Abstract
The concept of keyhole neurosurgery is not only to perform small incision and reduce the craniotomy size for the sake of a small opening as we called “keyhole,” but it is rather to make “minimum craniotomy” required to access deep intracranial lesions at the end of the route. Standard craniotomy forms a “funnel-shaped surgical corridor” to reach deeper area of the brain. In contrast, keyhole mini craniotomy forms a “reverse funnel-shaped surgical corridor” that provides adequate working space through a small incision and bone window to reach the target. The concept of this approach is that the deep area of the brain can be accessed through smaller craniotomy since the superficial optical field is widened if the size of craniotomy is bigger (Fig. 2.1).
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Basic Consept
The concept of keyhole neurosurgery is not only to perform small incision and reduce the craniotomy size for the sake of a small opening as we called “keyhole,” but it is rather to make “minimum craniotomy” required to access deep intracranial lesions at the end of the route. Standard craniotomy forms a “funnel-shaped surgical corridor” to reach deeper area of the brain. In contrast, keyhole mini craniotomy forms a “reverse funnel-shaped surgical corridor” that provides adequate working space through a small incision and bone window to reach the target. The concept of this approach is that the deep area of the brain can be accessed through smaller craniotomy since the superficial optical field is widened if the size of craniotomy is bigger (Fig. 2.1).
Intracranial aneurysm surgery using eyebrow keyhole approach has been reported by Van Lindert and Perneczky in 1998, and since then, this approach has been accepted as minimally invasive approach for aneurysm clipping surgery in addition to the existing standard approach.
2 Preoperative Planning
The planning and execution of the approach play a critical role in performing this keyhole surgery. The smaller the craniotomy, the greater the need for precise planning and self-made completion of the approach because the corridor of surgical dissection cannot be changed during the procedure.
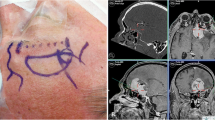
It is necessary to have preoperative consideration about the size and aneurysm dome projection, aneurysm location, perforating arteries, surrounding important structures, and how to plan the bone flap. Using excellent diagnostic facilities of CT , MRI , and digital subtraction angiography (DSA), one has today the possibility to demonstrate small details and specific anatomical orientation of the lesion related with surgical planning. In our experience, preoperative planning for eyebrow keyhole surgery is could be mainly by using and rely on 3D CT angiography (3D-CTA). The 3D reconstruction images maybe able to shows from the skin, then skull, cerebral arteries and veins, including size and shape of the aneurysm. The preoperative planning of the keyhole craniotomy can be simulated with 3D-CTA (Fig. 2.2).
Preoperative planning with 3D CTA images showing the skull, cerebral arteries, and aneurysm pathology. (a) The supraorbital keyhole craniotomy and its relationship to the aneurysm are well visualized. (b) The supraorbital craniotomy with the lesion is prepared at various angles to have an optimal microsurgical visualization
3 Step of the Approach
3.1 Positioning and Preparation
The surgeon must plan and perform the proper positioning of the patient by himself. Self-made preparation and positioning are essential for creating keyhole craniotomies. After the patient is anesthetized, the patient head is positioned in supine with head holder, and the head is higher up approximately 15° to facilitate venous drainage. A slightly chin-up position is preferable to support the frontal lobe that will slightly fall down according to the gravity force. The degree of head rotation should be determined by preoperative 3D simulation, but generally the head is rotated between 15° and 45° toward the contralateral side, determined by the location and dome projection of aneurysm. The placement of lumbar drain or extraventricular drainage also allows for brain relaxation specially in ruptured aneurysm case with brain edema .
Frontal anatomic landmarks should be precisely identified, including the foramen supraorbital, superior temporal line, orbital rim, and zygomatic arch, then drawing the skin incision plan on the skin (Fig. 2.3).
3.2 Skin Cut
The skin is cut according to the preoperative planning and anatomical orientation. The skin is cut at lateral two-thirds of the eyebrow , from supraorbital notch to the lateral part, sometimes extending few millimeters to the temporal line. To achieve a good cosmetic appearance, the incision should follow the orbital rim, in the hair line. It is advisable not to overuse bipolar coagulation to avoid damaging hair follicles and surrounding tissues. After skin incision, skin flap is dissected subcutaneously to obtain optimal exposure to surrounding muscles. We could clearly identify the frontal, orbicularis oculi and temporal muscles. After dividing the muscular layers gently, we have to identify pericranium at supraorbital edge, and it is cut perpendicularly following superior temporal line to get good bone exposure.
Skin flaps should be gently retracted with three or four temporary stiches at each upper and lower side of the flaps. The frontal muscle should be retracted upward, and the temporal muscle is detached gently from the attachment and retracted laterally to expose ipsilateral temporal line, and then keyhole area is exposed. Gentle detachment and pulling of the muscle are important to prevent local postoperative hematoma (Fig. 2.4).
3.3 Mini Craniotomy and Dural Incision
Making a single frontobasal burr hole at the frontozygomatic point just behind the temporal line by using high-speed drill. The placement and direction of the drilling procedure should be in correct manner. Wrong direction during drilling can cause the drill going into the orbit, while we actually want it to go to the anterior frontal floor. The craniotomy flap is then performed with high-speed craniotomy, starting from lateral orbital rim and following the orbital rim to medial, as long as 25–30 mm, then curving cranially about 15–25 mm, and cutting back to the burr hole site, thus creating a small bone flap. An important point is the bone cut should be very close and approaching orbital roof and if necessary additional drilling to make any prominence at the frontal floor totally flat. This may provide a few millimeters more exposure and avoid the bony prominence to obstruct surgical visualization and facilitate optimal microsurgical maneuvers using microscope and microinstruments (Fig. 2.5).
Opening the dura with semicircular shape and the base parallel along the orbital rim. The dura flap is reflected basally and fixed downward with three or four sutures so that dural window is formed in optimal opening following craniotomy corridor (Fig. 2.6).
3.4 Intradural Dissection
After opening the dura, the first-step maneuver is to gently remove sufficient cerebrospinal fluid by opening the arachnoid membrane through the chiasmatic and carotid cistern or furthermore to Sylvian fissure . Ventricular puncture and drainage sometimes may be needed in case of brain edema ; the authors only use the lumbar spinal drain for very selective cases. With adequate drainage of CSF (cerebrospinal fluid), the brain becomes relaxed, then a brain spatula is put in the frontal lobe, and the purpose is to protect the cortex and not to retract the cortex. With this efficient and adequate surgical corridor, we can get to the aneurysm precisely and avoid extensive cortical retraction (Fig. 2.7).
3.5 Closure and Bone Flap Replacement
After the intracranial procedure is performed, the next step is filling the intradural space with warm normal saline. Close the dura with watertight and interrupted sutures, and then make sure that any defects are well repaired. If the frontal sinus opened during the surgery, it is a must to seal off the frontal sinus to avoid postoperative infection. Bone flap is placed back, and hold it with mini plates and be careful not to penetrate frontal sinus by the screws. Authors prefer using three mini plate fixations at medial, lateral, and upper part of craniotomy to make sure a strong fixation to prevent postoperative deformity. Reapproximate the temporal muscle to zygoma by one or two sutures. After final hemostasis control, reapproximate the subcutaneous layer by interrupted sutures; then the skin is also closed by interrupted sutures in the eyebrow (Fig. 2.8).
4 Complications and How to Avoid
There are some complications that could be occurred associated with surgical technique in eyebrow keyhole approach.
-
1.
Temporary or permanent supraorbital hypesthesia. In eyebrow keyhole craniotomy, the surgical field is very narrow, and medially the surgical field is limited by supraorbital notch that contains supraorbital nerve . Perioperative anatomical landmark should be prepared precisely to avoid damaging these structures. Certainly, keeping a distance of the craniotomy site at least 5–10 mm lateral to the orbital notch can reduce the risk of supraorbital nerve injury. Sometimes stretching the nerve during surgery is unavoidable, but preserving the nerve continuity will provide good chance to have functional recovery after surgery.
-
2.
Frontal deformity. The frontobasal burr hole needs to be placed behind the temporal line after retracting the temporal muscle laterally. The burr hole site will be covered with the muscle to prevent deformity in this area. Proper repositioning of the bone flap is also an important step to prevent frontal deformity for a better cosmetic result. Bone flap should be fixed frontally and medially without any bony distance; make sure the mini plate tightly fixed the bone in proper position.
-
3.
Suboptimal cosmetic result. Skin incision should be made within the eyebrow and follow the orbital rim. Retraction of the skin flap should be in gentle manner to prevent soft tissue necrosis, and it is better to minimize the use of bipolar cauterization during skin and soft tissue procedures. The skin is closed with interrupted suture to have an optimal skin tension with good approximation.
-
4.
Infection . If the frontal sinus opened during procedure, careful repair is mandatory. The periosteum or fascia flap, bone wax, or abdominal fat tissue can be used to repair the injured sinus. Make sure the dura is closed watertightly with interrupted suture; if still dehiscence occurred, a small muscle patch should be used for this purpose.
5 Limitations
-
1.
This approach is contraindicated in patient with massive brain swelling after subarachnoid hemorrhage .
-
2.
This approach could not be a standard for all of aneurysm surgery; the indication should be strict and rely on the surgeon’s experience.
-
3.
The keyhole craniotomy may limit the microsurgery working angles, so it is mandatory to use a high magnification microscope and specific keyhole microsurgery instruments.
-
4.
It is preferred not to use this approach for patient with large frontal sinus, because the greater risk of infection may occur.
Bibliography
Jallo GI, Bognar L. Eyebrow surgery: the supraciliary craniotomy: technical note. Neurosurgery. 2006;59:ONSE157–8.
Mori K. Keyhole concept in cerebral aneurysm clipping and tumor removal by the supraciliary lateral supraorbital approach. Asian J Neurosurg. 2014;9:14–20.
Ormond DR, Hadjipanayis CG. The supraorbital keyhole craniotomy through an eyebrow incision: its origins and evolution. Minim Invasive Surg. 2013;2013:1–11.
Paladino J, Mrak G, Miklic JH, Mihaljevic D. The keyhole concept in aneurysm surgery—a comparative study: keyhole versus standard craniotomy. Minim Invas Neurosurg. 2005;48:251–8.
Perneczky A, Reisch R. Keyhole approaches in neurosurgery, vol. 1. Concept and surgical technique. Wien: Springer; 2008.
Reisch R, Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005;57:ONS242–55.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this book are included in the book's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the book's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2019 The Author(s)
About this chapter
Cite this chapter
Al Fauzi, A., Suroto, N.S., Bajamal, A.H. (2019). Eyebrow Keyhole Approach in Aneurysm Surgery. In: July, J., Wahjoepramono, E. (eds) Neurovascular Surgery . Springer, Singapore. https://doi.org/10.1007/978-981-10-8950-3_2
Download citation
DOI: https://doi.org/10.1007/978-981-10-8950-3_2
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-8949-7
Online ISBN: 978-981-10-8950-3
eBook Packages: MedicineMedicine (R0)