Abstract
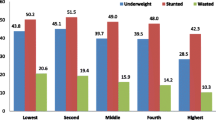
Malnutrition is an important health issue in people of all ages. For children, it is a risk for hindering normal growth and development, and in pregnancy it affects both mother and child, leading to low birth weight. In old age, malnutrition is a risk leading to the need for care, or endangers life through a person becoming bedridden or affected with pneumonia (Fig. 13.1) [1]. To maintain a proper state of nutrition, required nutrients must be eaten, and obtaining food is the first step. Food intake and malnutrition are affected by income and household economy. In the results of studies in infants and children not only in developing countries in Africa and Asia but also in developed countries in Europe and America, it has been reported that there is more malnutrition in children of parents in lower-income strata than higher-income strata [1]. For example, in a 2010 survey in Iran, a clear relationship was observed between socioeconomic status (SES) and stunting as a result of malnutrition, with a stunting frequency of 17.4% in children under 5 years in the poorest socioeconomic quintile compared to 6.4% in the richest [2].
Miyo Nakade is also the English translator for this chapter.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
1 Introduction
Malnutrition is an important health issue in people of all ages. For children, it is a risk for hindering normal growth and development, and in pregnancy it affects both mother and child, leading to low birth weight. In old age, malnutrition is a risk leading to the need for care, or endangers life through a person becoming bedridden or affected with pneumonia (Fig. 13.1) [1]. To maintain a proper state of nutrition, required nutrients must be eaten, and obtaining food is the first step. Food intake and malnutrition are affected by income and household economy. In the results of studies in infants and children not only in developing countries in Africa and Asia but also in developed countries in Europe and America, it has been reported that there is more malnutrition in children of parents in lower-income strata than higher-income strata [1]. For example, in a 2010 survey in Iran, a clear relationship was observed between socioeconomic status (SES) and stunting as a result of malnutrition, with a stunting frequency of 17.4% in children under 5 years in the poorest socioeconomic quintile compared to 6.4% in the richest [2].
In this chapter, we provide an overview of the problem of malnutrition inside and outside Japan, and then, narrowing our focus to community-dwelling older persons, we introduce findings that demonstrate the association between malnutrition and social determining factors of health, primarily SES components such as income and years of education. Finally, we discuss the future direction of measures to combat malnutrition.
2 The Problem of Malnutrition Inside and Outside Japan
Looking at the global situation, it was indicated in a World Health Organization report on integrating poverty and gender into health programs [1] that underweight young women remained underweight even as they aged and that growth of their children after birth was poor. In South Asia, a relationship between short stature in childhood and incidence of chronic disease in adulthood was reported. A 2017 report [3] by the Food and Agricultural Organization of the United Nations on food security and nutrition found that the number of malnourished people in the world was estimated to be 815 million in 2016, following a global rise in malnutrition from 2014. Africa has the highest prevalence of malnutrition in the world, with an average of 20% compared with the global average of 11%. Asia has the highest absolute number of undernourished people in the world, owing to population size [3].
For children, the global rate of stunting decreased from 29.5% in 2005 to 22.9% in 2016. However, there are still 155 million children under 5 years across the globe who suffer from stunting. In 2016, 52 million children under 5 years were affected by wasting, with around 27.6 million of that number living in southern Asia [4].
To summarize the worldwide state of nutrition, malnutrition is a health problem that is widespread in children in households of low social class in both developing countries and in developed countries. As described above, it is known that malnutrition is seen more widely in low-income strata, but that does not mean that material deprivation (poverty) alone brings about poor health such as malnutrition [5]. An association between years of education and nutritional state has also been reported [1], and this is thought to be caused by the kind of diet provided to children depending on parental knowledge about nutrition and health, differences in hygiene, and differences in health services that are utilized. In a study on stunting and trends toward being underweight or overweight in Indonesian children aged 2.0–4.9 years, it was found that a mother’s lack of formal education was closely associated with stunting and being underweight [6].
In Japan, for younger people, being underweight especially amongst women is a public health problem. According to the results of the 2016 National Health and Nutrition Survey in Japan [7], the proportion of people considered underweight [body mass index (BMI) < 18.5 kg/m2] stands at 4.4% for men, and 11.6% for women, with a significant increase in the percentage of underweight women over the past decade. The number of young women in their twenties considered underweight is 20.7%. For this reason, “Health Japan 21” [8] (a national health initiative) has specified a target value to reduce the number of underweight women in their twenties. It is considered that among underweight young Japanese women, a desire to be thin or excessive concern with body image are the main causes of being underweight [9], which is a different modality from the worldwide situation of being underweight described above (malnutrition because of low SES).
In middle-aged and older persons, there are people who are obese because of metabolic syndrome and require correction of high nutrition, while there are also people who are malnourished or at risk of malnutrition. According to a survey conducted in 2016, the percentage of obese people over 20 years of age (BMI ≧ 25 kg/m2) was 31.3% for men and 20.6% for women. These figures have remained relatively unchanged over the past decade. However, the percentage of older people aged over 65 years at risk of malnutrition (BMI ≦ 20 kg/m2) is 12.8% for men and 22.0% for women, of which the percentage for women has increased over the past decade [7]. To combat this problem among older people, “nutrition improvement” has been positioned as a key issue in preventative care measures, with a “nutrition improvement program” implemented to address issues associated with malnutrition and to target people at risk of malnutrition.
As summarized above, malnutrition has been very widely studied, from developing countries to developed countries and from childhood to old age. Next, we review the literature while narrowing our focus to community-dwelling older people as primary subjects.
3 Malnutrition in Older People (Determination of Nutritional State)
The most critical nutritional problem in older people is improvement of protein-energy malnutrition (PEM). PEM is a cause of disease in older people and is closely associated with an increased nursing care requirement level. The state of PEM and its causes must be understood, and improvement and prevention measures taken as early as possible.
In preventive care nutrition improvement programs in Japan, a person’s state of nutrition is assessed according to nutrition risk level, using indices such as the rate of weight loss, BMI, serum albumin level, food intake quantity, nutrition supply method, the presence of bedsores, and others. In older people, those with a serum albumin level of 3.5 g/dL or less in a basic health exam, or those who have lost 2–3 kg of weight in 6 months and are extremely thin with a BMI less than 18.5 kg/m2 on a basic checklist (checking performance of 25 vital functions), are determined to be at risk of malnutrition. Because there are people who maintain a healthy state even with a BMI less than 18.5 kg/m2, if such people have also lost weight they are judged as being at risk of malnutrition [10].
In an international comparison of malnutrition in older people, Kuzuya [11] cited the definition of malnutrition as a reason that there are almost no reports comparing rates of malnutrition in older people. BMI is used throughout the world, but it is only an indicator of physique and not necessarily an indicator of malnutrition. Furthermore, BMI is greatly influenced by differences in physical function and cognitive function in older people (regardless of whether reduction of these functions is included in the object of research) and class differences such as wealth or poverty. As a tool for assessing nutritional state, the mini nutritional assessment (MNA) has been used in various European countries as well as in Asian countries as a comprehensive method for nutrition assessment of older people [12, 13]. MNA is made up of 18 items in four categories: (1) physical measurements, (2) general state (ambulatory capacity, number of medicines taken, etc.), (3) dietary situation, and (4) self-assessment of nutritional state and state of health. First, 6 of the 18 items (total of 14 points) are evaluated as a screening step, and a score of 12 points or higher is considered normal. For subjects scoring 11 points or lower, the remaining 12 items are evaluated, and the nutritional state is determined based on the total score, where 30 points is a perfect score (24 points or more, good nutritional state; 17–23.5 points, at risk of malnutrition; less than 17 points, poor nutrition) [14, 15].
A variety of factors are associated with malnutrition in older people, including physical, psychological, environmental, and social factors such as chronic disease, missing teeth that directly affect food intake, poorly fitting dentures, reduced level of activity, taking medicine, psychological states such as depression, difficulty in buying food (no stores nearby, difficulty in shopping on foot), and lack of cooking skills and knowledge [10].
4 Association of SES and Older People’s Malnutrition and Food Intake Situation
4.1 SES and Nutritional State Assessment Using MNA
For studies in countries other than Japan that used MNA for nutritional assessment of community-dwelling older people, differences that were attributed to individual SES were seen in numerous reports [16,17,18,19,20,21].
For example, in Japan, when 130 healthy, community-dwelling older people attending a senior university were screened for malnutrition using MNA, 12.6% of participants were at risk of malnutrition, and many were in the poor economic status strata [16]. It has also been reported that many at risk of malnutrition (weight loss of at least 3 kg in 6 months) are in the strata of limited education and low income, and that more live in agricultural regions than in metropolitan areas [17]. In regard to extensive tooth loss as a cause of malnutrition, Aida et al. [18] reported that the odds ratio of people 65 years and older having 19 or fewer remaining teeth was 1.4 times higher in people with 9 or fewer years of education than those with 13 or more years, even after adjustment for age, gender, income, health behavior, smoking habit, and so forth.
In an MNA-SF (Mini Nutritional Assessment short form) survey of 698 community-dwelling older people in Italy, an association was found between low education levels, low economic status, and malnutrition [19], while a different survey reported a relationship between malnutrition and factors such as low income, distance from supermarkets, and lack of transport [20].
The prevalence rate is also higher when the degree of development of a country is lower. In a report from Bangladesh on 457 people aged 60 years and older who were not receiving nursing care services, an association was demonstrated between high degree of education or high level of household consumption and high MNA score (good nutritional state) even after adjustment for age and state of health [21]. In that survey, the prevalence rate of malnutrition was a high 62%, and it was shown that people with depression or low cognitive function had a poor nutritional state, as well as uneducated people and women with no income or irregular financial assistance [22].
In a survey of 1200 older people in Lebanon, it was found that while 8% of men were at risk of malnutrition, the percentage for women was much higher at 29.1%, with lower rates of literacy and income as well as high frequency of depression in women rather than men [23].
4.2 Association Between Individual SES and Quality of Food Consumed
A large-scale cohort survey conducted in Europe found that men in particular of lower income status and socioeconomic class consumed fewer different fruits or vegetables [24]. A similar survey in England found that older men with low SES had a poor-quality diet. Married men had higher diet quality than men living alone, with diet quality in older men also adversely influenced by factors such as SES (including manual social class of parents) in childhood [25].
In a review of epidemiological data, Darmon and Drewnowski [26] found that persons of higher SES tended to consume whole grains, fish, low-fat dairy products, and fresh fruit and vegetables, while consumption of refined grains and added fats is associated with persons of lower SES. However, it has been shown that while some European countries have comparatively lower SES than America, consumption of fruit and vegetables is not adversely affected. A relationship has also been identified between children’s food consumption and their parents’ level of education, where a lower level of schooling resulted in less fruit and vegetables, and more sugary beverages being consumed by the children of such parents [26].
In Japan, large-scale studies have shown that in recent years an individual’s SES has an influence on general health, meals, and dietary environment. The National Health and Nutrition Survey of Japan showed a direct correlation between household income and fat intake, while there was an inverse correlation with carbohydrate intake. Women with low education levels and household income were likely to be overweight or obese, but for men, there was no direct correlation between lower education level and rate of obesity [27, 28].
In a Japan Gerontological Evaluation Study (JAGES) of 100,000 participants, men with 19 teeth or less were found to be 1.5 times more at risk of being underweight, while women under the same conditions that did not consume fruit and vegetables on a daily basis had a 1.2 times higher risk of being underweight [29]. It was found that risk of death with a BMI of 18.5 kg/m2 or under increased, while obese males of low SES were also at a higher risk of dying [30]. In a 3-year study conducted by Tani et al. [31], older people with lower SES in childhood were 1.27 times more likely to develop depression as adults than those with a higher childhood SES. Moreover, men who ate meals alone had a higher risk of developing depression, higher risk of death, and even men who lived with family had a higher risk of death if eating alone [32, 33]. From these reports, it is seen that the SES of an individual is related in no small measure to quality and quantity of food consumed, and affects an individual’s state of health not only through malnutrition, but through obesity, improper nutrition intake, and so forth.
4.3 Association Between Community SES and Individual Food Intake
Several reports have stated that not only is an individual’s SES associated with his or her food intake, but also the socioeconomic environment of the community in which the individual lives [34,35,36]. For example, in a study of women living in 3204 communities in 26 states of India, a multilevel analysis by dividing the communities into wealthy, moderate, and poor communities found that community wealth was associated with BMI after adjusting for individual factors [34]. Furthermore, when adjusted for individual SES including household wealth (work, education, etc.), BMI was 0.29 kg/m2 higher in the wealthiest communities than in the poorest communities [34]. From the results of a survey of Cambodian women, Hong and Hong [36] demonstrated that the nutritional state of women was lower in low-SES communities and that differences were large depending on the community, even after adjustment for individual household economy level by multilevel analysis. In a different survey from 2010 of 4000 older people in Japan, after adjustment for individual factors were made, a relationship was reported between community income levels and the number of remaining teeth [37].
In a report on a large-scale survey in people aged 65 years and older based on the 2000 USA census [38], the death rate due to malnutrition was extracted by tracking the data of 190,000 households in 3141 counties over 4 years. The death rate was significantly higher in the lower education level strata, and even when adjusted for that, it was shown that social, physical, and social isolation factors are involved in regional patterns of death based on malnutrition in older people. As an example of the traditional diet of a community being related to SES, in a study in residents of the eastern Mediterranean islands of Greece (eight islands) aged 65–100 years [39], an association was seen between consumption of a Mediterranean diet (using a Mediterranean diet score) and education or financial status. The results indicated that people of the highest SES level more often consumed a traditional diet (i.e., fish, vegetables, wine, etc.) than people of other levels.
In a seven-country comparative study of SES and variances in fruit and vegetable consumption, an association was found between neighborhood-level SES and fruit consumption in Canada, New Zealand, and Scotland. In Australia, Canada, New Zealand, and Portugal, those residing in higher SES neighborhoods had an increased chance of greater vegetable intake [40].
Regarding community influences on diet, access or proximity to certain food stores such as supermarkets has been used as a normalizing factor of obesity and eating behavior [41]. For example, Zenk et al. [42] reported that women who shopped at supermarkets or specialty stores consumed fruit and vegetables more than people who shopped at grocery stores that were not specialty stores. There are also reports demonstrating the association between fast food and obesity [43, 44]. In the results of a study in 65 Los Angeles communities with a large low-income population, it was reported that BMI was high in communities with a large number of restaurants and fast food places, even after adjustment for individual factors and community SES [43].
In Japan, communities in which it is difficult to find inexpensive, good-quality perishable food in city centers and changes in community shops threaten to affect the health of residents living there. This situation has been called the food desert problem [45,46,47]. As smaller food stores disappear from communities, older people become disadvantaged, consuming less variety of foods and at higher risk of not consuming enough meat, fish, fruit, and vegetables. These factors were particularly pronounced in older men with low levels of neighborhood contact [48]. It is clear that community-dwelling SES, geographical factors, and lack of social contact with neighbors is linked to malnutrition.
5 Future Direction of Measures Against Malnutrition
Considering the association between malnutrition and social determining factors of health described above, we draw attention to four points regarding the future direction of measures against malnutrition.
First is the importance of a population-wide strategy. Although Japan has a “nutrition improvement” program in place as part of the country’s preventive care policy, the small number of program participants or people qualifying as at risk for malnutrition and the contents of the program have been pointed out as issues. The reasons cited include: many participants are healthy people with no nutritional problems; it is difficult to attract malnourished people who want to participate in a nutrition improvement program; information about nutrition is difficult for subjects to understand; and the albumin level of people who were anticipated to be malnourished was not low. Older people are inevitably at risk of malnutrition sooner or later. It is therefore important to take the view that malnutrition in older people is not just a problem for the people who participate in nutrition programs, but is a topic of preventive care in all community-dwelling older people, and a population-wide strategy must be established.
Second is the importance of perspective on the disparity among socioeconomic classes. As has been seen, however, there are disparities in food intake depending on individual SES, which influences malnutrition and the health of older people. People with a high level of education generally have a high level of knowledge about nutrition, consume healthy foods, as well as a variety of foods. Some reports have also shown that low-income groups demonstrate low serum albumin levels compared with middle-income groups. These results suggest that intake of meat and fish may be low [49]. Malnutrition countermeasures need to take differences in social classes into consideration, and food environments are required to provide older people with safe and appropriate dining options. For this to happen, the enhancement of food delivery services and communal dining facilities would be a welcome step [50].
Third is the importance of focusing on community environmental factors. The association between health and socioeconomic factors at a community level, rather than just differences in individual socioeconomic factors, has started to be reported. If there are no nearby stores where one can buy fresh fruit and vegetables, the nutritional state of people without access to transportation becomes affected. To establish a population-wide strategy and to counteract health disparities among social classes, measures against malnutrition must be examined in the future by compiling research that focuses on community environmental factors rather than just individual factors.
Although not touched upon here because of space constraints, the fourth point is the importance of research and countermeasures from a life course approach. As an example, in a Brazilian study, the quality of a child’s diet was associated with having no father in the household or having two parents with a low education level, and, in particular, it was four times worse in children whose parents did not finish elementary school than in children of parents who did [51]. A child’s SES is determined by the parents’ SES, and an undesirable foundation of eating habits is created by a parent’s SES being low, with the risk of it leading to poor health. This must be addressed while looking at all generations through the life course. Long-term comprehensive measures are required, such as improving the education level, knowledge about nutrition, and income security of mothers bearing the next generation.
6 Summary
“Nutrition improvement” is an important undertaking not only because it improves the state of malnutrition, but also because it leads to the maintenance of biological rhythm. The everyday act of eating is the foundation of individual self-actualization, through improvement of vital functions, restoration of communication, and social participation. It should be guaranteed regardless of SES or the community in which a person lives. On the other hand, nutritional state is influenced by social determining factors of health. To improve the nutritional state of all people, we must treat it as a population-wide problem rather than an individual one, and we must devise countermeasures with a life course approach while focusing on both disparities among socioeconomic classes and community environmental factors.
References
World Health Organization. Integrating poverty and gender into health programmes: a sourcebook for health professionals: module on nutrition. Geneva: WHO; 2010. Available at https://apps.who.int/iris/handle/10665/207658. Accessed Oct 2018.
Almasian Kia A, Rezapour A, Khosravi A, Afzali Abarghouei V. Socioeconomic inequality in malnutrition in under-5 children in Iran: evidence from the multiple indicator demographic and health survey, 2010. J Prev Med Public Health. 2017;50(3):201–9.
Food and Agricultural Organization of the United Nations (FAO). The state of food security and nutrition in the world. Rome: FAO; 2017. Available at http://www.fao.org/3/a-I7695e.pdf. Accessed Oct 2018.
UNICEF/WHO/The World Bank Group. Joint child malnutrition estimates - levels and trends. Geneva: WHO; 2017. Available at https://www.who.int/nutgrowthdb/jme_brochoure2017.pdf?ua=1. Accessed Oct 2018.
Kondo K. New public health paradigm: introduction to social epidemiology 2 - socioeconomic status and health. J Public Health Pract. 2004;68(2):132–6. (In Japanese).
Rachmi CN, Agho KE, Li M, Baur LA. Stunting, underweight and overweight in children aged 2.0-4.9 years in Indonesia: prevalence trends and associated risk factors. PLoS One. 2016;11(5):e0154756.
Office for Life-Style Related Diseases Control, General Affairs Division, Health Service Bureau, Ministry of Health, Labour and Welfare. Outline of results from 2016 National Health and Nutrition Survey in Japan. Tokyo: Ministry of Health, Labour and Welfare; 2017. Available at http://www.mhlw.go.jp/stf/houdou/0000177189.html. Accessed Oct 2018.
Japan Health Promotion and Fitness Foundation. Health Japan 21. Tokyo: JHPFF; 2013. Available at https://www.mhlw.go.jp/file/05-Shingikai-10601000-Daijinkanboukouseikagakuka-Kouseikagakuka/0000166300.pdf. Accessed Oct 2018. (In Japanese).
Yasutomo H, Yamanaka M, Tachibana E, et al. Study of body image and nutritional intake status among female students, vol. 7. Aichi: School of Nutritional Sciences, Nagoya University of Arts and Sciences; 2015. p. 15–23. (In Japanese).
“Nursing Care Prevention Manual” Distribution Research Group (Sugiyama M, Chairperson). Nutrition Improvement Manual (revised edition). 2009. Available at https://www.mhlw.go.jp/topics/2009/05/dl/tp0501-1e_0001.pdf. Accessed Oct 2018. (In Japanese).
Kuzuya M. Malnutrition in the elderly: international comparison of status and countermeasures. Ger Med. 2010;48(7):895–9. (In Japanese).
Malek Mahdavi A, Mahdavi R, Lotfipour M, et al. Evaluation of the Iranian mini nutritional assessment short-form in community-dwelling elderly. Health Promot Perspect. 2015;5(2):98–103.
Ferrari Bravo M, Gallo F, Marchello C, et al. Assessment of malnutrition in community- dwelling elderly people: cooperation among general practitioners and public health. Iran J Public Health. 2018;47(5):633–40.
Nestle Nutrition Institute. Mini Nutritional Assessment (MNA®). Available at https://www.mna-elderly.com/forms/MNA_english.pdf. Accessed Oct 2018.
Vellas B, Guigoz Y, Garry PJ, et al. The Mini Nutritional Assessment (MNA) and nomic differences in fruit and System • 8: 582--its use in grading the nutritional state of elderly patients. Nutrition. 1999;15(2):116–22.
Iizaka S, Tadaka E, Sanada H, et al. Comprehensive assessment of nutritional status and associated factors in the healthy, community-dwelling elderly. Geriatr Gerontol Int. 2008;8(1):24–31.
Kondo K, editor. Review “Health Disparity Society”: large-scale socio-epidemiological survey on preventive care in Japanese elderly. Tokyo: Igaku Shoin; 2007. (In Japanese).
Aida J, Hanibuchi T, Nakade M, et al. The different effects of vertical social capital and horizontal social capital on dental status: a multilevel analysis. Soc Sci Med. 2009;69(4):512–8.
Timpini A, Facchi E, Cossi S, et al. Self-reported socio-economic status, social, physical and leisure activities and risk for malnutrition in late life: a cross-sectional population-based study. J Nutr Health Aging. 2011;15(3):233–8.
Donini LM, Scardella P, Piombo L, et al. Malnutrition in elderly: social and economic determinants. J Nutr Health Aging. 2013;17(1):9–15.
Kabir ZN, Ferdous T, Cederholm T, et al. Mini Nutritional Assessment of rural elderly people in Bangladesh: the impact of demographic, socio-economic and health factors. Public Health Nutr. 2006;9(8):968–74.
Ferdous T, Kabir ZN, Wahlin A, et al. The multidimensional background of malnutrition among rural older individuals in Bangladesh - a challenge for the Millennium Development Goal. Public Health Nutr. 2009;12(12):2270–8.
Boulos C, Salameh P, Barberger-Gateau P. The AMEL study, a cross sectional population-based survey on aging and malnutrition in 1200 elderly Lebanese living in rural settings: protocol and sample characteristics. BMC Public Health. 2013;13:573.
Conklin AI, Forouhi NG, Suhrcke M, et al. Variety more than quantity of fruit and vegetable intake varies by socioeconomic status and financial hardship. Findings from older adults in the EPIC cohort. Appetite. 2014;83:248–55.
Atkins JL, Ramsay SE, Whincup PH, et al. Diet quality in older age: the influence of childhood and adult socio-economic circumstances. Br J Nutr. 2015;113(9):1441–52.
Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87(5):1107–17.
Nakamura T, Nakamura Y, Saitoh S, et al. Relationship between socioeconomic status and the prevalence of underweight, overweight or obesity in a general Japanese population: NIPPON DATA 2010. J Epidemiol. 2018;28(Suppl 3):S10–6.
Sakurai M, Nakagawa H, Kadota A, et al. Macronutrient intake and socioeconomic status: NIPPON DATA 2010. J Epidemiol. 2018;28(3):S17–22.
Nakamura M, Ojima T, Nakade M, et al. Poor oral health and diet in relation to weight loss, stable underweight, and obesity in community-dwelling older adults: a cross-sectional study from the JAGES 2010 project. J Epidemiol. 2016;26(6):322–9.
Nakade M, Takagi D, Suzuki K, et al. Influence of socioeconomic status on the association between body mass index and cause-specific mortality among older Japanese adults: the AGES Cohort Study. Prev Med. 2015;77:112–8.
Tani Y, Fujiwara T, Kondo N, et al. Childhood socioeconomic status and onset of depression among Japanese older adults: the JAGES prospective cohort study. Am J Geriatr Psychiatry. 2016;24(9):717–26.
Tani Y, Sasaki Y, Haseda M, Kondo K, et al. Eating alone and depression in older men and women by cohabitation status: the JAGES longitudinal survey. Age Ageing. 2015;44(6):1019–26.
Tani Y, Kondo N, Noma H, et al. Eating alone yet living with others is associated with mortality in older men: the JAGES cohort survey. J Gerontol B Psychol Sci Soc Sci. 2018;73(7):1330–4.
Ackerson LK, Kawachi I, Barbeau EM, et al. Geography of underweight and overweight among women in India: a multilevel analysis of 3204 neighborhoods in 26 states. Econ Hum Biol. 2008;6(2):264–80.
Subramanian SV, Kawachi I, Smith GD. Income inequality and the double burden of under - and overnutrition in India. J Epidemiol Community Health. 2007;61(9):802–9.
Hong R, Hong R. Economic inequality and undernutrition in women: multilevel analysis of individual, household, and community levels in Cambodia. Food Nutr Bull. 2007;28(1):59–66.
Tashiro A, Aida J, Shobugawa Y, et al. Association between income in quality and dental status in Japanese older adults: analysis of data from JAGES2013. Jpn Soc Public Health. 2017;64(4):190–6. (In Japanese).
Lee MR, Berthelot ER. Community covariates of malnutrition based mortality among older adults. Ann Epidemiol. 2010;20:371–9.
Katsarou A, Tyrovolas S, Psaltopoulou T, et al. Socio-economic status, place of residence and dietary habits among the elderly: the Mediterranean islands study. Public Health Nutr. 2010;13(10):1614–21.
Ball K, Lamb KE, Costa C, et al. Neighbourhood socioeconomic disadvantage and fruit and vegetable consumption: a seven countries comparison. Int J Behav Nutr Phys Act. 2015;12:68.
Frank BH. Epidemiology of obesity: Chapter 17 Social determining factors of obesity. Nagoya: The University of Nagoya Press; 2010.
Zenk SN, Schulz AJ, Hollis-Neely T, et al. Fruit and vegetable intake in African Americans income and store characteristics. Am J Prev Med. 2005;29(1):1–9.
Inagami S, Cohen DA, Brown AF, et al. Body mass index, neighborhood fast food and restaurant concentration, and car ownership. J Urban Health. 2009;86(5):683–95.
Fraser LK, Edwards KL, Cade J, et al. The geography of fast food outlets: a review. Int J Environ Res Public Health. 2010;7(5):2290–308.
Iwama N, Takana K, Sasaki M, et al. The dietary life of the elderly in local cities and food desert issues: a case study of Mito City, Ibaraki Prefecture. Hum Geograph Soc Jpn. 2009;61(2):139–56. (In Japanese).
Iwama N, Tanaka K, Komori N, et al. Mapping residential areas of elderly people at high risk of undernutrition: analysis of mobile sales wagons from the viewpoint of food desert issues. J Geogr. 2016;125(4):583–606. (In Japanese).
Asakawa T, Iwama N, Tanaka K, et al. Food deserts issues in a local city: empirical study in a local city that is composed of urban and rural area. Ann Jpn Assoc Urban Soc. 2016;34:1–13. (In Japanese).
Nakamura H, Nakamura M, Okada E, et al. Association of food access and neighbor relationships with diet and underweight among community-dwelling older Japanese. J Epidemiol. 2017;27(11):546–51.
Ota A, Kondo N, Murayama N, et al. Serum albumin levels and economic status in Japanese older adults. PLoS One. 2016;11(6):e0155022.
Takemi Y, Koiwai K. Strategy for prevention of undernutrition in the elderly: meal delivery service and eating together in the community for health care and promotion. J Natl Inst Public Health. 2017;66(6):603–11. (In Japanese).
Molina MCB, Lopéz PM, Faria CP, et al. Socioeconomic predictors of child diet quality. Rev Saude Publica. 2010;44(5):785–32.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (http://creativecommons.org/licenses/by-nc-nd/4.0/), which permits any noncommercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if you modified the licensed material. You do not have permission under this license to share adapted material derived from this chapter or parts of it.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
Nakade, M., Kondo, K. (2020). Malnutrition in Older People. In: Kondo, K. (eds) Social Determinants of Health in Non-communicable Diseases. Springer Series on Epidemiology and Public Health. Springer, Singapore. https://doi.org/10.1007/978-981-15-1831-7_13
Download citation
DOI: https://doi.org/10.1007/978-981-15-1831-7_13
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-1830-0
Online ISBN: 978-981-15-1831-7
eBook Packages: MedicineMedicine (R0)