Abstract
COVID-19, arising from novel, zoonotic coronavirus-2, has gripped the world in a pandemic. The present chapter discusses the current internationally implemented pandemic preparedness strategies succeeding/recommended to curb the COVID-19 threat to humankind. The updated phase-wise categorization of a pandemic as recommended by the WHO is described, and associated innovations in surveillance, response, and medical measures/advisory in practice across the globe are elaborated. From a bird’s eye view, the COVID-19 pandemic management relies on revolutionizing the disease surveillance by incorporating artificial intelligence and data analytics, boosting the response strategies—extensive testing, case isolation, contact tracing, and social distancing—and promoting awareness and access to pharmaceutical and non-pharmaceutical interventions, which are discussed in the present chapter. We also preview the economic bearing of the COVID-19 pandemic.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- COVID-19
- Pandemic preparedness
- Surveillance
- Artificial intelligence
- Infectious disease modeling
- Social distancing
14.1 Introduction
The present-day pandemic spotlight on COVID-19 (coronavirus disease-2019) was earlier placed on Zika virus, H1N1, severe acute respiratory syndrome (SARS), chikangunya, Middle East respiratory syndrome (MERS), and Ebola. The “advancements” of the human race—increased urbanization, global travel, changes in land use, and fervent exploitation of the nature—are also the prime reasons for zoonosis and emergence of novel infectious diseases such as above (Madhav et al. 2017; Ahmed et al. 2019). This rapid emergence of novel infectious diseases transmitting from surrounding animal life to humans and then from human to human, traveling quickly across the globe can trigger worldwide public health emergency situations, as prevalent today (https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11March2020, http://www.emro.who.int/fr/about-who/rc61/zoonotic-diseases.html). The World Health Organization (WHO) declared COVID-19 a pandemic on March 11, 2020. MeSH database defines pandemics as—“Epidemics of infectious disease that have spread to many countries, often more than one continent, and usually affecting a large number of people.” Such emergencies compromise human health, society, economics, and politics—a case in point: the COVID-19 pandemic is forecasted to cost the global economy one trillion US dollars (https://www.ncbi.nlm.nih.gov/mesh/?term=pandemics, https://news.un.org/en/story/2020/03/1059011).
As against the earlier guidelines of WHO where it classified a pandemic into six stages, the 2009 revision in pandemic descriptors and stages stands today as follows:
-
Predominantly animal infections, few human infections. This corresponds with the stages 1–3 of earlier classification, starting with phase 1 where the virus is in its animal host and has caused no known infection in humans, phase 2 where zoonosis has occurred and the virus has caused infection in humans, and phase 3 where sporadic cases or clusters of infectious disease occur in humans. Human-to-human transmission is limited in time and space and is insufficient to cause community-level outbreaks.
-
Sustained human–human transmission. Corresponds with the stage 4 of the classical description wherein animal–human and human–human transmissions have sustained a community-level outbreak. The risk for pandemic is greatly increased.
-
Widespread human infection or the stage 5–6 from the classical description where the same identified virus has caused a community-level outbreak in another country in another WHO region.
-
Post-peak period where there exists a possibility of recurrence of infection.
-
Post-pandemic phase when the disease activity is seasonal (https://web.archive.org/web/20110910112007/http://www.who.int/csr/disease/influenza/GIPA3AideMemoire.pdf, https://www.reuters.com/article/uk-china-health-who-idUKKCN20I0PD).
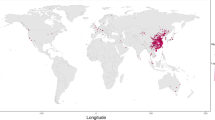
At the time of writing this chapter, coronavirus-2 (CoV-2)/COVID-19, though originated in Wuhan, China, the first case being reported in November 2019, had pervaded Africa, Americas, Europe, South-East Asia, Eastern Mediterranean, and the Western Pacific nations with 191,127 confirmed cases of COVID-19 and claimed 7807 lives, globally (https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200318-sitrep-58-covid-19.pdf?sfvrsn=20876712_2). Europe was declared the new epicenter of the pandemic on March 13, 2020. The number of new cases in China though declining and is believed to be in post-peak stage, the numbers are alarmingly increasing worldwide (https://www.nbcnews.com/health/health-news/europe-now-epicenter-pandemic-who-says-n1158341).
WHO and other leading epidemiology organizations unanimously agree on the indispensable role of pandemic preparation and planning at global and national levels to mitigate through the present public health emergency of COVID-19 and any future outbreaks. Pandemic preparation is not a job of single individual or organization. It requires inputs from each person susceptible to the infection agent as well as policy makers at national and international levels, frontline healthcare providers, infrastructure developers and maintenance personnel, pharmaceutical industry and researcher community, and so forth. Moreover, the pandemic preparedness plan needs constant reviewing and improvisation (https://www.ecdc.europa.eu/en/seasonal-influenza/preparedness/why-pandemic-preparedness). In line with the magnitude of the COVID-19 pandemic, worldwide action plans have been activated on national and international levels. The United Nations’ Strategic Preparedness and Response Plan (SPRS) Against COVID-19, in layman terms, is designed to control human–human transmission, preventing outbreaks and delaying spread; provide optimal care for all patients; and minimize the impact on healthcare systems and socioeconomic activities. Under SPRS each nation is assessed for risk and vulnerability, and the resource requirements to support the country to prepare for and respond to COVID-19 are estimated. Several nations are well placed to implement this action plan with minimal support. However, otherwise partners are to be introduced to facilitate implementation of measures where there is a gap in capacity, on either a national or a subnational level, in additional support to national governments. Thus, an extensive analysis and identification of an affected nation’s gaps and needs shall be the basis to develop a COVID-19 Country Preparedness and Response Plan (CPRP). These CPRPs will need constant monitoring and reviewing using indicators charted in the SPRP and updated as the situation evolves (https://www.who.int/docs/default-source/coronaviruse/covid-19-sprp-unct-guidelines.pdf).
Grossly, the extent of success of each pandemic action plan stands on the following pillars:
-
Surveillance of coronavirus-2 and COVID-19 infection: characterization of the virus, infection modes, diagnosing and detecting infection, contact tracing, annotation of data from confirmed cases, predicting mass infection outbreak, keeping a count, and estimation of mortality.
-
Response management: bulk production and supply of protective/preventive pharmaceutical interventions or non-pharmaceutical interventions.
-
Facilitating timely medical help: access to hospitals/healthcare providers, personal and public hygiene, disinfection, and quarantine services.
-
Lesson learning from the present outbreak of COVID-19 to facilitate future action plans and preparedness.
Hereafter we discuss the present salient strategies under the aegis of the COVID-19 pandemic preparation plan, globally, which are helping the humankind mitigate through this emergency. We also discuss the impact of COVID-19 on world economy and its bearing on future preparedness plans.
14.2 Strategies for Pandemic Preparedness for Coronavirus
14.2.1 Updated Surveillance Systems
As defined by the WHO, surveillance during pandemics is defined as “the ongoing collection, interpretation and dissemination of data to enable the development and implementation of evidence-based interventions during a pandemic event” (https://www.who.int/influenza/preparedness/pandemic/WHO_Guidance_for_surveillance_during_an_influenza_pandemic_082017.pdf). The present-day key worldwide surveillance activities against COVID-19 include:
-
(a)
Detection of coronavirus-2 and verification of COVID-19
-
(b)
Risk and severity assessment
-
(c)
Monitoring the pandemic
The rapidly expanding array of PCR/reverse transcriptase PCR-based diagnostics which are quick and efficient in identifying the virus (Pang et al. 2020; Lake 2020, https://www.finddx.org/covid-19/) are basic requirements for surveillance at every phase of the pandemic for identifying and segregating the infected from non-infected and risk assessment, as well as monitoring recurrences and seasonal disease activity. COVID-19 diagnostics have been discussed previously in this publication.
An emerging exciting field of disease surveillance is infectious disease modeling and incorporation of artificial intelligence. Notably, these are predictive techniques applicable to each of the three facets of disease surveillance (Siettos and Russo 2013). A classical epidemiological surveillance parameter is quantitation of R 0 (R nought, basic reproductive number) using mathematical models (https://wwwnc.cdc.gov/eid/article/25/1/17-1901_article). R 0 is a crucial metric indicating that on average the number of new infection cases are generated by a confirmed infection case, i.e., the potential transmissibility of an infectious disease. R 0 of COVID-19 infection is estimated as 2–3.5 in the early phase, as even the asymptomatic patients or with mild pneumonia extruded large amounts of virus (Wang et al. 2020). Important characteristics of R 0 are:
-
It is a dynamic number and changes with
-
Each stage of the disease
-
With interventions, e.g., vaccination, antivirals
-
Precautionary measures such as personal/community disinfection, social distancing, and travel restrictions
-
-
With the knowledge of R 0, one can predict:
-
New cases expected on a daily basis, and hence facilitate arrangement of healthcare services and interventions locally
-
Outbreak size and the dates of peak infection of the pandemic
-
Probable decline timeline
-
The extent of vaccination coverage required to prevent future outbreaks
-
-
An R 0 > 1 indicates that each infected individual is transmitting the disease to more than 1 new individual, and the infection is spreading increasingly. R 0 = 1 indicates stable transmission and R 0 < 1 indicates the decline in disease transmission (Fig. 14.1). The aim of pandemic action plans is to monitor and depreciate the R 0.
For instance, the median daily R 0 in Wuhan declined from 2.35 a week before the introduction of travel restrictions (January 23, 2020) to 1.05 one week later. The study used a stochastic transmission model of CoV-2 transmission with four datasets from within and outside Wuhan and estimated how transmission in Wuhan varied between December 2019 and February 2020 (Kucharski et al. 2020).
The most prominent mathematical model of COVID-19 infection is the SEIR (Susceptible-Exposed-Infected-Recovered) model put forth by Wu and coworkers and also endorsed by the WHO. This model estimates the size of epidemic in Wuhan between December 2019 and January 2020 and forecasts the extent of domestic and global public health risks of taking into account for social and non-pharmaceutical prevention interventions. It is a compartmental model comprising four compartments and the individuals comprising the sample population move through each compartment—“Susceptible” (not immune to infection) and get infected from other infection individuals and move to the “Exposed” compartment for the incubation period. Hereafter the infectious individuals move to the “Infected” compartment and eventually to the “Recovered” compartment after the disease has run its course, and they now have some immunity (Fig. 14.2). The changes in the population in each compartment are estimated using ordinary differential equations to simulate the progression of an infectious disease. The critical parameters associated with this model are:
-
Force of infection (λ) is the rate at which susceptible individuals are exposed. It depends on the transmission rate (β).
-
Incubation rate (E) is the rate at which exposed people become infectious.
-
Recovery rate (γ) is the rate at which infected individuals recover from the infection.
Through this model, it was predicted that the R 0 was 2.68, each confirmed case infected 2–3 other people, and the epidemic doubling time was 6.4 days. Also, the size of the outbreak in Wuhan was estimated to be up to 75,815 people (statistical uncertainty presented at 95% credible intervals). Most striking feature of this model was that it took into account the travel data from and to Wuhan over the period of study. Thus, it was able to predict that multiple major Chinese cities—Guangzhou, Beijing, Shanghai, and Shenzhen—had already imported the infection to trigger local epidemics. It also recommended that controlling the transmissibility by 25–50% could eventually rein the local epidemics, and a control of ≥63% would phase out the epidemics (Wu et al. 2020).
The application of artificial intelligence (AI) in close conjunction with technology in pandemic surveillance has demonstrated manifold advantages in surveillance activities as exemplified by China and other severely hit nations during the present COVID-19 outbreak. AI, data analytics, and technological support amalgamated to facilitate:
-
Track and forecast community outbreaks:
BlueDot is a Canadian AI company using natural language processing and machine learning algorithms to monitor news outlets, worldwide official healthcare reports in several different languages, and air-travel data and flag the mention of contagious or novel diseases such as coronavirus. Importantly this is followed by scrutiny by epidemiologists and thus also has a component of human analytics. BlueDot alerted its clients to the potential outbreak in Wuhan, China, on December 30, 2019, 9 days prior to the WHO recognized it as an epidemic (https://bluedot.global/products/).
-
Disease diagnosis and verification of infected individuals:
Chest computed tomography (CT) scans have been endorsed as a primary diagnostic tool for COVID-19 (Ai et al. 2020). Ali-baba group’s research academy has developed a deep-learning AI-enabled system that can diagnose COVID-19 in 20 s with 96% accuracy and hence possibly automate the diagnosis activity in the face of overburdened healthcare systems. The AI system identifies an infectious individual based on the chest CT scans. The algorithm has been trained with data and CT scans from nearly 5000 confirmed coronavirus cases from across China. It can be used to track the efficacy of treatment during the course of infection as well as rapidly diagnose COVID-19 (https://www.alizila.com/how-damo-academys-ai-system-detects-coronavirus-cases/).
-
Implementing public hygiene guidelines:
Risk communication in places of potential communication is critical to alert the public and implement mass hygiene measures such as use of sanitizers and face masks when in public places. Google Trends was used in Taiwan to monitor the public risk awareness following the first imported case of COVID-19 which correlated with the increased search keywords “COVID-19” and “face masks.” Moreover, search for “handwashing” increased coinciding with the face mask shortage. High to moderate correlations between Google relative search volume and COVID-19 cases were evident in several major cities of Taiwan (Husnayain et al. 2020). Similarly, in China an AI-based company SenseTime has developed a “Smart AI Epidemic Prevention Solutions”—a quick and effective system based on facial recognition and thermal imaging to screen for individuals with fever in a crowd without physical contact and hence preventing transmission. It can also monitor if any individual is wearing a face mask or violating the quarantine rules (https://www.sensetime.com/en/news/view/id/140.html).
-
Contact tracing:
Health Code, a Chinese government monitoring system, for which users can sign up through Alipay or WeChat, assigns individuals a color code (red—14 days self-quarantine/yellow—7 days self-quarantine/green—free movement) based on their travel history, time spent in outbreak hotspots and exposure to potential carriers of the virus. The software can be used to check the color of an individual on entering their identity numbers.
-
Characterization of the CoV-2 and vaccine/therapy development:
The Genome Detective Coronavirus Typing Tool is a web-based, user-friendly software application that can identify the novel severe acute respiratory syndrome (SARS)-related coronavirus (SARS-CoV-2) sequences isolated in the original outbreak in China and later around the world. The tool accepts 2000 sequences per submission, analyzing them in approximately 1 min. This tool facilitates tracking of new viral mutations as the outbreak expands globally, which may help to accelerate the development of novel diagnostics, drugs, and vaccines to stop the COVID-19 disease (Cleemput et al. 2020).
Google’s AI platform DeepMind-based protein structure prediction tool AlphaFold has predicted and released the 3D structures of several understudied proteins of the CoV-2 as an open source. These can be useful in designing antivirals/vaccines against COVID-19 in future outbreaks (Jumper et al. 2020).
In summary, the new-age pandemic surveillance using AI, data analytics, mathematical modeling of infectious diseases, and risk prediction has significantly contributed to the management of the present COVID-19 pandemic and is laying the foundation for future improvisation of the pandemic action plans.
14.2.2 Strategies for the Implementation of Laboratory Diagnostic Services
Critical issues to be addressed while recruiting laboratory diagnostic services during the novel COVID-19 pandemic are:
-
The authenticity of the diagnostic tool in light of the novelty of the coronavirus-2
-
Bulk of samples to be processed
-
The ease of obtaining the sample for use in the diagnostic tool
The coronavirus causing COVID-19 was first isolated from a clinical sample on January 7, 2020, and within weeks, several reliable and sensitive diagnostic tools were developed and deployed. By mid-January, the first RT-PCR assays for COVID-19 were accessible in Hubei. The viral sequences and PCR primers and probe sequences were open-sourced and uploaded to public platforms by the Centre for Disease Control, China. By February, there were ten kits for the detection of COVID-19 approved in China by the National Medical Products Association—six were RT-PCR kits, one isothermal amplification kit, one virus sequencing product, and two colloidal gold antibody detection kits (https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf). As of today, when the disease has assumed pandemic proportions, the volume of diagnostic tools needs to be multiplied, and hence, the United States Food and Drug Administration (USFDA) has provided regulatory relief to several testing companies like ThermoFisher, Hologic, and LabCorp under the Emergency Use Authorizations, to facilitate ease of diagnosis. Also it is keeping a tight watch on fraudulent companies claiming to sell interventions against COVID-19 (https://www.fda.gov/emergency-preparedness-and-response/mcm-issues/coronavirus-disease-2019-covid-19). Moreover, the world’s first CRISPR (clustered regularly interspaced short palindromic repeats)-based diagnostic kit has been developed for COVID-19 by Mammoth Biosciences, USA, and University of California. Notably, the diagnostic kit is a simple strip-based assay and is easy to use and allows rapid detection without the need of transporting samples over long distances. The kit is still under approval evaluation by the FDA (https://www.medrxiv.org/content/10.1101/2020.03.06.20032334v1).
Nose and mouth swabs, the most widespread samples for CoV-2 diagnostics, require trained personnel to procure samples. However, the study by To and coworkers recommends saliva as an easy-to-procure, noninvasive sample not requiring any trained personnel in COVID-19 screening. They detected CoV-2 in 11 out of 12 patient samples and also could trace the declining titers post-hospitalization (To et al. 2020).
Additionally, a long-term goal of evolving the diagnostics for this novel disease is to develop a prognostic marker of COVID-19. Although it is too soon to say, Qu and coworkers have proposed platelet counts and platelet to lymphocyte ratios as prognostic marker to distinguish between severe and non-severe patients. Severe patients had higher platelet peaking and platelet to lymphocyte ratio correlating with deranged chest CT and longer hospital stays against the lower platelet peaks and platelet to lymphocyte ratios and lesser hospitalization stay (Qu et al. 2020).
14.2.3 Management of Bulk Vaccines and Antiviral Drugs
Vaccines and antiviral drugs are the prophylactic and therapeutic measures against a viral disease CoV-2. On March 17, 2020, Pfizer Inc. and BioNTech announced to co-develop and distribute a potential mRNA-based coronavirus vaccine which is likely to enter clinical testing by the end of April 2020 (https://www.pfizer.com/news/press-release/press-release-detail/pfizer_and_biontech_to_co_develop_potential_covid_19_vaccine). However, in pandemic scenarios of new infectious diseases such as COVID-19, vaccine supplies will be limited or nonexistent at the early phase in lieu of the novelty of the disease and the unpredictability of the pandemic occurrence. Thus, vaccines cannot be stockpiled, and production can only start once the novel virus has been recognized. With the current state-of the-art, the first doses of vaccine are not likely to become available in the early months of the pandemic. However, the pandemic action plans have accounted for forward planning to increase the likelihood that the vaccine will progressively become available as the pandemic unfolds. Importantly, national or regional priorities need to be fixed in the action plan for the rational use of the building/limited supply of the novel vaccine. Also, production and use of vaccines during the inter-pandemic period will influence their availability during a pandemic. Thus, improving the infrastructure and logistics for vaccine production, administration, cold-chain, and professional training with the novel vaccines are important to avert/cruise through future outbreak events. The WHO advisory on prioritizing the population groups are as enlisted in descending order. However, the priorities need tailoring in each country/region according to local needs and epidemiological circumstances.
Recommended prioritizing of the groups is as follows:
-
Healthcare workers and essential service providers
-
Groups at high risk of death and severe complications requiring hospitalization
-
Individuals (adults and children aged more than 6 months) in the community who have chronic cardiovascular, pulmonary, metabolic or renal disease, or are immunocompromised
-
Persons without risk factors for complications (https://www.who.int/csr/resources/publications/influenza/11_29_01_A.pdf)
Antivirals are a crucial adjunct to vaccination as a potential strategy for managing COVID-19. Several drugs such as chloroquine, arbidol, remdesivir, and favipiravir are currently undergoing clinical studies to establish their efficacy and safety against COVID-19. It is important to establish a regular supply chain of antivirals and a high surge capacity in the face of CoV-2 pandemic and future outbreaks. Antivirals have a significant impact in reducing morbidity and mortality in light of unlikelihood of availability of vaccine against in early phases of pandemic. It is important to evaluate the non-interference of the antiviral interventions with the eventual vaccination, as well as the epidemiology of the group of individuals most seriously affected. It is also advisable to make available the information about the performance characteristics, side effects, and costs of antiviral therapy to public. Also the commonly used neuraminidase inhibitors in influenza pandemics are ineffective in the case of CoV-2 mediated infection and outbreaks (Pang et al. 2020; Dong et al. 2020a, https://www.who.int/csr/resources/publications/influenza/11_29_01_A.pdf). The incorporation of antiviral therapy can be categorized as a prophylactic and for treatment use. As with vaccines, prioritizing of groups for antiviral therapy is advised as follows:
-
Essential service providers, including healthcare workers (prophylaxis or treatment). Especially, healthcare providers are in a position to be in direct contact with infectious individuals and are thus entitled to priority antiviral therapy. Other community services such as those responsible for vaccine manufacture and delivery and personnel responsible for enforcing law and order and public safety.
-
Groups at high risk of death and severe complications requiring hospitalization. The goal of prophylaxis or treatment here is to rein the mortality and morbidity. Thus, high-risk persons living in the community outbreaks, seriously ill hospitalized patients, patients for whom a potential CoV-2 vaccination is contraindicated are prioritized.
-
Persons without known risk factors for complications from COVID-19. Here the approach is generally therapeutic and aims to rein the morbidity and rationalize the use of healthcare resources such as antibiotics. Though, the logistics of this strategy are extensive and expensive (requires large quantities of antivirals and access to healthcare service providers), it is most likely to limit the economic and social destabilization associated with a pandemic (Monto 2006; Henry 2019, https://www.who.int/csr/resources/publications/influenza/11_29_01_A.pdf).
A major step in ensuring bulk supplies of antivirals and vaccines is the setting up of medical stockpiles as a part of the pandemic preparedness plans. The USA has constituted a Strategic National Stockpile which is the nation’s largest supply of potentially life-saving pharmaceuticals and medical supplies—antibiotics, chemical antidotes, antitoxins, vaccines, life-support medication, IV administrations, airway maintenance supplies, and other emergency medical and surgical items, for use in a public health emergency severe enough to deplete the local supplies. The facility also houses a data bank of other stockpiles and supply agencies, so that any emergency requirements can be procured in the shortest possible time (https://www.phe.gov/about/sns/Pages/default.aspx).
14.2.4 Promoting facilities for treatment and hospitalization, healthcare personnel, maintenance of hygiene and disinfection during pandemics
Response component of a pandemic action plan constitutes
-
Rapid facilitation of treatment/prophylaxis, hospital centers, quarantine centers
-
Caring for the patients as well as the health service providers to ensure uninterrupted care
-
Communicating awareness about public and personal hygiene and implementing measure to ensure personal and public hygiene
In the face of a highly infectious disease causing novel virus, China has successfully executed an ambitious, swift, and aggressive disease containment effort in the history of mankind. The laudable of its responses to facilitate timely medical care for infected was construction of two dedicated hospitals—1000-bed Huoshenshan facility and the 1600-bed Leishenshan Hospital in 2 weeks (https://www.wsj.com/articles/how-china-can-build-a-coronavirus-hospital-in-10-days-11580397751). Moreover, it ensured coordinated medical supplies, reserve beds were used and relevant premises were repurposed medical care facilities, and prices of commodities were controlled to ensure the smooth operation of the society (https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf).
Ensuring the care of the medical service providers is a key response strategy to warrant efficient care for the general public. Under the China’s response plan, the healthcare workers were facilitated with personal protective equipment. Nosocomial infections accounted were reported to be nearly 2055 from 476 hospitals across China. The majority of this nosocomial infection (88%) were reported from Hubei. A deeper contact tracing indicates infection of the healthcare worker from households than the workplace and were pinpointed to the early stages of the epidemic when understanding of the COVID-19 transmission and medical supplies were limited (https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf). In fact a novel infection control system for averting nosocomial infections of COVID-19 was proposed by Chen and coworkers, titled “the observing system.” Designated personnel called “infection control observers” were appointed by the Department of Infection Control and Nursing in Guangdong Second Provincial General Hospital who underwent training to familiarize infection control requirements in the negative pressure isolation wards. The wards were under camera surveillance and the infection control observer monitors medical staff in real-time via computer monitors outside the ward. The observer ensures normal operation of the negative pressure isolation wards, supervise the implementation of disinfection, ensure a sufficient supply of protective materials, arrange specimens for inspection, and relieve anxiety of the medical personnel while treating patients (Chen et al. 2020).
Personal and public hygiene/disinfection implementation is a key step to control transmission and prevent community outbreaks. Good hand hygiene and respiratory hygiene have been aggressively promoted by WHO worldwide in this COVID-19 pandemic. The basic personal and public hygiene practices are depicted in Fig. 14.3. A key parameter to consider while disinfecting in households and public places hence avoid contact with infected surfaces is the estimation of decay rates of CoV-2 in aerosols and on various materials composing the surfaces. It has been estimated that CoV-2 in an aerosol (<5 μm, similar to those observed in samples obtained from the upper and lower respiratory tract in humans) was viable for up to 3 h, up to 4 h on copper surfaces, up to 24 h on cardboard, and 2–3 days on plastic and stainless steel (van Doremalen et al. 2020). On the basis of these findings, disinfection protocols can be set up for public places/medical facilities depending on the surfaces involved, and even in households’ frequently touched surfaces like door handles, slabs, and tables be disinfected.
14.3 Global Management Strategies for Coronavirus Infection
The exponential transmission of CoV-2—starting with few infectious individuals with COVID-19 quickly increasing manifold in a geographical location within a short time—is a recurring observation (Dong et al. 2020b, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports, https://www.ecdc.europa.eu/en/publications-data/download-todays-data-geographic-distribution-covid-19-cases-worldwide).
Figure 14.4 depicts the exponential surge in new confirmed cases per day plotted against time lapse post outbreak. The highly implemented global COVID-19 management strategies of social distancing, travel restrictions, implementation of personal and public hygiene (non-pharmaceutical interventions), and pursuit of pharmaceutical interventions aim to delay the peaking of the outbreak, avoid burden on the healthcare infrastructure and personnel to ensure quality care for all in need, and rein overall mortality and declined health effects. This phenomenon has been described as “flattening of the curve” and is much shared on social media platforms facilitating awareness in the public (https://www.cdc.gov/flu/pandemic-resources/pdf/community_mitigation-sm.pdf). Hereafter, we discuss the key, successful globally adopted strategies for COVID-19 management.
14.3.1 Social Distancing
It is a non-pharmaceutical infection prevention and control intervention to avoid or control contact between infectious and uninfected individuals to rein the disease transmission in a community eventually culminating into decreased infection spread, morbidity and mortality. The individuals infected with CoV-2 shed the virus from their respiratory tract during the early infection stage when there are minor clinical manifestations leading to the extensive community transmission. While practicing social distancing, each healthy individual behaves like an infected individual, self-restricting contact with others. The main advantage is gleaned when an individual in incubation period/early infectious stage of COVID-19 restricts coming in contact with other healthy individuals. This strategy involves the policymakers, and strict advisories/orders are issued under the pandemic action plan to restrict public gatherings and events, shutting down of educational institutes/offices/restaurants, avoiding nonessential travel and use of public transport, maintaining a distance of 1 m at least between two individuals, restricting visit to hospitals, and avoiding online shopping. Additionally, the elderly and individuals with hypertension, cardiovascular disease, diabetes, chronic respiratory diseases, and cancer are at a higher mortality risk (https://www.mohfw.gov.in/SocialDistancingAdvisorybyMOHFW.pdf, https://onlinelibrary.wiley.com/doi/pdf/10.1111/ijcp.13501; Zou et al. 2020).
14.3.2 Extensive Testing, Case Isolation, and Contact Tracing
The WHO Director-General at a media briefing on COVID-19 on March 16, 2020, recommends testing of any suspected case, isolation to break the chain of transmission, and contact tracing for the prior 2 days the subject came in contact with and then testing them as well (https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19%2D%2D-16-march-2020). A case in point—South Korea carried out 286,716 COVID-19 tests until March 17, 2020—second highest across the world trailing behind China (https://ourworldindata.org/coronavirus-testing-source-data), combined with strict social distancing implementation and is now seeing a fall in the number of COVID-19 cases (https://ourworldindata.org/grapher/daily-cases-covid-19-who?time=1..52&country=KOR, https://www.sciencemag.org/news/2020/03/coronavirus-cases-have-dropped-sharply-south-korea-whats-secret-its-success). Social distancing combined with case isolation and contact tracing has demonstrated its effectiveness in controlling the transmission from imported infection cases to the community transmission scenario (Wilder-Smith and Freedman 2020). The relevance of case isolation and contact tracing are highlighted in a study by Hu and coworkers where they have performed a clinical characterization of 24 asymptomatic patients—confirming infection by a laboratory-confirmed positive for the COVID-19 virus nucleic acid from pharyngeal swab samples. The asymptomatic cases did not present any obvious symptoms while nucleic acid screening. About 20.8% developed classical symptoms of fever, cough, and fatigue, during hospitalization; 50.0% presented CT images of ground-glass chest and 20.8% presented stripe shadowing in the lungs; 29.2% cases presented normal CT image and had no symptoms during hospitalization, comprising the younger subset (median age: 14.0 years). None developed severe COVID-19 pneumonia, and no mortality was observed. However, epidemiological investigation indicated at typical asymptomatic transmission to the cohabiting family members, which even caused severe COVID-19 pneumonia. This study puts a spotlight on close contact tracing and longitudinally surveillance via virus nucleic acid tests. Case isolation and continuous nucleic acid tests are also recommended (Hu et al. 2020). De-isolating of suspect cases where the first confirmatory test has returned negative is also an emerging issue of concern and needs improvement in testing capacity as well as strict implementation of social distancing during pandemic scenarios (Tay et al. 2020).
14.3.3 Travel Restrictions
Approaching January 13, 2020, the daily risk of exporting at least a one COVID-19 infected individual from mainland China through international travel exceeded 95%. For containment of the global spread of CoV-2 and a COVID-19 epidemic, China implemented border control measures—airport screening and travel restrictions, and were later also adopted by several other countries. Wells and coworkers in their study in Proceedings of Natural Academy of Sciences used daily incidence data of COVID-19 outbreak from China from December 8, 2019, to February 15, 2020, as well as airline network data, to predict the number of exported cases with and without measures of travel restriction and screening. The group put forth that the lockdown of Wuhan and 15 more cities in Hubei province on January 23–24, 2020, averted export of 779 more COVID-19 cases by mid-February. However, it is to be highlighted that these travel restrictions and lockdown measures only slowed the rate of infection exportation from China to other countries. The global spread of COVID-19 was based on most cases arriving during the asymptomatic incubation period. The authors recommend rapid contact tracing at the epicenter and at importation sites to limit human-to-human transmission outside of the location of first outbreak (Wells et al. 2020).
14.3.4 Foiling Myths to Control Mass Hysteria
The COVID-19 pandemic in today’s times of excessive electronic connectivity and several social media platforms has a potential to alleviate the global mental stress levels. Especially, if local myths and rumors are circulated in the already home-quarantined population, restriction in fear of the disease can lead to additional mass hysteria. Thus it is important to create awareness and dispel any negative myth, as put forth by the WHO in context of CoV-2 (https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters). Some myths dispelled are:
-
COVID-19 virus can be transmitted in areas with hot and humid climates or cold and snowy climates. CoV-2 can be transmitted in all areas.
-
Hot bath cannot prevent CoV-2 transmission.
-
CoV-2 is not transmitted by mosquito bites. It is a respiratory illness and respiratory hygiene is a key protective strategy.
-
Heat generated from hand dryers is not effective against killing CoV-2 on your hands. The only way to disinfect hands is washing with soap-water or alcohol-based sanitizers.
-
Thermal scanners are effective in detecting only the elevated body temperatures. A confirmatory nucleic acid test is the most guaranteed test.
-
All age groups can be infected by CoV-2. Elderly people and people with pre-existing medical conditions—asthma, diabetes, cardiovascular disease— are more vulnerable to exhibit severe COVID-19. Thus, WHO advises people from all age groups to protect themselves by implementing good hand hygiene and respiratory hygiene.
-
SARS-CoV-2 is not a bioengineered organism arising out of manipulations from earlier SARS-CoV. Andersen and coworkers have analyzed the genome sequence of the novel coronavirus-2 and compared it with several other zoonotic viruses. They claim that the viral–human point of contact—the high affinity receptor binding domain of CoV-2 binding with the angiotensin-converting enzyme 2 (ACE2) of the target host—is acquired through natural selection. Also they have shed light of probable animal host being Rhinolophus affinis, as another virus RaTG13, sampled from a bat, is ~96% identical overall to CoV-2 (https://www.nature.com/articles/s41591-020-0820-9).
14.4 Economic Consequences of Pandemic Risk
The COVID-19 pandemic can cause short-term fiscal distress and longer-term damage to the global economic growth. If we trace the economic trajectory of a pandemic:
-
Early phase measures to contain/limit outbreak—shutting down of workplaces and public businesses, mobilization of healthcare supplies and surveillance activities, contact tracing, social distancing by isolation of contacts/quarantines incur significant human resource and staffing costs (Achonu et al. 2005).
-
As the scale of the epidemic expands, new medical infrastructure will need to be constructed to manage building number of confirmed infected individuals, the surge in demand for medical consumables can increase the health system expenditures (Herstein et al. 2016).
-
The quarantine and lockdown impositions disrupt trans-national supply chains, transportation industry, agriculture, entertainment, and travel industry. Hoarding and black marketing of essential and medical commodities are expected.
-
Behavioral changes during pandemic—avoiding association with other people to avoid infection—are the major determinant for economic impact of pandemics (Fig. 14.5) and not mortality. The behavioral change fear driven which in turn is driven by awareness and ignorance (Burns et al. 2008).
-
National and international relief funds have been constituted to mitigate the world through the COVID-19 pandemic. For example, the SPRP estimates a funding support of nearly US$675 million for key response efforts against COVID-19 in countries most in need of help through April 2020. A first-of-its-kind COVID-19 Solidarity Response Fund was constituted for arranging for funding support through individual and organizational donations on March 13, 2020. The COVID-19 Solidarity Response Fund is hosted by two foundations, the UN Foundation (registered in the United States) and the Swiss Philanthropy Foundation (registered in Switzerland) in association with the WHO (https://www.who.int/emergencies/diseases/novel-coronavirus-2019/donate).
-
Increased fiscal distress due to decrease in tax revenues and increased expenditures are expected in low middle-income countries, where fiscal framework is weak. This situation aroused earlier in West Africa Ebola epidemic in Liberia: response costs surged, economic activity slowed, and quarantines and curfews compromised government capacity to collect revenue (https://www.worldbank.org/content/dam/Worldbank/document/HDN/Health/WDR14_bp_Pandemic_Risk_Jonas.pdf).
-
The high-income countries in scenario of a moderate pandemic can offset fiscal distress by providing official development assistance to affected countries and budgetary support. However, during a severe pandemic, a high-income country will also confront the same fiscal stresses and may be unwilling to provide assistance.
Pandemic outcomes leading to economic impact. During pandemics, economic disturbances are an outcome of averting public contact/fear to avoid infections, absent from workplace due to illness, and mortality (https://www.worldbank.org/content/dam/Worldbank/document/HDN/Health/WDR14_bp_Pandemic_Risk_Jonas.pdf)
14.5 Conclusions and Future Perspectives
On March 19, 2020, worldwide 191,127 confirmed cases were reported, mortality was 7807 against 118,319 confirmed cases, and mortality of 280 on March 13, 2020 when the COVID-19 crisis was declared a pandemic (https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports). It is increasingly becoming evident that no region of the world will remain untouched by CoV-2 invasion. However, pandemic preparedness is the key to tackle the present-day COVID-19 health emergency worldwide. The rapid and effective enforcement of existing international and national action plans, as well as parallel review and improvisation, is facilitating the affected countries to contain transmission and possibly delay the peak of outbreak and mortality and garner recovery. It is notable that in the present pandemic scenario, innovative AI-powered surveillance, quick and strategic response actions—the trinity of testing-isolation-contact tracing, committed social distancing measures—travel restrictions, self-isolation, implementation of personal and public hygiene, and extensive mobilization of medical care facilities are helping the world mitigate through. The most insightful trend emerging from the global clinical and epidemiological data is that the identification of asymptomatic infected individuals is a crucial step to contain community outbreaks. For preventing future outbreaks of CoV-2 infection, high-volume cutting-edge investigations are warranted in understanding the COVID-19 pathology, CoV-2 origin, biology, structural data of potential surface antigens, and precise anti-CoV-2 antiviral therapies. Although the global economy is suffering at the hands of CoV-2, it is important to review the current action plans and suitably improvise the future action plans to avoid potential recurrence.
Executive Summary
Pandemics are unforeseen. National and international preparedness are crucial to tackle a pandemic. World over, humanity is grappling with COVID-19. The pandemic preparedness charter prescribed by international and national agencies to tackle COVID-19 is evolving on the go. The key facets of pandemic preparedness emerging from global success and failure scenarios are:
-
Active surveillance employing state-of-the art technology:
-
Development of mathematical models for simulating the infection of CoV-2 in a given country. The models can help predict the basic reproductive number which in turn facilitates monitoring the pandemic on day-to-day basis.
-
Incorporation of contactless artificial intelligence-based technologies for mass thermal screening, track and forecast community outbreaks, implement public hygiene and use of masks, and contact tracing.
-
-
Expanding the diagnose capacity/testing for CoV-2 (the infectious agent) to catch any asymptomatic carriers, but at the same time ensuring:
-
Precision of the test.
-
Test is adaptable to processing bulk samples.
-
Easy procurement of sample from suspected infected individuals.
-
-
Management of bulk antiviral interventions and vaccines:
-
National or regional priorities need to be fixed for rational use of antiviral/emerging vaccines
-
Prioritizing the population has been recommended: the healthcare workers and essential service providers are top priority.
-
Medical stockpiles should be established.
-
-
Promoting facilities for healthcare/healthcare workers and facilitating public disinfection and hygiene via:
-
Rapid expansion of hospitalization facilities for treatment and isolation/quarantine centers.
-
Ensuring minimal nosocomial infections to the healthcare workers.
-
Issuing and implementation of guidelines for ensuring good hand and respiratory hygiene.
-
Public disinfection (and personal household as well) based on the established life of CoV-2 on different surfaces.
-
-
Globally successful strategies are:
-
Social distancing and lockdowns to ensure minimal human–human contact.
-
Travel restrictions to facilitate containment.
-
Trifecta of test–isolate–contact tracing.
-
-
The economic cost of the COVID-19 pandemic management is expanding due to:
-
Disruption of economic activities due to implementation of social distancing via lockdowns.
-
Battling the diseased and the increasing mortality.
-
Diversion of resources to expansion of healthcare systems.
-
International and national relief funds are being constituted.
-
Fiscal reliefs and aid from developed nations to the developing or under-developed countries can release the surmounting economic pressure.
-
Abbreviations
- ACE2:
-
Angiotensin-converting enzyme 2
- AI:
-
Artificial intelligence
- CoV-2:
-
Coronavirus-2
- COVID-19:
-
Corona viral disease-2019
- CPRP:
-
COVID-19 Country Preparedness and Response Plan
- CRISPR:
-
Clustered regularly interspaced short palindromic repeats
- MERS:
-
Middle East respiratory syndrome
- SARS:
-
Severe acute respiratory syndrome
- SPRS:
-
Strategic preparedness and response plan
- USFDA:
-
United States Food and Drug Administration
- WHO:
-
World Health Organization
References
Achonu C, Laporte A, Gardam MA (2005) The financial impact of controlling a respiratory virus outbreak in a teaching hospital: lessons learned from SARS. Can J Public Health 96(1):52–54
Ahmed S, Dávila JD, Allen A, Haklay MM, Tacoli C, Fèvre EM (2019) Does urbanization make emergence of zoonosis more likely? Evidence, myths and gaps. Environ Urban 31(2):443–460. https://doi.org/10.1177/0956247819866124
Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L (2020) Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 26:200642. https://doi.org/10.1148/radiol.2020200642
Burns A, van der Mensbrugghe D, Timmer H (2008) Evaluating the economic consequences of avian influenza. World Bank, Washington, DC
Chen X, Tian J, Li G, Li G (2020. pii:S1473-3099(20)30110-9) Initiation of a new infection control system for the COVID-19 outbreak. Lancet Infect Dis. https://doi.org/10.1016/S1473-3099(20)30110-9
Cleemput S, Dumon W, Fonseca V, Karim WA, Giovanetti M, Alcantara LC, Deforche K, de Oliveira T (2020. pii: btaa145) Genome Detective Coronavirus Typing Tool for rapid identification and characterization of novel coronavirus genomes. Bioinformatics. https://doi.org/10.1093/bioinformatics/btaa145
Dong L, Hu S, Gao J (2020a) Discovering drugs to treat coronavirus disease 2019 (COVID-19). Drug Discov Ther 14(1):58–60. https://doi.org/10.5582/ddt.2020.01012
Dong E, Du H, Gardner L (2020b. pii: S1473-3099(20)30120-1) An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. https://doi.org/10.1016/S1473-3099(20)30120-1
van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ (2020) Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. https://doi.org/10.1056/NEJMc2004973
Henry B (2019) Canadian pandemic influenza preparedness: antiviral strategy. Can Commun Dis Rep 45(1):38–43. https://doi.org/10.14745/ccdr.v45i01a05
Herstein JJ, Biddinger PD, Kraft CS, Saiman L, Gibbs SG, Smith PW, Hewlett AL, Lowe JJ (2016) Initial costs of Ebola treatment centers in the United States. Emerg Infect Dis 22(2):350–352. https://doi.org/10.3201/eid2202.151431
Hu Z, Song C, Xu C, Jin G, Chen Y, Xu X, Ma H, Chen W, Lin Y, Zheng Y, Wang J, Hu Z, Yi Y, Shen H (2020) Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. https://doi.org/10.1007/s11427-020-1661-4
Husnayain A, Fuad A, Su EC (2020. pii: S1201-9712(20)30140-5) Applications of google search trends for risk communication in infectious disease management: a case study of COVID-19 outbreak in Taiwan. Int J Infect Dis. https://doi.org/10.1016/j.ijid.2020.03.021
Jumper J, Tunyasuvunakool K, Kohli P, Hassabis D, The AlphaFold Team (2020) Computational predictions of protein structures associated with COVID-19. DeepMind website. https://deepmind.com/research/open-source/computational-predictions-of-protein-structures-associated-with-COVID-19
Kucharski AJ, Russell TW, Diamond C, Liu Y, Edmunds J, Funk S, Eggo RM. Centre for Mathematical Modelling of Infectious Diseases COVID-19 Working Group(2020. pii: S1473-3099(20)30144-4) Early dynamics of transmission and control of COVID-19: a mathematical modelling study. Lancet Infect Dis. https://doi.org/10.1016/S1473-3099(20)30144-4
Lake MA (2020) What we know so far: COVID-19 current clinical knowledge and research. Clin Med (Lond) 20(2):124–127.. pii: clinmed.2019-coron. https://doi.org/10.7861/clinmed.2019-coron
Madhav N, Oppenheim B, Gallivan M, Mulembakani P, Rubin E, Wolfe N (2017) Chapter 17: Pandemics: risks, impacts, and mitigation. In: Jamison DT, Gelband H, Horton S, Jha P, Laxminarayan R, Mock CN, Nugent R (eds) Disease control priorities: improving health and reducing poverty, 3rd edn. The International Bank for Reconstruction and Development/The World Bank, Washington, DC
Monto AS (2006 Jan) Vaccines and antiviral drugs in pandemic preparedness. Emerg Infect Dis 12(1):55–60
Pang J, Wang MX, Ang IYH, Tan SHX, Lewis RF, Chen JI, Gutierrez RA, Gwee SXW, Chua PEY, Yang Q, Ng XY, Yap RK, Tan HY, Teo YY, Tan CC, Cook AR, Yap JC, Hsu LY (2020) Potential rapid diagnostics, vaccine and therapeutics for 2019 novel coronavirus (2019-nCoV): a systematic review. J Clin Med 9(3). pii: E623. https://doi.org/10.3390/jcm9030623
Qu R, Ling Y, Zhang YH, Wei LY, Chen X, Li X, Liu XY, Liu HM, Guo Z, Ren H, Wang Q (2020) Platelet-to-lymphocyte ratio is associated with prognosis in patients with Corona Virus Disease-19. J Med Virol. https://doi.org/10.1002/jmv.25767
Siettos CI, Russo L (2013) Mathematical modeling of infectious disease dynamics. Virulence 4(4):295–306. https://doi.org/10.4161/viru.24041
Tay JY, Lim PL, Marimuthu K, Sadarangani SP, Ling LM, Ang BSP, Chan M, Leo YS, Vasoo S (2020. pii: ciaa179) De-isolating COVID-19 suspect cases: a continuing challenge. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa179
To KK, Tsang OT, Chik-Yan Yip C, Chan KH, Wu TC, Chan JMC, Leung WS, Chik TS, Choi CY, Kandamby DH, Lung DC, Tam AR, Poon RW, Fung AY, Hung IF, Cheng VC, Chan JF, Yuen KY (2020. pii: ciaa149) Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa149
Wang Y, Wang Y, Chen Y, Qin Q (2020) Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. https://doi.org/10.1002/jmv.25748
Wells CR, Sah P, Moghadas SM, Pandey A, Shoukat A, Wang Y, Wang Z, Meyers LA, Singer BH, Galvani AP (2020. pii: 202002616) Impact of international travel and border control measureson the global spread of the novel 2019 coronavirus outbreak. Proc Natl Acad Sci U S A. https://doi.org/10.1073/pnas.2002616117
Wilder-Smith A, Freedman DO (2020) Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med 27(2). https://doi.org/10.1093/jtm/taaa020
Wu JT, Leung K, Leung GM (2020) Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet 395(10225):689–697. https://doi.org/10.1016/S0140-6736(20)30260-9. Erratum in: Lancet. 2020 Feb 4
Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, Yu J, Kang M, Song Y, Xia J, Guo Q, Song T, He J, Yen HL, Peiris M, Wu J (2020) SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. https://doi.org/10.1056/NEJMc2001737
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 The Editor(s) (if applicable) and The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Chawla, S., Saxena, S.K. (2020). Preparing for the Perpetual Challenges of Pandemics of Coronavirus Infections with Special Focus on SARS-CoV-2. In: Saxena, S. (eds) Coronavirus Disease 2019 (COVID-19). Medical Virology: From Pathogenesis to Disease Control. Springer, Singapore. https://doi.org/10.1007/978-981-15-4814-7_14
Download citation
DOI: https://doi.org/10.1007/978-981-15-4814-7_14
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-4813-0
Online ISBN: 978-981-15-4814-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)