Abstract
Human rights discourse related to sexuality has increased dramatically since the mid-1990s. The 1994 International Conference on Population and Development (ICPD) in Cairo, followed by the Fourth World Conference on Women (FWCW) held in Beijing in 1995 were arguably major steps forward in terms of women’s rights and the rights of all regardless of age, sex and gender, health-related conditions, and Sexual Orientation, Gender Identity and Expression and Sex Characteristics (SOGIESC). FGM/C receives significant attention at a global level, and the eradication campaigns graphically highlight the serious negative impact this has on girls and women as a global human rights and reproductive health issue. At the same time, medically unnecessary male genital cutting without informed consent has been relatively unchallenged if ever discussed by major bodies advocating for sexual and reproductive health and rights (SRHR) as human rights.
As with the push against sex-normalizing medical procedures employed on intersex infants and children, there are strong, reasoned arguments against medically unnecessary genital cutting without free, full and informed consent that applies to all, regardless of gender and sex characteristics. The ripples of movements of advocacy including “intactivism” and respect for bodily/sexual boundaries and privacy are slowly but surely progressing. Despite all the complexities and challenges, double standards in the promotion of SRHR must be addressed. “Leave no one behind” is the central promise of the Sustainable Development Goals (SDGs) and asserts the rights of all infants and young children to grow to an age where they can make their own informed decisions about their bodies.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
11.1 Introduction
In 2019, the 3rd International Experts Meeting on female genital mutilation/cutting (FGM/C) was held in Brussels, Belgium, and was attended by interdisciplinary experts from all five regions of the world. Concerns about widespread inaccuracies, inconsistencies, double standards, and Western cultural bias in the prevailing discourses on the genital cutting of children were shared and discussed. Unlike FGM/C and other forms of genital cutting of children (e.g., genital “normalizing” surgery of intersex children), male genital cutting, namely male circumcision, has been relatively unchallenged and rarely (if ever) discussed by major bodies advocating for human rights. This chapter is inspired by a call for a more coherent sex- and gender-inclusive approach to the debate on genital cutting, that recognizes the special vulnerability of children and young people, regardless of the race, religion, or immigration status of their parents, to medically unnecessary genital cutting; and the moral importance of bodily integrity, respect for bodily/sexual boundaries, and a free, full, and informed consent (The Brussels Collaboration on Bodily Integrity 2019: 24). No one, certainly no child, including infant males and young boys, should be left behind.
11.2 From Reproductive Health to Sexual Rights
The human rights discourse related to sexuality has increased dramatically since the mid-1990s. The 1994 International Conference on Population and Development (ICPD) in Cairo, the largest intergovernmental conference on population and development ever held at that time, was a historic turning point. According to Correa and Howe (2007), it was the first time the term “sexual rights” appeared in negotiations among representatives of the governments participating in the conference. The conference covered numerous controversial issues, but the outcome document, the Cairo Programme of Action (United Nations 1994), failed to include the term “sexual rights” or any references to homosexuality in the final text. Nevertheless, the fact that the concept was explored was a significant milestone and led to the understanding that Chap. 7 (“Reproductive Rights and Health”) pertains to more than just reproductive health rights.
The following year, the Fourth World Conference on Women (FWCW) was held in Beijing, where the term sexual rights was explored again. The concept was elaborated and reflected upon in the outcome document (United Nations 1995) as:
The human rights of women include their right to have control over and decide freely and responsibly on matters related to their sexuality, including sexual and reproductive health, free of coercion, discrimination and violence. Equal relationships between women and men in matters of sexual relations and reproduction, including full respect for the integrity of the person, require mutual respect, consent and shared responsibility for sexual behaviour and its consequences.
These two conferences were arguably major steps forward in terms of women’s rights, and indeed the rights of all regardless of age, sex and gender, health-related conditions, and sexual orientation, gender identity and expression and sex characteristics (SOGIESC). The chronological advancement of rights, with acknowledgement of its oversimplification, was laid out by Lottes (2013), who modified the original timeline of progression presented by Ruth Dixon Muller: Human Rights → Women’s Rights → Reproductive Rights → Women’s Sexual Rights → Sexual Rights for All.
Various lists of sexual rights have been issued by experts and international organizations (see HERA 1998; IPPF 2008; Kirkendall 1976; WAS 1999, 2014; WGNRR 1996; WHO 2006), with a significant overlap in content. A revised version of the Declaration of Sexual Rights issued by the World Association for Sexual Health (WAS), formerly known as the World Association for Sexology, provides the most comprehensive list of sexual rights in terms of age, gender, and SOGIESC. It has been revised for clear alignment with human rights and supports numerous human rights treaties and consensus statements (WAS 2014; see appendix).
The focus of this chapter is the child’s right to autonomy and bodily integrity, which is a critical component of sexual rights. Autonomy is characterized as the ability to make informed decisions (self-determination) and be treated as the principal actor and decision-maker in matters regarding one’s own sexuality and reproduction (personhood). A frequently cited definition of bodily integrity, by Martha Nussbaum, is as follows: “being able to move freely from place to place; being able to be secure against violent assault, including sexual assault; having opportunities for sexual satisfaction and for choice in matters of reproduction” (Nussbaum 2007: 23). WAS (2014) emphasized the right to autonomy and bodily integrity in relation to sexuality thusly:
Everyone has the right to control and decide freely on matters related to their sexuality and their body. This includes the choice of sexual behaviors, practices, partners, and relationships with due regard to the rights of others. Free and informed decision making requires free and informed consent prior to any sexually-related testing, interventions, therapies, surgeries, or research.
An example of the violation of this right is forced, coercive, or otherwise involuntary sterilization. In 2014, the World Health Organization (WHO) and other UN agencies, such as the Office of the High Commissioner for Human Rights (OHCHR), UN Women, Joint United Nations Programme on HIV/AIDS (UNAIDS), United Nations Development Programme (UNDP), United Nations Population Fund (UNFPA), and United Nations Children's Fund (UNICEF) issued an interagency statement calling for the elimination of forced, coercive, or otherwise involuntary sterilization (WHO 2014). This document recognized the disproportionate use of sterilization and other forms of deconversion among certain populations, including persons living with HIV, persons with disabilities, indigenous peoples and ethnic minorities, and trans and gender diverse (TGD) and intersex persons. It clearly stated that any form of involuntary, coercive or forced sterilization violates ethical principles, including respect for autonomy and bodily integrity, beneficence, and non-maleficence. The statement strongly condemns violations of those human rights guaranteed by various national and international instruments, including the right to privacy, reproductive rights, and the right to be free from discrimination, torture and cruel, inhumane, or degrading treatment or punishment. This document is a critical reminder of the famous slogan “My Body, My Choice” according to which no-one, including parents and spouses, leaders of communities and clans, professionals, or the state, has the right to decide what an individual does with their own body.
In addition to sterilization, body (genital) modification has been used as a medical intervention for TGD people and intersex infantsFootnote 1 in many countries. According to Japan’s Act on Special Cases in Handling Gender for People with Gender Identity Disorder (Law No. 111 of 2003; Effective Jul. 16, 2004), as of April 2022, a person who wishes to change their gender on Koseki, the official family registry, must fulfill the following conditions: diagnosed with gender identity disorder by two independent medical professionals; aged 20 years or older; not currently married; not the parent of a minor; does not have gonads/functioning gonads; and endowed with genitalia that closely resemble those of another gender. Even if a TGD person desires to undergo gender affirmation surgery, these prerequisites undermine their ability to give free, full, and informed consent.Footnote 2
With regard to intersex persons, sex-normalizing procedures, among others, have been performed on the genitalia and/or reproductive organs of infants and children with little consideration of their views and rights. The aim of such medical interventions is to “correct” perceived ambiguities, including by making the genital phenotype appear more stereotypically male or female (Beh and Diamond 2000; GIRES 2006). This has been the standard protocol since the 1960s, when gender identity clinics were first established in the United States (US), since then it has been widely accepted in other countries where surgical interventions are available (Colapinto 2000; Kessler 1998). The underlying rationale is that the body must strictly conform to one gender; thus, atypical sex characteristics (external genitalia in this case) are viewed as both a medical problem and psychosocial emergency that impede the healthy development of the child; therefore, according to this view, there is a need for correction through surgical, hormonal, or other medical treatments, and sometimes via psychological means, as that is in the best interests of the child. It should be emphasized that it should be acceptable for any individual, regardless of their intersex status, to decide themselves to undergo such medical interventions if it is based on free and informed decision-making; in any other circumstance, the principle of “respect for autonomy and bodily integrity, self-determination, and human dignity” (WHO 2014: 7)is violated. Thus, if a person is too young to give free, full, and informed consent, it is unethical to expect or demand any type of irreversible intervention be considered or conducted.
11.3 Medically Unnecessary Genital Cutting
11.3.1 Terminology
Communication theory tells us that language has the power to manifest change. Referring to medical interventions for intersex infants and children as “so-called sex-normalizing or other procedures” (WHO 2014: 7), together with the use of similar language in global human rights campaigns on diverse SOGIESC (e.g., UN Free and Equal campaign), shows that efforts have been made to de-medicalize diverse sex characteristics and highlights that such irreversible early interventions are harmful (Human Rights Watch 2017; OHCHR 2019; UN 2016; WHO 2014).Footnote 3
This chapter uses the term “genital cutting” regardless of gender, sex, and cultural, religious, and health-related factors, to acknowledge that terms are inherently culturally bound and evolve over time. The author recognizes the dilemma shared by researchers and human rights advocates regarding which terms to use to avoid the stigmatization of certain practices, especially those that are culturally and religiously motivated (see Chap. 6). The significance of the use of the term “genital cutting” in this chapter is related to the political justification and context underlying the replacement of “female circumcision” with “FGM”.
The WHO, along with other major bodies behind anti-FGM campaigns, explained that replacement of the term “female circumcision” was done to establish “a clear linguistic distinction from male circumcision and emphasize the gravity and harm of the act. Use of the word ‘mutilation’ reinforces the fact that the practice is a violation of girls’ and women’s rights” (WHO 2008: 22). Thus, some even consider the use of the term “female genital cutting” (FGC) for girls and women to be problematic, because “[This term] draws a parallel with male circumcision and, as a result, creates confusion between these two distinct practices” (WHO 2008: 22). Although they never clearly state that male genital cutting, i.e., male circumcision, is not harmful, the inference is that it can be viewed as considerably less invasive and debilitating, and the negative psychological and emotional consequences are thus ignored. This is partly designed to mitigate conflict with Judaism and Islam (Iguchi and Rashid 2019).
Positive values are promoted in relation to the act of male circumcision, whether it is performed in a ceremonial, cultural, or religious context, or even in a health-related (propylic) context, but this obfuscates the issue of un-consenting, non-therapeutic surgical interventions for male infants and young boys. Thus, ethical issues surrounding male genital cutting remain unchallenged and undiscussed at the global scale, where permanent removal of the foreskin is viewed as less harmful than a needle prick to the clitoral hood, as performed in Malaysia, Indonesia, and some other countries (see Taher 2017; Iguchi and Rashid 2019) which falls under the definition of FGM. The term genital cutting is thus used in this chapter to draw attention to the double standards and inaccuracies in global human rights discourse regarding these practices.
11.3.2 Circumcision
Circumcision may predate recorded human history (Cox and Morris 2012; El-Gohary 2015). Although there is little proof beyond anecdotal evidence, it is believed that circumcision as a rite of passage during puberty was practiced as long ago as 1000 B.C. Herodotus’ The Histories cites the Egyptians as the earliest people to practice circumcision, and ancient Egyptian reliefs representing rites of passage have been uncovered, along with the mummies of circumcised youth and adults (Waszak 1978; Morimoto 1989; Dunsmuir and Gordon 1999; WHO and UNAIDS 2007).
The term “circumcision” is derived from the Latin words circum (meaning “around”) and caedere (meaning “to cut”), which refers to the partial or total removal of the sleeve of skin and mucosal tissue that covers the glans of the penis, known as the foreskin. Genital cutting and modification have been performed for faith-based, perceived health-related, sociocultural, and cosmetic reasons, along with other perceived personal benefits. Sara Johnsdotter, a medical anthropologist from Sweden, notes that the “rationales for the circumcision of boys and girls vary with local context, but genital modifications are often performed with similar motives irrespective of gender” (Johnsdotter 2018: 22). It has been suggested that in many societies “female circumcision” was introduced in imitation of the male rite, i.e., female circumcision may be practiced within a culture or clan where male circumcision is practiced, but not in one where it is not (Cohen 1997: 562).
11.3.3 Genital Cutting for “Health Benefits”
With advances in surgery, male genital cutting was introduced into some previously non-circumcising cultures for both health-related and social reasons; male genital cutting became increasingly popular in English-speaking industrialized countries toward the end of the nineteenth century (Dunsmuir and Gordon 1999). The perceived health benefits at that time included prevention of a range of “unwanted” conditions and “undesirable” behaviors, including masturbation, syphilis, nocturnal incontinence, and the enhancement of sexual pleasure. Male genital cutting also became widely practiced in North America, New Zealand, and Europe due to these perceived benefits (WHO and UNAIDS 2007).
Male genital cutting is one of the most common surgical procedures conducted today. As of 2007, the WHO estimates that approximately 30% of boys and men aged 15 years and older worldwide have been circumcised. Around two thirds (69%) are Muslim (mainly living in Asia, the Middle East and North Africa), 0.8% are Jewish, and 13% are non-Muslim and non-Jewish men living in the US (WHO and UNAIDS 2007: 7). A more recent study based on data from 237 countries estimates that the global prevalence of circumcision ranges from 37 to 39%, with approximately half of all procedures being performed for religious and cultural reasons (Morris et al. 2016).
Although male genital cutting gained in popularity in English-speaking countries and Europe during the mid-1800s, the US is the only country where infant male genital cutting, namely neonatal male circumcision (NMC), has been routinely practiced to date. The prevalence rose to about 80% in the 1960s and remains high, at 76–92%, compared to Central and South America (<20%) (Nelson et al. 2005). The American Academy of Pediatrics (AAP) did stop endorsing routine NMC in 1971, but that had little impact on the popularity of the practice. This high prevalence of NMC explains why an estimated 13% of circumcised males in the world are non-Muslim and non-Jewish men living in the US.
It should be noted that the AAP has never banned NMC, but have rather supported the parents’ decision based on the advantages and disadvantages of NMC indicated by “scientific evidence.” The 2012 Technical Report on male circumcision concluded that the health benefits of newborn male circumcision outweigh the risks according to current evidence (AAP 2012).
Interestingly, the high prevalence of male circumcision in the US has greatly influenced South Korea, which is the only country with an exceptionally high prevalence of circumcision in East Asia despite body modification being rare due to the strong Confucian and Buddhist tradition.Footnote 4 One community-based survey found that the prevalence was more than 90% in some age groups (Pang and Kim 2002), while another community-based survey found that 78.0% of randomly sampled men aged 20 years were circumcised, predominantly during their elementary school years, while 11.5% wished to be circumcised later. This high prevalence was believed to be associated with their close relationship and direct contact with the US military, particularly throughout the Korean War (Kim et al. 2012; Ku et al. 2003).
In addition to previously advertised health benefits (e.g., penile hygiene and the prevention of cancers and infections) male circumcision has been touted as “a highly cost-effective intervention for preventing HIV acquisition,” especially in African countries where HIV infection through heterosexual vaginal intercourse is prevalent (WHO and UNAIDS 2016: 2). A contemporary voluntary medical male circumcision (VMMC) campaign has reached new territories through its promotion in sub-Saharan Africa, where it is called “VMMC2021”; the goal is to achieve a 90% circumcision rate among males aged 10–29 years by 2021. The VMMC campaign is also referenced in the widely used International Technical Guidance on Sexuality Education (UNESCO 2018). This invaluable publication, co-published by the United Nations Educational, Scientific and Cultural Organization (UNESCO), UNAIDS, UNFPA, UNICEF, UN Women and WHO, promotes comprehensive sex education worldwide. The importance of the VMMC campaign is mentioned in the “Understanding, recognizing, and reducing the risk of STIs (sexually transmitted infections), including HIV for children older than 12 years old” program, and is referenced together with pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) (UNESCO 2018: 79).
11.3.4 A New Trend
There has been an increasing trend toward the promotion of “intactivism”, which advocates for the eradication of routine NMC. The AAP’s position statement has been criticized by non-US-based physicians and representatives of general medical associations and societies for pediatrics, pediatric surgery, and pediatric urology in northern Europe. They argued that “the possible protection against urinary tract infections in infant boys…can easily be treated with antibiotics without tissue loss. The other claimed health benefits, including protection against HIV/AIDS, genital herpes, genital warts, and penile cancer, are questionable, weak, and likely to have little public health relevance in a Western context, and they do not represent compelling reasons for surgery before boys are old enough to decide for themselves” (Frisch et al. 2013: 796). The Nordic Ombudsmen for Children and Pediatric Experts issued the following joint statement: “Circumcision, performed without a medical indication, on a person who is incapable of giving consent, violates fundamental medical-ethical principles, not least because the procedure is irreversible, painful, and may cause serious complications. There are no health-related reasons for circumcising young boys in the Nordic countries. Circumstances that may make circumcision advantageous for adult men are of little relevance to young boys in the Nordic countries, and on these matters the boys will have the opportunity to decide for themselves when they reach the age and maturity required to give consent” (Lindboe et al. 2013). The Child Rights International Network and Council of Europe also issued their position statements, which articulate that the autonomy and bodily integrity of all children should be protected regardless of gender or intersex condition (CRIN 2013; Council of Europe 2013).
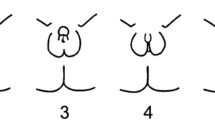
The ripples of this advocacy movement are slowly but surely progressing, even though male genital cutting has not been profiled as a human rights violation to the same extent as FGM/C at a global level. The Brussels Collaboration on Bodily Integrity (2019) summarized the shared features of different forms of un-consenting, medically unnecessary genital cutting as follows: an invasive surgical procedure that results in permanent physical alteration of a body part; medically unnecessary; overwhelmingly performed on minors, including infants or children without free, full, and informed consent; and performed in accordance with norms, beliefs, or values that may not be the child’s own, and which the child may not adopt when of age (see Fig. 11.1).
As of April 2022, the major bodies leading human rights campaigns, namely the UN, Amnesty International, and Human Rights Watch, along with other agencies specializing in the protection of children’s rights (such as UNICEF and UNESCO) and major sexual and reproductive health and rights (SRHR) advocacy groups, such as the International Planned Parenthood Federation (IPPF) and WAS, have not stated that involuntary nontherapeutic genital cutting is a violation of human rights regardless of gender. Again, it seems inaccurate to describe the pricking and piercing of female body parts as a more invasive practice than partial or total removal of the foreskin, as performed on boys within the same communities without their consent and with no therapeutic merit; nevertheless, the latter has somehow been tolerated. Why is this the case?
11.4 A Conflict of Issues
One reason for this tolerance could be a conflict of issues. Charli Carpenter, a professor in the Department of Political Science and Legal Studies at the University of Massachusetts-Amherst specializing in international law and human security, analyzed why some issues get neglected by the “elite gatekeepers” of global human rights campaigns (Carpenter 2014). In the case of male circumcision, some critical challenges faced by “intactivists” were cited (e.g., child rights vs. religious or cultural rights, failure to recognize the vulnerable victim and guilty perpetrator, competition between the two genders associated with gender-mainstreaming, and the global promotion of VMMC). Building on Carpenter’s work, the complexities and challenges can be summarized as follows:
-
(1)
Despite the longstanding medical debate surrounding VMMC and the criticism of campaigns such as VMMC2021 in eastern and southern Africa on grounds of perceived racism, stereotypes, and Western neocolonialism (Fish et al. 2020), global promotion of male circumcision is intensifying. This type of campaign can be easily misconstrued as encouraging routine NMC or other types of medically unnecessary genital cutting in childhood. The current author’s concern extends to the insufficient emphasis on the autonomy and bodily integrity of boys and young men, even in an inarguably valuable document such as International Technical Guidance on Sexuality Education (UNESCO 2018). This document refers to genital cutting/male circumcision only in the context of VMMC. However, it does highlight the importance of learning about values, rights, and culture, and sets a goal for learners (aged ≥15 years) of being able to “analyze local and/or national laws and policies concerning child, early, and forced marriage (CEFM), FGM/C, non-consensual surgical interventions on intersex children, forced sterilization, age of consent, gender equality, sexual orientation, gender identity, abortion, rape, sexual abuse, sex trafficking; and people’s access to sexual and reproductive health services and reproductive rights” (UNESCO 2018: 47). It seems peculiar that male circumcision is missing from such a comprehensive list.
Sexual health, as defined by the WHO, is “a state of physical, emotional, mental, and social well-being in relation to sexuality, and is not merely the absence of disease, dysfunction, or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination, and violence. For sexual health to be attained and maintained, the sexual rights of all persons must be respected, protected, and fulfilled” (WHO 2006). Children (and parents who may be considering having their children circumcised) have the right to learn more about the foreskin and its protective, sexual, sensory, mechanical, and immunological functions. The foreskin is elastic, double-layered, and comprised of skin, mucosa, specialized nerves, blood vessels, and muscle fibers; it protects the glans of the penis, keeping it moist and sensitive, provides lubrication that enhances pleasure during sexual activity, and has specialized immunological components. As with any medical procedure circumcision has potential risks, including not only immediate and post-operative damage (e.g., excessive bleeding and accidental amputation of the glans), but also long-term psychosocial damage (e.g., diminished sexual pleasure, and negative body and self-image). Awareness of peer and social pressure regarding how the penis should appear must be also discussed to enable free, full, and informed consent.
-
(2)
While children are not considered to have absolute autonomy, their autonomy tends to be negated entirely in debates regarding children’s rights versus religious, cultural and parental rights. These debates thus remain contentious and highly polarized. Analysis of both the scale and impact of female and male circumcision exposes a clear double standard within a male-controlled system that legitimizes and justifies acts of violence against, and repression and stigmatization of girls and women. In contrast, male circumcision is normalized as a relatively safe, harmless and common practice.
-
(3)
Gender mainstreaming has created competition. As Carpenter notes, “the gender equity argument through reference to FGM linked circumcision not to children’s human rights but to health and to gender—two issue clusters where the strong ethical argument about children’s rights held far less sway” (Carpenter 2014: 145). The fixed position of the vulnerable victim makes the pain, scarring, suffering, and other psychosocial complications experienced by girls and women even more profound and intergenerational, while infant males and young boys are automatically assumed to face little or no social or psychological stigma as the result of circumcision. Ilsa Lottes, an American Sociologist, draws attention to the inclusive nature of sexual rights by using the phrase “human rights related to sexuality”, where “the term sexual rights is sometimes narrowly interpreted in terms of reproductive rights and abortion, women’s rights, or the rights of LGBT individuals” (Lottes 2013: 383).
-
(4)
In relation to parents’ rights, definitions of the obviously vulnerable victim and obviously guilty perpetrator are missing from the male genital mutilation debate. Parents are considered to make decisions regarding NMC in the best interests of their child, rather than engaging in an abusive act. However, studies of parental decisions about elective NMC indicate that whether the father is circumcised influences the decision to perform NMC on the son. It should be noted that families in which the father was circumcised were overwhelmingly more likely to view NMC as a safe procedure for all boys; in fact, only families in which the father was not circumcised stated that NMC was unsafe (Rediger and Muller 2013; Ku et al. 2003).
This children’s rights versus parents’ rights debate parallels the intersex rights movement. During the 1990s, US-based intersex rights advocates began to openly and explicitly argue against medically unnecessary surgeries performed on un-consenting intersex children. The beliefs/recommendations of these advocates were as follows: intersexuality is primarily a problem of stigma and trauma, not gender; the child is the patient, not the parents; professional mental health care is essential; honest, complete disclosure represents good medicine; and all children should be assigned as male or female, without un-consenting “normalizing” surgery (Chase 2003).
According to a 2015 European Union Agency for Fundamental Rights (FRA) report on the fundamental rights of intersex people in the European Union, “normalizing” surgery is carried out on intersex children in at least 21 member states, in 8 of which “a legal representative can consent to sex ‘normalizing’ medical interventions independently of the child’s ability to decide” (FRA 2015). This situation mirrors that occurring globally, where such medical intervention is widely available. However, conventional norms, beliefs, and values holding that a child’s body must conform to a strict gender binary code have been challenged and discussed (such that views are slowly changing), with the goal of ensuring autonomy and bodily integrity (which is considered to be in the best interests of the child). The Free and Equal global public awareness/human rights campaign was concerned with SOGIESC (OHCHR 2019). Other notable agencies, such as the Human Rights Watch and Amnesty International, have also condemned such surgical intervention as “harmful”, and have called on governments and parents to wait until a child is old enough to make a free, full, and informed consent (Amnesty International 2013; Human Rights Watch 2017; OHCHR 2019; WHO 2014). Current worldwide efforts to raise awareness about intersex issues are a good example of how an unnoticed, “neglected” issue can achieve international prominence.
11.5 Conclusion: Leave No One Behind
As stated in the Introduction, “no one should be left behind.” This is the central tenet of the transformative, aspirational Sustainable Development Goals (SDGs) outlined in the 2030 Agenda for Sustainable Development (which set out a 15-year plan to achieve the goals). It represents the commitment made by all UN Member States to work towards eradicating poverty, discrimination and exclusion, and to reduce inequalities that render people vulnerable, particularly children. Goal 5.3., pertaining to gender equality, is to “Eliminate all harmful practices, such as child, early, and forced marriage and female genital mutilation” (United Nations 2015: 18).
There is growing public interest in FGM/C eradication campaigns that highlight its severe negative impact on girls and women. These campaigns frame FGM/C as a global human rights and reproductive health issue. Coalitions promoting intactivism, i.e., the eradication of NMC and any other form of involuntary male genital cutting, share these same common goals and aspirations. The concept of gender is not, and should not be, restricted to cisgender and/or heterosexual girls and women.
Autonomy and bodily integrity should be protected through approaches based on human rights, empowerment and capabilities, regardless of race, immigration status, assigned sex, experienced gender, sex characteristics, or sexual orientation. The importance of free, full, and informed consent requires us to delay surgery until the individuals involved are old enough to make their own decisions.
Notes
- 1.
The prevalence of intersex conditions is estimated to be between 0.05% and 1.7% in the general population (Fausto-Sterling 2000; Blackless et al. 2000). Some intersex conditions do not fall under the medical diagnosis of disorders of sexual development (DSD), a group of approximately 60 conditions in which chromosomal sex is inconsistent with phenotypic sex, or in which the phenotype is not classifiable as either male or female (Sax 2002).
- 2.
There has been a global trend toward new gender recognition laws that do not have medical interventions as prerequisites, and toward the reformation of existing laws (see ILGA World 2020).
- 3.
The UN Free & Equal campaign did not include intersex issues in their global campaign, stating that: “If transgender people are often overlooked, intersex people have been nearly invisible, at least until recently. This is reflected in the acronyms used. Until a few years ago, the official UN acronym was LGBT. The ‘I’ was added after consultations with intersex people, though not all intersex activists were in favor of being associated with the LGBT community” (Trithart 2021:11–12).
Using the term “intersex”, as in LGBTI in human rights campaigns, is a conscious political choice. The adoption of this term instead of “people with a disorder of sexual development (DSD)” represents the “de-medicalization” of diverse sex characteristics.
- 4.
For example, circumcision has always been extremely rare in Japan, where it is generally referred to as “phimosis surgery” or “foreskin cutting”. The most recent community-based study reported that, among 4126 male respondents (aged >18 years) recruited online, only 4% reported being circumcised (Onuki and Higashi 2019). Male genital cutting in Japan is practiced largely at beauty and aesthetic clinics, typically as a means to regain control of the body and enhance self-confidence (Castro-Vázquez 2012). The prevalence of NMC remains unknown.
References
AAP Task Force on Circumcision (2012) Circumcision policy statement. Pediatrics 130(3):585–586
Amnesty International (2013) Amnesty international policy statement on the rights of intersex individuals. https://interactadvocates.org/wp-content/uploads/2017/03/Amnesty-International-Policy-on-Intersex.pdf. Accessed 18 March 2022
Beh HG, Diamond M (2000) An emerging ethical and medical dilemma: should physicians perform sex assignment surgery on infants with ambiguous genitalia? Michigan J Gender Law 7(1):1–63
Blackless M, Charuvastra A, Derryck A, Fausto-Sterling A, Lauzanne K, Lee L (2000) How sexually dimorphic are we? Review and synthesis. Am J Hum Biol 12(2):151–166
Brussels Collaboration on Bodily Integrity (2019) Medically unnecessary genital cutting and the rights of the child: Moving toward consensus. Am J Bioeth 19(10):17–28
Carpenter C (2014) Lost cause: agenda vetting in global issue networks and shaping of human security. Cornell University, New York
Castro-Vázquez G (2012) The “Beauty” of male circumcision in Japan: gender, sexuality and the male body in a medical practice. Sociology 47(4):687–704
Chase C (2003) What is the agenda of the intersex patient advocacy movement? Endocrinol 13(3):240–242
Child Rights International Network (CRIN) (2013) Submission of the child rights international network (CRIN) to the OHCHR study on children’s right to health (Human Rights Council Resolution 19/37). https://www.ohchr.org/sites/default/files/Documents/Issues/Children/Study/RightHealth/Child_Rights_International_Network_CRIN.pdf. Accessed 18 March 2022
Cohen SD (1997) Why aren’t Jewish women circumcised? Gender Hist 9(3):560–578
Colapinto J (2000) As nature made him: the boy who was raised as a girl. HarperCollins Publishers, Toronto
Correa S, Howe C (2007) Global perspectives on sexual rights. In: Herdt G, Howe C (eds) 21st century sexualities: contemporary issues in health, education, and rights. Routledge, New York, pp 170–173
Council of Europe (2013) Children’s right to physical integrity [resolution 1952]. http://assembly.coe.int/nw/xml/XRef/Xref-XML2HTML-en.asp?fileid=20174. Accessed 18 March 2022
Cox G, Morris BJ (2012) Why circumcision: from pre-history to the twenty-first century. In: Bolnick DA, Koyle MA, Yosha A (eds) Surgical guide to circumcision. Springer, London, pp 243–259
Dunsmuir WD, Gordon EM (1999) The history of circumcision. BJU Int 83(1):1–12
El-Gohary MA (2015) Circumcision: history, philosophy and facts. Open J Urol 5:14–117. https://doi.org/10.4236/oju.2015.58018
European Union Agency for Fundamental Rights (FRA) (2015) FRA focus: the fundamental rights situation of intersex people. https://fra.europa.eu/sites/default/files/fra_uploads/fra-2015-focus-04-intersex_en.pdf. Accessed 18 March 2022
Fausto-Sterling A (2000) Sexing the body: gender politics and the construction of sexuality. Basic Books, New York
Fish M, Shahvisi A, Gwaambuka T et al (2020) A new Tuskegee? Unethical human experimentation and Western neocolonialism in the mass circumcision of African men. Dev World Bioeth 21:211–226
Frisch M, Aigrain Y, Barauskas V et al (2013) Cultural bias in the AAP’s 2012 technical report and policy statement on male circumcision. Pediatrics 131(4):796–800. https://doi.org/10.1542/peds.2012-2896
Gender Identity Research and Education Society (GIRES) (2006) Atypical gender development: a review. Int J Transgenderism 9(1):29–44
Health, Empowerment, Rights, & Accountability (HERA) (1998) HERA action sheet on sexual rights. http://www.users.interport.net/i/w/iwhc/hera/. Accessed 18 March 2022
Human Rights Watch (2017) “I want to be like nature made me.” Medically unnecessary surgeries on intersex children in the US. Author, New York
Iguchi Y, Rashid A (2019) “Female genital mutilation” and the politics of discourse: questioning the self-evidence of the modern medical scientific Gaze. Ann Rev Cult Stud 7:27–45
ILGA World (2020) Trans legal mapping report 2019: recognition before the law. ILGA World, Geneva.https://ilga.org/downloads/ILGA_World_Trans_Legal_Mapping_Report_2019_EN.pdf. Accessed 18 March 2022
International Planned Parenthood Federation (IPPF) (2008) Sexual rights: an IPPF declaration. Author, London
Johnsdotter S (2018) Girls and boys as victims: asymmetries and dynamics in European public discourses on genital modifications in children. In: Fusaschi M, Cavarta G (eds) FGM/C: from medicine to critical anthropology. Meti Edizioni, Turin, pp 31–50
Kessler S (1998) Lessons from the intersexed. Rutgers University Press, NJ
Kim DS, Koo SA, Pang MG (2012) Decline in male circumcision in South Korea. BMC public health, 12, pp 1067–1074, http://www.biomedcentral.com/1471-2458/12/1067. Accessed 18 March 2022
Kirkendall LA (1976) A new bill of sexual rights and responsibilities. Prometheus Books, Buffalo
Ku JH, Kim ME, Lee NK, Park YH (2003) Circumcision practice patterns in South Korea: community based survey. Sex Transm Infect 79:65–67
Lindboe A, Malmberg F, Aula MK et al (2013) Let the boys decide on circumcision: joint statement from the Nordic Ombudsmen for children and pediatric experts. https://www.arclaw.org/wp-content/uploads/Nordic-Ombudsmen-for-Children-Joint-Statement-Let-the-Boys-Decide-on-Circumcision-Cosigned-by-Norway-nursing-union-9-13.pdf. Accessed 18 March 2022
Lottes IL (2013) Sexual rights: meanings, controversies, and sexual health promotion. J Sex Res 50(3–4):367–391
Morimoto I (1989) External genital organs in male mummies from Qurna, Egypt. J Anthropol so. Nippon 97(2):169–187
Morris BJ, Wamai RG, Henebeng EB, Tobian AAR, Klausner JD, Banerjee J, Hankins CA (2016) Estimation of country-specific and global prevalence of male circumcision. Popul Health Metrics 14(4):1–13
Nelson CP, Dunn R, Wan J, Wei JT (2005) The increasing incidence of newborn circumcision: data from the nationwide inpatient sample. J Urol 173:978–981
Nussbaum MC (2007) Human rights and human capabilities. Harvard Human Rights J 20:21–24
Office of the United Nations High Commissioner for Human Rights (OHCHR). (2019). BORN FREE AND EQUAL Sexual orientation, gender identity and sex characteristics in international human rights law (Second Edition). https://www.ohchr.org/sites/default/files/Documents/Publications/Born_Free_and_Equal_WEB.pdf. Accessed 18 March 2022
Onuki D, Higashi Y (2019) Is the Japanese penis different?–The “Third Way” to circumcision debate. Int J Sex Health 31:284–285
Pang MG, Kim DS (2002) Extraordinarily high rates of male circumcision in South Korea: history and underlying causes. BJU Int 89:48–54
Rediger C, Muller A (2013) Parents’ rationale for male circumcision. Can Fam Physician 59(2):110–115
Sax L (2002) How common is intersex? A response to Anne Fausto-Sterling. J Sex Res 39(3):174–178
Taher M (2017) Understanding female genital cutting in the Dawoodi Bohra community: an exploratory survey (SAHIYO report). https://sahiyo.files.wordpress.com/2017/02/sahiyo_report_final-updatedbymt2.pdf. Accessed 18 March 2022
Trithart A (2021) Twenty-five years of advancement on SOGIESC at the UN. In: A UN for All?: UN policy and programming on sexual orientation, gender identity and expression, and sex characteristics. International. Peace Institute, pp 2–12
United Nations (UN) (1994) Report of the international conference on population and development (United Nations No. A/Conf. 171/13). Author, NY
United Nations (UN) (1995) Report of the fourth world conference on women (United Nations No. A/Conf 177/20). Author, Beijing, NY
United Nations (UN) (2015) Transforming our world: the 2030 agenda for sustainable development, 21 October 2015, A/RES/70/1, https://www.refworld.org/docid/57b6e3e44.html. Accessed 18 March 2022
United Nations (UN) (2016) End violence and harmful medical practices on intersex children and adults, UN and regional experts urge (joint statement). https://www.ohchr.org/en/2016/10/intersex-awareness-day-wednesday-26-october?LangID=E&NewsID=20739. Accessed 18 March 2022
United Nations Educational, Scientific and Cultural Organization (UNESCO) (2018) International technical guidance on sexuality education: an evidence-informed approach (Revised edition). https://www.unfpa.org/sites/default/files/pub-pdf/ITGSE.pdf. Accessed 18 March 2022
Waszak SJ (1978) The historic significance of circumcision. Obstet Gynecol 51(4):499–501
Women’s Global Network for Reproductive Rights (WGNRR) (1996) What are women’s sexual rights? Women’s Global Network for Reproductive Rights Newsletter 53:31
World Association for Sexual Health (WAS) (1999) Declaration of sexual rights. In: WAS Sexual health for the millennium. A declaration and technical document, 2008
World Association for Sexual Health (WAS) (2008) Sexual health for the millennium. A declaration and technical document. World Association for Sexual Health, Minneapolis, MN, USA
World Association for Sexual Health (WAS) (2014) Declaration of sexual rights. https://worldsexualhealth.net/wp-content/uploads/2013/08/Declaration-of-Sexual-Rights-2014-plain-text.pdf. Accessed 18 March 2022
World Health Organization (WHO) (2006) Defining sexual health. https://www.who.int/teams/sexual-and-reproductive-health-and-research/key-areas-of-work/sexual-health/defining-sexual-health (updated in 2010). Accessed 18 March 2022
World Health Organization (WHO) (2008) Eliminating female genital mutilation: an interagency statement (UNAIDS, UNDP, UNECA, UNESCO, UNFPA, UNHCHR, UNHCR, UNICEF, UNIFEM and WHO). https://www.who.int/publications/i/item/9789241596442. Accessed 18 March 2022
World Health Organization (WHO) (2014) Eliminating forced, coercive and otherwise in-voluntary sterilization: an interagency statement (OHCHR, UN Women, UNAIDS, UNDP, UNFPA, UNICEF and WHO). https://apps.who.int/iris/bitstream/handle/10665/112848/9789241507325_eng.pdf?sequence=1. Accessed 18 March 2022
World Health Organization (WHO) and Joint United Nations Programme on HIV/AIDS (UNAIDS) (2007) Male circumcision: global trends and determinants of prevalence, safety and acceptability. https://apps.who.int/iris/bitstream/handle/10665/43749/9789241596169_eng.pdf?sequence=1. Accessed 18 March 2022
World Health Organization (WHO) and Joint United Nations Programme on HIV/AIDS (UNAIDS) (2016) A framework for voluntary medical male circumcision: effective HIV prevention and a gateway to improved adolescent boys’ & men’s health in Eastern and Southern Africa by 2021. https://apps.who.int/iris/handle/10665/246234. Accessed 18 March 2022
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Appendix: Declaration of Sexual Rights
Appendix: Declaration of Sexual Rights
In recognition that sexual rights are essential for the achievement of the highest attainable sexual health, the World Association for Sexual Health:
States that sexual rights are grounded in universal human rights that are already recognized in international and regional human rights documents, in national constitutions and laws, human rights standards, and principles, and in scientific knowledge related to human sexuality and sexual health.
Reaffirms that sexuality is a central aspect of being human throughout life, encompasses sex, gender identities and roles, sexual orientation, eroticism, pleasure, intimacy, and reproduction. Sexuality is experienced and expressed in thoughts, fantasies, desires, beliefs, attitudes, values, behaviors, practices, roles, and relationships. While sexuality can include all of these dimensions, not all of them are always experienced or expressed. Sexuality is influenced by the interaction of biological, psychological, social, economic, political, cultural, legal, historical, religious, and spiritual factors.
Recognizes that sexuality is a source of pleasure and wellbeing and contributes to overall fulfillment and satisfaction.
Reaffirms that sexual health is a state of physical, emotional, mental, and social wellbeing in relation to sexuality, and not merely the absence of disease, dysfunction or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination, and violence.
Reaffirms that sexual health cannot be defined, understood, or made operational without a broad understanding of sexuality.
Reaffirms that for sexual health to be attained and maintained, the sexual rights of all persons must be respected, protected, and fulfilled.
Recognizes that sexual rights are based on the inherent freedom, dignity, and equality of all human beings and include a commitment to protection from harm.
States that equality and non-discrimination are foundational to all human rights protection and promotion, and include the prohibition of any distinction, exclusion, or restriction on the basis of race, ethnicity, color, sex, language, religion, political, or other opinion, national or social origin, property, birth or other status, including disability, age, nationality, marital and family status, sexual orientation and gender identity, health status, place of residence, or economic and social situation.
Recognizes that persons’ sexual orientations, gender identities, gender expressions, and bodily diversities require human rights protection.
Recognizes that all types of violence, harassment, discrimination, exclusion, and stigmatization are violations of human rights, and impact the wellbeing of individuals, families, and communities.
Affirms that the obligations to respect, protect, and fulfill human rights apply to all sexual rights and freedoms.
Affirms that sexual rights protect all people’s rights to fulfill and express their sexuality and enjoy sexual health, with due regard for the rights of others.
Sexual rights are human rights pertaining to sexuality:
-
1.
The right to equality and non-discrimination
Everyone is entitled to enjoy all sexual rights set forth in this Declaration without distinction of any kind such as race, ethnicity, color, sex, language, religion, political or other opinion, national or social origin, place of residence, property, birth, disability, age, nationality, marital and family status, sexual orientation, gender identity and expression, health status, economic and social situation, or other status.
-
2.
The right to life, liberty, and security of the person
Everyone has the right to life, liberty, and security that cannot be arbitrarily threatened, limited, or taken away for reasons related to sexuality. These include: sexual orientation, consensual sexual behavior and practices, gender identity and expression, or the access to or provision of services related to sexual and reproductive health.
-
3.
The right to autonomy and bodily integrity
Everyone has the right to control and decide freely on matters related to their sexuality and their body. This includes the choice of sexual behaviors, practices, partners, and relationships with due regard to the rights of others. Free and informed decision making requires free and informed consent prior to any sexually-related testing, intervention, therapy, surgery, or research.
-
4.
The right to be free from torture and cruel, inhuman, or degrading treatment or punishment
Everyone shall be free from torture and cruel, inhuman, or degrading treatment or punishment related to sexuality, including harmful traditional practices; forced sterilization, contraception, or abortion; and other forms of torture, cruel, inhuman, or degrading treatment perpetrated for reasons related to someone’s sex, gender, sexual orientation, gender identity and expression, and bodily diversity.
-
5.
The right to be free from all forms of violence and coercion
Everyone shall be free from sexuality related violence and coercion, including: rape, sexual abuse, sexual harassment, bullying, sexual exploitation and slavery, trafficking for purposes of sexual exploitation, virginity testing, and violence committed because of real or perceived sexual practices, sexual orientation, gender identity and expression, and bodily diversity.
-
6.
The right to privacy
Everyone has the right to privacy related to sexuality, their sexual life, and choices regarding their own body and consensual sexual relations and practices without arbitrary interference and intrusion. This includes the right to control the disclosure of sexuality-related personal information to others.
-
7.
The right to the highest attainable standard of health, including sexual health, with the possibility of pleasurable, satisfying, and safe sexual experiences
Everyone has the right to the highest attainable level of health and wellbeing in relation to sexuality, including the possibility of pleasurable, satisfying, and safe sexual experiences. This requires the availability, accessibility, acceptability of quality health services, and access to the conditions that influence and determine health, including sexual health.
-
8.
The right to enjoy the benefits of scientific progress and its application
Everyone has the right to enjoy the benefits of scientific progress and its applications in relation to sexuality and sexual health.
-
9.
The right to information
Everyone shall have access to scientifically accurate and understandable information related to sexuality, sexual health, and sexual rights through diverse sources. Such information should not be arbitrarily censored, withheld, or intentionally misrepresented.
-
10.
The right to education and the right to comprehensive sexuality education
Everyone has the right to education and comprehensive sexuality education. Comprehensive sexuality education must be age appropriate, scientifically accurate, culturally competent, and grounded in human rights, gender equality, and a positive approach to sexuality and pleasure.
-
11.
The right to enter, form, and dissolve marriage and other similar types of relationships based on equality and full and free consent
Everyone has the right to choose whether or not to marry and to enter freely and with full and free consent into marriage, partnership or other similar relationships. All persons are entitled to equal rights when entering into, during, and at the dissolution of marriage, partnerships, and other similar relationships, without discrimination and exclusion of any kind. This right includes equal entitlements to social welfare and other benefits regardless of the form of such relationships.
-
12.
The right to decide whether to have children, the number and spacing of children, and to have the information and the means to do so
Everyone has the right to decide whether to have children and the number and spacing of children. To exercise this right requires access to the conditions that influence and determine health and wellbeing, including sexual and reproductive health services related to pregnancy, contraception, fertility, pregnancy termination, and adoption.
-
13.
The right to the freedom of thought, opinion, and expression
Everyone has the right to freedom of thought, opinion, and expression regarding sexuality and has the right to express their own sexuality through, for example, appearance, communication, and behavior, with due respect to the rights of others.
-
14.
The right to freedom of association and peaceful assembly
Everyone has the right to peacefully organize, associate, assemble, demonstrate, and advocate including about sexuality, sexual health, and sexual rights.
-
15.
The right to participation in public and political life
Everyone is entitled to an environment that enables active, free, and meaningful participation in and contribution to the civil, economic, social, cultural, political, and other aspects of human life at local, national, regional, and international levels. In particular, all persons are entitled to participate in the development and implementation of policies that determine their welfare, including their sexuality and sexual health.
-
16.
The right to access to justice, remedies, and redress
Everyone has the right to access justice, remedies, and redress for violations of their sexual rights. This requires effective, adequate, accessible, and appropriate educative, legislative, judicial, and other measures. Remedies include redress through restitution, compensation, rehabilitation, satisfaction, and guarantee of non-repetition.
The World Association for Sexual Health (WAS) is a multidisciplinary, worldwide group of scientific societies, NGOs, and professionals in the field of human sexuality, which promotes sexual health throughout the lifespan and through the world by developing, promoting, and supporting sexology and sexual rights for all. The WAS accomplishes this by advocacy actions, networking, facilitating the exchange of information, ideas, and experiences and advancing scientifically based sexuality research, sexuality education and clinical sexology, with a trans-disciplinary approach. The WAS Declaration of Sexual Rights was originally proclaimed at the 13th World Congress of Sexology in Valencia, Spain, in 1997 and then, in 1999, a revision was approved in Hong Kong by the WAS General Assembly and then reaffirmed in the WAS Declaration: Sexual Health for the Millennium (2008). This revised declaration was approved by the WAS Advisory Council in March, 2014.
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (http://creativecommons.org/licenses/by-nc-nd/4.0/), which permits any noncommercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if you modified the licensed material. You do not have permission under this license to share adapted material derived from this chapter or parts of it.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Higashi, Y. (2023). Autonomy, Bodily Integrity and Male Genital Cutting. In: Nakamura, K., Miyachi, K., Miyawaki, Y., Toda, M. (eds) Female Genital Mutilation/Cutting. Springer, Singapore. https://doi.org/10.1007/978-981-19-6723-8_11
Download citation
DOI: https://doi.org/10.1007/978-981-19-6723-8_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-6722-1
Online ISBN: 978-981-19-6723-8
eBook Packages: Law and CriminologyLaw and Criminology (R0)