Abstract
Although sudden death caused by digestive system diseases, accounting for about 7% of sudden death diseases, is not common compared with other diseases such as cardiovascular disease, it is also worthy of attention. Among them, sudden death caused by acute pancreatitis is the most common, accounting for 0.2%-0.5% of natural sudden death, and is one of the important causes of non-cardiac sudden death. This chapter mainly focuses on a series of sudden death related digestive system diseases, including ischemic bowel disease, variceal upper gastrointestinal bleeding in cirrhotic portal hypertension, hepatic encephalopathy, liver failure, acute suppurative cholangitis and acute pancreatitis. This type of disease is characterized by a rapid onset, a rapid progress, and a high mortality rate. Combining typical cases, this chapter describes the pathogenesis, diagnosis and treatment progress of the above-mentioned diseases that may cause sudden death.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Brandt LJ, Boley SJ. AGA technical review on intestinal ischemia. Gastroenterology. 2000;118(5):954–68.
Jaster A, Choudhery S, Ahn R, Sutphin P, Kalva S, Anderson M, et al. Anatomic and radiologic review of chronic mesenteric ischemia and its treatment. Clin Imaging. 2016;40(5):961–9.
Corcos O, Nuzzo A. Gastro-intestinal vascular emergencies. Best Pract Res Clin Gastroenterol. 2013;27(5):709–25.
Brandt LJ, Feuerstadt P, Longstreth GF, Boley SJ. ACG clinical guideline: epidemiology, risk factors, patterns of presentation, diagnosis, and management of colon ischemia (CI). Am J Gastroenterol. 2015;110(1):18–44.
Flynn AD, Valentine JF. Update on the diagnosis and management of colon ischemia. Curr Treat Option Gastroenterol. 2016;14(1):128–39.
Yadav S, Dave M, Edakkanambeth VJ, Harmsen WS, Tremaine WJ, Zinsmeister AR, et al. A population-based study of incidence, risk factors, clinical spectrum, and outcomes of ischemic colitis. Clin Gastroenterol Hepatol. 2015;13(4):731–8.
Brandt L, Boley S, Goldberg L, Mitsudo S, Berman A, et al. Colitis in the elderly. A reappraisal. Am J Gastroenterol. 1981;76(3):239–45.
Kozuch PL, Brant LJ. Review article: diagnosis and management of mesenteric ischemia with an emphasis on pharmacotherapy. Aliment Pharmacol Ther. 2005;21(3):201–15.
Van der Voort PH, Westra B, Wester JP, Bosman RJ, van Stijn I, Haagen IA, et al. Can serum L-lactate, D-lactate, creatine kinase and I-FABP be used as diagnostic markers incritically ill patients suspected for bowel ischemia. BMC Anesthesiol. 2014;14:111.
Assadian A, Assadian O, Senekowitsch C, Rotter R, Bahrami S, Furst W, et al. Plasma D-lactate as a potential early marker for colon ischaemia after open aortic reconstruction. Eur J Vasc Endovasc Surg. 2006;31(5):470–4.
Levy E, Menard D, Delvin E, Montoudis A, Beaulieu JF, Mailhot G, et al. Localization, function and regulation of the two intestinal fatty acid-binding protein types. Histochem Cell Biol. 2009;132(3):35l–67.
Kanda T, Hujii H, Tani T, Murakami H, Suda T, Sakai Y, et al. Intestinal fatty acid-binding protein is a useful diagnostic marker for mesenteric infarction in humans. Gastroenterology. 1996;110(2):339–43.
Akyildiz H, Akcan A, Oztürk A, Sozuer E, Kucuk C, Karahan I. The correlation of the D-dimer test and biphasic computed tomography with mesenteric computed tomography angiography in the diagnosis of acute mesenteric ischemia. Am J Surg. 2009;197(4):429–33.
Sutherland F, Cunningham H, Pontikes L, Parsons L, Klassen J. Elevated serum interleukin-6 levels in patients with acute intestinal ischemia. Hepato-Gastroenterology. 2003;50(50):419–21.
Acosta S, Nilsson TK, Bjorck M. Preliminary study of D-dimer as a possible marker of acute bowel ischaemia. Br J Surg. 2001;88(3):385–8.
Woodhams R, Nishimaki H, Fujii K, Kakita S, Hayakawa K. Usefulness of multidetector-row CT (MDCT) for the diagnosis of non-occlusive mesenteric ischemia (NOMI): assessment of morphology and diameter of the superior mesenteric artery (SMA) on multi-planar reconstructed (MPR) images. Eur J Radiol. 2010;76(1):96–102.
Resch T, Lindh M, Dias N, Sonesson B, Uher P, Malina M, et al. Endovascular recanalisation in occlusive mesenteric ischemia feasibility and early results. Eur J Vasc Endovasc Surg. 2005;29(2):199–203.
Acosta S, Wadman M, Syk I, Elmstahl S, Ekberg O. Epidemiology and prognostic factors in acute superior mesenteric artery occlusion. J Gastrointest Surg. 2010;14(4):628–35.
Cangemi JR, Picco MF. Intestinal ischemia in the elderly. Gastroenterol Clin N Am. 2009;38(3):527–40.
Wadman M, Syk I, Elmståhl B, Ekberg O, Elmstahl S. Abdominal plain film findingsin acute ischemic bowel disease differ with age. Acta Radiol. 2006;47(3):238–43.
Laissy JP, Trillaud H, Douek P. MR angiography: noninvasive vascular imaging of the abdomen. Abdom Imaging. 2002;27(5):488–506.
Stathaki MI, Koutroubakis IE, Koukouraki SI, Kouroumalis EA, Karkavitsas NS. Is there a role for Tc-99m(V) DMSA scintigraphy in ischemic colitis? World J Gastroenterol. 2008;14(35):5432–5.
Polk JD, Rael LT, Craun ML, Mains CW, Davis-Merritt D, Bar-Or D. Clinical utility of the cobalt-albumin binding assay in the diagnosis of intestinal ischemia. J Trauma. 2008;64(1):42–5.
Theodoropoulou A, Koutroubakis IE. Ischemic colitis: clinical practice in diagnosis and treatment. World J Gastroenterol. 2008;14(48):7302–8.
Clinical Services and Standards Committee of the British Society of Gastroenterology. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015;64(11):1680–704.
De Franchis R, Baveno VI Faculty. Expanding consensus in portal hypertension: report of the Baveno VI Consensus workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63(3):743–52.
European Association for the Study of the Liver. EASL clinical practice guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69(2):406–60.
Acute upper gastrointestinal bleeding: management. 2012. NGC:009131 National Clinical Guideline Centre—National Government Agency [Non-U.S].
Esophageal varices. World Gastroenterology Organisation Global Guidelines. 2014.
Carbonell N, Pauwels A, Serfaty L, Fourdan O, Lévy VG, Poupon R. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology. 2004;40(3):652–9.
Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, et al. UK guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015;64(11):1680–704.
Kim YD. Management of acute variceal bleeding. Clin Endosc. 2014;47(4):308–14.
Vorobioff JD, Groszmann RJ. Prevention of portal hypertension:from variceal development to clinical decompensation. Hepatology. 2015;61(1):375–81.
Li M, Xu X. Researches on the prevention and treatment of bleeding gastroesophageal varices secondary to portal hypertension in patients with cirrhosis. Zhonghua Gan Zang Bing Za Zhi. 2015;23(4):247–9. (in Chinese)
Kim DH, Park JY. Prevention and management of variceal hemorrhage. Int J Hepatol. 2013;2013:434609.
Lee YY, Tee HP, Mahadeva S. Role of prophylactic antibiotics in cirrhotic patients with variceal bleeding. World J Gastroenterol. 2014;20(7):1790–6.
Hwang JH, Shergill AK, Acosta RD, Chandrasekhara V, Chathadi KV, Decker GA, et al. The role of endoscopy in the management of variceal hemorrhage. Gastrointest Endosc. 2014;80(2):221–7.
Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association; Chinese Society of Endoscopy, Chinese Medical Association. Guidelines for the diagnosis and treatment of esophageal and gastric variceal bleeding in cirrhotic portal hypertension. J Chin Hepatol. 2016;32(2):203–19. (in Chinese)
Hearnshaw S, Logan R, Lowe D, Travis S, Murphy M, Palmer K. Acute upper gastrointestinal bleeding in the UK: patient characteristics, diagnoses and outcomes in the 2007 UK audit. Gut. 2007;60:1327–35.
Garcia-Tsao G, Bosch J. Management of varices and variceal haemorrhage in cirrhosis. N Engl J Med. 2010;362:823–32.
Garbuzenko DV. Contemporary concepts of the medical therapy of portal hypertension under liver cirrhosis. World J Gastroenterol. 2015;21(20):6117–26.
Sarin SK, Kumar A. Endoscopic treatment of gastric varices. Clin Liver Dis. 2014;18(4):809–27.
Huang L, Yu QS, Zhang Q, Liu JD, Wang Z. Transjugular intrahepatic portosystemic shunt versus surgical shunting in the management of portal hypertension. Chin Med J. 2015;128(6):826–34.
Orloff MJ, Hye RJ, Wheeler HO, Isenberg JI, Haynes KS, Vaida F, et al. Randomized trials of endoscopic therapy and transjugular intrahepatic portosystemic shunt versus portacaval shunt for emergency and elective treatment of bleeding gastric varices in cirrhosis. Surgery. 2015;157(6):1028–45.
Chinese Medical Association Surgery Branch, Department of Portal Hypertension. Expert agreement on diagnosis and treatment of esophageal and gastric varices bleeding in cirrhotic portal hypertension. J Pract Surg. 2015;23(10):1086–90. (in Chinese)
Hadjihambi A, Arias N, Sheikh M, Jalan R. Hepatic encephalopathy: a critical current review. Hepatol Int. 2018;12(61):135–47.
Tranah TH, Paolino A, Shawcross DL. Pathophysiological mechanisms of hepatic encephalopathy. Clin Liver Dis. 2015;5(3):59–63.
Elwir S, Rahimi RS. Hepatic encephalopathy: an update on the pathophysiology and therapeutic options. J Clin Transl Hepatol. 2017;5(2):142–51.
Ochoasanchez R, Rose CF. Pathogenesis of hepatic encephalopathy in chronic liver disease. J Clin Exp Hepatol. 2018;8(3):262–71.
Kenston SS, Song X, Li Z, Zhao J. Mechanistic insight, diagnosis, and treatment of ammonia-induced hepatic encephalopathy. J Gastroenterol Hepatol. 2019;34(1):31–9.
Jayakumar AR, Norenberg MD. Hyperammonemia in hepatic encephalopathy. J Clin Exp Hepatol. 2018;8(3):272–80.
Zwingmann C, Butterworth R. An update on the role of brain glutamine synthesis and its relation to cell-specific energy metabolism in the hyperammonemic brain: further studies using NMR spectroscopy. Neurochem Int. 2005;47:19–30.
Grover VP, Tognarelli JM, Massie N, Crossey MM, Cook NA, Taylorrobinson SD. The why and wherefore of hepatic encephalopathy. Int J General Med. 2015;8(1):381–90.
Felipo V. Hepatic encephalopathy: effects of liver failure on brain function. Nat Rev Neurosci. 2013;14(12):851–8.
Krieger D, Krieger S, Theilmann L, Jansen O, Gass P, Lichtnecker H. Manganese and chronic hepatic encephalopathy. Lancet. 1995;346(8970):270–4.
Chinese Society of Gastroenterology, Chinese Society of Hepatology, Chinese Medical Association. Consensus on the diagnosis and treatment of hepatic encephalopathy in China (Chongqing, 2013). Chin J Hepatol. 2013;21(9):641–51.
Amodio P. Hepatic encephalopathy: diagnosis and management. Liver Int. 2018;38(6):966–75.
Ferenci P, Lockwood A, Mullen K, et al. Hepatic encephalopatlly—definition, nomenclature, diagnosis ,and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna. Hepatology. 2002;35(3):716–21.
Patidar KR, Bajaj JS. Covert and overt hepatic encephalopathy: diagnosis and management. Clin Gastroenterol Hepatol. 2015;13(12):2048–61.
Fischer JE, Rosen HM, Ebeid AM, James JH, Keane J, Soeters PB. The effect of normalization of plasma amino acids on hepatic encephalopathy in man. Surgery. 1976;80(1):77–91.
Coronel-Castillo CE, Contreras-Carmona J, Frati-Munari AC, Uribe M, Méndez-Sánchez N. Efficacy of rifaximin in the different clinical scenarios of hepatic encephalopathy. Rev Gastroenterol Mex. 2020;85(1):56–68.
Tilg H, Cani PD, Mayer EA. Gut microbiome and liver diseases. Gut. 2016;65(12):2035–44.
Schwenger KJ, Clermont-Dejean N, Allard JP. The role of the gut microbiome in chronic liver disease: the clinical evidence revised. JHEP Rep. 2019;1(3):214–26.
Dam G, Aamann L, Vistrup H, Gluud LL. The role of branched chain amino acids in the treatment of hepatic encephalopathy. J Clin Exp Hepatol. 2018;8(4):448–51.
Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association et al. Guideline for diagnosis and treatment of liver failure. Chin J Hepatol. 2019;27(1):18–26.
Wendon J, Cordoba J, Dhawan A, Larsen FS, Manns M, Samuel D, et al. EASL clinical practical guidelines on the management of acute(fulminant)liver failure. J Hepatol. 2017;66(5):1047–81.
Flamm SL, Yang YX, Singh S, Falck-Ytter YT. American gastroenterological association institute guidelines for the diagnosis and management of acute liver failure. Gastroenterology. 2017;152(3):644–7.
Sarin SK, Choudhury A, Sharma MK, Maiwall R, Al Mahtab M, Rahman S, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific association for the study of the liver (APASL): an update. Hepatol Int. 2019;13(4):353–90.
Shao J, Li S, Liu Y, Zheng M. Extracellular vesicles participate in macrophage-involved immune responses under liver diseases. Life Sci. 2020;240:117094.
Dong V, Nanchal R, Karvellas CJ. Pathophysiology of acute liver failure. Nutr Clin Pract. 2020;35(1):24–9.
Han T, Li LJ. Guideline for diagnosis and treatment of liver failure. J Clin Hepatol. 2018;35(1):38–44.
Tujios SR, Lee WM. Acute liver failure induced by idiosyncratic reaction to drugs: challenges in diagnosis and therapy. Liver Int. 2018;38(1):6–14.
Louvet A, Mathurin P. Alcoholic liver disease: mechanisms of injury and targeted treatment. Nat Rev Gastroenterol Hepatol. 2015;12(4):231–42.
Im GY. Acute alcoholic hepatitis. Clin Liver Dis. 2019;23(1):81–98.
Ishibashi H, Komori A, Shimoda S, Gershwin ME. Guidelines for therapy of autoimmune liver disease. Semin Liver Dis. 2007;27(2):214–26.
Yi LP, Zhang W, Wu Z, Duan WJ, Wang Y, Huang J, et al. Present status of diagnosis and treatment of hepatolenticular degeneration. Zhonghua Gan Zang Bing Za Zhi. 2019;27(3):161–5.
Emmanuel T, Audrey C, Silvio N, Josh L, Yaman T, Mark G, et al. International liver transplantation consensus statement on end-stage liver disease due to nonalcoholic steatohepatitis and liver transplantation. Transplantation. 2019;103(1):45–56.
Andrew DJ, Johnson SE. Acute suppurative cholangitis, a medical and surgical emergency. A review of ten years experience emphasizing early recognition. Am J Gastroenterol. 1970;54:141–54.
Shimada H, Nakagawara G, Kobayashi M, et al. Pathogenesis and clinical features of acute cholangitis accompanied by shock. Jpn J Surg. 1984;14:269–77.
Gigot JF, Leese T, Dereme T, et al. Acute cholangitis. Multivariate analysis of risk factors. Ann Surg. 1989;209:435–8.
Kimura Y, Takada T, Kawarada Y, et al. Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepato-Biliary-Pancreat Surg. 2007;14:15–26.
Attasaranya S, Fogel EL, Lehman GA. Choledocholithiasis, ascending cholangitis, and gallstone pancreatitis. Med Clin North Am. 2008;92:925–60.
van den Hazel SJ, Speelman P, Tytgat GN, et al. Role of antibiotics in the treatment and prevention of acute and recurrent cholangitis. Clin Infect Dis. 1994;19:279–86.
Tanaka A, Takada T, Kawarada Y, et al. Antimicrobial therapy for acute cholangitis: Tokyo Guidelines. J Hepato-Biliary-Pancreat Surg. 2007;14:59–67.
Navaneethan U, Jayanthi V, Mohan P. Pathogenesis of cholangitis in obstructive jaundice-revisited. Minerva Gastroenterol Dietol. 2011;57:97–104.
Schwed AC, Boggs MM, Pham XD, et al. Association of admission laboratory values and the timing of endoscopic retrograde cholangiopancreatography with clinical outcomes in acute cholangitis. JAMA Surg. 2016;151:1039–45.
Lee BS, Hwang JH, Lee SH, et al. Risk factors of organ failure in patients with bacteremic cholangitis. Dig Dis Sci. 2013;58:1091–9.
Yokoe M, Hata J, Takada T, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:41–54.
Sulzer JK, Ocuin LM. Cholangitis: causes, diagnosis, and management. Surg Clin North Am. 2019;99:175–84.
Umefune G, Kogure H, Hamada T, et al. Procalcitonin is a useful biomarker to predict severe acute cholangitis: a single-center prospective study. J Gastroenterol. 2017;52:734–45.
Shinya S, Sasaki T, Yamashita Y, et al. Procalcitonin as a useful biomarker for determining the need to perform emergency biliary drainage in cases of acute cholangitis. J Hepatobiliary Pancreat Sci. 2014;21:777–85.
Watanapa P. Recovery patterns of liver function after complete and partial surgical biliary decompression. Am J Surg. 1996;171:230–4.
Solomkin JS, Mazuski JE, Bradley JS, et al. Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:133–64.
Gomi H, Solomkin JS, Schlossberg D, et al. Tokyo Guidelines 2018: antimicrobial therapy for acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2018;25:3–16.
Abboud PA, Malet PF, Berlin JA, et al. Predictors of common bile duct stones prior to cholecystectomy: a meta-analysis. Gastrointest Endosc. 1996;44:450–5.
Buyukasik K, Toros AB, Bektas H, et al. Diagnostic and therapeutic value of ERCP in acute cholangitis. ISRN Gastroenterol. 2013;2013:191729.
Sun Z, Zhu Y, Zhu B, et al. Controversy and progress for treatment of acute cholangitis after Tokyo Guidelines (TG13). Biosci Trends. 2016;10:22–6.
Ramchandani M, Pal P, Reddy DN. Endoscopic management of acute cholangitis as a result of common bile duct stones . Dig Endosc. 2017;29 Suppl 2:78–87.
Boulay BR, Lo SK. Endoscopic ultrasound-guided biliary drainage. Gastrointest Endosc Clin N Am. 2018;28:171–85.
Miura F, Okamoto K, Takada T, et al. Tokyo Guidelines 2018: initial management of acute biliary infection and flowchart for acute cholangitis. J Hepatobiliary Pancreat Sci. 2018;25:31–40.
Liu C-T, Li P, Zhang S-T. ENBD. In: Mine T, Fujita R, editors. Advanced therapeutic endoscopy for pancreatico-biliary diseases. Tokyo: Springer Japan; 2019. p. 51–62.
Sharaiha RZ, Khan MA, Kamal F, et al. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: a systematic review and meta-analysis. Gastrointest Endosc. 2017;85:904–14.
Nennstiel S, Weber A, Frick G, et al. Drainage-related complications in percutaneous transhepatic biliary drainage: an analysis over 10 years. J Clin Gastroenterol. 2015;49:764–70.
Lai EC, Mok FP, Tan ES, et al. Endoscopic biliary drainage for severe acute cholangitis. N Engl J Med. 1992;326:1582–6.
Portelli M, Jones CD. Severe acute pancreatitis: pathogenesis, diagnosis and surgical management. Hepatobiliary Pancreat Dis Int. 2017;16:155–9.
Roberts SE, Akbari A, Thorne K, Atkinson M, Evans PA. The incidence of acute pancreatitis: impact of social deprivation, alcohol consumption, seasonal and demographic factors. Aliment Pharmacol Ther. 2013;38:539–48.
Vege SS, Gardner TB, Chari ST, Munukuti P, Pearson RK, Clain JE, Petersen BT, Baron TH, Farnell MB, Sarr MG. Low mortality and high morbidity in severe acute pancreatitis without organ failure: a case for revising the Atlanta classification to include “moderately severe acute pancreatitis”. Am J Gastroenterol. 2009;104:710–5.
Lankisch PG, Schirren CA, Kunze E. Undetected fatal acute pancreatitis: why is the disease so frequently overlooked? Am J Gastroenterol. 1991;86:322–6.
Forsmark CE, Vege SS, Wilcox CM. Acute pancreatitis. N Engl J Med. 2016;375:1972–81.
Lankisch PG, Apte M, Banks PA. Acute pancreatitis. Lancet. 2015;386:85–96.
Whitcomb DC. Genetic risk factors for pancreatic disorders. Gastroenterology. 2013;144:1292–302.
Sadr-Azodi O, Andren-Sandberg A, Orsini N, Wolk A. Cigarette smoking, smoking cessation and acute pancreatitis: a prospective population-based study. Gut. 2012;61:262–7.
Smeets X, Knoester I, Grooteman KV, Singh VK, Banks PA, Papachristou GI, Duarte-Rojo A, Robles-Diaz G, Kievit W, MGH B, Verdonk RC, Van Santvoort HC, JPH D, Belias M, EJM VG, Dutch Pancreatitis Study G. The association between obesity and outcomes in acute pancreatitis: an individual patient data meta-analysis. Eur J Gastroenterol Hepatol. 2019;31:316–22.
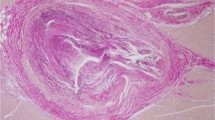
Di Paolo M, Marradi I. Haemorrhagic complication of acute necrotizing pancreatitis presenting with sudden death. J Clin Forensic Med. 2006;13:271–3.
Pastor CM, Matthay MA, Frossard JL. Pancreatitis-associated acute lung injury: new insights. Chest. 2003;124:2341–51.
Browne GW, Pitchumoni CS. Pathophysiology of pulmonary complications of acute pancreatitis. World J Gastroenterol. 2006;12:7087–96.
Zhao X, Andersson R, Wang X, Dib M, Wang X. Acute pancreatitis-associated lung injury: pathophysiological mechanisms and potential future therapies. Scand J Gastroenterol. 2002;37:1351–8.
IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology 2013;13:e1–15.
Turner B. Acute pancreatitis: symptoms, diagnosis and management. Nurs Times. 2003;99:38–40.
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS. Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–11.
Karagoz A, Unluer EE, Oyar O, Topal FE, Topal F. The ability of emergency physicians to diagnose and score acute pancreatitis on computed tomography. Eur J Trauma Emerg Surg. 2017;43:287–92.
Bollen TL, Singh VK, Maurer R, Repas K, van Es HW, Banks PA, Mortele KJ. A comparative evaluation of radiologic and clinical scoring systems in the early prediction of severity in acute pancreatitis. Am J Gastroenterol. 2012;107:612–9.
Siregar GA, Siregar GP. Management of severe acute pancreatitis. Maced J Med Sci. 2019;7:3319–23. Open Access
Balthazar EJ, Ranson JH, Naidich DP, Megibow AJ, Caccavale R, Cooper MM. Acute pancreatitis: prognostic value of CT. Radiology. 1985;156:767–72.
King NK, Powell JJ, Redhead D, Siriwardena AK. A simplified method for computed tomographic estimation of prognosis in acute pancreatitis. Scand J Gastroenterol. 2003;38:433–6.
Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN. American gastroenterological association institute guideline on initial management of acute pancreatitis. Gastroenterology. 2018;154:1096–101.
Zhao G, Zhang JG, Wu HS, Tao J, Qin Q, Deng SC, Liu Y, Liu L, Wang B, Tian K, Li X, Zhu S, Wang CY. Effects of different resuscitation fluid on severe acute pancreatitis. World J Gastroenterol. 2013;19:2044–52.
Bhadade RR, de Souza RA, Harde MJ, Khot A. Clinical characteristics and outcomes of patients with acute lung injury and ARDS. J Postgrad Med. 2011;57:286–90.
Sun B, Zhang C, Lin T, Liu S, Wang Z, Zhang J, Liu C. Effect of continuous renal replacement therapy during percutaneous drainage in severe acute pancreatitis patients: a retrospective cohort study. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2019;31:714–8.
Faghih M, Fan C, Singh VK. New advances in the treatment of acute pancreatitis. Curr Treat Option Gastroenterol. 2019;17:146–60.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Qi, S. et al. (2021). Digestive System Disease and Sudden Death. In: Zhu, H. (eds) Sudden Death. Springer, Singapore. https://doi.org/10.1007/978-981-15-7002-5_23
Download citation
DOI: https://doi.org/10.1007/978-981-15-7002-5_23
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-7001-8
Online ISBN: 978-981-15-7002-5
eBook Packages: MedicineMedicine (R0)