Abstract
This chapter explores the role of healthcare organizations and their professionals in producing and reproducing inequality in health. Ethnographic fieldwork and interviews were conducted with key professionals involved in transferring patients with acquired brain injury from acute to subacute, and from subacute to stable rehabilitation. Our analytical framework combines Bourdieu’s theory of practice with Abbott’s concepts of jurisdiction. The study revealed a descent in specialization level and financial resources during patient trajectories, as well as changing patterns of decision-making practices affecting transfer. Paradoxically, many resources are available to save patients’ lives during the acute stage, but resources dwindle as the patient approaches long-term rehabilitation, thus perpetuating inequality in healthcare.
Similar content being viewed by others
11.1 Introduction
Inequality in treatment and rehabilitation in general is well documented in Western countries (Devaux and de Looper 2012; Eikemo et al. 2008; Willis et al. 2016). Although most health expenses are paid through taxes in the Nordic welfare states, and therefore cost is not a barrier for accessing healthcare services, inequality in health still exists (Kamper-Jørgensen and Rasmussen 2008; Bambra 2012; Larsen et al. 2013; Mackenbach et al. 2008). Socioeconomic variables such as education, income, housing, and family situation among patients are commonly used to examine the success of rehabilitation in Denmark (Andersen et al. 2014; Guldager 2018). In this study, though, we have chosen a different approach by exploring the role of healthcare organizations and healthcare professionals (HCPs) in relation to inequality in health outcomes. By empirically focusing on transfer practices during the rehabilitation of patients with severe acquired brain injury (sABI ), our ambition is to gain knowledge about how inequality may also be generated among HCPs in organizations. This chapter presents an empirical study of the trajectories of patients with sABIs, including severe traumatic and non-traumatic brain injury (e.g., stroke and subarachnoid haemorrhage from acute to long-term rehabilitation), to investigate how HCPs at different levels influence transfer practices. The analysis is based on Pierre Bourdieu’s theory of practice and key concepts of Andrew Abbott’s theory of profession.
11.2 Rehabilitation of Patients with Acute Brain Injury
Rehabilitation after acute brain injury has developed in recent years from nonspecialized practice with limited expertise and access to highly specialized interdisciplinary neurorehabilitation units in many Western countries (Engberg et al. 2006). Specialization and centralization of neurorehabilitation has resulted in better patient outcomes (Anke et al. 2015; Engberg et al. 2006). The typical trajectory for the most severely injured patients is acute hospital admission via the trauma centre and neurointensive care unit, followed by transfer to in-house specialized rehabilitation and finally rehabilitation in primary care (National Board of Health 2011). The length of stay at hospitals has been reduced dramatically in recent years (Husted et al. 2012) and, consequently, HCPs must ensure that patients are transferred to the ‘right’ department for the ‘right’ treatment and care at the ‘right’ time. The constant focus on cost and effectiveness also sets standards for streamlining the HCPs’ work. Incentive structures have been introduced to direct professional practices (e.g., rates according to the ‘diagnose related groups’ system) (Bossen et al. 2016). Efficient transfer has traditionally been driven by physicians, as they represent the group of professionals with authority to make decisions on diagnoses and treatment. However, because of the involvement of interdisciplinary staff working in more specialized healthcare institutions, we assume that decision-making in this context is no longer solely a medical issue. We regard organizational and professional values and standards as an integrated part of clinical decision-making when it comes to transferring patients in a highly specialized healthcare sector.
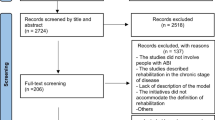
11.3 Design and Methods
The study featured a prospective qualitative design using ethnographic fieldwork and in situ interviews at three institutions in the Capital Region of Denmark. We strategically selected the sites and settings according to their levels and areas of specialization. The institutions represented three stages in the rehabilitation trajectory: the acute stage (institution A), including acute hospital admission and intensive care; the subacute stage (institution B), including highly specialized intensive neurorehabilitation; and the stable stage (institution C), including long-term outpatient rehabilitation at the municipal level.
The intention with the ethnographic fieldwork was to focus on observations of interdisciplinary meetings in which we assumed that decisions were made about patient transfer to the ‘next’ institution/department according to each patient’s specific rehabilitation needs. It was discovered, however, that transfer decisions were not necessarily made at the regular meetings. The procedures at the acute and stable stage institutions were more ad hoc, emerging during the everyday work, whereas formal discharge meetings were held at the subacute institution.
We emphasize that the empirical material reflects the differences in transfer-related decisions. Our data consist of field notes and interview transcripts from institutions A, B, and C. The three institutions were each visited for three days as an introduction to fieldwork to get a feel for the work and organization of patient transfer. At institutions A and C, fieldwork was conducted as nonparticipatory observation for five days at each site, focusing on the ad hoc situations wherein transfer was negotiated. At institution B, where specific transfer meetings were organized, we observed ten meetings and supplemented our notes from these with debriefings and interviews.
At institution A, the physicians were the primary objects of observation because they were formally in charge of the transfer procedure. Coordinating nurses and a physiotherapist were also observed to describe their roles in the decision process. We interviewed the head physician, the coordinating nurse, and three other physicians at the site.
At institution B, we observed interdisciplinary meetings with potential patient and family participation. During the days of introduction, a physician, a nurse, and an occupational therapist were observed in their everyday work with severely brain-injured patients. Ten interdisciplinary meetings were observed, focusing on the dominant argument bringing the patient further in the rehabilitation process. The HCPs had to determine whether the patient should stay in specialized rehabilitation or transfer to the next stage of rehabilitation as an outpatient. Eight of the ten interdisciplinary meetings were recorded and transcribed by a student with assistance from the researcher present at the meetings. The number of participants at the interdisciplinary meetings ranged from 8 to 12 persons including the relatives. In situ interviews were conducted after the meetings with participants with or without influence on the decisions. The idea was to explore the decisional nuances and what might be at stake for the HCPs.
The main focus of fieldwork at institution C was the licensed practical nurses, also known as ‘social and healthcare assistants’Footnote 1 (SHAs), since they were the active professionals with the responsibility of getting the patients further towards discharge from the institution. Other HCPs were interviewed, such as an occupational therapist, the leader of a volunteer group, and the leader and deputy of the institution. Although our data are heterogeneous, we argue with the ethnographic tradition that a ‘desk design’ of our study must adapt to real-life practices and not the other way around (Hammersley and Atkinson 2007; Walford 2009).
We adhered to the ethical principles of the Declaration of Helsinki (World Medical Association 2018). Managers and staff at the three institutions were informed of the aim of the study, as well as the planned observations and interviews. The HCPs and relatives who were observed and interviewed provided their informed consent to participate. The HCPs involved were advised that participation was voluntary and that they could withdraw their consent at any time.
11.4 Analytical Framework and Operationalization
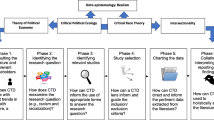
The theoretical approach is mainly based on Pierre Bourdieu’s theory of practice or praxeology (Bourdieu 1990, 1994, 1997), while Andrew Abbott’s concept of ‘jurisdiction’ is used to highlight the professional aspects of practice (Abbott 1988, 2005).
When focusing on the HCPs’ practices, we rely on Bourdieu’s relational and dispositional approach (Bourdieu 1997, 2002). Relations become real out of the tension emerging from the result of something being ascribed and acknowledged as having more value than something else, and the assumption that the distribution of who has the valuable ‘capital’ becomes bodily knowledge to the professionals and orients but does not determine their practices. This perspective gives voice to the HCPs’ subjective experiences and preferences (Bourdieu 2000a; Bourdieu and Passeron 2000). However, this subjectivity must, according to Bourdieu, be contextualized by objectifying or constructing the platform on which the professionals speak and act. The introduction of the present chapter is meant to illustrate the contours of the objective conditions as a platform for practising transfer , and also the following ‘descriptive analysis’ of the different organizations should function as such. In this description, the material aspects and architectural conditions are included to show how these aspects of an organization are not solely objective but encompass cumulated values, and, as such, represent the institution.
The concepts of ‘field’, ‘capital’ , and ‘habitus’ are crucial thinking tools and have been used accordingly in order to analyse the transfer practices (Bourdieu 1994, 1997). ‘Practice’ is an overarching concept, whereas the notion of ‘strategy’ is an understanding and explanation of practice closely connected to the concept of habitus. What counts as capital when making clinical decisions of transferring patients within a specific setting (i.e., field) is understood as naturalized among the HCPs. ‘Habitus’ refers to a system of embodied dispositions orienting people to act and think in the social world (Bourdieu 2000b, p. 161). A society frames life conditions for its individuals through its collective history. Habitus undergoes changes constantly, but they are always added to what was the starting point. ‘System of dispositions’ refers to the fact that an individual habitus must be perceived as a structural variant of a group habitus (Bourdieu 1990, p. 60). We draw on the work of Reay (1998) and colleagues, who defined institutional habitus as ‘the impact of a cultural group or social class on an individual’s behaviour as it is mediated through an organization’. Furthermore, we use the notion of group habitus to guide our understanding of a profession’s strategies. Thus, healthcare institutions may be able to determine what values, language, and knowledge are regarded as legitimate within a specific institution, but, to this, we add group habitus to distinguish the different collective habitus since the individual professions, such as physicians, nurses, SHAs, physiotherapists, psychologists, and so on, have more in common with individuals from the same profession than with those from other professions.
According to most profession researchers, the HCPs’ knowledge base is the main source legitimizing professional practice. When professional monopoly of practice is defended, the professions’ knowledge base becomes crucial (Abbott 1988). Abbott’s concept of ‘jurisdiction’ has been used to grasp the HCPs’ sphere of operation based on knowledge particular to a profession. By analysing the limits of tasks—in our study, the tasks related to patient transfer—it has been possible to identify jurisdictional disturbances and control. In this way, we have been able to show the strength or weakness of negotiation of patient transfer among HCPs. Both the ethnographic field notes and the transcribed interviews have been coded manually, guided by the distribution of dominant symbolic capital in a relational perspective.
11.4.1 Descriptive Analysis of the Organizations: Transfer Practices
11.4.1.1 Institution A: The Acute Stage
This institution performs by several parameters as one of the most prestigious institutions within the medical field. It is the largest and most specialized hospital in the country. Only three other hospitals treat this category of severely brain-injured patients, and this particular neurointensive care unit offers treatment and care to patients with the most vital organs at risk. In such circumstances, the main organ at risk is the brain, which is considered one of the most significant organs in relation to medical specialities (Album et al. 2017). Patients arrive at the ward by emergency transportation, either by ambulance or a helicopter landing on the hospital roof. The responsibility of the specialized hospital extends to Danish residents abroad, who are also medevacked to this facility. Thus, the highly specialized hospital is not only for local residents but functions as the main referral institution for patients with brain injuries.
Emergency situations overrule other activities at the hospital. Elevators are reserved for emergency patients, interrupting other activities to provide the most expedient service for the acute and critically ill patients arriving at the hospital. When patients arrive at the trauma centre, which functions at a level consistent with that of a Level I centre, specialists from all imaginable somatic subspecialties are at their disposal. The trauma team consists of at least 16 HCPs providing the most important stabilizing treatment before the patient is transferred to surgery or one of the more intensive care units. The medical staff team members at the trauma centre and at the intensive care units have two years of specialty training and the nurses hold two-year critical care certification. The team consists of medical specialists, nurses, physiotherapists, X-ray technicians, and other core staff. The hospital no longer employs non-registered nurses, due to the high level of specialization. All patient rooms are placed on the side of the ward facing the windows. There is a front office with ward secretaries and nurses working on computers and observing patient monitors. For an outsider, the technical equipment is overwhelming. All patients’ vital organs are monitored and maintained continuously. The daily cost for a patient at this unit runs at approximately EUR 3500.
Transfer Practices Maintaining Acquired Highly Prestigious Position and Managing Hyper-Specialization of Healthcare
The physicians at the neurointensive care unit are mostly neuro-anaesthesiologists . Day shifts start with an 8 a.m. conference in a room away from the unit. About 10–12 physicians and 1 coordinating nurse are present. The doctor in charge from the night shift leads the meeting, during which the most urgent patient problems are presented and discussed. All issues focus on whether the patient should stay or be transferred to another ward or hospital.
Around 9 a.m., the physicians and the coordinating nurse meet again. In the meantime, they have seen some of their patients, checked up on their computers, or participated in an academic ‘15-minute meeting’. The ‘nine o’clock-meeting’ is conducted in a different conference room within the ward. Here, more specific plans are made for the patients. Following the logic of the patient rooms, all diagnoses, treatments, and patient responses are presented by the doctor in charge of each patient. The final topic of discussion is whether the patient should stay or transfer out of the unit.
At noon, anaesthesiologists and neurosurgeons meet to discuss whether patients are fully treated from a neurosurgical perspective. If treatment has finished and the patient is free of the mechanical ventilator, the anaesthesiologists are responsible for finding a bed for the patient after transfer. If the patient has not fully responded to treatment, the physicians conclude: ‘Not going anywhere’.
The neurosurgical department must at all times be triple-prepared to provide anaesthesia during (a) acute thrombectomy (blood clot removal), (b) acute magnetic resonance imaging (MRI) scans (if anaesthesia is needed), and (c) neurosurgery. These procedures provide legitimate access to the ward regardless of a patient’s age. These structural conditions challenged the survival statistics as older people who have suffered strokes are given the same access to acute treatment. The ward manager and physicians experience constant pressure to admit patients and to transfer patients out of the unit. In addition to the meetings in which ‘stay-or-go’ decisions are a central part of the agenda, the neurosurgeons and anaesthesiologists must keep abreast of which patients might be ready for transfer. Although the neurosurgeons might consider the patient fully treated, the anaesthesiologists have the final say regarding patient transfer.
After neurointensive care, the ‘next-step institution’ is the subacute rehabilitation department located at a different hospital site. If a patient requiring close observation is not ready for subacute rehabilitation and a new patient is being admitted, the physicians are responsible for finding an appropriate placement for the patient transferring out of the unit.
Considered from Abbott’s perspective, according to which the physician’s medical specialty is seen as a jurisdiction, it might be assumed that the anaesthesiologists would try to keep compromised patients in the unit in order to control the boundaries of their jurisdiction until the patients are stable. In this way, the jurisdiction could be maintained and the anaesthesiologists could exercise their particular skills. But, this was not the case in our study. Seen as a strategy, we found that the physicians incorporate the structural conditions (i.e., all patients with severe brain trauma and compromised vital functions must be received in this ward). With Bourdieu’s concept of capital, the explanation for the transfer practice seems to offer more nuances. Possessing the exceptional skills of saving lives and mastering health problems related to the vital organs represents high stakes within the medical field. When negotiating over the phone with other anaesthesiologists regarding whether or not to transfer a patient to another intensive care unit, they are also confirming each other in their exclusive positions.
Transferring to temporarily stay in another hospital is an inconvenience to the patient and their family. It represents a ‘detour’ in the trajectory towards the ‘right place’ (i.e., the neurorehabilitation department). As one physician explained:
Of course, we think that it was even better if the patient was fully treated at the intensive care unit at [hospital A], which means that he was off the ventilator and sent directly to rehabilitation unit (hospital B) where he belongs. Of course, that is the ideal … even though [hospital A] has expanded the number of beds, it seems that there is never enough space.
Equally, an anaesthesiologist from a ‘detour hospital’, who received a ‘detour patient’, experienced the transfer procedure as ‘exemplary’, explaining:
Well, I think it has something to do with … of course, besides that, we are good people and we want to help each other … that we know each other very, very well within the intensive care units. … It’s a small specialty; often, I would know somebody’s name. And we all know the problem of overcrowding; the next day, I might be in the same situation. It’s not like we are talking about a random admission … I mean, a neat and equal distribution of patients among the available beds at all hospital at all times … You have to take the patients to where the empty beds are …
The physicians are probably aware of the structural constraints and lack of vacant beds, and they have not completely naturalized the conditions—one anaesthesiologist referred to the transfer practice as a ‘logistic hell’. At first glance, the physicians act pragmatically, but, applying the theories of Bourdieu and Abbott, it becomes apparent that the specialist physicians confirm their exclusive position while they transfer the patient. The negotiation of vacant beds at the receiving unit serves as an act of consolidating joint jurisdiction. According to Bourdieu’s argument, we see a maintenance of an exclusive position strengthened by a strong network among the peer privileged.
Challenges to the Boundaries of Jurisdiction at Institution A
Following the boundaries of the jurisdiction, the structural conditions (i.e., triple-preparedness to provide anaesthesia) disturb the jurisdiction and challenge the a priori privilege of physicians to autonomously admit and discharge patients.
The physicians use an implicit algorithm for patient transfer between units and hospitals. Treating medical problems in multiple organ failure means that a dominant organ has to be defined in order to place the patient at the ‘correct’ ward. It is negotiable whether a patient can be accepted as a ‘detour patient’, but other limitations are non-negotiable: if the main diagnosis is not treated at the ‘detour hospital’ (i.e., intensive care needs in addition to urology, and abdominal surgery) and the specific medical specialty is not backed up at the hospital, the anaesthesiologists do not even ask for a ‘detour bed’. As formulated by a ‘detour anaesthesiologist’ (doctor receiving a patient from hospital A, neuro-anaesthesiological ward):
We don’t want patients out here with urological problems, since we do not have an urologist at our hospital. If urology is the main problem, it is only hospital x, y, or z [regional hospitals]. We have to cooperate in this way, right? Of course, it is an advantage that we know how the region has distributed its medical specialties, but we know that, of course.
The ‘necessity’ of hyper-specialism of modern-day hospitals seems to be incorporated and naturalized in an uncompromised way. Exercising a medical specialty can only persist if the physicians are able to call other specialists. If the boundaries of a particular jurisdiction are blurred, though, it is hard to distinguish between specialties. In this way, transfer practices serve to maintain a specific medical specialty and to support its distinctiveness. In addition to the distinct knowledge of a prestigious medical specialty, it appears that the physicians have acquired a specific competence by knowing which hospital or ward to contact for a patient transfer. Furthermore, the physicians are aware that this knowledge is crucial and provides access to the administrative domain that often challenges their own dominant medical capital.
11.4.1.2 Institution B: The Subacute Stage
At this neurorehabilitation institution, patients are accepted when they are no longer ventilator dependent, although they still might need some breathing support. At this stage of rehabilitation, a virtue is made of the need for interdisciplinary healthcare services. All the clinical staff from the dayshift meet at 8 a.m. in the morning for a so-called safety debriefing. About 25 people sit in a large staff room. Nobody drinks coffee here. A senior physician leads the meeting, all subdepartments (divided according to patient beds) have their own rounds, and the HCPs have a chance to present specific problems, such as, ‘We need to discuss patient x more’; a meeting is planned through a request from the physiotherapists; a patient coughs during physical training and it is discussed whether the timing of exercise could be rescheduled; the senior physician speaks about a report from the central working environment council; some technical equipment is re-located, and so on.
The HCPs wear uniforms in different colours: turquoise or white. Apparently, there is no particular colour code for the professions. Physicians and therapists wear T-shirts and trousers, both wear turquoise T-shirts; nurses prefer white, but wear turquoise as well. The traditional white lab coats worn by physicians over street clothes are banned, but some physicians still use them. The daily cost for a patient at this unit runs at approximately EUR 2000.
Transfer Practices as Interdisciplinary Joint Practices
Transfer decisions are made during ‘treatment meetings’ or ‘team meetings’. Treatment meetings, held every two weeks, are used to plan ongoing rehabilitation, whereas in team meetings, held every six weeks, decisions are made regarding whether to transfer or discharge a patient or to continue rehabilitation for another six weeks.
Physicians, neuropsychologists, physiotherapists, occupational therapists, nurses, and occasionally SHAs and social workers participate in both treatment meetings and team meetings. At the latter, where transfer is the main issue on the agenda, the physician leads the meeting. When the physician for some reason has to leave the meeting early, the next in line to lead the meeting is the neuropsychologist, who also holds an academic degree. The physician gives all the HCPs a chance to speak and they each describe the positive or negative progress of the patient in question. When the round of updates is over, the physician decides whether the patient should be offered another six weeks of rehabilitation. Representatives from municipal outpatient care join the meeting at this time. Up to three different coordinators participate: the municipal coordinator, a brain injury coordinator, and a triage manager. The purpose is to find the best place to meet the needs of the patient while adhering to the municipal regulations for treatment costs. When the patient leaves the hospital, payment is transferred from the region to the municipality.
Challenges to the Boundaries of Jurisdiction at Institution B
At the subacute institution, transfer practices are organized collectively, and transfer decisions are shared among HCPs. This flatter organizational structure is a contrast to the paternalism observed in the acute organization. What can threaten the legitimacy of the ward is, as we saw at institution A, conditions preventing HCPs from exercising their specialty.
During observation, a male patient exhibited highly agitated behaviour probably due to brain damage. His uncooperative behaviour and hostility towards the staff were so extreme that it was discussed whether a psychiatric diagnosis was dominant. The physicians at institution B pushed towards transfer to the psychiatric ward, whereas the psychiatric personnel did not support this proposal. Although the meeting was led by the physician, transfer decisions were ideally based on equality among the HCPs present. The physician made the initial decision on patient transfer (stay or go), but the decision could be changed if other HCPs had a stronger argument. Relatives also had a voice and, for example, could argue for an extension of six more weeks in rehabilitation. In two of the ten observed meetings, the relatively underprivileged relatives managed to change the HCPs’ (specifically, the physician’s) decision. In one case, a Filipino airport housekeeper and mother in a family with strong caring values became emotional and almost begged the physician to grant the patient another six weeks of rehabilitation. Another mother, herself disabled and in a wheelchair, from a low-income family succeeded in changing the decision by using strong language. As the physician explained, ‘We are not ironbound, we are open for new impressions’. Strong emotions, personalities, and family ties together with a flatter hierarchy and the opinions of additional actors, yet still with the physician as the final decision-maker, can apparently succeed in influencing an administrative and medical decision.
By being an exceptional, specialist unit (only one other institution has the same status in Denmark), the unit becomes attractive to the patients and their relatives. It also seems to be commonly acknowledged that, once the patient has moved on to the next step—either another local community institution or back to their own home—the rehabilitation is less intensive.
11.4.1.3 Institution C: The Stable Stage
The local municipality has the responsibility of organizing rehabilitation for patients in the stable stage after severe brain injury. Institution C is run as a self-governed institution managing rehabilitation tasks on behalf of the municipality. This institution is the last step before discharge to home or a permanent care institution. Patients—or ‘residents’, as they are called when they leave the hospital—are rehabilitated for complex reasons, but the overall criterion for admission to municipal rehabilitation is an inability to take care of oneself. The specialty of institution C is social complexity, and one of the three floors at the institution is dedicated to residents with severe alcoholic abuse issues, although residents with other problems might also have problems with alcohol abuse. Residents with acquired brain injury are located on the two other floors, mixed with residents suffering multiple health problems as well as socioeconomic issues. As the institution leader explained, ‘Our main focus is to speak up for those who are unable to speak up for themselves’. The leader adheres to the principles of ‘taking the side of the resident’, ‘being a watchdog’, and ‘acknowledging professional indignation’. The leader also emphasizes user participation and user involvement as institutional values. The cafeteria in the institution is open to the public but is primarily used by former residents with close relations to other residents and the institution. The staff team consists of professionals, former residents, and volunteers. The two institution leaders are equipped with degrees in sociology and psychology, whereas the ‘street-level’ staff are unlicensed nurses or SHAs. There are no nurses or doctors employed at the institution. The residents, like the general population, have their own municipal general practitioner (GP), who can be called by the SHA if needed. SHAs are in charge in the wards, and also in charge of the decision to transfer a patient home. The daily cost for a resident at this institution runs at approximately EUR 220.
Transfer Practices as Pulling and Pushing Tardy Structures
The institution leaders and SHAs experience the GPs as reluctant to show up when they are needed, causing major problems. One day during our study’s fieldwork, the SHAs discovered an unresponsive patient/resident. The patient had multiple diagnoses, including diabetes, liver disease, and complications following a brain injury. The SHAs conferred with one another and decided that the patient’s level of consciousness had changed markedly. An SHA called the GP several times, and, the next day, the GP called for an ambulance that brought the resident to the hospital. The resident was later diagnosed with pneumonia and remained at the hospital for intensive observation. The SHA said, ‘His own doctor doesn’t really want to have anything to do with him’.
In comparison to the acute and subacute stages of rehabilitation, where, as has been described, a patient’s physical function and brain damage are the central focuses, the focal point at institution C is the wider social complexity of the situation. The following exchange observed between two SHAs demonstrates this:
INTERVIEWER: What happened to this resident? Why is he [the resident] here?
SHA1 (rehabilitation assistant grabs the chart and starts to read): ‘A 60-year-old man admitted to the trauma centre. Patient found unconscious in his home by the janitor’…
INTERVIEWER: Oh, the janitor was there too…
SHA1: He was evicted from his apartment, I guess…
SHA2: It looks like he didn’t pay the rent. He couldn’t manage staying in his own apartment. They say the apartment was in a terrible condition. (Also reading now) ‘On arrival, the patient had nomoterm’… I don’t know what that means. (Reads again) ‘The patient is probably suffering from alcohol abuse. Not further information on arrival.’
SHA1: ‘… showing a big subdural haematoma’ … (mumbling … reading to herself)
INTERVIEWER: Could you read it aloud?
SHA1: He has had something after he fell, right?
INTERVIEWER: Yes, when was that?
SHA1: August 26th (it is now September 18th).
INTERVIEWER: So, that was just before he came here?
SHA1: I guess it was. That’s what it says happened …
INTERVIEWER: So … he was at the trauma centre at [institution A]?
SHA1: I think he was … it doesn’t really say where he was, it just says ‘neurosurgical clinic’…
INTERVIEWER: It’s most likely [institution A].
SHA1: Then it says something about ‘GCS 7 with slowly reacting pupils’ … I don’t know what that means.
The complexity of a resident’s needs is not limited to the body, as we had observed at the acute stage institution. Here, a body was a body regardless of age, due to the new regulations. Moreover, in addition to physical problems, the patients have severe psychosocial issues. Their housing situation, finances, social networks, and work relations (if any) are taken into consideration during negotiations regarding the final housing for a resident. Often, the brain damage was caused by risky behaviour combined with drug or alcohol abuse, and, in these circumstances, it is unclear whether a patient’s behaviour is a result of brain damage or chemical abuse. Another major issue the staff had to deal with as part of the transfer practice was that the resident was illiterate in respect of the modern digitalized world, including the management of various credit cards and codes and communicating with authorities (bank, computerized information systems, etc.). Accordingly, the SHAs had to escort the residents to the bank or municipal office to acquire new cards and codes, if they for some reason had lost their cards or forgotten their codes. They organized regular visits with the residents to renew these cards and codes, and, for each individual, they had to decide how to integrate the ethics and the practicalities around these issues.
On top of this, the SHAs struggled with slow service at the municipal office that managed the housing situation as a precondition to get residents transferred to a permanent housing and healthcare situation. SHAs were continually pushing the municipal office to speed up progress regarding a resident’s housing situation in the system. One SHA called several times and left messages, all in vain, while she waited for an official answer to a request for a specific apartment. She began to describe her experiences in a calm voice, but had trouble keeping her anger down:
SHA1: So you know, Steen [resident] should have received a letter within two weeks … And this is the problem! I tell Bob [the social worker in charge], ‘Steen is suffering from amnesia, he forgets stuff, he can’t do things’. Then Bob says, ‘But I have sent it! Maybe I have sent it electronically?’ So I think to myself, ‘What is this idiot thinking? Steen has been evicted. He has no credit card. He gets a new credit card every week because he forgets where he puts it. He hasn’t got a health insurance card, he has nothing … He wouldn’t even open his mail … And then they send an e-mail?’ I say, ‘Very clever’ … really … he doesn’t even have a wallet.’ He [the social worker] works with this kind of residents, and I think, ‘Can’t he even put two and two together?’ I get pretty upset by these cases …
11.5 Discussion
11.5.1 Organizationally Produced Inequalities in Transfer Practices
Taking for granted that a smooth-running flow through the involved organizations is beneficial for the acute brain injury patients’ rehabilitation process, we have identified some constraining dynamics that need attention. Perhaps most troublingly, the sick organ, the brain, and the neurosurgical and ensuing neuro-anaesthesiological treatment seem to have undergone a dramatic decline during the rehabilitation process. According to Album et al. (2017), the brain is, along with the heart, an organ associated with most prestige among medical professionals and specialities. From a relational perspective (see also Table 11.1), we observed all the prestigious attributes attached to the acute stage of neurorehabilitation (institution A): artefacts supporting life-saving (helicopter, medico-technical equipment, everything must yield at the escalator to allow the medical staff to act) and the ward is staffed with the best-educated HCPs, who possess strong social capital by knowing their transfer partners at the other end and by understanding the way all the specialties are organized and thereby whom should be contacted for a successful transfer.
At the subacute stage (institution B), a firmly orchestrated transfer procedure seems to keep the rehabilitation process on track, and, to a certain degree, overcomes the traditional professional hierarchy. This study has not examined the interdisciplinary dynamics at a micro level, but we did notice a common approach among the ten team meetings wherein the transfer of patients was decided. There were no written procedures or rules, yet the HCPs acted almost ritualistically in respect of who had a say and at what time within the scheduled hour for the meeting. A professional hierarchy was maintained, with the physician the leader of the meeting and having the final say about whether the patient should ‘stay’ or ‘go’. Nonetheless, we inferred that the institution’s transfer practice featured strong democratic traits, according to which the decision of what should happen to the patient’s rehabilitation process was clear to the participants. Ironically, however, it was not always clear to the patient—but here we have to take the patient’s cognitive condition into consideration, due to the brain damage. Additionally, the structure of the transfer meetings could, to some extent, overcome the asymmetric relation between high-positioned physician and low-positioned relatives.
Regarding institution C—corresponding to the so-called stable stage, during which a patient’s transfer to the final housing destination is handled—we saw a severe decline in action and progress in the transfer processes. The next stop after rehabilitation should be either home, with assisted care, or a nursing home. Institution C was regarded as being applicable during the stable stage, which reflects a biophysical view of brain damage. However, the patients’ socioeconomic situations were often anything but stable. Their housing situations, in particular, were often unclear and the patients were stuck at the institution. The patients’ needs at this stage were complex and multiple, but in other, more socially complex ways than in the life-threatening context of their needs at the acute stage of their illness. There seems to be a strong discrepancy between the intense treatment and relatively smooth transfer from institution A (acute) to institution B (subacute) and that from institution B to institution C (stable stage).
From a relational perspective, the low-positioned social- and healthcare workers in charge of transfer had little power concerning slow-acting structures, compared to the physicians with highly specialized and long educations and appropriate social capital with which to pave the way for smooth patient transfers. The strong organization of transfer from institution B to institution C stabilized the transfer processes. The municipal presence and the economic capital might play a major role too, since the municipal representatives had an interest in minimizing the costs of an expensive stay at the hospital (institution B).
The physicians’ transfer practices at institution A were characterized by confirming jurisdiction and by maintaining acquired position through acting in closed circles. At institution C, the health professionals (SHAs ) expanded their jurisdiction. However, their ‘new’ jurisdiction—pulling and pushing slow-acting authorities and helping residents to re-establish lost cards and codes—are not exactly high-stake tasks from a field perspective. In fact, the tasks were unsuccessful ‘leftovers’ from the other cooperating partners.
11.6 Conclusion
Viewed through the relational perspective applied in this study, it appears that healthcare organizations produce and reproduce inequality in health. At the highly specialized institutions close to the medical field, the privileged HCPs solidify their positions, whereas the less privileged HCPs, even as they produce new tasks and, in doing so, expand their jurisdiction, feel inadequate and frustrated by their experience of practising tasks of patient transfer. The economic and symbolic resources expended at the acute care stage contrast significantly to those spent at the final institution prior to discharge. In this way, the uneven resources spread over the trajectory of the rehabilitation process reduce the quality and likelihood of a coherent rehabilitation, which clearly does not benefit patients. Therefore, future discussions should consider the extent to which efforts expended during the acute stage match the outcome when patients reach the stable stage of their rehabilitation; in other words, saved lives must be lived.
Notes
- 1.
Licensed practical nurses—or, directly translated, ‘social and healthcare assistants’—complete two years, nine months, and three weeks of education, admitting students with a secondary school diploma. In comparison, registered nurses are admitted with a high school diploma and complete a three-year, six-month baccalaureate education.
References
Abbott, A. (1988). The system of professions – An essay on the division of expert labor. Chicago: University of Chicago Press.
Abbott, A. (2005). Linked ecologies – States and universities as environments for professions. Sociological Theory, 23, 245–274.
Album, D., Johannessen, L. E., & Rasmussen, E. B. (2017). Stability and change in disease prestige: A comparative analysis of three surveys spanning a quarter of a century. Social Science & Medicine, 180, 45–51.
Andersen, K. K., Dalton, S. O., Steding-Jessen, M., & Olsen, T. S. (2014). Socioeconomic position and survival after a stroke in Denmark, 2003 to 2012: Nationwide hospital-based study. Stroke, 45(12), 3556–3560. https://doi.org/10.1161/STROKEAHA.114.007046.
Anke, A., Andelic, N., Skandsen, T., Knoph, R., Ader, T., Manskow, U., et al. (2015). Functional recovery and life satisfaction in the first year after severe traumatic brain injury: A prospective multicenter study of a Norwegian national cohort. Journal of Head Trauma Rehabilitation, 30(4), E38–E49. https://doi.org/10.1097/HTR.0000000000000080.
Bambra, C. (2012). Social inequalities in health: The Nordic welfare state in comparative context. In J. Kvist, J. Fritzell, B. Hvinden, & O. Kangas (Eds.), Changing social equality: The Nordic welfare model in the 21st century (pp. 143–164). Bristol: Policy Press.
Bossen, C., Danholt, P., & Klausen, M. (2016). Diagnoser som styringshybrider Diagnoserelaterede grupper i sundhedsvæsenet. Tidsskrift for Forskning i Sygdom og Samfund, 13(25). https://doi.org/10.7146/tfss.v13i25.24995.
Bourdieu, P. (1990). The logic of practice. Stanford: Stanford University Press.
Bourdieu, P. (1994). De tre former for teoretisk viden (M. Nørholm & K. A. Petersen, Trans.). In S. Callewaert, P. Bourdieu, M. Munk, M. Nørholm, & K. A. Petersen (Eds.), Pierre Bourdieu: Centrale tekster indenfor sociologi og kulturteori (pp. 72–108). Copenhagen: Akademisk. Original work published as: Bourdieu, P. (1973). The three forms of theoretical knowledge. Social Science Information, 12(1), 53–80.
Bourdieu, P. (1997). Af praktiske grunde: omkring teorien om menneskelig handlen [Practical reason: On the theory of action]. Copenhagen: Hans Reitzels.
Bourdieu, P. (2000a). Homo academicus (Reprint). Stanford: Stanford University Press.
Bourdieu, P. (2000b). Pascalian meditations. Oxford: Polity Press.
Bourdieu, P. (2002). Distinction – A social critique of the judgement of taste. London: Routledge.
Bourdieu, P., & Passeron, J. C. (2000). Reproduction in education, society and culture (New ed.). London: Sage.
Devaux, M., & de Looper, M. (2012). Income-related inequalities in health service utilisation in 19 OECD countries, 2008–2009 (OECD health working papers, No. 58). Paris: OECD Publishing. https://doi.org/10.1787/5k95xd6stnxt-en.
Eikemo, T. A., Bambra, C., Joyce, K., & Dahl, E. (2008). Welfare state regimes and income-related health inequalities: A comparison of 23 European countries. The European Journal of Public Health, 18(6), 593–559.
Engberg, A. W., Liebach, A., & Nordenbo, A. (2006). Centralized rehabilitation after severe traumatic brain injury – A population-based study. Acta Neurologica Scandinavica, 113(3), 178–184.
Guldager, R. (2018). Inequality in neurorehabilitation: Different practices among patients and relatives during rehabilitation after stroke and severe traumatic brain injury: A qualitative study. Doctoral dissertation, Aalborg Universitetsforlag.
Hammersley, M., & Atkinson, P. (2007). Ethnography: Principles in practice. London: Routledge.
Husted, H., Jensen, C. M., Solgaard, S., & Kehlet, H. (2012). Reduced length of stay following hip and knee arthroplasty in Denmark 2000–2009: From research to implementation. Archives of Orthopaedic and Trauma Surgery, 132(1), 101–104. https://doi.org/10.1007/s00402-011-1396-0.
Kamper-Jørgensen, F., & Rasmussen, J. G. (2008). Ulighed i behandling [Inequality in healthcare]. In F. Diderichsen, J. G. Rasmussen, & N. Döllner (Eds.), Den tunge ende: sandheden om ulighederne og uretfærdighederne i den danske sundhed: debatbog (pp. 27–45). Copenhagen: Dagens Medicin Bøger.
Larsen, K., Cutchin, M. P., & Harsløf, I. (2013). Health capital: New health risks and personal investments in the body in the context of changing Nordic welfare states. In I. Harsløf & R. Ulmestig (Eds.), Changing social risks and social policy responses in the Nordic welfare states (pp. 165–188). London: Palgrave Macmillan.
Mackenbach, J. P., Stirbu, I., Roskam, A.-J. R., Schaap, M. M., Menvielle, G., Leinsalu, M., & Kunst, A. E. (2008). Socioeconomic inequalities in health in 22 European countries. New England Journal of Medicine, 358(23), 2468–2481.
National Board of Health. (2011). Hjerneskaderehabilitering – en medicinsk teknologivurdering [Brain injury rehabilitation – A medical technology assessment]. Copenhagen: National Board of Health.
Reay, D. (1998). ‘Always knowing’ and ‘never being sure’: Familial and institutional habituses and higher education choice. Journal of Education Policy, 13(4), 519–529.
Walford, G. (2009). For ethnography. Ethnography and Education, 4(3), 271–282.
Willis, K., Collyer, F., Lewis, S., Gabe, J., Flaherty, I., & Calnan, M. (2016). Knowledge matters: Producing and using knowledge to navigate healthcare systems. Health Sociology Review, 25(2), 202–216. https://doi.org/10.1080/14461242.2016.1170624.
World Medical Association. (2018). Declaration of Helsinki – Ethical principles for medical research involving human subjects. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects. Accessed 4 July 2018.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 The Author(s)
About this chapter
Cite this chapter
Højbjerg, K., Egerod, I., Poulsen, I. (2019). Transfer Practices During Acquired Brain Injury Rehabilitation: A Descent in the Medical Hierarchy. In: Harsløf, I., Poulsen, I., Larsen, K. (eds) New Dynamics of Disability and Rehabilitation. Palgrave Macmillan, Singapore. https://doi.org/10.1007/978-981-13-7346-6_11
Download citation
DOI: https://doi.org/10.1007/978-981-13-7346-6_11
Published:
Publisher Name: Palgrave Macmillan, Singapore
Print ISBN: 978-981-13-7345-9
Online ISBN: 978-981-13-7346-6
eBook Packages: Social SciencesSocial Sciences (R0)