-19 Times
The global mental health burden triggered by the COVID-19 pandemic is staggering [56]. Ethiopia is no exception to the global trend. In this chapter, we discuss the high degree of mental distress experienced by Ethiopians during the COVID-19 pandemic. The Breakthrough Action Ethiopia report on psychological and economic distress showed that almost half (49%) of the respondents reported feeling distressed and about 44% felt nervous [57]. This parallel stress can be mitigated by providing adequate mental health support and services. The biggest challenge for mental health services is the provider gap in most countries [58]. Volunteers and grassroots champions can be trained for mental health support [59]. We suggest that community-based mental support services be integrated into the five pillars of risk communication. Integrating mental health with community engagement activities will result in promoting wellbeing and calmness.
Another learning from the mental health peer-reviewed literature was that almost every segment of the population was negatively impacted by the COVID-19 pandemic. The most affected were healthcare workers who are most susceptible to the COVID-19 infection. Consistent mental health screening of these workers is essential and those detected with symptoms must be referred for care. There is evidence to indicate that women are significantly more likely to have symptoms of depression compared to men. Developing a mental health support plan for different population segments such as older adults, women, young people, healthcare workers, and prisoners will lead to better COVID-19 prevention outcomes.
The following are guidelines for SBC preparedness for improving mental health during the COVID-19 pandemic:
-
(a)
Community-based mental health support should be integrated into risk communication and SBC preparedness approaches.
-
(b)
Public communication campaigns should encourage people to talk with others in case they are experiencing symptoms of depression or anxiety.
-
(c)
Simple mental health support videos should be developed to train volunteers. Existing resources on community-based mental health support can also be used or adapted to local situations.
-
(d)
Counseling preparedness implies that all COVID-19 counselors and volunteers are trained.
-
(e)
Public communication campaigns should promote calmness within households and communities to cope better with pandemic stress.
In conclusion, the chapter focuses on three crucial elements of SBC preparedness within the realm of risk communication. The first section of the chapter describes how to implement a systematic first response to a new epidemic or outbreak. The WHO/GOARN framework provides a comprehensive structure to operationalize the immediate national-level response for SBC. Ethiopia’s first response was well coordinated and planned, and importantly was started before the detection of the first COVID-19 case in the country. The second section of the chapter provides pooled estimates of COVID-19 prevention behaviors in the country which show a pattern of uneven adoption. The need to develop strategic SBC approaches for both behavior change and behavior maintenance is highlighted. Finally, the third section of the chapter deals with the mental health context during the pandemic in Ethiopia. We propose an integration of community-based mental health support with SBC preparedness activities.
The guidelines for practice provided in this chapter are globally applicable, and we hope that Ethiopia’s collective experience results in a better understanding of SBC preparedness in the global fight against COVID-19.
References
The World Bank. Ethiopia population (2020). [https://www.worldbank.org/en/country/ethiopia/overview].
World Health Organization. WHO coronavirus disease (COVID-19) dashboard with vaccination data. World Health Organization.[https://covid19.who.int]
Okonji EF, Okonji OC, Mukumbang FC , Van Wyk B (2021) Understanding varying COVID‐19 mortality rates reported in Africa compared to Europe, Americas, and Asia. Trop Med Int Health 26(7):716–719. https://onlinelibrary.wiley.com/share/VHYD2BFZHHCPWJKNP8WF?target=10.1111/tmi.13575
Resolve to Save Lives & Prevent Epidemics. Country Preparedness and Covid-19. https://preventepidemics.org/covid19/science/insights/country-preparedness-and-covid-19/May
World Health Organization (2022) International Health Regulations (2005) 3rd edn. World Health Organization. 2022. https://www.who.int/publications-detail-redirect/9789241580496]
World Health Organization. Joint external evaluation tool: International Health Regulations (2005). World Health Organization. 2016. [https://www.who.int/publications-detail-redirect/9789240051980]
Tolu LB, Ezeh A , Feyissa GT (2020) How prepared is Africa for the COVID-19 pandemic response? The case of Ethiopia. Risk Manag Healthc Policy 13:771–776. https://www.dovepress.com/how-prepared-is-africa-for-the-covid-19-pandemic-response-the-case-of--peer-reviewed-fulltext-article-RMHP]
Health Communication Capacity Collaborative and United States Agency for International Development. Emergency communication preparedness implementation kit – social and behavior change communication for emergency preparedness implementation kit. Health Communication Capacity Collaborative & United States Agency for International Development. https://healthcommcapacity.org/hc3resources/social-behavior-change-communication-emergency-preparedness-implementation-kit/]
John Hopkins Center for Communication Programs. Breakthrough ACTION Liberia: The Compass for SBC. Compass. https://www.usaid.gov/sites/default/files/documents/Health_Sector_Project_Fact_Sheet_Breakthrough_ACTION.pdf]
Rice R, Atkin CK (2012) Public communication campaigns, 4th edn, Thousand Oaks [CA]. Sage Publications. https://sk.sagepub.com/books/public-communication-campaigns-fourth-edition/i138.xml]
Lanyero B, Edea ZA, Musa EO, Watare SH, Mandalia ML, Livinus MC, Ebrahim FK, Girmay A, Bategereza AK, Abayneh A, Sambo BH, Abate E (2021) Readiness and early response to COVID-19: Achievements, challenges, and lessons learnt in Ethiopia. BMJ Global Health 6(6):e005581.[https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/fr/covidwho-1266382]
Mohammed H, Oljira L, Roba KT, Yimer G, Fekadu A , Manyazewal T (2020) Containment of COVID-19 in Ethiopia and implications for tuberculosis care and research. Inf Dis Pov 9(1):131. https://pubmed.ncbi.nlm.nih.gov/32938497/]
Fana Broadcasting Corporate S.C. (2020) Ethiopia begins screening for Coronavirus at Bole Int’l Airport. Fana Broadcasting Corporate S.C. https://www.fanabc.com/english/ethiopia-begins-screening-for-coronavirus-at-bole-intl-airport/]
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Br Med J 327(7414):557–560. https://www.bmj.com/content/327/7414/557.long
Abeya SG, Barkesa SB, Sadi CG, Gemeda DD, Muleta FY, Tolera AF, Ayana DN, Seada AM, Wako EB, Hurisa MB, Bayisa DA, Sarbesa MK, Yesuf EY, Tufa AA (2021) Adherence to COVID-19 preventive measures and associated factors in Oromia regional state of Ethiopia Wang J (ed.). Public Libr Sci ONE 16(10): e0257373. https://europepmc.org/article/med/34669723
Aemro A, Amare NS, Shetie B, Chekol B, Wassie M (2021) Determinants of COVID-19 vaccine hesitancy among health care workers in Amhara region referral hospitals, Northwest Ethiopia: A cross-sectional study. Epidemiol & Infect 149: e225. https://pubmed.ncbi.nlm.nih.gov/34645533/
Asemahagn MA (2020) Factors determining the knowledge and prevention practice of healthcare workers towards COVID-19 in Amhara region, Ethiopia: A cross-sectional survey. Trop Med Health 48(1):72. https://tropmedhealth.biomedcentral.com/articles/10.1186/s41182-020-00254-3
Azene ZN, Merid MW, Muluneh AG, Geberu DM, Kassa GM, Yenit MK, Tilahun SY, Gelaye KA, Mekonnen HS, Azagew AW, Wubneh CA, Belay GM, Asmamaw NT et al. (2020) Adherence towards COVID-19 mitigation measures and its associated factors among Gondar City residents: A community-based cross-sectional study in Northwest Ethiopia. Di Gennaro F (ed.). Public Libr Sci ONE 15(12): e0244265. https://journals.plos.org/plosone/article?id=https://doi.org/10.1371/journal.pone.0256954
Belete ZW, Berihun G, Keleb A, Ademas A, Berhanu L, Abebe M, Gizeyatu A, Hassen S, Teshome D, Lingerew M, Feleke A, Natnael T, Adane M (2021) Knowledge, attitude, and preventive practices towards COVID-19 and associated factors among adult hospital visitors in South Gondar Zone Hospitals, Northwest Ethiopia. Di Gennaro F (ed.). Public Libr Sci ONE 16(5): e0250145. [https://europepmc.org/article/pmc/pmc8128268]
Defar A, Molla G, Abdella S, Tessema M, Ahmed M, Tadele A, Getachew F, Hailegiorgis B, Tigabu E, Ababor S, Bizuwork K, Deressa A, Tasaw G, Kebede A, Melese D, Gashu A, Eshetu K, Tayachew A, Wossen M, Hassen A, Habebe S, Assefa Z, Abayneh A, Abate E, Tollera G (2021) Knowledge, practice, and associated factors towards the prevention of COVID-19 among high-risk groups: A cross-sectional study in Addis Ababa, Ethiopia. Tu WJ (ed.) Public Libr Sci ONE 16(3): e0248420. https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/covidwho-1127799
Deressa W, Worku A, Abebe W, Getachew S, Amogne W (2021) Social distancing and preventive practices of government employees in response to COVID-19 in Ethiopia. Hasnain SE (ed.). Public Libr Sci ONE 16(9): e0257112. https://journals.plos.org/plosone/article?id=https://doi.org/10.1371/journal.pone.0257112
Desalegn Z, Deyessa N, Teka B, Shiferaw W, Yohannes M, Hailemariam D, Addissie A, Abagero A, Kaba M, Abebe W, Abrha A, Nega B, Ayele W, Haile T, Gebrehiwot Y, Amogne W, Kantekhardt EJ, Abebe T (2021) Evaluation of COVID-19 related knowledge and preparedness in health professionals at selected health facilities in a resource-limited setting in Addis Ababa, Ethiopia. Thet Wai K (ed.). Public Libr Sci ONE 16(2): e0244050. https://europepmc.org/article/pmc/pmc7875347
Feleke BT, Wale MZ, Yirsaw MT (2021) Knowledge, attitude, and preventive practice towards COVID-19 and associated factors among outpatient service visitors at Debre Markos compressive specialized hospital, north-west Ethiopia, 2020. Mitra P (ed.). Public Libr Sci ONE 16(7): e0251708. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0251708
Hailemariam D, Kumie A, Wakuma S, Tefera Y, Abegaz T, Tefera W, Ayele W, tamire M, Yirsaw S (2021) Trends in non-pharmaceutical intervention (NPI) related community practice for the prevention of COVID-19 in Addis Ababa, Ethiopia. Conly J (ed.). Public Libr Sci ONE 16(11): e0259229. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0259229
Hassen S, Adane M (2021) Facemask-wearing behavior to prevent COVID-19 and associated factors among public and private bank workers in Ethiopia. Wang Z (ed.). Public Libr Sci ONE 16(12): e0259659. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8635365
Kaso AW, Hareru HE, Agero G, Ashuro Z (2021) Assessment of practice of COVID-19 preventive measures and associated factors among residents in Southern, Ethiopia. Wang Z, (ed.). Public Libr Sci ONE. 16(12): e0261186. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0261186
Yoseph A, Tamiso A, Ejeso A (2021) Knowledge, attitudes, and practices related to COVID-19 pandemic among adult population in Sidama Regional State, Southern Ethiopia: A community based cross-sectional study. Erbil N (ed.). Public Libr Sci ONE 16(1): e0246283. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0246283
Zewude B, Melese B, Habtegiorgis T, Tadele M, Solomon W (2021) Compliance with protective behavioral recommendations in the outbreak of COVID-19 Among people working in the urban-based informal economy in Southern Ethiopia. Front Public Health 9:716814. https://www.frontiersin.org/articles/10.3389/fpubh.2021.716814/full
Desalegn Z, Deyessa N, Teka B, Shiferaw W, Hailemariam D, Addissie A, Abagero A, Kaba M, Abebe W, Nega B, Ayele W, Haile T, Gebrehiwot Y, Abebe T et al. (2021) COVID-19 and the public response: Knowledge, attitude, and practice of the public in mitigating the pandemic in Addis Ababa, Ethiopia. Thet Wai K (ed.). Public Libr Sci ONE 16(1): e0244780. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0244780
Dessu S, Tsehay T, Girum T, Timerga A, Solomon M, Tsegaye B, Geremew M, Migora B, Mesfin Y, Kemal A, Alebel A, Tolosa O, Tesfa S, Yasin F (2021) The applicability of basic preventive measures of the pandemic COVID-19 and associated factors among residents in Guraghe Zone. Kabir E (ed.). Public Libr Sci ONE 16(8): e0256598. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0256598
Akalu TY, Gelaye KA, Bishaw MA, Tilahun SY, Yeshaw Y, Azale T, Tsegaye T, Asmelash D, Akalu Y (2021) Depression, anxiety, and stress symptoms and its associated factors among residents of Gondar Town during the early stage of COVID-19 pandemic. Risk Manag Healthc Policy 14:1073–1083. https://www.dovepress.com/depression-anxiety-and-stress-symptoms-and-its-associated-factors-amon-peer-reviewed-fulltext-article-RMHP
Asnakew S, Amha H, Kassew T (2021) Mental health adverse effects of COVID-19 pandemic on health care workers in North West Ethiopia: A multicenter cross-sectional study. Neuropsychiatr Dis Treat 17:1375–1384. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8113010/
Assefa ZM, Haile TG, Wazema DH, Tafese WT, Berrie FW, Beketie ED, Hailemariam BZ, Zewudie BT, Teke NE, Metebo KN (2021) Mental health disorders during COVID-19 pandemic among Southwest Ethiopia University students: An institutional-based cross-sectional study. SAGE Open Nurs 7:237796082110643. https://journals.sagepub.com/doi/full/https://doi.org/10.1177/23779608211064374
Ayalew M, Deribe B, Abraham Y, Reta Y, Tadesse F, Defar S, Hoyiso D, Ashegu T (2021) Prevalence and determinant factors of mental health problems among healthcare professionals during COVID-19 pandemic in southern Ethiopia: Multicentre cross-sectional study. Br Med J Open 11(12): e057708. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8718344/
GebreEyesus FA, Tarekegn TT, Amlak BT, Shiferaw BZ, Emeria MS, Geleta OT, Terefe TF, Tadareregew MM, Jimma MS, Degu FS, Abdisa EN, Eshetu MA, Misganaw NM & Chanie ES. Levels and predictors of anxiety, depression, and stress during COVID-19 pandemic among frontline healthcare providers in Gurage zonal public hospitals, Southwest Ethiopia, 2020: A multicenter cross-sectional study. Kasuga K, editor. Public Libr Sci ONE 16(11): e0259906. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0259906
Habtamu Y, Admasu K, Tullu M, Damene W, Birhanu A, Beyero T, Tereda AB (2021) Mental health outcomes among frontline health-care workers at Eka Kotebe National COVID-19 Treatment Center, Addis Ababa, Ethiopia, 2020: A cross-sectional study. Neuropsychiatr Dis Treat 17: 2831–2840. https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/covidwho-1833990
Hagezom HM, Gebrehiwet AB, Haftom Goytom M, Alemseged EA (2020) Prevalence of depression and associated factors among quarantined individuals during the COVID-19 pandemic in Tigrai Treatment and Quarantine Centers, Tigrai, Ethiopia, 2020: A Cross-Sectional Study. Infect Drug Resist 14:2113–2119. https://www.dovepress.com/prevalence-of-depression-and-associated-factors-among-quarantined-indi-peer-reviewed-fulltext-article-IDR
Hajure M, Tariku M, Mohammedhussein M, Dule A (2020) Depression, anxiety and associated factors among chronic medical patients amid COVID-19 pandemic in Mettu Karl Referral Hospital, Mettu, Ethiopia, 2020. Neuropsychiatr Dis Treat 16:2511–2518. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7605548
Jemal K, Deriba BS, Geleta TA (2021) Psychological distress, early behavioral response, and perception toward the COVID-19 pandemic among health care workers in North Shoa Zone, Oromiya Region. Front Psychiatry 12:628898. https://www.frontiersin.org/articles/10.3389/fpsyt.2021.628898/full
Necho M, Birkie M, Gelaye H, Beyene A, Belete A, Tsehay M (2020) Depression, anxiety symptoms, Insomnia, and coping during the COVID-19 pandemic period among individuals living with disabilities in Ethiopia, 2020. Na KS (ed.). Public Libr Sci ONE 15(12): e0244530. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0244530
Simegn W, Dagnew B, Yeshaw Y, Yitayih S, Woldegerima B, Dagne H (2021) Depression, anxiety, stress and their associated factors among Ethiopian University students during an early stage of COVID-19 pandemic: An online-based cross-sectional survey. Spradley FT (ed.). Public Libr Sci ONE 16(5): e0251670. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0251670
Tsehay M, Necho M, Gelaye H, Beyene A, Birkie M (2021) Generalized anxiety disorder, depressive symptoms, and sleep problem during COVID-19 outbreak in Ethiopia Among police officers: A cross-sectional survey. Front Psychol 12:713954. https://www.frontiersin.org/articles/10.3389/fpsyg.2021.713954/full
Wayessa ZJ, Melesse GT, Amaje Hadona E, Wako WG (2021) Prevalence of depressive symptoms due to COVID-19 and associated factors among healthcare workers in Southern Ethiopia. SAGE Open Med 9:205031212110328. https://journals.sagepub.com/doi/abs/10.1177/20503121211032810
Chekole YA, Yimer Minaye S, Mekonnen Abate S, Mekuriaw B (2020) Perceived stress and its associated factors during COVID-19 among healthcare providers in Ethiopia: A cross-sectional study. Adv Public Health 2020:1–7. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0252809
Girma A, Ayalew E, Mesafint G (2021) Covid-19 pandemic-related stress and coping strategies among adults with chronic disease in Southwest Ethiopia. Neuropsychiatr Dis Treat 17:1551–61. https://www.dovepress.com/covid-19-pandemic-related-stress-and-coping-strategies-among-adults-wi-peer-reviewed-fulltext-article-NDT
Yitayih Y, Mekonen S, Zeynudin A, Mengistie E, Ambelu A (2021) Mental health of healthcare professionals during the early stage of the COVID-19 pandemic in Ethiopia. Br J Psychiatry Open 7(1): e1. https://www.cambridge.org/core/journals/bjpsych-open/article/mental-health-of-healthcare-professionals-during-the-early-stage-of-the-covid19-pandemic-in-ethiopia/DBEFE0E42C7443350E30F3B6DCFA9783
Berihun G, Walle Z, Berhanu L, Teshome D (2021) Acceptance of COVID-19 vaccine and determinant factors among patients with chronic disease visiting Dessie Comprehensive Specialized Hospital, Northeastern Ethiopia. Patient Prefer Adherence 15:1795–1805. https://www.dovepress.com/acceptance-of-covid-19-vaccine-and-determinant-factors-among-patients--peer-reviewed-fulltext-article-PPA
Dagne H, Atnafu A, Alemu K, Azale T, Yitayih S, Dagnew B, Alemayehu AM, Andualem Z, Sisay MM, Tadesse D, Chekol SH, Mamo EM, Simegn W (2021) Anxiety and associated factors among Ethiopian health professionals at early stage of COVID-19 pandemic in Ethiopia. Spradley FT (ed.). Public Libr Sci ONE 16(6): e0252664. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0252664
Kibret S, Teshome D, Fenta E, Hunie M, Tamire T (2020) Prevalence of anxiety towards COVID-19 and its associated factors among healthcare workers in a Hospital of Ethiopia. Tu WJ (ed.). Public Libr Sci ONE 15(12): e0243022. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0243022
Tesema AK, Shitu K, Adugna A, Handebo S (2021) Psychological impact of COVID-19 and contributing factors of students’ preventive behavior based on HBM in Gondar, Ethiopia. Pakpour AH (ed.). Public Libr Sci ONE 16(10): e0258642. https://journals.plos.org/plosone/article?id=https://doi.org/10.1371/journal.pone.0258642
Jemal K, Deriba BS, Geleta TA, Tesema M, Awol M, Mengistu E, Annous Y (2021) Self-reported symptoms of depression, anxiety, and stress among healthcare workers in ethiopia during the COVID-19 pandemic: A cross-sectional study. Neuropsychiatr Dis Treat 17:1363–1373. https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/covidwho-1229112
Shields-Zeeman L, Pathare S, Walters BH, Kapadia-Kundu N, Joag K (2017) Promoting wellbeing and improving access to mental health care through community champions in rural India: The Atmiyata intervention approach. Int J Ment Health Syst 11(1):6. https://psycnet.apa.org/record/2017-00357-001
Alula M (2022) Formative assessment for USAID’s integrated youth activity in Ethiopia. Unpublished report. Ethiopia: AMREF Ethiopia. Report No.: V1. https://pdf.usaid.gov/pdf_docs/PA00X5D8.pdf
Kapadia Kundu N (2019) The digital relay. Unpublished paper
Gardner B (2015) A review and analysis of the use of ‘habit’ in understanding, predicting and influencing health-related behavior. Health Psychol Rev 9(3):277–295. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4566897/
Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. (2021) Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet 398(10312):1700–1712. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)02143-7/fulltext
Rosen E (2022) Global-level depression, nervousness and worry about food and financial security amidst the COVID-19 pandemic in 113 countries. Johns Hopkins center communication programs. https://covidbehaviors.org/dep_nerv_worry_technical_brief.pdf
Kohn R, Saxena S, Levav I, Saraceno B (2004) The treatment gap in mental health care. Bull World Health Organ 82(11):858–866. https://apps.who.int/iris/handle/10665/269274
Joag K, Shields-Zeeman L, Kapadia-Kundu N, Kawade R, Balaji M, Pathare S (2020) Feasibility and acceptability of a novel community-based mental health intervention delivered by community volunteers in Maharashtra, India: The Atmiyata programme. BMC Psychiatry 20(1):48. https://www.researchgate.net/publication/339092843_Feasibility_and_acceptability_of_a_novel_community-based_mental_health_intervention_delivered_by_community_volunteers_in_Maharashtra_India_the_Atmiyata_programme
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Kapadia-Kundu, N. et al. (2023). Social and Behavior Change Preparedness for COVID-19 Prevention: Evidence and Experience from Ethiopia. In: Pachauri, S., Pachauri, A. (eds) Global Perspectives of COVID-19 Pandemic on Health, Education, and Role of Media. Springer, Singapore. https://doi.org/10.1007/978-981-99-1106-6_21
Download citation
DOI: https://doi.org/10.1007/978-981-99-1106-6_21
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-1105-9
Online ISBN: 978-981-99-1106-6
eBook Packages: Social SciencesSocial Sciences (R0)