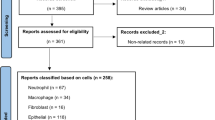
Abstract
The current treatments offered to patients with chronic respiratory diseases are being re-evaluated based on the loss of potency during long-term treatments or because they only provide significant clinical benefits to a subset of the patient population. For instance, glucocorticoids are considered the most effective anti-inflammatory therapies for chronic inflammatory and immune diseases, such as asthma. But they are relatively ineffective in asthmatic smokers, and patients with chronic obstructive pulmonary disease (COPD) or cystic fibrosis (CF). As such, the pharmaceutical industry is exploring new therapeutic approaches to address all major respiratory diseases. The previous chapters demonstrated the widespread influence of purinergic signaling on all pulmonary functions and defense mechanisms. In Chap. 8, we described animal studies which highlighted the critical role of aberrant purinergic activities in the development and maintenance of chronic airway diseases. This last chapter covers all clinical and pharmaceutical applications currently developed based on purinergic receptor agonists and antagonists. We use the information acquired in the previous chapters on purinergic signaling and lung functions to scrutinize the preclinical and clinical data, and to realign the efforts of the pharmaceutical industry.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
9.1 Introduction
For nearly 30 years, extracellular purines have been suspected to play important roles in the pathogenesis of chronic respiratory diseases. In the 1980s, Cushley et al. reported that inhaled ADO causes bronchoconstriction in asthmatic patients, but not in healthy subjects [1]. Later, it was discovered that asthmatics maintain high airway ADO levels, which is further raised following a challenge [2, 3]. In the past 5 years, the list of respiratory diseases with aberrant airway ADO and/or ATP regulation was extended to CF, COPD and idiopathic pulmonary fibrosis [4–6] (see Chap. 4 for details). Also, the recent finding that ADO induces bronchoconstriction in smokers with COPD supports a role in the “overlapping syndrome” [7–9]. Such widespread occurrence of excess airway ADO motivated scientists and clinicians to investigate the implications of this metabolic aberrance in all aspects of chronic respiratory diseases.
The consequences of excess ADO for lung homeostasis were clearly demonstrated by mice lacking adenosine deaminase (ADA) (review: [10]). These ADA−/− mice develop bronchial hyperresponsiveness (BHR), severe lung inflammation, mucin hypersecretion, sub-epithelial fibrosis, basement membrane thickening, smooth muscle cell hyperplasia and a disruption of the alveolar network typical of emphysema (see Chap. 8 for details). This stunning discovery launched a series of initiatives to identify which ADO and ATP receptors promote, or attenuate, lung complications. The previous chapters were carefully organized to describe all purinergic receptors, their properties, distribution and roles on the lung resident, immune and inflammatory cells. Chapter 8 described the animal studies that were conducted to compare their impact on lung homeostasis and the potential of selective ligands for the treatment of chronic respiratory diseases.
This final chapter describes the progress made, over the past 15 years, in this new field of drug development. First, evidence is provided for the higher diagnostic stringency of ADO-induced BHR for asthma, with respect to histamine and methacholine. Then, we tell the tale of Adagen (Enzon Pharmaceuticals), which was designed for the treatment of ADA-related severe combined immunodeficiency (ADA-SCID), but shows considerable potential for the correction of airway ADO levels in chronic airway diseases. Finally, this chapter covers the ADO and ATP receptor ligands selected by pharmaceutical companies for the treatment of acute lung injury and chronic respiratory diseases, and to improve the outcome of lung transplant. Based on the current understanding of purinergic signaling in the respiratory system, this section offers a critical view on the design of the ligands and the delivery route, which may assist the pharmaceutical industry in future drug discovery.
9.2 AMP Challenges: Diagnostic Tool and Signaling Pathways
Airflow obstruction is a characteristic feature of airway diseases, including asthma and COPD. Adenine nucleotides and nucleosides have been shown to trigger immediate airflow obstruction in asthmatic patients following aerosolized administration. Since the bronchoconstriction does not occur in normal subjects, adenosine monophosphate (AMP) has been used worldwide to detect and monitor bronchial hyperresponsiveness (BHR), as a tool to diagnose asthma and guide therapy. In this section, we review the clinical use of AMP challenges, and the current knowledge on the mechanism of action.
9.2.1 Using AMP as a Diagnostic Tool
In 1983, Cushley, Tattersfield and Holgate were the first to report that inhalational exposure to ADO resulted in a concentration-dependent bronchoconstriction in allergic and non-allergic asthmatic patients [1]. In contrast, ADO concentrations up to 30-fold higher had no effect on the airway caliber of normal subjects [11]. Adenine nucleotides, ADP and AMP, also elicited airway narrowing in asthmatics, while the ADO metabolite, inosine, did not induce bronchoconstriction [12]. The airway epithelial surfaces express ectonucleotidases which rapidly dephosphorylate adenine nucleotides into ADO (see Chap. 2 for details). While it is well accepted that the effects of these nucleotides on airway caliber are mediated by ADO, AMP remains the drug of preference for solubility purposes (review: [13]).
Prior to the observations of Cushley et al. [1], pharmacological tests for BHR relied on direct airway challenges with methacholine or histamine. These substances activate M3 muscarinic receptors and H1 histamine receptors on airway smooth muscle (ASM) to elicit bronchoconstriction in asthmatics at concentrations having no effect in the airways of normal subjects. While the sensitivity and negative predictive values of methacholine and histamine challenges approach 100%, their specificity and positive predictive values for asthma are very low [14–17]. In fact, adult COPD patients and children with bronchiectasis, bronchiolitis obliterans or CF, typically develop BHR in response to methacholine and histamine [18–22]. In contrast, non-smoking adults with COPD and children with airway diseases other than asthma are less responsive to an AMP challenge [7–9, 22, 23]. This higher specificity for asthma suggests that aerosol AMP may constitute a powerful diagnostic test to differentiate these airway diseases in children and non-smoking adults. Furthermore, contrary to methacholine, the magnitude of the BHR response to AMP is highly correlated with the degree of underlying airway inflammation in asthmatics [24, 25].
For these reasons, measurement of BHR by AMP challenge has been endorsed by the European Respiratory Society Task Force on indirect airway challenges [26]. It is more specific for asthma than methacholine and histamine challenges [22, 27], correlates more closely with the degree of inflammation in the lower airways [24, 25], and may be used to evaluate the efficacy and potency of inhaled steroids [28–31]. However, the sensitivity of an AMP challenge to detect asthma is limited, the rate of AMP responsiveness varying from 39% to 95.5% in children [32–35] and 50% to 89% in adults [24, 36]. The studies reporting a high degree of sensitivity included large numbers of atopic asthmatics. Accordingly, a study designed to elucidate the determinants of AMP responsiveness revealed that atopic sensitization, assessed by positive skin prick testing, was the major variable affecting AMP sensitivity [32]. Compared to non-atopic asthmatics, atopic asthmatics exhibit exaggerated mast cell activation by antigens and allergens. Consequently, these cells have been the focus of intense investigation to better understand the mechanisms of ADO-induced bronchoconstriction.
9.2.2 Signaling Pathways of Bronchoconstriction
The signaling pathways responsible for AMP-induced BHR have been extensively investigated using its active metabolite: ADO. This ubiquitous signaling molecule has been shown to regulate the activities of all mammalian cell types through the activation of cell surface G protein-coupled receptors. Four P1 receptors have been identified and are widely expressed: A1Rs, A2ARs, A2BRs, and A3Rs. The studies conducted in humans and animals support three potential mechanisms for ADO-induced bronchoconstriction targeting different cell types: mast cells, ASM and neurons (Fig. 9.1).
Mechanisms of adenosine-induced bronchoconstriction in human airways. Adenosine (ADO; red) can induce muscle contraction directly via A1 receptors (A1R) located on airway smooth muscle (ASM). These receptors are also expressed by the sensory neurons, allowing ADO to induce the release of acetylcholine (Ach; green). This neurotransmitter can induce muscle contraction directly via muscarinic receptors on ASM, or indirectly by the stimulation of histamine release (blue) from mast cells
The first argument supporting a mast cell-dependent mechanism was provided by a clinical study reporting the accumulation of histamine in the airways of asthmatic patients in response to endobronchial ADO [37]. Accordingly, ADO-induced BHR was attenuated by mast cell stabilizing agents (i.e. nedocromil) [38–40] and antagonists of the histamine receptor (i.e. terfenadine) [41–43] or leukotriene receptor (i.e. Montelukast) [44]. These studies led many to believe that ADO-induced bronchoconstriction results from mast cell activation. In rodents, the P1 receptor causing mast cell degranulation was identified as the A3R [45–48], whereas this role was ascribed to the A2BR in human mast cells [49–51]. Nonetheless, aerosolized treatment with a dual A2BR/A3R antagonist (QAF805) failed to affect PC20 (provocative concentration required to induce a 20% fall in lung function) in asthmatics [52], suggesting that ADO induces bronchoconstriction by other mechanisms.
Human and animal studies suggest that A1Rs located on ASM mediate the ADO-induced bronchoconstriction. On cultures of human ASM, A1R activation stimulated cell contraction by the mobilization of intracellular Ca2+ stores [53]. Their tissue expression was confirmed by immunolocalization in biopsy sections, which also showed that A1Rs are overexpressed in the airway epithelium and ASM of asthmatics [54]. Furthermore, the incubation of normal ASM cultures with serum from asthmatic patients induced the up-regulation of A1Rs [55]. Incidentally, animal studies conducted with A1R agonists and antagonists also support a role for A1Rs located on ASM in ADO-induced BHR [56–58]. The use of knockout mice targeting each P1 receptor revealed that only A1R−/− mice fail to react to an ADO challenge [59]. On the other hand, ADO-induced bronchoconstriction was abolished following bilateral vagotomy [59], suggesting a role for sensory neurons.
In asthmatic patients, AMP-mediated BHR was attenuated by the anticholinergic drug ipratropium, and by depletion of contractile neuropeptides with bradykinin [60, 61]. These studies support a role for cholinergic neural pathways in the bronchoconstrictor response to ADO. In allergic (not naïve) guinea pigs, the fact that bilateral vagotomy or capsaicin strongly inhibited airway obstruction to AMP (75%), or an A1R agonist (N(6)-cyclopentyladenosine; CPA) (50%), suggests that cholinergic neural input to the ASM is critical for A1R-mediated bronchoconstriction [62]. In human airways, acetylcholine can activate muscarinic receptors on ASM and mast cells (review: [63]). Whether cholinergic mediators induce ASM contraction directly, or through mast cell activation, has not been determined.
9.2.3 Summary
Recent studies on the signaling pathways responsible for ADO-induced BHR have revealed important clues about the airway pathophysiology of asthma, by uncovering a complex interplay between mast cells, neurons and ASM. The continuous investigation of the mechanisms by which nucleotides and nucleosides influence airway caliber in the asthmatic lung may lead to the exploitation of these pathways for therapeutic approaches. For instance, future studies comparing the relative impact of A1R and A2BR antagonists on AMP-mediated BHR may reveal a more prominent role for A2BR-mast cell signaling in the atopic asthmatic patients. Meanwhile, AMP challenges remain an important tool for clinicians and researchers sharing common interests in the diagnosis and treatment of asthma and other respiratory disease.
9.3 Adenosine Deaminase Replacement Therapies
9.3.1 Current Clinical Application for ADA-SCID
As part of the purine salvage pathway, intracellular ADA is responsible for the deamination of ADO and deoxyadenosine into inosine and deoxyinosine, respectively [64]. Over 50 mutations spanning the entire Ada gene have been identified, 29 of them resulting in >85% reduction of ADA activity [65, 66]. These functional mutations allow toxic levels of substrates to accumulate and interfere with the development of thymocytes in the thymus and bone marrow, which prevents or weakens the immune responses to infection [67]. Accordingly, inherited ADA deficiency is catalogued as an autosomal recessive immunodeficiency disorder exhibiting a wide range of severity, depending on the level of residual activity: (1) a neonatal and fatal severe combined immunodeficiency disease (SCID) characterized by the absence of cellular and humoral immunity; (2) a delayed onset progressive disease retaining some humoral immunity; (3) a late juvenile onset with progressive attrition of immune defenses; (4) an adult onset disorder [66]. With respect to lung complications, they exhibit recurrent otitis, sinusitis, chronic bronchitis and pneumonia, the severity correlating negatively with ADA activity [68].
Over the years, many therapeutic approaches have been explored for ADA-SCID patients. The best option remains an allogenic bone marrow transplant, which generally leads to complete recovery [69]. In the event that a histocompatible sibling is unavailable, these patients are administered irradiated purified erythrocytes as a source of functional ADA [70]. Unfortunately, this approach only provides a partial and transient recovery of immune functions, and long-term infusions give rise to various complications [71].
In 1981, Stephen Davis proposed that covalent linking of purified bovine ADA to polyethylene glycol (PEG) would prolong its half-life and reduce its antigenicity [71]. This approach proved successful in laboratory animals, extending the half-life of ADA activity in mouse serum from 30 min for the naked protein to 28 h for PEG-ADA. The antigenic properties were virtually eliminated as well, as the serum from mice receiving intravenous PEG-ADA was unable to immunoprecipitate ADA or PEG-ADA, even after repeated injections over a period of several weeks. The circulating PEG-ADA was also able to reduce the intracellular levels of ADO [71] due to the ubiquitous expression of transporters in the plasma membrane of mammalian cells (see Chap. 2 for details).
In 1985, Michael Herschfield initiated the therapeutic evaluation of PEG-ADA (Adagen; Enzon Pharmaceuticals) in ADA-SCID patients. The therapy successfully reduced tissue ADO concentrations and dramatically improved immune functions [69]. However, the levels of T, B and natural killer lymphocytes rose over the first few years, but never reached normal values. Also, about 65% of the patients developed antibodies against PEG-ADA within the first year. Their lymphocyte levels began to drop, as they faced a steady decline in immune function. Another major obstacle to this therapy was the cost of biweekly injections of PEG-ADA, which rose to $200,000/year [72]. These serious limitations called for alternative approaches for the restoration of ADA.
Future directions in the treatment of ADA-SCID include the genetic replacement of ADA function (review: [73]). Over nearly two decades, the gene therapy consisted almost exclusively in the use of retroviral vectors targeting the lymphocytes and hematopoietic progenitors. Patients were successfully colonized by hematopoietic stem cells transfected with the ADA gene, following partial ablation of the bone marrow [74]. However, this groundbreaking approach came with the risk of inspectional mutagenesis. Recent studies suggest that this highly invasive protocol may be replaced by ex vivo lentiviral therapy. In ADA-deficient mice, the intravenous injection of human immunodeficiency virus 1-based lentiviral vector at birth induced the long-term expression of enzymatically active ADA at levels comparable to long-term PEG-ADA treatments [72]. This approach effectively restored immune function and significantly extended survival. As such, this non-invasive method may provide long-term restoration of ADA activity in ADA-SCID patients.
9.3.2 Long-Term Treatments for Pulmonary Diseases
Despite the development of successful treatments for ADA-SCID, the underlying causal link between the metabolic disturbances and associated immunodeficiency were unknown. An animal model of ADA deficiency was developed to investigate this link, but the ADA−/− mice suffered from a perinatal lethality due to hepatotoxicity [75]. This complication was circumvented using an ADA minigene possessing only the promoter elements required for expression in the trophoblast, which preserved liver function [76]. These partially ADA-deficient mice were born without ADA activity, as evidenced by a steady accumulation of the ADA substrates: ADO and deoxyadenosine. They displayed typical immunodeficiency in the lymphoid line for ADA-SCID patients [77]. In addition, these mice developed severe pulmonary complications, characterized by BHR to inhaled ADO [78], inflammatory cell infiltration and mucus hypersecretion [77]. The defective alveogenesis resulted in an emphysema-like phenotype by postnatal day 10, and the mice died by postnatal day 21 due to respiratory distress [79] (see Chap. 8 for details). These studies demonstrate that the high systemic ADO levels of SCID patients are responsible for the development of severe lung complications. More importantly, they suggested that the high airway ADO levels of asthmatic [3, 80, 81] and COPD [82] patients promote the inflammation, remodeling and fibrosis leading to BHR and the loss of lung function.
The therapeutic potential of PEG-ADA for chronic respiratory diseases was tested in the ADA−/− mice. The animals treated with intramuscular PEG-ADA from birth did not develop any lung complication [83]. On the other hand, ADA−/− mice which develop lung inflammation over 20 days completely recovered after 3 days of PEG-ADA treatment at a dose that fully restored normal lung ADO levels [79]. Interestingly, the microarray analysis of lung tissue revealed that PEG-ADA restored the normal expression of genes critical for inflammatory responses, as well as factors promoting remodeling and fibrosis. This observation supported the therapeutic potential of PEG-ADA for patients with well-established chronic respiratory diseases. This hypothesis was tested using ADA−/− mice maintained on a low-dose PEG-ADA regimen from birth, which prolonged their lifespan to 4–5 months [84]. After 3 months, the resulting intermediate ADO level fostered the development of severe pulmonary inflammation, collagen deposition and alteration in airway structure. Their BAL fluid accumulated, both, pro-inflammatory and pro-fibrotic mediators (IL1β, osteopontin, MMP12, TGFβ, and PAI-1). All these complications were fully resolved by shifting these mice to high-dose PEG-ADA for 5 weeks.
This animal model clearly demonstrated the dramatic consequences of high ADO levels reported in the airways of asthmatic and COPD patients (see Chap. 4 for details), and the therapeutic potential of PEG-ADA for all lung complications, including fibrosis.
9.3.3 Suppression of the ADO/IL-13 Amplification Cycle
Clinical studies showed that the airways of asthmatic, CF and COPD patients also accumulate the cytokine: IL-13 [85–87]. An earlier report of normal IL-13 concentration in COPD sputum [88] may have resulted from the use of enzyme-linked immunoassay, instead of the more sensitive cytometric bead array, as the authors only detected IL-13 in 6/34 patients. In CF patients, a significant negative relationship was established between airway IL-13 levels and lung functions [86]. The significance of IL-13 for chronic airway diseases is supported by the plethora of studies which identified this cytokine as upstream element responsible for the imbalance in metalloproteinase production promoting airway remodeling (reviews: [89, 90]). Incidentally, IL-13 transgenic mice develop mucus cell metaplasia, hypersecretion and sub-epithelial fibrosis [91, 92]. Interestingly, they share many phenotypic traits with the ADA-deficient mice, including eosinophilia, emphysema and fibrosis, and they survive less than 4 months [92]. The development of these lung complications coincides with a steady rise in lung ADO level and reduction in lung ADA activity. One month of PEG-ADA treatment corrected the ADO levels and significantly reduced inflammation, mucin secretion, collagen deposition and emphysema [91].
The existence of an amplification cycle for lung IL-13 and ADO regulation is also supported by the fact that ADA−/− mice overexpress IL-13, which was corrected by PEG-ADA treatment [91]. It is proposed that excess ADO, generated in stressed and damaged tissues, induces an up-regulation of IL-13 and recruits inflammatory cells. This cytokine initiates airway remodeling and down-regulates ADA, resulting in further ADO accumulation, which completes the cycle. Consequently, many aspects of chronic airway diseases could be addressed by ADA replacement therapy, by the concomitant reduction of ADO- and IL-13-mediated responses.
9.3.4 Summary
The current literature highlights the tremendous potential of PEG-ADA to identify the inflammatory, remodeling and fibrotic processes targeted by the excess airway ADO of asthmatic and COPD patients. This remarkably stable compound also has the potential of becoming an effective therapy for a variety of lung diseases dominated by fibrosis and emphysema, that is, if the pharmaceutical industry can reduce the cost of the treatments. At Enzon Pharmaceuticals, PEG-ADA (pegademase bovine) has been prescribed for over 20 years for the treatment of ADA-SCID under the name: Adagen. Patents were recently issued for therapeutic applications in pulmonary diseases, and clinical trials are pending. It is important to note that ADA offers no therapeutic benefit unless pegylated, which provides the metabolic stability. Since this discovery, this stabilizing technique has been applied to a number of bioagents, including interferons (review: [93]).
9.4 Clinical Trials Involving Adenosine Receptors
There are dozens of ADO receptor ligands currently designed by various research laboratories and pharmaceutical companies. This activity has provided pharmacological tools to distinguish the roles of each ADO receptor in the regulation of airway defenses. For details on the strategies behind their structural design, the readers are redirected to excellent reviews for A1Rs [94], A2ARs [95, 96], A2BRs [97, 98] and A3Rs [99]. This chapter focuses on the ligands selected for preclinical and clinical evaluation. In each case, the experimental designs (animal models, delivery routes) chosen to evaluate their therapeutic potential are weighed against the knowledge we have acquired in the first eight chapters of this book, regarding ADO regulation and cell-specific functions.
9.4.1 The A1R Antagonists
The animal models of chronic respiratory diseases predict that A1R antagonists may attenuate BHR, mucin hypersecretion and lung inflammation (see Chap. 8 for details). These bioagents would take advantage of the high A1R expression reported on the airway epithelial and smooth muscle cells of asthmatic patients [54]. On the other hand, smoking was recently reported to down-regulate A1Rs on inflammatory cells [100], suggesting that A1R antagonists may be less effective in smoking asthmatics and most COPD patients. In terms of delivery route, systemic delivery of A1R antagonists in oral capsules would more efficiently prevent the migration of dendritic cell to the lymph nodes, as well as leukocyte adhesion to the endothelial barrier (see Chap. 7 for details). With all this information in mind, we will review the current preclinical and clinical studies with a critical view of the drug development strategies adopted for A1R antagonists.
9.4.1.1 Mixed Theophylline/Corticosteroid Treatments
Chemical structure: 1,3-dimethylxanthine
The first report of methylxanthines for the treatment of bronchoconstriction was published in 1859 by an asthmatic, Henry Hyde Salter, who described the effects of a strong coffee on his airway symptoms (review: [101]). In the 1920s, Theophylline was demonstrated to relax airway smooth muscle, and was prescribed orally for the treatment of airway hyperresponsiveness [102]. In the 1970s, Theophylline was a popular treatment for stable asthmatic patients. Unfortunately, the dose needed to initiate bronchodilation often induces cardiovascular and gastric side-effects. This drug became less popular as more effective β2 adrenoceptor agonists became available.
Over the past decade, Theophylline was revisited using lower doses (0.1–0.5 mg) avoiding most side-effects caused by phosphodiesterase inhibition. Under these conditions, Theophylline exerts potent anti-inflammatory effects, predominantly as an A1R antagonist (review: [103]). In the OVA sensitization/challenge model of allergic asthma, low dose Aminophylline (Theophylline pro-drug) given intraperitoneal prevented early and late phase airway hyperresponsiveness to an OVA challenge, and reduced the inflammatory markers in BAL fluid (IL-4, IL-5, IL-6, IL-10 and TNFα) [104].
In 2006, the anti-inflammatory potential of low-dose Theophylline for asthmatic patients was tested in a clinical study using Aminophylline [105]. A single intravenous injection significantly improved the lung functions, measured as peak expiratory flow (PEF) and peripheral oxygen saturation (SpO2). These clinical benefits were comparable to those of aerosolized Salbutamol, a β2 adrenoceptor agonist. Also, Aminophylline (but not Salbutamol) reduced pulmonary inflammation, measured in BAL fluid as eosinophil cationic protein, histamine, serotonin, thromboxane B2, leukotriene C4.
Nowadays, clinicians refine the treatment of asthma and COPD by combining the bronchodilating effect of inhaled corticosteroids with the anti-inflammatory effect of low dose oral Theophylline [106–108] (Table 9.1). In July 2010, the Theophylline extended-release tablet was granted marketing approval by the United States FDA.
9.4.1.2 Bamiphylline Approved in Europe
Chemical structure: 8-benzyl-7,[2-[ethyl(2-hydroxyethyl)amino]-ethyl] Theophylline Trentadil; bamifylline; benzetamophylline, Cloperastine
Over the years, more selective A1R antagonists were designed to avoid the side-effects associated with Theophylline. Several clinical trials, conducted over the past 20 years, reported the potential of Bamiphylline for the treatment of bronchoconstriction and mucin clearance in asthmatic and COPD patients. In 1991, a placebo-controlled study was conducted with COPD patients matched for age [109]. The 7-day oral treatment significantly improved lung functions, based on the breathing pattern, inspiratory muscle strength, neural drive and index of inspiratory neuromuscular coupling.
In 1995, a double-blind clinical study assessed the effect of Bamiphylline on mucus clearance in 20 smokers with chronic bronchitis, compared to healthy controls [110]. All subjects received oral Bamiphylline (600 mg per day) or placebo during 15 days. Only the Bamiphylline treated COPD patients exhibited better mucus clearance, clinical score and pulmonary function, with no reported side-effects. This study suggests that Bamiphylline could improve mucus clearance in other chronic obstructive diseases, such as CF.
Oral Bamiphylline has been approved for the treatment of asthma and COPD in Europe, where it shows low incidence of side-effects, such as headaches or gastralgia (1/100,000 patients) [111]. This drug is also sold, as a cough suppressant, by Biocure Pharmaceutical under the name of cloperastine.
9.4.1.3 Is L-97-1 Better than Montelukast?
Chemical structure: [3-[2-(4-aminophenyl)-ethyl]-8-benzyl-7-{2-ethyl-(2-hydroxy- ethyl)-amino-ethyl}-1-propyl-3,7-dihydro-purine-2,6-dione]
Based on the success story of Bamiphylline, Mustafa et al. developed a selective antagonist of this receptor: L-97-1 [57]. Radioligand binding analysis showed a strong affinity for A1Rs (IC50 = 1.42 μM) compared to A2ARs and A2BRs (IC50 > 100 μM). This is a considerable improvement from Bamiphylline, in terms of affinity and selectivity.
In the house dust mite sensitization/challenge model of allergic asthma, the oral gavage of L-97-1 prevented the BHR to the final challenge for at least 6 h [57]. This treatment also inhibited late allergic responses, measured after 24 h, by histamine-induced bronchoconstriction. Therefore, L-97-1 has the potential to prevent early and late allergic responses in asthmatic patients.
Mustafa et al. also used this animal model to compare the efficiencies of L-97-1 and Montelukast [112], a cysteinyl leukotriene-1 receptor antagonist regularly prescribed to asthmatic patients for the treatment of reversible airflow limitation [113]. First, L-97-1 pretreatment maintained lung dynamic compliance higher than Montelukast over at least 5 h after a house dust mite challenge. Second, L-97-1 blocked both early and late allergic responses, whereas Montelukast only blocked the late response. Finally, both drugs caused comparable anti-inflammatory effects, in terms of leukocyte accumulation in BAL fluid. In summary, L-97-1 is an anti-inflammatory drug as potent as Montelukast, with the added benefit of a more efficient treatment of reversible airflow limitation.
The small water-soluble molecule, L-97-1, is under development as oral treatment for asthmatics by Andacea Inc., a company devoted to purinoceptor-based technologies.
9.4.1.4 EPI-2010: A Respiratory Antisense Oligodeoxynucleotide
In 2006, Drs Fire and Mello were awarded the Nobel Prize for discovering the mechanism behind RNA interference in 1998 (review: [114]). The regulation of gene expression through “silencing” was found essential for many cellular processes. The immense impact of this discovery on biomedical research led to the development of a new generation of aerosolized drugs for chronic respiratory diseases. In 1999, Metzger and Nyce designed respirable antisense oligonucleotides (RASONs) as short, single-stranded nucleic acid sequences modified to enhance their stability [58]. They bind the initiation codon of the messenger RNA (mRNA), which prevents translation and targets the message for degradation by RNAses. A clear advantage over traditional drugs is that they are metabolized locally by endogenous nucleases, confining their reactivity to the airways (review: [115]).
During a joined venture with Chiesi Pharmaceuticals and Taisho Pharmaceuticals, EpiGenesis Pharmaceutical developed the A1R-specific RASON, named EPI-2010, for the treatment of asthma [116]. A fortuitous homology between the human and rabbit mRNA sequences of the A1R allowed EPI-2010 to be tested in the model of allergic asthma described above for L-97-1. Following house dust mite sensitization, nebulized EPI-2010 caused a dose-dependent attenuation of airway hyperresponsiveness to ADO [58]. The fact that EPI-2010 also reduced airway obstruction caused by house dust mite and histamine challenges supported the existence of an anti-inflammatory effect. In these animals, EPI-2010 was deposited throughout the lung, with no detectable systemic active metabolites, and was excreted primarily in the urine. This original study demonstrated that RASONs can be efficiently delivered to the peripheral lung, where they potently and selectively attenuate the expression of disease-associated genes. In primates, EPI-2010 attenuated the allergen responses to Ascaris lumbricoides for about 7 days, which corresponds to the kinetics of A1R expression. Hence, EPI-2010 may represent the first once-a-week treatment for asthma.
In 2003, a Phase 1 clinical trial conducted on asthmatic patients demonstrated that aerosolized EPI-2010 is well-tolerated and shows indications of efficacy [116]. A single dose reduced the need for bronchodilator drugs and the symptom scores during about 1 week. However, because of the disappointing results of a Phase 2 clinical trial, EPI-2010 was discontinued from clinical testing [117]. In this study, 146 patients with persistent airway obstruction (FEV1 = 74.5% predicted; ≥12% reversibility), currently receiving inhaled corticosteroids, were administered EPI-2010 (1, 3, or 9 mg) through a nebulizer once or twice weekly. In asthmatic patients under corticosteroid treatment, EPI-2010 caused no significant change in lung function or inflammatory responses over 29 days.
Some arguments still support the therapeutic potential of inhaled EPI-2010 for asthmatic patients. In the above clinical trial, the patients had mild-to-moderate asthma, depending on the frequency of symptoms and the variability in peak expiratory flow rate. Despite the apparent stable FEV1 of 74.5% predicted, corticosteroids will raise the FEV1 values to 90–100% of predicted between exacerbations. Consequently, measurements of FEV1 do not constitute a sensitive assessment of asthma severity, compared to the acute changes in airway function caused by bronchoprovocation. This trial should have tested the therapeutic potential of EPI-2010 in asthmatic patients not receiving corticosteroid treatments, and using challenged BHR responses as parameter of clinical benefit. Also, because of safety concerns about the use of antisense oligonucleotides in humans, the doses of EPI-2010 may have been sub-therapeutic.
For these reasons, the scientific and clinical communities both support further investigation of aerosolized EPI-2010 for the attenuation of BHR in asthma and COPD. On the other hand, the current information on A1Rs suggests that oral delivery would provide a more potent anti-inflammatory treatment of chronic lung diseases.
9.4.2 The A2AR Agonists
The animal studies and known functions of A2ARs predict that agonists would be prescribed primarily for the treatment of chronic lung inflammation (see Chap. 8 for details). However, this approach faces a serious challenge, as A2AR expression and/or surface affinity are reduced in the lungs of asthmatic and COPD patients [100, 118]. Since these ligands have been shown to cause significant cardiovascular side-effects, including hypotension, strategies have been designed to confine the drugs to the airways. On the other hand, this flaw has been exploited for the benefit of patients undergoing elaborate surgical procedures, such as lung transplant, to prevent the resulting increase in pulmonary arterial blood pressure. This section reviews the A2AR agonists which were selected for preclinical and clinical evaluation of these two major applications.
9.4.2.1 CGS21680 More Efficient than Budesonide
Chemical structure: 2-p-(2-carboxyethyl)phenethylamino-5'-N ethylcarboxamido adenosine hydrochloride
The animal studies described in Chap. 8 clearly support the use of A2AR agonists for the treatment of lung inflammation in chronic respiratory diseases. However, the drug should be administered as an aerosol because systemic injection has been shown to cause considerable cardiovascular side-effects, including hypotension in human subjects [119]. Therefore, studies were conducted to test the safety and efficacy of the aerosolized A2AR agonists in animal models of airway diseases.
The first study evaluated the potential of CGS21680 in an animal model of allergic asthma. In OVA sensitized/challenged Norway rats, intratracheal CGS21680 given 15 min before and after the final challenge reduced eosinophil and neutrophil counts in the BAL fluid [120]. Similar findings were obtained in OVA sensitized/challenged mice [121]. In addition, CGS21680 was found ten times more efficient than Budesonide [121], a corticosteroid currently prescribed to asthmatic patients (review: [122]). On the other hand, CGS21680 did not address OVA-induced bronchoconstriction or mucin secretion, as expected from the pharmacological properties of the A2AR (see Chap. 8 for details). And these doses caused significant hypotension in the anesthetized animals, which may limit the clinical utility (Table 9.2).
Aerosolized CGS21680 did not prevent the development of lung inflammation in two models of acute lung injury: intranasal LPS and cigarette smoke inhalation [121]. In Chap. 8, we provided evidence that the microvascular endothelial barrier constitutes the primary target for the treatment of acute lung injury, as A2AR activation inhibits vascular leakage and inflammatory cell infiltration. In the LPS- and smoke-challenged mice, the lack of effect of intranasal CGS21680 may reflect a poor choice of delivery route.
A study showed that rats subjected to hemorrhagic shock, then given intravenous CGS21680 during resuscitation, developed significantly less acute lung injury than the untreated animals, in terms of vascular leakage and BAL myeloperoxidase activity [123]. This study suggests that the systemic administration of CGS21680 may prevent the acute development of lung injury in situations where blood pressure is monitored.
9.4.2.2 GW328267X: Flaw in the Design
Chemical structure: (2R,3R,4S,5R)-2-{6-amino-2-[(1-benzyl-2-hydroxyethyl)amino]-9H-purin-9-yl}-5-(2-ethyl-2H-tetrazol-5-yl)tetrahydrofuran-3,4- diol
The company GlaxoSmithKline identified a new selective agonist for the A2AR: GW328267X [124]. Binding studies conducted in Chinese hamster ovary cells showed that this high-affinity (pKi = 7.8) ligand is a potent agonist (pEC50 = 9.0) of the A2AR. This compound has a lower affinity for A1Rs and A2BRs (pKi ≤ 6) and shows relatively weak agonist activity at these receptors. In vitro assays demonstrated that GW328267X inhibits neutrophil and eosinophil activities (oxidative stress and degranulation), which are antagonized by an A2AR antagonist, CGS15943. However, GW328267X also binds A3Rs (pKi = 7.8) as a competitive antagonist. Hence, GW328267X activates A2ARs and blocks A3R-mediated responses equally well. Since A3Rs mediate neutrophil elastase secretion [125], this drug would offer additional protection as a blocker of this receptor.
In 2007, the company published results from two clinical studies conducted to evaluate the therapeutic potential of GW328267X for allergic rhinitis [126] and allergic asthma [127]. In a randomized, double-blind, placebo-controlled, three-way balanced, crossover study, 48 men with allergic rhinitis where challenged with house dust mite. Then, they received a nasal spray of GW328267X (50 μg) or Fluticasone (200 μg) twice daily [126]. The corticosteroid is currently prescribed for the treatment of allergic rhinitis. After 7 days, the patients given GW328267X had improved nasal blockage, but not peak nasal inspiratory flow, whereas Fluticasone significantly improved both parameters. Intranasal GW328267X also produced a small, but significant, reduction of inflammatory marker concentrations in the BAL fluid (tryptase and eosinophil cationic protein), while Fluticasone normalized the concentrations of eosinophil cationic protein and neutrophil chemoattractant IL-8. It was concluded that this novel A2AR agonists has limited clinical benefit for the treatment of allergic responses.
In the second double-blind, placebo-controlled, three-way balanced crossover study, 15 non-smoking atopic asthmatic patients, not under corticosteroid treatments, were challenged with house dust mite, then inhaled GW328267X (25 μg) or Fluticasone (200 μg) twice daily for 7 days [127]. The A2AR ligand did not protect against early and late asthmatic reactions, or significantly attenuate the inflammatory responses. And higher doses caused considerable side-effects, in terms of hypotension and tachycardia. In contrast, Fluticasone completely inhibited the early and late asthmatic responses, and significantly suppressed inflammation, including the lung eosinophilia. Given such low therapeutic index, GlaxoSmithKline discontinued the evaluation of GW328267X.
The failure of GW328267X to provide therapeutic benefits to allergic patients is consistent with the properties of this complex ligand. First, chronic airway diseases, in humans and animal models, are associated with a dramatic down-regulation of A2ARs (see Chap. 8 for details). Second, the antagonistic effect of GW328267X on A3Rs is expected to inhibit the degranulation of eosinophils, but to promote their recruitment to the lungs [128]. As such, this drug could not suppress allergic airway inflammation.
9.4.2.3 New UK371,104 Remains in the Lungs
Chemical structure: N-(2,2-diphenylethyl)-2-{[(2-piperidin-1-ylethyl)amino] carbonyl}adenosine
In 2008, Pfizer Inc. presented a new selective A2AR agonist carefully designed to minimize side-effects by restricting the molecule to the airways (review: [119]). In rats given an intratracheal dose of 1 mg/kg, the maximum free plasma concentration (C max) of UK371,104 was 20 nM, compared to 271 nM for CGS21680. This tenfold difference results from the higher lipophilicity, molecular weight, in vivo clearance and plasma protein binding capacity of UK371,104.
The safety and potency of UK371,104 were evaluated in anesthetized guinea-pigs monitored simultaneously for pulmonary and cardiovascular functions [129]. Whereas intratracheal CGS21680 or UK371,104 prevented capsaicin-induced bronchoconstriction, only CGS21680 provoked hypotension [129]. Furthermore, the protective effect of the new drug against BHR lasted more than tenfold longer than with CGS21680. Overall, UK371,104 offers a sevenfold improvement in potency and 150-fold reduction in side-effect over the lead compound, CGS21680 [119]. These data suggest that aerosolized UK371,104 constitutes the drug of choice for the treatment of chronic airway diseases.
The company further refined the structure of UK371,104 to generate UK432,097, [130]. In Phase 1 clinical trial, healthy subjects administered UK432,097 as an inhaled dry powder presented very little dispersal outside of the airways, and no effect on heart rate. In a Phase 2, randomized, double-blind, placebo controlled, parallel group clinical trial designed to evaluate the efficacy and safety of UK432,097 in adults with moderate-to-severe COPD, the patients showed no improvement in lung function over 6 weeks [131]. At the moment, alternative applications are considered for UK432,097, including cough suppression and improving the outcome of mechanically ventilated patients.
9.4.2.4 The ATL Family of A2AR Agonists
Stedivaze was originally developed by Clinical Data Inc. as pharmacological stress agent for myocardial perfusion imaging, to avoid the bronchoconstrictive effects of ADO in patients with asthma and COPD. In summer 2010, a Phase 2 clinical trial showed that a fixed dose, bolus injection, of Stedivaze generates sufficient coronary artery vasodilation for myocardial perfusion imaging, and without causing bronchoconstriction. This study constitutes a milestone toward the goal of developing a safe and well tolerated coronary vasodilator for these patients. Stedivaze is currently in Phase 3 trial for this application.
Given the potent anti-inflammatory properties of A2ARs, Stedivaze could represent an asset for the treatment of chronic respiratory diseases, while avoiding bronchospasms. Incidentally, the company Adenosine Therapeutics LLC (acquired by Clinical Data Inc. in 2008) was awarded funding in 2010 by the National Institute of Allergy and Infectious Diseases to explore applications for the treatment of asthma, arthritis and sepsis.
9.4.2.4.1 Stedivaze (Apadenoson; BMS 068645 or ATL146e)
Chemical Structure: 4-(3-[6-amino-9-(5-ethylcarbamoyl-3,4-dihydroxy-tetrahydro- furan-2-yl)-9H-purin-2-yl]-prop-2-ynyl)-cyclohexanecarboxylic acid methyl ester
In 2001, Linden et al. synthesized and characterized Stedivaze as a potent inhibitor of human neutrophil oxidative activity [132]. This compound was found to have 50 times more affinity for the human neutrophil A2AR than CGS21680. Since LPS causes a rapid up-regulation of A2ARs on inflammatory cells [133], a bacterial infection would provide additional binding sites for Stedivaze to suppress inflammation.
In 2004, Linden et al. provided evidence that Stedivaze may constitute a potent anti-inflammatory agent for the treatment of sepsis [134]. Human neutrophils primed by LPS responded to the bacterial chemoattractant, formyl-Met-Leu-Phe (fMLP), by an up-regulation of α4/β1 integrin, as reported for the circulating neutrophils of sepsis patients [135]. This sepsis-like neutrophil phenotype has been shown to bind more readily to the vascular cell adhesion molecule-1 (VCAM-1) on endothelial cells, which facilitates their transmigration into the lung tissue. Stedivaze, added before or after priming, was equally effective in inhibiting the up-regulation of α4/β1 integrin, which reduced the neutrophil adhesive properties.
In 2010, Linden et al. presented in vivo evidence for the therapeutic potential of Stedivaze in pulmonary diseases. In sickle cell disease, misshapen erythrocytes trigger transient episodes of microvascular ischemia-reperfusion, which reduces the baseline lung functions and maintains lung inflammation. Therefore, they used the murine model of sickle cell disease, NY1DD mice, to test Stedivaze. In these mice, continuous infusion of Stedivaze (10 ng/mg/min) initiated a dose-dependent improvement of the baseline lung functions, which reached maximal efficacy within 3 days [136]. In the NY1DD mice subjected to hypoxia-reperfusion, stedivaze added at the onset of reperfusion prevented further lung injury. This study supports the potential of stedivaze for the treatment of the lung inflammation caused by recurrent ischemia-reperfusion in sickle cell disease. On the other hand, this study did not document the impact the circulating A2AR agonist on blood pressure, which is a major concern for this class of bioagent.
9.4.2.4.2 The Next Generation of ATL Derivatives: ATL313
Chemical Structure: 4-(3-(6-amino-9-(5-cyclopropylcarbamoyl-3,4 dihydroxy tetra hydrofuran-2-yl)-9H-purin-2-yl)prop-2-ynyl) piperidine-1- carboxylic acid methyl ester
In collaboration with Adenosine Therapeutics Inc., Dr. Linden et al. designed and characterized a series of derivatives of Stedivaze. In 2007, they conducted radioligand binding experiments which yielded the following ranked order of affinity: ATL313 (IC50 = 1.9 nM) > ATL309 and ATL310 > ATL202 [137]. This class of compounds offers an additional improvement from Stedivaze, with 100-fold higher affinity for the A2AR than CGS21680. Functional assays conducted with equine neutrophils showed that all these compounds stimulate cAMP formation, and inhibit the production of reactive oxygen species induced by LPS, while respecting this order of potency.
Their therapeutic potential for respiratory diseases was first tested with ATL202 in a model of LPS-induced lung injury [138]. Most animal studies, described in Chaps. 8 and 9, were conducted by giving the drug before the challenge. In the present work, the authors compared the efficiency of aerosolized ATL202 given before or after aerosolized LPS. They showed that both strategies significantly decreased the number of neutrophils and cytokine concentrations measured in the BAL fluid. On the other hand, ATL202 only reduced extravasation when administered before a challenge. This experimental design is critical to identify the best delivery route for a specific treatment.
The most promising ATL derivative is ATL313, which exhibits a 100-fold higher selectivity for A2ARs than for A1Rs and A3Rs. Since 2007, more than 30 studies have been published on this ligand. This section reviews only those addressing the impact of ATL313 on lung injury and inflammation. Linden’s group conducted a series of ex vivo and in vivo experiments to test whether the vascular administration of ATL313 protects the lungs against ischemia-reperfusion injury, which remains a major complication after organ transplant. In the first study, they used isolated, buffer-perfused murine lungs to determine whether the therapeutic potential of ATL313 targets the resident cells [139]. Their model of ischemia-reperfusion significantly impaired pulmonary functions (higher airway resistance and pulmonary artery pressure, lower compliance), caused extensive tissue injury (vascular leakage and edema) and lung inflammation (BAL levels of TNFα, KC, MIP-2 and RANTES). These lung complications were all significantly attenuated by a bolus dose of ATL313 (30 nM) added to the perfusate at the onset of reperfusion. This dose had no significant effect on the lung functions or hemodynamics of control animals. The specificity of the receptor agonist was demonstrated using lung isolated from A2AR−/− mice, which showed no reduction in lung complications in response to ATL313. The fact that vascular ATL313 attenuated lung inflammation in the absence of circulating blood reiterates the critical role of the A2AR for the maintenance endothelial barrier integrity (see Chap. 8, Fig. 8.1). As such, ATL313 administered intravenous before the surgical procedure may significantly improve the outcome of lung transplant.
In Chap. 8, we provided evidence that all four ADO receptors mediate protection against vascular leakage, edema and inflammation in models of acute lung injury, such as ischemia-reperfusion (Table 9.1). Therefore, experiments were conducted to determine the relative potency of ATL313 using isolated, blood-perfused lungs infused with a selective agonist/antagonist of the A1R (CCPA/DCPCX), the A2AR (ATL313/ZM241385) or the A3R (IB-MECA/MRS1191) during reperfusion [140]. As expected, all receptor agonists significantly improved the lung functions (increased compliance and oxygenation, and decreased pulmonary artery pressure), reduced edema and inflammation (BAL levels of neutrophil myeloperoxidase and TNFα), compared to the untreated animals. When each agonist was paired with its antagonist, the protective effects were lost. More importantly, the ATL313 treatment improved lung functions and reduced neutrophil recruitment more efficiently than the A1R and A3R agonists, supporting a superior protective effect during lung transplant. In another study, these authors used the same protocol to show that the addition of ATL313 1 h before ischemia offers the same degree of protection [141]. Together, these studies suggest that ATL-313 infusion before, or at the time of transplant, may protect the lungs against the development of injury and rejection. Incidentally, this drug was reported to improve the outcome of organ islet transplant [142], supporting broad applications for clinical transplantation.
Another surgical application currently proposed for ATL313 is the protection of patients against the post-operative trauma caused by cardiopulmonary bypass. In the rats subjected to this procedure, addition of ATL313 to the blood priming solution completely prevented the development of lung edema, tissue injury and inflammation (IL-1β, IL-6, IFNγ, and neutrophil myeloperoxidase activity) [143]. This study suggests that ATL313 may prevent acute lung injury caused by cardiopulmonary bypass.
The protective anti-inflammatory effect of ATL313 during ischemia-reperfusion extends beyond the lungs’ resident cells [144]. In mice subjected to hilar occlusion, the intravenous injection of ATL313 before the onset of reperfusion significantly preserved lung function and prevented vascular leakage, compared to control animals. Based on BAL neutrophil myeloperoxidase activity and immunohistochemistry, ATL313 was also shown to inhibit the infiltration of neutrophils and CD4+ T cells during reperfusion. It is common knowledge that the number of circulating neutrophils is regulated by IL-17A, a cytokine released by the CD4+ T lymphocytes (review: [145]). The mice subjected to ischemia-reperfusion, after depletion of the CD4+ T cells or neutrophils, had significantly reduced lung injury, but ATL313 did not provide additional protection. In contrast, the BAL fluid levels of IL-17, KC, MCP-1, MIP-1 and RANTES were significantly lower in the neutrophil- and CD4+ T cell-depleted mice, but only further reduced by ATL313 in the neutrophil-depleted mice. This study demonstrates that ATL313 attenuates acute lung injury and inflammation by inhibiting the secretion of IL-17 by CD4+ T cells, and the subsequent neutrophil recruitment to the lungs.
This A2AR agonist is currently the focus of negotiations between Clinical Data Inc. and Santen Pharmaceutical Co. regarding ophthalmic diseases, while Clinical Data Inc. is reserving the rights to explore other applications.
In this section, all A2AR agonists evaluated for the treatment of chronic respiratory diseases were intensely scrutinized with respect to cardiovascular side-effects, especially hypotension. Yet, in the case of acute insults, such as surgical procedures or trauma, the above studies suggest that short-term vascular administration of an A2AR agonist would essentially normalize the arterial blood pressure raised by ischemia-reperfusion. Thus, a detrimental property for chronic lung diseases may be beneficial for acute lung injury.
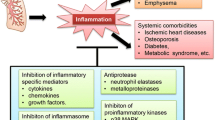
9.4.3 The A2BR Antagonists
The animal models of chronic respiratory diseases revealed that A2BR activation promotes BHR, inflammation, mucin hypersecretion, airway remodeling, fibrosis and emphysema (see Chap. 8 for details). This impressive portfolio suggests that A2BR antagonists may address all major pulmonary complications of patients diagnosed with asthma, COPD and fibrotic pulmonary diseases. In terms of delivery, inhalation should be avoided to preserve the A2BR-mediated airway clearance of mucins and pathogens (see Chap. 5 for details). Pharmaceutical companies have selected three A2BR antagonists, which are now emerging in the pipeline. The report that A2BR expression increases with disease severity in COPD and IPF [146] should be taken into consideration during clinical trials with respect to the targeted population and expected therapeutic index.
9.4.3.1 Comparing CVT-6883 and Montelukast
Chemical Structure: [3-ethyl-1-propyl-8-[1-(3-trifluoromethylbenzyl)-1H-pyrazol-4- yl]-3,7-dihydropurine-2,6-dione]
Over the past 5 years, chemists at CV Therapeutics synthesized a large number of Theophylline derivatives in search of a selective A2BR antagonist for the treatment of asthma (review: [147]). Based on binding assays, they selected CVT-6883, which has an affinity for A2BRs (Ki = 8 nM) at least 1,000-fold higher than for the other ADO receptors [148]. In various human cell lines, CVT-6883 inhibits cAMP production induced by the stable ADO analog: N-ethyl-carboxamidoadenosine (NECA). The pharmacodynamic and pharmacokinetic properties of CVT-6883 were determined in the rat. An oral dose of 2.0 mg/kg displayed an excellent systemic exposure, a Cmax of 1,100 ng/ml, a dose adjusted under the curve of (dAUC) of 6,500 ng.h/ml, and a half-life of 4 h.
The preclinical evaluation of CVT-6883 was conducted in mice using the ragweed sensitization/challenge model of allergic asthma [149]. The intraperitoneal injection of CVT-6883 completely prevented airway hyperresponsiveness to aerosol AMP, the pro-drug of ADO. Interestingly, CVT-6883 was as potent as an optimal dose of Montelukast [112], the cysteinyl leukotriene-1 receptor antagonist currently prescribed to asthmatic patients (review: [113]). The intraperitoneal delivery of CVT-6883 also inhibited the late allergic responses of these mice to ragweed for at least 5 h. On the other hand, the authors chose aerosol delivery to compare the anti-inflammatory properties of CVT-6883 and Theophylline. The drugs were nebulized prior to the last aerosol ragweed challenge, and the BAL fluid analyzed after 5 h. The optimal dose of each drug reduced total cell counts by nearly 50%. While they were similarly efficient in suppressing eosinophil recruitment, only CVT-6883 significantly reduced the lymphocyte counts. Therefore, aerosol CVT-6883 shows promises for the treatment of inflammation in allergic asthma.
The potential of long-term treatment with CVT-6883 to resolve all complications of chronic respiratory diseases was addressed using an animal model which develops the airway hyperresponsiveness, inflammation, remodeling, fibrosis and alveolar destruction: ADA-deficient mice [148]. The 14-day treatment consisted of intraperitoneal injections, administered twice daily to animals after they developed significant lung complications. The CVT-6883-treated mice presented significantly reduced airway inflammation (BAL cytokine levels, lymphocytes, eosinophils, neutrophils and macrophages), fibrosis (α1-procollagen and collagen deposition) and alveolar airspace enlargement. These results support substantial benefits for the long-term treatment of chronic lung diseases.
In 2008, CV Therapeutics had completed two randomized, single-blind, placebo-controlled, ascending dose clinical trials, in which CVT-6883 was determined to be safe and well tolerated by healthy volunteers [150]. The pharmacokinetic data support the use of one daily oral dose of CVT-6883 for the long-term treatment of chronic respiratory diseases (Table 9.3). This delivery route would also minimize the inhibitory effect of A2BR antagonists on the airway clearance of mucin and pathogens (see Chap. 5 for details).
In 2009, Gilead took over CV Therapeutics, which may cause a reorganization of their priorities, with respect to the drugs currently in the pipeline.
9.4.3.2 Anti-Inflammatory MRE 2029-F20
Chemical Structure: N-benzo[1,3]dioxol-5-yl-2-[5-(2,6-dioxo-1,3-dipropyl-2,3,6,7- tetrahydro-1H-purin-8-yl)-1-methyl-1H-pyrazol-3-yloxy] acetamide
In 2004, Baraldi et al. announced that they synthesized a large number of xanthine derivatives as potential A2BR antagonists [151]. The most selective compound was named MRE 2029-F20 (KiA2BR = 5.5 nM; KiA1R = 200 nM; KiA2AR, A3R > 1,000). Using isolated human neutrophils, lymphocytes or mast cells, MRE 2029-F20 was shown to inhibit the NECA-mediated cAMP production with IC50 values in the low nanomolar range, which supported a potent anti-inflammatory property. Therefore, MRE 2029-F20 was selected for further evaluation by King Pharmaceuticals [151].
In 2005, Borea et al. developed a radiolabelled MRE 2029-F20 [152, 153], which has been instrumental in the discovery that A2BR expression rises with disease severity in the lungs of COPD patients [118]. In recombinant systems, tritiated MRE 2029-F20 binds selectively to A2BRs, with KD values around 2 nM [153].
The same year, they tested the selectivity of MRE 2029-F20 in a human melanoma cell line [154]. The cell proliferation induced by the selective A3R agonist, Cl-IB-MECA, was not inhibited by this A2BR antagonist.
Preclinical data in animal models have not yet been reported for this bioagent.
9.4.3.3 LAS38096 for the Treatment of Asthma
Chemical Structure: 4'-(2-furyl)-N-pyridin-3-yl-4,5'-bipyrimidin-2'-amine
In 2007, a third compound, LAS38096 was discovered by Almirall Prodesfarma, which exhibits high affinity and selectivity for the A2BR (KiA2BR = 17 nM; KiA1R > 1,000 nM; KiA2AR > 2,500 nM; and KiA3R > 1,000 nM) [155]. In heterologous systems expressing human or murine A2BRs, LAS38096 inhibited NECA-mediated cAMP production with IC50 values in the 320–350 nM range. The capacity of LAS38096 to inhibit inflammatory responses was tested using human and mouse dermal fibroblasts. The bioagent induced a dose-dependent decrease in NECA-mediated IL-6 secretion, with IC50 values of 340 and 640 nM, respectively [155]. These data demonstrate that LAS38096 is a functional A2BR antagonist with similar affinity on the human and murine receptor.
The pharmacokinetic parameters of an oral dose of LAS38096 were determined in the rat, mouse and dog [155]. The drug exhibited excellent bioavailability in all species. It was absorbed rapidly (tmax < 60 min), with an AUC of 4.0 μM.h and a moderate-to-high plasma clearance.
The efficacy of LAS38096 was tested in vivo in the OVA sensitization/challenge model of allergic asthma [156]. Mice treated with the bioagent showed significantly less airway hyperresponsiveness, mucus production, eosinophil infiltration and OVA-specific IgE in the BAL fluid than untreated animals.
LAS38096 has been advanced for evaluation of safety and toxicology.
9.4.4 The A3R Agonists
The terms “complex” and “enigmatic” are frequently ascribed to the A3R because this receptor has been shown to induce inflammatory and anti-inflammatory responses (review: [157]). For instance, it stimulates neutrophil chemotaxis, but inhibits eosinophil recruitment to the airways. Nonetheless, A3R-mediated responses are predominantly anti-inflammatory, as demonstrated by the knockout mouse (see Chap. 8 for details). Thus, while agonists and antagonists are available as pharmacological agents, only agonists are currently tested for the treatment of chronic inflammatory disorders.
Over the last decade, new approaches have been introduced for the treatment of autoimmune diseases (review: [158]). Among the most potent drugs, TNFα antibodies are prescribed for arthritis, psoriasis and Crohn’s diseases. However, to block all TNFα-mediated inflammatory responses compromises host defenses and causes severe adverse effects. Recent studies revealed that the secretion of TNFα from inflammatory cells is inhibited by ADO acting selectively on A3Rs [159, 160]. Since the A3R is not expressed on airway epithelial cells, this approach may reduce lung inflammation by focusing on non-resident cells, with minimal effects on defenses mediated by the epithelial barrier.
Major concerns about the use of aerosolized A3R agonists were fueled by reports of BHR in murine models [45–48]. However, it is important to mention that histamine secretion is mediated by A2BRs in canine and human mast cells [49–51], which motivated the use of canine models for the evaluation of A3R agonists as anti-inflammatory agents. Furthermore, our current understanding of ADO-mediated BHR in asthmatics supports an A1R-mediated neural signal upstream from mast cell activation (see Sect. 9.2). As such, the A3R-mediated bronchospasms observed in murine models of asthma are not expected in human subjects. Hopefully, these precisions will stimulate the pharmaceutical industry to develop selective A3R agonists for chronic inflammatory lung diseases.
9.4.4.1 Rebirth of IB-MECA as CF101
Chemical Structure: 1-deoxy-1-[6-[[(iodophenyl)methyl]amino]9H-purine-9-yl]-N- methyl-(-D-ribofuranuronamide)
We owe a dept of gratitude to Dr. Kenneth A. Jacobson, who devoted his career to the development of ADO receptor ligands (review: [99]). In 1993, he designed the first selective A3R agonist, IB-MECA, which has been used in over 300 in vitro and in vivo studies. This metabolically stable molecule binds and activates the human A3R with an affinity (Ki = 0.5 nM) 1,000-fold higher than on the other ADO receptors (review: [157]). In 2000, Dr. Pnina Fishman obtained an exclusive license for IB-MECA, which was renamed CF101, and launched the company Can-Fite Biopharma.
The therapeutic potential of CF101 for lung complications was assessed mainly in models of acute lung injury. In isolated, blood-perfused rabbit lungs subjected to 18 h of cold ischemia, the addition of CF101 before reperfusion improved lung compliance and oxygenation, without affecting arterial pressure [140]. With respect to the inflammatory mediators measured in the BAL fluid, the A3R agonist reduced TNFα concentrations by 50% and neutrophil myeloperoxidase activity by 30%. Acute lung injury, quantified in terms of vascular leakage and edema, was also significantly lower in the animals treated with CF101. This study highlights the pleitropic protective effects of intravenous CF101 against acute lung inflammation and injury initiated by episodes of ischemia-reperfusion. Interestingly, Methotrexate was recently shown to enhance the anti-inflammatory effects of CF101 by causing an up-regulation of the A3R on monocytes and macrophages [161], which could offer additional clinical benefits for the treatment of acute lung injury.
The signaling mechanisms by which CF101 protects the lungs against injury and apoptosis during ischemia-reperfusion were investigated in spontaneously breathing cats [162, 163]. The presence of systemic CF101 during reperfusion significantly reduced the acute lung injury (% injured alveoli, wet/dry weight ratio) and apoptosis (TdT-mediated dUTP nick-end labeling positive cells and caspase 3 activity). Using selective inhibitors, the protective effects of CF101 were found to require ATP-sensitive K+ channels, but not nitric oxide production [163]. The signaling pathways activated by CF101 were identified by monitoring the expression of major protein kinases by SDS-PAGE and Western blot analysis of lung tissue specimens [162]. The A3R agonist induced a gradual up-regulation of the extracellular signal-regulated kinases 1 and 2 (ERK1/2), but not the c-Jun amino-terminal protein kinase (JNK) or p38. Injection of a selective A3R antagonist (MRS1191), before CF101, abolished the response of ERK1/2 without affecting p38 and JNK. These data suggest that the CF101-A3R signals are mediated predominantly by the ERK1/2-dependent pathways. However, A3Rs have been reported to regulate apoptosis via other signaling cascades, such as the phosphoinositide-3 kinase (PI3K)-dependent pathway (review: [157]). Therefore, future studies should verify the impact of selective ERK1/2 inhibitors on the acute lung injury and inflammation caused by ischemia-reperfusion.
In two controlled, double-blind, single ascending Phase 1 clinical trials conducted on healthy subjects, oral CF101 was demonstrated to be safe and well tolerated [164]. In oral solution, CF101 was readily absorbed (Tmax = 1–2 h) with a half-life of 9 h.
In December 2010, Can-Fite BioPharma announced that CF101 entered Phase 2 or 3 clinical trials for the treatment of cancer, dry eye syndrome, psoriasis and rheumatoid arthritis (Table 9.4). They retained the services of Plexus Ventures for the identification of a partner to support the clinical development and commercialization of CF101 in the United States and Europe, while it is already licensed in Japan and South Korea.
9.4.4.2 The More Selective Cl-IB-MECA (CF102)
Chemical structure: 2-chloro-N6-(3-lodobenzyl)-adenosine-5'-N-methyluronamide
Can-Fite BioPharma is also evaluating the potential of Cl-IB-MECA (CF102), a more selective analogue of IB-MECA (CF101) with binding affinities of 1.4 nM for the A3R, compared to 220 nM for the A1R, and 5,400 nM for the A2AR (review: [157]). Like his close relative, CF102 has been widely used as a pharmacological agent to identify the complex pharmacological properties of the A3R in mammalian tissues.
Wagner et al. tested the impact of CF102 on the lung inflammation induced by aerosolized LPS in wild-type and A3R−/− mice [165]. The endotoxin induced a linear increase in A3R expression over time in whole lung tissue, reaching sixfold above the baseline after 3 h. In addition, LPS inhalation stimulated leukocyte recruitment into the pulmonary vasculature, lung tissue and airspace. Pretreatment by intraperitoneal injection of CF102 significantly reduced the number of leukocytes in all compartments in the wild-type mice, but not in the A3R−/− mice. The CF102 treatment significantly reduced the levels of inflammatory cytokines (TNFα and IL-6) in the BAL fluid of LPS-exposed wild-type mice. In accordance with the barrier protective role of A3Rs during acute lung injury (see Chap. 8 for details), CF102 suppressed the LPS-induced vascular leakage in wild-type mice. One foreseeable side-effect of intraperitoneal CF102 is the enhancement of neutrophil migration speed (review: [166]). Nonetheless, the ligand did not affect the leukocyte counts in the pulmonary vasculature in the control and LPS-exposed animals.
In November 2010, Can-Fite Biopharma completed a Phase 1 clinical trial to assess the safety and pharmacokinetic behavior of CF102 in patients with advanced liver cancer. The patients received oral doses of 1, 5 or 25 mg (twice daily) over 28 days. Overall, the drug is safe and well tolerated at doses up to 25 mg, shows good oral bioavailability and linear pharmacokinetic behavior. Also, patient infected with hepatitis virus C experience a significant reduction in virus titer with CF102, consistent with its preclinical anti-viral activity. This A3R agonist hold promises as a novel therapeutic strategy in the treatment of cancer and viral infections.
9.4.4.3 New Generation MRS3558 (CF502)
Chemical Structure: [(1′R,2′R,3′S,4′R,5′S)-4-{2-chloro-6-[(3-chlorophenylmethyl) amino] purin-9-yl}-1-(methylaminocarbonyl)bicyclo [3.1.0] hexane-2,3-diol]
A novel A3R agonist, CF502, was recently synthesized at the National Institutes of Health (review: [157]). This molecule displays enhanced selectivity and specificity with >1,000-fold more affinity for the A3R than the A1R, A2AR, and A2BR. Functionally, this molecule represents a significant improvement from the first generation compounds. In the breathing cat model of ischemia-reperfusion, CF502 was found more efficient than CF101 against acute lung injury [162].
Jacobson et al. used the breathing cat model of ischemia-reperfusion to assess the potential of CF502 for the treatment of acute lung injury [167]. Interestingly, the sedated animals were monitored over 27 h of reperfusion, instead of the usual <3 h, to determine the long-term effects of ischemia-reperfusion and CF502. The immediate responses to in vivo ischemia-reperfusion were inflammation, apoptosis and edema, restricted to the left lobe subjected to ischemia. After 27 h of reperfusion, this lobe became more edematous, with evidence of hypoxemia, but exhibited less apoptosis and no change in inflammation. The control perfused right lobe presented edema after 27 h, suggesting a systemic effect of ischemia-reperfusion. The animals treated with one bolus dose of CF502, added to the left lobe perfusate during ischemia, developed milder inflammation and injury during at least 27 h of reperfusion. In addition, CF502 further reduced the parameters of apoptosis from the 3 h, to the 27 h, reperfusion time-point. Finally, this treatment also protected the lungs against the increase in blood pressure caused by ischemia-reperfusion. This study supports long-term clinical benefits for a bolus dose of CF502 during surgical procedures associated with acute lung injury, such as organ transplant.
Can-Fite Biopharma is currently developing CF502 as a second generation anti-inflammatory drug.
9.4.5 Crossing Swords with Other Therapies
9.4.5.1 Aspirin-Intolerant Asthma and Adenosine
Acetyl salicylic acid (ASA; aspirin) has been used for decades for the treatment of various inflammatory conditions. However, a subset of asthmatic patients exhibit violent allergic reactions to this common drug (review: [168]). Aspirin-intolerant asthma, also known as ASA-exacerbated respiratory disease, is associated with aspirin-induced BHR and a severe eosinophilic inflammation of the upper and lower airways, which maintains chronic rhinitis, sinusitis and polyposis. This disease is caused by an aberrant metabolism of arachidonic acid (review: [169]). The two products, prostaglandins and leukotrienes, bind to specific cell surface G protein-coupled receptors to orchestrate airway defenses. Prostaglandins stimulate mucociliary clearance, inhibit the development of fibrosis and the activities of inflammatory cells. In contrast, leukotrienes promote the recruitment and activation of inflammatory cells, mucus secretion, vascular permeability, fibrosis and bronchoconstriction. In aspirin-intolerant asthmatic patients, the metabolic balance of arachidonic acid is tilted toward leukotrienes, which leads to dramatic increases in the airway concentrations following ASA exposure (review: [170]). A recent clinical study suggests that ASA-induced leukotriene accumulation in exhaled breadth condensate may constitute a diagnostic tool to identify the aspirin-intolerant asthmatic patients [171].
In 2009, Kim et al. compared aspirin-tolerant and -intolerant asthmatics for the presence of single nucleotide polymorphisms (SNPs) in the sequences of ADA and the ADO receptors [172]. Using multivariate logistic regression analysis, they compared the frequencies of SNP genotypes and haplotypes in 136 aspirin-intolerant asthmatics, 181 aspirin-tolerant asthmatics and 183 normal individuals. They identified SNPs specific to the A1R and the A2AR which were significantly associated with aspirin intolerance. This survey suggests that airway ADO may contribute to the allergic reactions.
In 2010, Moon et al. provided evidence that ASA exacerbates lung eosinophilic inflammation by interfering with ADO regulation [173]. In this study, murine models of asthma were developed by intraperitoneal sensitization with OVA or OVA/LPS, followed by OVA challenges. Only the OVA/LPS-sensitized mice responded to intraperitoneal ASA by developing the aspirin-intolerant asthma phenotype of severe eosinophilia in the upper and lower tissue, and in BAL fluid. Since eosinophils represent <10% of all cells recruited to the airways, their response to ASA would be overlooked by total cell counts. Interestingly, ASA also caused a dramatic increase in lung ADO levels in the OVA/LPS mice. Expression analysis of the enzymes regulating ADO indicated that LPS selectively up-regulates ADA. This protective mechanism against excess ADO was obliterated by ASA. In addition, ASA-treated OVA/LPS mice accumulated lung IL-13, which has been shown to maintain an ADO/IL-13 amplification cycle by suppressing ADA expression (see Chap. 8 for details). These data predict that aspirin-intolerant asthmatic patients maintain higher airway ADO concentrations than the other asthmatics. This excess lung ADO, exacerbated by ASA, caused a down-regulation of Th17 responses via A1R and A3R engagement [173], which shifted the lung inflammation from a neutrophilic to an eosinophilic phenotype.
Collectively, these studies suggest that ASA intolerance results from the combined bronchoconstrictive effects of excess ADO accumulating in the airways of all asthmatics, and the high leukotriene concentrations reported only in the aspirin-intolerant subjects. Furthermore, the high ADO levels are expected to contribute to the severe eosinophilic inflammation through modulation of Th17 cell functions. As such, treatments reducing airway ADO levels (see Sect. 9.3) would be particularly beneficial for these patients.
9.4.5.2 Hypertonic Saline and the A2AR/A3R Balance
During severe trauma or elaborate surgical operations, like organ transplantation, the massive release of cytotoxic mediators by activated neutrophils causes major lung complications, such as acute lung injury and acute respiratory distress syndrome (ARDS). Since the early 1980s, resuscitation by small-volume injection of hypertonic saline (HS; 7.5% NaCl/6% dextran 70) is routinely performed to attenuate neutrophil-related trauma (reviews: [174, 175]). This procedure stems from several in vitro studies showing that HS inhibits neutrophil degranulation. However, some patients respond to HS resuscitation by an exacerbation of the complications. In a murine model of hemorrhagic shock, an early HS resuscitation prevented lung tissue damage, whereas delayed treatment aggravated the complications [176]. Since early treatments rarely occur within clinical settings, a better understanding of HS-mediated neutrophil activation was required to design resuscitation regimens that would minimize the risks of side-effects.
Junger et al. demonstrated that the dual regulation of neutrophil degranulation by HS is caused by a shift in ADO receptor expression during cell activation [125]. Naïve neutrophils express predominantly A2ARs, which inhibit cell degranulation by cAMP-dependent signaling pathways (review: [166]). Their stimulation by bacterial products, like formyl methionyl-leucyl-phenylalanine (fMLP), induces the expression and surface translocation of A3Rs, which stimulate degranulation by inhibition of cAMP production. Junger et al. showed that HS treatment of human neutrophils, before fMLP, prevented A3R induction and cell degranulation, whereas HS treatment after fMLP enhanced the A3R-mediated release of cytotoxic compounds [177]. In a model of sepsis, the addition of an A3R antagonist (MRS1191) to the HS solution enhanced the beneficial effects of resuscitation by avoiding the side-effects resulting from delayed administration [125].
This study supports a new therapeutic application for MRS1191 administration during HS resuscitation procedures, which may be required during lung transplant.
9.4.6 Summary
Finally, we have acquired sufficient maturity in the evaluation of ADO receptor ligands for the treatment of acute and chronic lung complications to formulate general principles and guidelines. With respect to A1Rs, the pharmaceutical industry understands the need to administer antagonists to suppress pulmonary inflammation (Table 9.1). The first two compounds developed, Theophylline and Bamiphylline, are currently available as oral prescriptions for asthmatic and COPD patients. On the other hand, the nebulized antisense oligodeoxynucleotide, EPI-2010, designed to remain in the airways to address BHR presented no clinical benefit in clinical trials. The story of Theophylline discovery tells us that the bronchodilating properties of the drug were mediated by the non-specific inhibition of phosphodiesterase. While in vitro and animal studies support a role for A1Rs in BHR, the importance of this mechanism in human subjects remains to be determined. With respect to A2ARs, everyone agrees on the benefits of selective agonists, but dosages which avoid cardiovascular side-effects (i.e. hypotension) were shown ineffective in the clinical trials, regardless of the selectivity or affinity of the compound (Table 9.2). On the other hand, these agonists hold promises for the reduction of lung complications resulting from cardiopulmonary bypass or lung transplant. The three A2BR antagonists selected for clinical evaluation all remain in the pipeline and the choice of oral delivery is consistent with the need to preserve A2BR-mediated airway clearance (Table 9.3). Finally, the highly controversial A3R is targeted for the development of selective agonists, which appear to provide effective anti-inflammatory protection for various disorders, including arthritis and psoriasis. Given the recent success of these drugs in animal models of lung disorders, clinical testing should be on the horizon.
9.5 Clinical Trials Involving ATP Receptors
The vast majority of the P2 receptor ligands selected for clinical applications are P2Y12R antagonists which target cardiovascular disorders and coagulation, including PLAVIX (clopidogrel; Sanofi Aventis/Bristol-Myers Squibb), Cangrelor (The Medicines Co.), Ticagrelor (AstraZeneca) and Eelinogrel (Portola/Norvatis). Among the receptors expressed along the airways, only one P2Y2R ligand is currently the subject of clinical trials for chronic respiratory diseases: denufosol (Inspire Pharmaceutical). This section also describes the first application of soluble apyrases to the treatment of lung injury.
9.5.1 The P2Y2R Agonist Denufosol and Airway Clearance
The most promising therapeutic approaches currently developed for the treatment of CF are designed to improve mucociliary clearance (MCC), a process which combines the activities of ion channels and transporters expressed at the surface of airway epithelia (see Chap. 5 for details). This disease is driven by a severe dehydration of the airway surfaces due to mutations in the cystic fibrosis transmembrane regulator (CFTR). The restoration of airway surface hydration would facilitate cilia beating, dislodge adhesive mucus plaques and facilitate MCC (review: [178]). The current strategy explored by the company Inspire Pharmaceutical is centered on P2Y2Rs, because their engagement can bypass the defective CFTR Cl− channel by activating the Ca2+-activated Cl− channel. The resulting osmotic gradient causes water to leave the cells to hydrate the surface.
A decade of research conducted in collaboration between Inspire Pharmaceutical and the Cystic Fibrosis Pulmonary Research/Treatment Center (NC, USA) demonstrated the therapeutic potential of metabolically-stable P2Y2R agonists (review: [179]). Their original work showed that the endogenous selective agonist, UTP, is highly unstable on human airway surfaces [180]. Therefore, they turned to dinucleotides because the tertiary structure offers more stability to the phosphate chain. From this first round of synthesis, they selected the potent P2Y2R agonist: Up4U (INS365; diquafosol). This molecule was further stabilized by substituting one uridine moiety by a deoxycytidine, which generated dCP4U (INS37217; denufosol) [180, 181]. The affinity of denufosol for the P2Y2R (EC50 = 0.3 μM) is over five times higher than for the other P2 receptors activated by uridine-based agonists on airway epithelia, namely the P2Y4R (EC50 = 1.2 μM) and the P2Y6R (EC50 = 16.0 μM) [181]. Preclinical studies demonstrated that denufosol restores normal surface hydration on cultures of human airway epithelial cells from CF patients, and also improves MCC in animals with impaired clearance [180, 181].
Given the severe lung complications experienced by CF patients, the tolerability of aerosolized denufosol was first tested in healthy subjects and smokers. The randomized double-blind placebo-controlled study, conducted with a wide concentration range (20–200 mg), provided evidence of tolerability and set the stage for clinical testing in CF.
In 2005, they conducted a double-blind, placebo-controlled, multicenter clinical trial to test the safety and tolerability of aerosolized denufosol in adult and pediatric (5–17 years of age) CF subjects [182]. Ascending single doses (10, 20, 40, and 60 mg) were followed by twice-daily administration of the maximum tolerated dose for 5 days. In summary, doses up to 60 mg of denufosol were well-tolerated by most subjects.
In 2007, Inspire Pharmaceutical and the Therapeutics Development Network of the Cystic Fibrosis Foundation presented results of a multicenter Phase 2 safety and efficacy clinical trial for denufosol inhalation in CF subjects with mild disease (FEV1 > 75% of predicted) [183]. The randomized, double-blind, placebo-controlled study showed that 20–60 mg denufosol significantly improved lung functions during ≥28 days. This study provided the first evidence of clinical benefit for denufosol.
In 2008, a placebo-controlled Phase 3 clinical trial (TIGER-1) tested the impact of 60 mg denufosol on 350 adolescent CF patients with FEV1 ≥75% of predicted. Results showed that TIGER-1 met the primary end-point, with significant improvement of FEV1 from baseline compared to the placebo group, and with limited systemic exposure. This study supports the therapeutic potential of early interventions with denufosol, in young CF patients, to prevent the accelerated loss of lung function.
In November 2009, Inspire Pharmaceuticals completed the patient enrollment for the second Phase 3 clinical trial (TIGER-2). This randomized, double-blind, placebo-controlled study of 48 days will test the long-term clinical benefits of 60 mg aerosolized denufosol in 450 patients with mild CF lung disease (FEV1 ≥75% of predicted). Results are expected to become available in the first quarter of 2011.
9.5.2 APT102: A Soluble Apyrase for Acute Lung Injury
Endothelial cells are well known to express the membrane-bound surface enzyme named the ecto nucleoside diphosphate triphosphohydrolase1 (NTPDase1; CD39). This enzyme is responsible for limiting thrombus formation through dephosphorylation of the circulating ATP/ADP released by activated platelets and red blood cells (review: [184]). Numerous in vivo and in vitro studies showed that oxidative stress caused by ischemia-reperfusion causes a dramatic down-regulation of endothelial CD39 (review: [185]). The potential of enzyme replacement therapy for cardiovascular and pulmonary diseases was originally tested using a soluble form of CD39 (apyrase) derived from the potato [186]. Eventually, the growing interest for therapeutic applications motivated the development of soluble human CD39 (review: [184]).
In 2006, Medina et al. generated a soluble recombinant apyrase named APT102 [187]. They demonstrated that APT102 inhibits tumor cell-induced platelet aggregation in colon cancer, which provided evidence of functional expression.
In 2008, APT Therapeutics determined the pharmacokinetic properties of APT102. [188]. Rats received a bolus intravenous injection (0.75 mg/kg), then serum samples were collected over time to monitor the metabolism of ATP and ADP using a malachite green assay. After 24 h, the enzyme activity remained tenfold above baseline, with a half-life of about 20 h. This study demonstrated the potential of a bolus injection of APT102 for the prevention of acute lung injury caused by trauma or extensive surgical procedures.
This success prompted APT Therapeutics to test whether APT102 could protect the lungs during their transport and transplant [189]. They preserved rat lungs in cold low K+ dextrose solution in the absence or presence of APT102 for 18 h before transplant. After the procedure, the recipients received a bolus dose of saline or APT102. Four hours later, the lungs that received APT102 showed significantly less damage (apoptotic endothelial cells and pulmonary edema) and were better oxygenated than the untreated transplanted lungs. The apyrase also attenuated lung inflammation, in terms of neutrophil infiltration and BAL fluid concentrations of pro-inflammatory mediators and myeloperoxidase. This study supports that APT102 can limit lung damage during prolonged cold storage and significantly improve the outcome of lung transplantation.
In 2009, APT Therapeutics received an award to evaluate therapeutic applications of human apyrase.
9.6 Conclusion
This final chapter is a testimony to the concerted efforts of research laboratories and pharmaceutical companies to develop therapeutic approaches safe and effective for the entire asthmatic population, as well as patients with COPD or fibrotic lung diseases. We have reached a point where we can learn from success stories and failures to refine our drug development strategies. For instance, we heard about the potential of the “low-hanging fruits”, like Adagen (PEG-ADA) initially developed for ADA-SCID. The tale of the A1R antagonist, Theophylline, shows how revisiting the properties of an inefficient bronchodilator lead to the discovery of a well-tolerated anti-inflammatory drug currently prescribed to asthmatics, in combination with a β-adrenergic bronchodilator. While A2AR agonists were once perceived as the most promising anti-inflammatory drugs for chronic respiratory diseases, the frequent reports of cardiovascular side-effects are redirecting these compounds toward surgical applications, to prevent the hypertension and acute lung injury resulting from ischemia-reperfusion. Our gaze is turned toward A2BR antagonists for the suppression of airway hyperresponsiveness. Furthermore, animal studies suggest that long-term treatments could reverse airway remodeling and fibrosis in chronic airway diseases. Finally, clinical trials support the benefits of A3R agonists for inflammatory disorders and acute lung injury. Therapeutic applications for ATP receptor ligands are also emerging. For instance, denufosol has entered the final stage of clinical evaluation for the improvement of P2Y2R-mediated airway clearance in CF patients. And animal studies suggest that P2X7R antagonists may suppress the production of the “first wave” pro-inflammatory mediator, IL-1β, as well as tissue damage by apoptosis. In conclusion, we are clearly witnessing the maturation of a young field of clinical research which will, no doubt, continue to fascinate and surprise us for years to come.
References
Cushley M, Tattersfield A, Holgate S (1983) Inhaled adenosine and guanosine on airway resistance in normal asthmatic subjects. Br J Clin Pharmacol 15:161–165
Driver AG, Kukoly CA, Ali S, Mustafa SJ (1993) Adenosine in the bronchoalveolar lavage fluid in asthma. Am Rev Respir Dis 148:91–97
Huszar E, Vass G, Vizi E, Csoma Z, Barat E, Molnar Vilagos G, Herjavecz I, Horvath I (2002) Adenosine in exhaled breath condensate in healthy volunteers and in patients with asthma. Eur Respir J 20:1393–1398
Lommatzsch M, Cicko S, Muller T, Lucattelli M, Bratke K, Stoll P, Grimm M, Durk T, Zissel G, Ferrari D, Di Virgilio F, Sorichter S, Lungarella G, Virchow JC, Idzko M (2010) Extracellular adenosine triphosphate and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 181:928–934
Esther CR Jr, Alexis NE, Clas ML, Lazarowski ER, Donaldson SH, Ribeiro CM, Moore CG, Davis SD, Boucher RC (2008) Extracellular purines are biomarkers of neutrophilic airway inflammation. Eur Respir J 31:949–956
Riteau N, Gasse P, Fauconnier L, Gombault A, Couegnat M, Fick L, Kanellopoulos J, Quesniaux VFJ, Marchand-Adam S, Crestani B, Ryffel B, Couillin I (2010) Extracellular ATP is a danger signal activating P2X7 receptor in lung inflammation and fibrosis. Am J Respir Crit Care Med 182:774–783
Oosterhoff Y, de Jong JW, Jansen MA, Koeter GH, Postma DS (1993) Airway responsiveness to adenosine 5′-monophosphate in chronic obstructive pulmonary disease is determined by smoking. Am Rev Respir Dis 147:553–558
Rutgers SR, Kerstjens HA, Timens W, Tzanakis N, Kauffman HF, Postma DS (2000) Airway inflammation and hyperresponsiveness to adenosine 5′-monophosphate in COPD. Chest 117:285S
Rutgers SR, ten Hacken NH, Koeter GH, Postma DS (2000) Borg scores before and after challenge with adenosine 5′-monophosphate and methacholine in subjects with COPD and asthma. Eur Respir J 16:486–490
Zhou Y, Schneider DJ, Blackburn MR (2009) Adenosine signaling and the regulation of chronic lung disease. Pharmacol Ther 123:105–116
Cushley MJ, Tattersfield AE, Holgate ST (1983) Adenosine antagonism as an alternative mechanism of action of methylxanthines in asthma. Agents Actions Suppl 13:109–113
Mann JS, Holgate ST, Renwick AG, Cushley MJ (1986) Airway effects of purine nucleosides and nucleotides and release with bronchial provocation in asthma. J Appl Physiol 61:1667–1676
Rorke S, Holgate ST (2002) Targeting adenosine receptors: novel therapeutic targets in asthma and chronic obstructive pulmonary disease. Am J Respir Med 1:99–105
Townley RG, Bewtra AK, Nair NM, Brodkey FD, Watt GD, Burke KM (1979) Methacholine inhalation challenge studies. J Allergy Clin Immunol 64:569–574
Hopp RJ, Bewtra AK, Nair NM, Townley RG (1984) Specificity and sensitivity of methacholine inhalation challenge in normal and asthmatic children. J Allergy Clin Immunol 74:154–158
Backer V, Groth S, Dirksen A, Bach-Mortensen N, Hansen KK, Laursen EM, Wendelboe D (1991) Sensitivity and specificity of the histamine challenge test for the diagnosis of asthma in an unselected sample of children and adolescents. Eur Respir J 4:1093–1100
Cockcroft DW, Murdock KY, Berscheid BA, Gore BP (1992) Sensitivity and specificity of histamine PC20 determination in a random selection of young college students. J Allergy Clin Immunol 89:23–30
Ramsdell JW, Nachtwey FJ, Moser KM (1982) Bronchial hyperreactivity in chronic obstructive bronchitis. Am Rev Respir Dis 126:829–832
Ramsdale EH, Morris MM, Roberts RS, Hargreave FE (1984) Bronchial responsiveness to methacholine in chronic bronchitis: relationship to airflow obstruction and cold air responsiveness. Thorax 39:912–918
Ramsdale EH, Roberts RS, Morris MM, Hargreave FE (1985) Differences in responsiveness to hyperventilation and methacholine in asthma and chronic bronchitis. Thorax 40:422–426
Verma VK, Cockcroft DW, Dosman JA (1988) Airway responsiveness to inhaled histamine in chronic obstructive airways disease. Chronic bronchitis vs emphysema. Chest 94:457–461
Avital A, Springer C, Bar-Yishay E, Godfrey S (1995) Adenosine, methacholine, and exercise challenges in children with asthma or pediatric chronic obstructive pulmonary disease. Thorax 50:511–516
Godfrey S, Springer C, Noviski N, Maayan C, Avital A (1991) Exercise but not methacholine differentiates asthma from chronic lung disease in children. Thorax 46:488–492
Van Den Berge M, Meijer RJ, Kerstjens HA, de Reus DM, Koeter GH, Kauffman HF, Postma DS (2001) PC(20) adenosine 5′-monophosphate is more closely associated with airway inflammation in asthma than PC(20) methacholine. Am J Respir Crit Care Med 163:1546–1550
van den Berge M, Kerstjens HA, Meijer RJ, de Reus DM, Koeter GH, Kauffman HF, Postma DS (2001) Corticosteroid-induced improvement in the PC20 of adenosine monophosphate is more closely associated with reduction in airway inflammation than improvement in the PC20 of methacholine. Am J Respir Crit Care Med 164:1127–1132
Joos GF, O’Connor B, Anderson SD, Chung F, Cockcroft DW, Dahlen B, DiMaria G, Foresi A, Hargreave FE, Holgate ST, Inman M, Lotvall J, Magnussen H, Polosa R, Postma DS, Riedler J (2003) Indirect airway challenges. Eur Respir J 21:1050–1068
Avital A, Picard E, Uwyyed K, Springer C (1995) Comparison of adenosine 5′-monophosphate and methacholine for the differentiation of asthma from chronic airway diseases with the use of the auscultative method in very young children. J Pediatr 127:438–440
Ketchell RI, Jensen MW, Lumley P, Wright AM, Allenby MI, O’Connor BJ (2002) Rapid effect of inhaled fluticasone propionate on airway responsiveness to adenosine 5′-monophosphate in mild asthma. J Allergy Clin Immunol 110:603–606
Luijk B, Kempsford RD, Wright AM, Zanen P, Lammers JW (2004) Duration of effect of single-dose inhaled fluticasone propionate on AMP-induced bronchoconstriction. Eur Respir J 23:559–564
Holgate ST, Arshad H, Stryszak P, Harrison JE (2000) Mometasone furoate antagonizes AMP-induced bronchoconstriction in patients with mild asthma. J Allergy Clin Immunol 105:906–911
Taylor DA, Jensen MW, Kanabar V, Engelstatter R, Steinijans VW, Barnes PJ, O’Connor BJ (1999) A dose-dependent effect of the novel inhaled corticosteroid ciclesonide on airway responsiveness to adenosine-5′-monophosphate in asthmatic patients. Am J Respir Crit Care Med 160:237–243
Bakirtas A, Turktas I (2006) Determinants of airway responsiveness to adenosine 5′-monophosphate in school-age children with asthma. Pediatr Pulmonol 41:515–521
Avital A, Godfrey S, Springer C (2000) Exercise, methacholine, and adenosine 5′-monophosphate challenges in children with asthma: relation to severity of the disease. Pediatr Pulmonol 30:207–214
Doull J, Sandall D, Smith S, Schreiber J, Freezer NJ, Holgate ST (1997) Differential inhibitory effect of regular inhaled corticosteroid on airway responsiveness to adenosine 5′ monophosphate, methacholine, and bradykinin in symptomatic children with recurrent wheeze. Pediatr Pulmonol 23:404–411
Berkman N, Avital A, Breuer R, Bardach E, Springer C, Godfrey S (2005) Exhaled nitric oxide in the diagnosis of asthma: comparison with bronchial provocation tests. Thorax 60:383–388
Fowler SJ, Dempsey OJ, Sims EJ, Lipworth BJ (2000) Screening for bronchial hyperresponsiveness using methacholine and adenosine monophosphate. Relationship to asthma severity and beta2-receptor genotype. Am J Respir Crit Care Med 162:1318–1322
Polosa R, Ng WH, Crimi N, Vancheri C, Holgate ST, Church MK, Mistretta A (1995) Release of mast-cell-derived mediators after endobronchial adenosine challenge in asthma. Am J Respir Crit Care Med 151:624–629
Crimi N, Palermo F, Oliveri R, Vancheri C, Polosa R, Palermo B, Maccarrone C, Mistretta A (1988) Comparative study of the effects of nedocromil sodium (4 mg) and sodium cromoglycate (10 mg) on adenosine-induced bronchoconstriction in asthmatic subjects. Clin Allergy 18:367–374
Phillips GD, Scott VL, Richards R, Holgate ST (1989) Effect of nedocromil sodium and sodium cromoglycate against bronchoconstriction induced by inhaled adenosine 5′-monophosphate. Eur Respir J 2:210–217
Summers QA, Honeywell R, Renwick AG, Holgate ST (1990) The protective efficacy of inhaled, oral and intravenous nedocromil sodium against adenosine-5′-monophosphate-induced bronchoconstriction in asthmatic volunteers. Pulm Pharmacol 3:190–197
Phillips GD, Rafferty P, Beasley R, Holgate ST (1987) Effect of oral terfenadine on the bronchoconstrictor response to inhaled histamine and adenosine 5′-monophosphate in non-atopic asthma. Thorax 42:939–945
Rafferty P, Beasley R, Holgate ST (1987) The contribution of histamine to immediate bronchoconstriction provoked by inhaled allergen and adenosine 5′ monophosphate in atopic asthma. Am Rev Respir Dis 136:369–373
Phillips GD, Polosa R, Holgate ST (1989) The effect of histamine-H1 receptor antagonism with terfenadine on concentration-related AMP-induced bronchoconstriction in asthma. Clin Exp Allergy 19:405–409
Rorke S, Jennison S, Jeffs JA, Sampson AP, Arshad H, Holgate ST (2002) Role of cysteinyl leukotrienes in adenosine 5′-monophosphate induced bronchoconstriction in asthma. Thorax 57:323–327
Salvatore CA, Tilley SL, Latour AM, Fletcher DS, Koller BH, Jacobson MA (2000) Disruption of the A3 adenosine receptor gene in mice and its effect on stimulated inflammatory cells. J Biol Chem 275:4429–4434
Tilley SL, Wagoner VA, Salvatore CA, Jacobson MA, Koller BH (2000) Adenosine and inosine increase cutaneous vasopermeability by activating A3 receptors on mast cells. J Clin Invest 105:361–367
Tilley SL, Tsai M, Williams CM, Wang ZS, Erikson CJ, Galli SJ, Koller BH (2003) Identification of A3 receptor- and mast cell-dependent and -independent components of adenosine-mediated airway responsiveness in mice. J Immunol 171:331–337
Zhong H, Shlykov SG, Molina JG, Sanborn BM, Jacobson MA, Tilley SL, Blackburn MR (2003) Activation of murine lung mast cells by the adenosine A3 receptor. J Immunol 171:338–345
Feoktistov I, Biaggioni I (1995) Adenosine A2B receptors evoke interleukin-8 secretion in human mast cells. An enprofylline-sensitive mechanism with implications for asthma. J Clin Invest 96:1979–1986
Forsythe P, McGarvey LP, Heaney LG, MacMahon J, Ennis M (1999) Adenosine induces histamine release from human bronchoalveolar lavage mast cells. Clin Sci 96:349–355
Ryzhov S, Goldstein AE, Matafonov A, Zeng D, Biaggioni I, Feoktistov I (2004) Adenosine-activated mast cells induce IgE synthesis by B lymphocytes: an A2B-mediated process involving Th2 cytokines IL-4 and IL-13 with implications for asthma. J Immunol 172:7726–7733
Pascoe SJ, Knight H, Woessner R (2007) QAF805, an A2B/A3 antagonist, does not attenuate AMP challenge in sujects with asthma. Proc Am Thorac Soc A682
Ethier MF, Madison JM (2006) Adenosine A1 receptors mediate mobilization of calcium in human bronchial smooth muscle cells. Am J Respir Cell Mol Biol 35:496–502
Brown RA, Clarke GW, Ledbetter CL, Hurle MJ, Denyer JC, Simcock DE, Coote JE, Savage TJ, Murdoch RD, Page CP, Spina D, O’Connor BJ (2008) Elevated expression of adenosine A1 receptor in bronchial biopsy specimens from asthmatic subjects. Eur Respir J 31:311–319
Hakonarson H, Shanbaky I, Guerra FM, Grunstein MM (1998) Modulation of adenosine A1, bradykinin B1, and histamine H1 receptor expression and function in atopic asthmatic sensitized airway smooth muscle. Am J Respir Crit Care Med C56
Abebe W, Mustafa SJ (1998) A1 adenosine receptor-mediated Ins(1,4,5)P3 generation in allergic rabbit airway smooth muscle. Am J Physiol 275:L990–L997
Obiefuna PC, Batra VK, Nadeem A, Borron P, Wilson CN, Mustafa SJ (2005) A novel A1 adenosine receptor antagonist, L-97–1 [3-[2-(4-aminophenyl)-ethyl]-8-benzyl-7-{2-ethyl-(2-hydroxy-ethyl)-amino]- ethyl}-1-propyl-3, 7-dihydro-purine-2, 6-dione], reduces allergic responses to house dust mite in an allergic rabbit model of asthma. J Pharmacol Exp Ther 315:329–336
Nyce JW, Metzger WJ (1997) DNA antisense therapy for asthma in an animal model. Nature 385:721–725
Hua X, Erikson CJ, Chason KD, Rosebrock CN, Deshpande DA, Penn RB, Tilley SL (2007) Involvement of A1 adenosine receptors and neural pathways in adenosine-induced bronchoconstriction in mice. Am J Physiol 293:L25–L32
Polosa R, Phillips GD, Rajakulasingam K, Holgate ST (1991) The effect of inhaled ipratropium bromide alone and in combination with oral terfenadine on bronchoconstriction provoked by adenosine 5′-monophosphate and histamine in asthma. J Allergy Clin Immunol 87:939–947
Polosa R, Rajakulasingam K, Church MK, Holgate ST (1992) Repeated inhalation of bradykinin attenuates adenosine 5′-monophosphate (AMP) induced bronchoconstriction in asthmatic airways. Eur Respir J 5:700–706
Keir S, Boswell-Smith V, Spina D, Page C (2006) Mechanism of adenosine-induced airways obstruction in allergic guinea pigs. Br J Pharmacol 147:720–728
Gosens R, Zaagsma J, Meurs H, Halayko A (2006) Muscarinic receptor signaling in the pathophysiology of asthma and COPD. Respir Res 7:73
Hirschhorn R, Ratech H (1980) Isozymes of adenosine deaminase. Isozymes Curr Top Biol Med Res 4:131–157
Silver JN, Flotte TR (2008) Towards a rAAV-based gene therapy for ADA-SCID: from ADA deficiency to current and future treatment strategies. Pharmacogenomics 9:947–968
Hershfield MS (1998) Adenosine deaminase deficiency: clinical expression, molecular basis, and therapy. Semin Hematol 35:291–298
Aldrich MB, Blackburn MR, Kellems RE (2000) The importance of adenosine deaminase for lymphocyte development and function. Biochem Biophys Res Commun 272:311–315
Hershfield M (2006) Adenosine deaminase deficiency. In: Pagon RA, Bird TC, Dolan CR, Stephens K (eds) Genereviews. University of Washington, Seattle
Hershfield MS (1993) Enzyme replacement therapy of adenosine deaminase deficiency with polyethylene glycol-modified adenosine deaminase (PEG-ADA). Immunodeficiency 4:93–97
Bax BE, Bain MD, Fairbanks LD, Webster AD, Chalmers RA (2000) In vitro and in vivo studies with human carrier erythrocytes loaded with polyethylene glycol-conjugated and native adenosine deaminase. Br J Haematol 109:549–554
Davis S, Abuchowski A, Park YK, Davis FF (1981) Alteration of the circulating life and antigenic properties of bovine adenosine deaminase in mice by attachment of polyethylene glycol. Clin Exp Immunol 46:649–652
Carbonaro DA, Jin X, Petersen D, Wang X, Dorey F, Kil KS, Aldrich M, Blackburn MR, Kellems RE, Kohn DB (2006) In vivo transduction by intravenous injection of a lentiviral vector expressing human ADA into neonatal ADA gene knockout mice: a novel form of enzyme replacement therapy for ADA deficiency. Mol Ther 13:1110–1120
Aiuti A, Roncarolo MG (2009) Ten years of gene therapy for primary immune deficiencies. Hematology 2009:682–689
Kaptein LC, Einerhand MP, Braakman E, Valerio D, van Beusechem VW (1993) Bone marrow gene therapy for adenosine deaminase deficiency. Immunodeficiency 4:335–345
Wakamiya M, Blackburn MR, Jurecic R, McArthur MJ, Geske RS, Cartwright J Jr, Mitani K, Vaishnav S, Belmont JW, Kellems RE et al (1995) Disruption of the adenosine deaminase gene causes hepatocellular impairment and perinatal lethality in mice. Proc Natl Acad Sci USA 92:3673–3677
Blackburn MR, Datta SK, Kellems RE (1998) Adenosine deaminase-deficient mice generated using a two-stage genetic engineering strategy exhibit a combined immunodeficiency. J Biol Chem 273:5093–5100
Blackburn MR, Datta SK, Wakamiya M, Vartabedian BS, Kellems RE (1996) Metabolic and immunologic consequences of limited adenosine deaminase expression in mice. J Biol Chem 271:15203–15210
Chunn JL, Young HW, Banerjee SK, Colasurdo GN, Blackburn MR (2001) Adenosine-dependent airway inflammation and hyperresponsiveness in partially adenosine deaminase-deficient mice. J Immunol 167:4676–4685
Banerjee SK, Young HW, Volmer JB, Blackburn MR (2002) Gene expression profiling in inflammatory airway disease associated with elevated adenosine. Am J Physiol 282:L169–L182
Vass G, Huszar E, Augusztinovicz M, Baktai G, Barat E, Herjavecz I, Horvath I (2006) The effect of allergic rhinitis on adenosine concentration in exhaled breath condensate. Clin Exp Allergy 36:742–747
Esther CR Jr, Boysen G, Olsen BM, Collins LB, Ghio AJ, Swenberg JW, Boucher RC (2009) Mass spectrometric analysis of biomarkers and dilution markers in exhaled breath condensate reveals elevated purines in asthma and cystic fibrosis. Am J Physiol 296:L987–L993
Esther CR Jr, Lazaar A (2009) Airway adenosine is elevated in COPD and correlates with disease severity. Am J Respir Crit Care Med 179:A3764
Blackburn MR, Aldrich M, Volmer JB, Chen W, Zhong H, Kelly S, Hershfield MS, Datta SK, Kellems RE (2000) The use of enzyme therapy to regulate the metabolic and phenotypic consequences of adenosine deaminase deficiency in mice. Differential impact on pulmonary and immunologic abnormalities. J Biol Chem 275:32114–32121
Chunn JL, Molina JG, Mi T, Xia Y, Kellems RE, Blackburn MR (2005) Adenosine-dependent pulmonary fibrosis in adenosine deaminase-deficient mice. J Immunol 175:1937–1946
Saha SK, Berry MA, Parker D, Siddiqui S, Morgan A, May R, Monk P, Bradding P, Wardlaw AJ, Pavord ID, Brightling CE (2008) Increased sputum and bronchial biopsy IL-13 expression in severe asthma. J Allergy Clin Immunol 121:685–691
Hartl D, Griese M, Kappler M, Zissel G, Reinhardt D, Rebhan C, Schendel DJ, Krauss-Etschmann S (2006) Pulmonary TH2 response in Pseudomonas aeruginosa-infected patients with cystic fibrosis. J Allergy Clin Immunol 117:204–211
Eickmeier O, Huebner M, Herrmann E, Zissler U, Rosewich M, Baer PC, Buhl R, Schmitt-Grohé S, Zielen S, Schubert R (2010) Sputum biomarker profiles in cystic fibrosis (CF) and chronic obstructive pulmonary disease (COPD) and association between pulmonary function. Cytokine 50:152–157
Saha S, Mistry V, Siva R, Parker D, May R, Bradding P, Pavord ID, Brightling CE (2008) Induced sputum and bronchial mucosal expression of interleukin-13 is not increased in chronic obstructive pulmonary disease. Allergy 63:1239–1243
Doherty T, Broide D (2007) Cytokines and growth factors in airway remodeling in asthma. Curr Opin Immunol 19:676–680
Blease K (2008) Therapeutics targeting IL-13 for the treatment of pulmonary inflammation and airway remodeling. Curr Opin Investig Drugs 9:1180–1184
Blackburn MR, Lee CG, Young HW, Zhu Z, Chunn JL, Kang MJ, Banerjee SK, Elias JA (2003) Adenosine mediates IL-13-induced inflammation and remodeling in the lung and interacts in an IL-13-adenosine amplification pathway. J Clin Invest 112:332–344
Zhu Z, Homer RJ, Wang Z, Chen Q, Geba GP, Wang J, Zhang Y, Elias JA (1999) Pulmonary expression of interleukin-13 causes inflammation, mucus hypersecretion, subepithelial fibrosis, physiologic abnormalities, and eotaxin production. J Clin Invest 103:779–788
Kang JS, DeLuca PP, Lee KC (2009) Emerging PEGylated drugs. Expert Opin Emerg Drugs 14:363–380
Schenone S, Brullo C, Musumeci F, Bruno O, Botta M (2010) A1 receptors ligands: past, present and future trends. Curr Top Med Chem 10:878–901
Cristalli G, Lambertucci C, Taffi S, Vittori S, Volpini R (2003) Medicinal chemistry of adenosine A2A receptor agonists. Curr Top Med Chem 3:387–401
Cristalli G, Lambertucci C, Marucci G, Volpini R, Dal Ben D (2008) A2A adenosine receptor and its modulators: overview on a druggable GPCR and on structure-activity relationship analysis and binding requirements of agonists and antagonists. Curr Pharm Des 14:1525–1552
Beukers MW, Meurs I, Ijzerman AP (2006) Structure-affinity relationships of adenosine A2B receptor ligands. Med Res Rev 26:667–698
Kalla RV, Zablocki J, Tabrizi MA, Baraldi PG (2009) Recent developments in A2B adenosine receptor ligands. Handb Exp Pharmacol 193:99–122
Jacobson KA, Klutz AM, Tosh DK, Ivanov AA, Preti D, Baraldi PG (2009) Medicinal chemistry of the A3 adenosine receptor: agonists, antagonists, and receptor engineering. Handb Exp Pharmacol 193:123–159
Versluis M, Van Den Berge M, Timens W, Luijk B, Rutgers B, Lammers JWJ, Postma DS, Hylkema MN (2008) Allergen inhalation decreases adenosine receptor expression in sputum and blood of asthma patients. Allergy 63:1186–1194
Persson CG (1985) On the medical history of xanthines and other remedies for asthma: a tribute to HH Salter. Thorax 40:881–886
Macht DI, Ting GC (1921) A study of antispasmodic drugs drugs on the bronchus. Pharmacol Exp Ther 18:373–398
Rabe KF, Dent G (1998) Theophylline and airway inflammation. Clin Exp Allergy 28:35–41
Lin CC, Lin CY, Liaw SF, Chen A (2002) Pulmonary function changes and immunomodulation of Th 2 cytokine expression induced by aminophylline after sensitization and allergen challenge in brown Norway rats. Ann Allergy Asthma Immunol 88:215–222
Nakano J, Yano T, Yamamura K, Yoshihara H, Ohbayashi O, Yamashita N, Ohta K (2006) Aminophilline suppresses the release of chemical mediators in treatment of acute asthma. Respir Med 100:542–550
Spears M, Donnelly I, Jolly L, Brannigan M, Ito K, McSharry C, Lafferty J, Chaudhuri R, Braganza G, Adcock IM, Barnes PJ, Wood S, Thomson NC (2009) Effect of low-dose theophylline plus beclometasone on lung function in smokers with asthma: a pilot study. Eur Respir J 33:1010–1017
Cowman S, Butler J (2008) Bet 3. The use of intravenous aminophylline in addition to beta-agonists and steroids in acute asthma. Emerg Med J 25:289–290
Ford PA, Durham AL, Russell RE, Gordon F, Adcock IM, Barnes PJ (2010) Treatment effects of low-dose theophylline combined with an inhaled corticosteroid in COPD. Chest 137:1338–1344
Spinelli A, Fanelli A, Gorini M, Sanna A, François C, Scano G (1991) Control of breathing in patients with chronic pulmonary obstructive disease: response to bamiphylline. Respiration 58:241–248
Todisco T, Baglioni S, Amir E, Palumbo R (1995) Effect of bamiphylline on tracheobronchial mucus clearance in subjects with smokers’ simple chronic bronchitis. Respiration 62:16–20
Cogo R, Monzani GP, Fusillo M, Vota M (1991) Therapeutic effectiveness of bamifylline in elderly patients with COPD. Minerva Med 82:115–118
Nadeem A, Obiefuna PC, Wilson CN, Mustafa SJ (2006) Adenosine A1 receptor antagonist versus montelukast on airway reactivity and inflammation. Eur J Pharmacol 551:116–124
Castro-Rodriguez JA, Rodrigo GJ (2010) The role of inhaled corticosteroids and montelukast in children with mild-moderate asthma: results of a systematic review with meta-analysis. Arch Dis Child 95:365–370
Lele RD (2009) Epigenetics-gene silencing. J Assoc Physicians India 57:60–66
Nyce JW (1999) Insight into adenosine receptor function using antisense and gene-knockout approaches. Trends Pharmacol Sci 20:79–83
Ball HA, Sandrasagra A, Tang L, Van Scott M, Wild J, Nyce JW (2003) Clinical potential of respirable antisense oligonucleotides (RASONs) in asthma. Am J Pharmacogenomics 3:97–106
Langley SJ, Allen DJ, Houghton C, Woodcock A (2005) Efficacy of EPI-2010 (An inhaled respirable anti-sense oligonucleotide: RASON) in moderate/severe persistent asthma. Am J Respir Crit Care Med 171:A360
Varani K, Caramori G, Vincenzi F, Adcock I, Casolari P, Leung E, MacLennan S, Gessi S, Morello S, Barnes PJ, Ito K, Chung KF, Cavallesco G, Azzena G, Papi A, Borea PA (2006) Alteration of adenosine receptors in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 173:398–406
Mantell SJ, Stephenson PT, Monaghan SM, Maw GN, Trevethick MA, Yeadon M, Keir RF, Walker DK, Jones RM, Selby MD, Batchelor DV, Rozze S, Chavaroche H, Hobson TJ, Dodd PG, Lemaitre A, Wright KN, Stuart EF (2008) Inhaled adenosine A2A receptor agonists for the treatment of chronic obstructive pulmonary disease. Bioorg Med Chem Lett 18:1284–1287
Fozard JR, Ellis KM, Villela Dantas MF, Tigani B, Mazzoni L (2002) Effects of CGS 21680, a selective adenosine A2A receptor agonist, on allergic airways inflammation in the rat. Eur J Pharmacol 438:183–188
Bonneau O, Wyss D, Ferretti S, Blaydon C, Stevenson CS, Trifilieff A (2006) Effect of adenosine A2A receptor activation in murine models of respiratory disorders. Am J Physiol 290:L1036–L1043
Chipps BE (2009) Inhaled corticosteroid therapy for patients with persistent asthma: learnings from studies of inhaled budesonide. Allergy Asthma Proc 30:217–228
Hasko G, Xu DZ, Lu Q, Nemeth ZH, Jabush J, Berezina TL, Zaets SB, Csoka B, Deitch EA (2006) Adenosine A2A receptor activation reduces lung injury in trauma/hemorrhagic shock. Crit Care Med 34:1119–1125
Bevan N, Butchers PR, Cousins R, Coates J, Edgar EV, Morrison V, Sheehan MJ, Reeves J, Wilson DJ (2007) Pharmacological characterization and inhibitory effects of (2R, 3R, 4 S, 5R)-2-(6-amino-2-{[(1 S)-2-hydroxy-1-(phenylmethyl)ethyl]amino}-9 H-purin-9-yl)-5-(2-ethyl-2 H-tetrazol-5-yl)tetrahydro-3, 4-furandiol, a novel ligand that demonstrates both adenosine A2A receptor agonist and adenosine A3 receptor antagonist activity. Eur J Pharmacol 564:219–225
Inoue Y, Tanaka H, Sumi Y, Woehrle T, Chen Y, Hirsh MI, Junger WG (2011) A3 Adenosine receptor inhibition improves the efficacy of hypertonic saline resuscitation. Shock 35(2):178–183
Rimmer J, Peake HL, Santos CMC, Lean M, Bardin P, Robson R, Haumann B, Loehrer F, Handel ML (2007) Targeting adenosine receptors in the treatment of allergic rhinitis: a randomized, double-blind, placebo-controlled study. Clin Exp Allergy 37:8–14
Luijk B, Van Den Berge M, Kerstjens HAM, Postma DS, Cass L, Sabin A, Lammers JWJ (2008) Effect of an inhaled adenosine A2A agonist on the allergen-induced late asthmatic response. Allergy 63:75–80
Morschl E, Molina JG, Volmer JB, Mohsenin A, Pero RS, Hong JS, Kheradmand F, Lee JJ, Blackburn MR (2008) A3 adenosine receptor signaling influences pulmonary inflammation and fibrosis. Am J Respir Cell Mol Biol 39:697–705
Trevethick MA, Mantell SJ, Stuart EF, Barnard A, Wright KN, Yeadon M (2009) Treating lung inflammation with agonists of the adenosine A2A receptor: promises, problems and potential solutions. Br J Pharmacol 155:463–474
Mantell SJ, Stephenson PT, Monaghan SM, Maw GN, Trevethick MA, Yeadon M, Walker DK, Selby MD, Batchelor DV, Rozze S, Chavaroche H, Lemaitre A, Wright KN, Whitlock L, Stuart EF, Wright PA, Macintyre F (2009) SAR of a series of inhaled A2A agonists and comparison of inhaled pharmacokinetics in a preclinical model with clinical pharmacokinetic data. Bioorg Med Chem Lett 19:4471–4475
Polosa R, Blackburn MR (2009) Adenosine receptors as targets for therapeutic intervention in asthma and chronic obstructive pulmonary disease. Trends Pharmacol Sci 30:528–535
Sullivan GW, Rieger JM, Michael Scheld W, Macdonald TL, Linden J (2001) Cyclic AMP-dependent inhibition of human neutrophil oxidative activity by substituted 2-propynylcyclohexyl adenosine A2A receptor agonists. Br J Pharmacol 132:1017–1026
Murphree LJ, Sullivan GW, Marshall MA, Linden J (2005) Lipopolysaccharide rapidly modifies adenosine receptor transcripts in murine and human macrophages: role of NF-kappaB in A2A adenosine receptor induction. Biochem J 391:575–580
Sullivan GW, Lee DD, Ross WG, DiVietro JA, Lappas CM, Lawrence MB, Linden J (2004) Activation of A2A adenosine receptors inhibits expression of a4/b1 integrin (very late antigen-4) on stimulated human neutrophils. J Leukoc Biol 75:127–134
Ibbotson GC, Doig C, Kaur J, Gill V, Ostrovsky L, Fairhead T, Kubes P (2001) Functional alpha4-integrin: a newly identified pathway of neutrophil recruitment in critically ill septic patients. Nat Med 7:465–470
Wallace KL, Linden J (2010) Adenosine A2A receptors induced on iNKT and NK cells reduce pulmonary inflammation and injury in mice with sickle cell disease. Blood 116:5010–5020
W-c S, Moore JN, Hurley DJ, Vandenplas ML, Linden JM, Murray TF (2007) Pharmacologic characterization of novel adenosine A2A receptor agonists in equine neutrophils. Am J Vet Res 68:981–987
Reutershan J, Cagnina RE, Chang D, Linden J, Ley K (2007) Therapeutic anti-inflammatory effects of myeloid cell adenosine receptor A2A stimulation in lipopolysaccharide-induced lung injury. J Immunol 179:1254–1263
Sharma AK, Linden J, Kron IL, Laubach VE (2009) Protection from pulmonary ischemia-reperfusion injury by adenosine A2A receptor activation. Respir Res 10:58
Gazoni LM, Walters DM, Unger EB, Linden J, Kron IL, Laubach VE (2010) Activation of A1, A2A, or A3 adenosine receptors attenuates lung ischemia-reperfusion injury. J Thorac Cardiovasc Surg 140:440–446
Gazoni LM, Laubach VE, Mulloy DP, Bellizzi AM, Unger EB, Linden J, Ellman PI, Lisle TC, Kron IL (2008) Additive protection against lung ischemia-reperfusion injury by adenosine A2A receptor activation before procurement and during reperfusion. J Thorac Cardiovasc Surg 135:156–165
Chhabra P, Wang K, Zeng Q, Jecmenica M, Langman L, Linden J, Ketchum RJ, Brayman KL (2010) Adenosine A2A agonist administration improves islet transplant outcome: evidence for the role of innateimmunity in Islet graft rejection. Cell Transplant 19:597–612
Lisle TC, Gazoni LM, Fernandez LG, Sharma AK, Bellizzi AM, Schifflett GD, Laubach VE, Kron IL (2008) Inflammatory lung injury after cardiopulmonary bypass is attenuated by adenosine A2A receptor activation. J Thorac Cardiovasc Surg 136:1280–1287
Sharma AK, Laubach VE, Ramos SI, Zhao Y, Stukenborg G, Linden J, Kron IL, Yang Z (2010) Adenosine A2A receptor activation on CD4+ T lymphocytes and neutrophils attenuates lung ischemia-reperfusion injury. J Thorac Cardiovasc Surg 139:474–482
Ley K, Smith E, Stark MA (2006) IL-17A-producing neutrophil-regulatory Tn lymphocytes. Immunol Res 34:229–242
Zhou Y, Murthy JN, Zeng D, Belardinelli L, Blackburn MR (2010) Alterations in adenosine metabolism and signaling in patients with chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis. PLoS ONE 5:e9224
Kalla RV, Zablocki J (2009) Progress in the discovery of selective, high affinity A2B adenosine receptor antagonists as clinical candidates. Purinergic Signal 5:21–29
Sun CX, Zhong H, Mohsenin A, Morschl E, Chunn JL, Molina JG, Belardinelli L, Zeng D, Blackburn MR (2006) Role of A2B adenosine receptor signaling in adenosine-dependent pulmonary inflammation and injury. J Clin Invest 116:2173–2182
Mustafa SJ, Nadeem A, Fan M, Zhong H, Belardinelli L, Zeng D (2007) Effect of a specific and selective A2B adenosine receptor antagonist on adenosine agonist AMP and allergen-induced airway responsiveness and cellular influx in a mouse model of asthma. J Pharmacol Exp Ther 320:1246–1251
Wilson CN, Mustafa SJ, Kalla RV, Zablocki J, Tabrizi MA, Baraldi PG (2009) Recent developments in A2B adenosine receptor ligands. Handb Exp Pharmacol 193:99–122
Baraldi PG, Tabrizi MA, Preti D, Bovero A, Romagnoli R, Fruttarolo F, Zaid NA, Moorman AR, Varani K, Gessi S, Merighi S, Borea PA (2004) Design, synthesis, and biological evaluation of new 8-heterocyclic xanthine derivatives as highly potent and selective human A2B adenosine receptor antagonists. J Med Chem 47:1434–1447
Baraldi PG, Aghazadeh Tabrizi M, Preti D, Bovero A, Fruttarolo F, Romagnoli R, Moorman AR, Gessi S, Merighi S, Varani K, Andrea Borea P (2004) [3 H]-MRE 2029-F20, a selective antagonist radioligand for the human A2B adenosine receptors. Bioorg Med Chem Lett 14:3607–3610
Gessi S, Varani K, Merighi S, Cattabriga E, Pancaldi C, Szabadkai Y, Rizzuto R, Klotz K-N, Leung E, Mac Lennan S, Baraldi PG, Borea PA (2005) Expression, pharmacological profile, and functional coupling of A2B receptors in a recombinant system and in peripheral blood cells using a novel selective antagonist radioligand, [3 H]MRE 2029-F20. Mol Pharmacol 67:2137–2147
Merighi S, Benini A, Mirandola P, Gessi S, Varani K, Leung E, Maclennan S, Borea PA (2005) A3 adenosine receptor activation inhibits cell proliferation via phosphatidylinositol 3-Kinase/Akt-dependent inhibition of the extracellular signal-regulated kinase 1/2 phosphorylation in A375 human melanoma cells. J Biol Chem 280:19516–19526
Vidal B, Nueda A, Esteve C, Domenech T, Benito S, Reinoso RF, Pont M, Calbet M, Lopez R, Cadavid MI, Loza MI, Cardenas A, Godessart N, Beleta J, Warrellow G, Ryder H (2007) Discovery and characterization of 4'-(2-Furyl)-N-pyridin-3-yl-4, 5′-bipyrimidin-2'-amine (LAS38096), a potent, selective, and efficacious A2B adenosine receptor antagonist. J Med Chem 50:2732–2736
Aparici M, Nueda A, Beleta J, Prats N, Fernandes R, Miralpeix M (2006) A potent adenosine A2B antagonist attenuates methacholine-induced hyperresponsiveness, mucus production and IgE levels in an allergic mouse model. CIA Symposium Abstract162
Gessi S, Merighi S, Varani K, Leung E, Mac Lennan S, Borea PA (2008) The A3 adenosine receptor: an enigmatic player in cell biology. Pharmacol Ther 117:123–140
Borea PA, Gessi S, Bar-Yehuda S, Fishman P (2009) A3 adenosine receptor: pharmacology and role in disease. Handb Exp Pharmacol 193:297–327
Lee JY, Jhun BS, Oh YT, Lee JH, Choe W, Baik HH, Ha J, Yoon KS, Kim SS, Kang I (2006) Activation of adenosine A3 receptor suppresses lipopolysaccharide-induced TNF-alpha production through inhibition of PI 3-kinase/Akt and NF-kappaB activation in murine BV2 microglial cells. Neurosci Lett 396:1–6
Levy O, Coughlin M, Cronstein BN, Roy RM, Desai A, Wessels MR (2006) The adenosine system selectively inhibits TLR-mediated TNF-alpha production in the human newborn. J Immunol 177:1956–1966
Ochaion A, Bar-Yehuda S, Cohn S, Del Valle L, Perez-Liz G, Madi L, Barer F, Farbstein M, Fishman-Furman S, Reitblat T, Reitblat A, Amital H, Levi Y, Molad Y, Mader R, Tishler M, Langevitz P, Zabutti A, Fishman P (2006) Methotrexate enhances the anti-inflammatory effect of CF101 via up-regulation of the A3 adenosine receptor expression. Arthritis Res Ther 8:R169
Matot I, Weiniger CF, Zeira E, Galun E, Joshi BV, Jacobson KA (2006) A3 adenosine receptors and mitogen-activated protein kinases in lung injury following in vivo reperfusion. Crit Care 10:R65
Rivo J, Zeira E, Galun E, Matot I (2004) Activation of A3 adenosine receptors attenuates lung injury after in vivo reperfusion. Anesthesiology 101:1153–1159
Bar-Yehuda S, Silverman MH, Kerns WD, Ochaion A, Cohen S, Fishman P (2007) The anti-inflammatory effect of A3 adenosine receptor agonists: a novel targeted therapy for rheumatoid arthritis. Expert Opin Investig Drugs 16:1601–1613
Wagner R, Ngamsri K-C, Stark S, Vollmer I, Reutershan J (2010) Adenosine receptor A3 is a critical mediator in LPS-induced pulmonary inflammation. Am J Physiol 299:L502–L512
Chen Y, Yao Y, Sumi Y, Li A, To UK, Elkhal A, Inoue Y, Woehrle T, Zhang Q, Hauser C, Junger WG (2010) Purinergic signaling: a fundamental mechanism in neutrophil activation. Sci Signal 3:ra45
Matot I, Einav S, Weiniger CF, Pearl RG, Abramovitch R, Joshi BV, Jacobson KA (2008) Lung injury after in vivo reperfusion: outcome at 27 hours after reperfusion. Anesthesiology 109:269–278
Palikhe NS, Kim J-H, Park H-S (2009) Update on recent advances in the management of aspirin exacerbated respiratory disease. Yonsei Med J 50:744–750
Drakatos P, Lykouras D, Sampsonas F, Karkoulias K, Spiropoulos K (2009) Targeting leukotrienes for the treatment of COPD? Inflamm Allergy Drug Targets 8:297–306
Huang SK, Peters-Golden M (2008) Eicosanoid lipid mediators in fibrotic lung diseases: ready for prime time? Chest 133:1442–1450
Sanak M, Kiełbasa B, Bochenek G, Szczeklik A (2004) Exhaled eicosanoids following oral aspirin challenge in asthmatic patients. Clin Exp Allergy 34:1899–1904
Kim SH, Kim YK, Park HW, Kim SH, Kim SH, Ye YM, Min KU, Park HS (2009) Adenosine deaminase and adenosine receptor polymorphisms in aspirin-intolerant asthma. Respir Med 103:356–363
Moon HG, Tae YM, Kim YS, Gyu Jeon S, Oh SY, Song Gho Y, Zhu Z, Kim YK (2010) Conversion of Th17-type into Th2-type inflammation by acetyl salicylic acid via the adenosine and uric acid pathway in the lung. Allergy 65:1093–1103
Kramer GC (2003) Hypertonic resuscitation: physiologic mechanisms and recommendations for trauma care. J Trauma 54:S89–S99
Rocha-e-Silva M, Poli de Figueiredo LF (2005) Small volume hypertonic resuscitation of circulatory shock. Clinics 60:159–172
Murao Y, Hoyt DB, Loomis W, Namiki S, Patel N, Wolf P, Junger WG (2000) Does the timing of hypertonic saline resuscitation affect its potential to prevent lung damage? Shock 14:18–23
Inoue Y, Chen Y, Pauzenberger R, Hirsh MI, Junger WG (2008) Hypertonic saline up-regulates A3 adenosine receptor expression of activated neutrophils and increases acute lung injury after sepsis. Crit Care Med 36:2569–2575
Boucher RC (2007) Evidence for airway surface dehydration as the initiating event in CF airway disease. J Intern Med 261:5–16
Kellerman D, Rossi Mospan A, Engels J, Schaberg A, Gorden J, Smiley L (2008) Denufosol: a review of studies with inhaled P2Y2 agonists that led to Phase 3. Pulm Pharmacol Ther 21:600–607
Yerxa BR, Sabater JR, Davis CW, Stutts MJ, Lang-Furr M, Picher M, Jones AC, Cowlen M, Dougherty R, Boyer J, Abraham WM, Boucher RC (2002) Pharmacology of INS37217 [P(1)-(uridine 5′)-P(4)-(2'-deoxycytidine 5’)tetraphosphate, tetrasodium salt], a next-generation P2Y2 receptor agonist for the treatment of cystic fibrosis. J Pharmacol Exp Ther 302:871–880
Shaver SR, Rideout JL, Perdergast W, Douglass JG, Brown EG, Boyer JL, Patel RI, Redick CC, Jones AC, Picher M, Yerxa BR (2005) Structure-activity relationship of dinucleotides: potent and selective agonists of P2Y receptors. Purinergic Signal 1:183–191
Deterding R, Retsch-Bogart G, Milgram L, Gibson R, Daines C, Zeitlin PL, Milla C, Marshall B, Lavange L, Engels J, Mathews D, Gorden J, Schaberg A, Williams J, Ramsey B (2005) Safety and tolerability of denufosol tetrasodium inhalation solution, a novel P2Y2 receptor agonist: results of a phase 1/phase 2 multicenter study in mild to moderate cystic fibrosis. Pediatr Pulmonol 39:339–348
Deterding RR, LaVange LM, Engels JM, Mathews DW, Coquillette SJ, Brody AS, Millard SP, Ramsey BW (2007) Phase 2 randomized safety and efficacy trial of nebulized denufosol tetrasodium in cystic fibrosis. Am J Respir Crit Care Med 176:362–369
Fung CY, Marcus AJ, Broekman MJ, Mahaut-Smith MP (2009) P2X1 receptor inhibition and soluble CD39 administration as novel approaches to widen cardiovascular therapeutic window. Trends Cardiovasc Med 19:1–5
Van Linden A, Eltzschig HK (2007) Role of pulmonary adenosine during hypoxia: extracellular generation, signaling and metabolism by surface adenosine deaminase/CD26. Expert Opin Biol Ther 7:1437–1447
Beaudoin AR, Sevigny J, Picher M (1996) ATP-diphosphohydrolases, apyrases and nucleotide phosphohydrolases: biochemical properties and functions. JAI Press, Greenwich
Medina C, Jurasz P, Santos-Martinez MJ, Jeong SS, Mitsky T, Chen R, Radomski MW (2006) Platelet aggregation-induced by caco-2 cells: regulation by matrix metalloproteinase-2 and adenosine diphosphate. J Pharmacol Exp Ther 317:739–745
Uluçkan Ö, Eagleton MC, Floyd DH, Morgan EA, Hirbe AC, Kramer M, Dowland N, Prior JL, Piwnica-Worms D, Jeong SS, Chen R, Weilbaecher K (2008) APT102, a novel ADPase, cooperates with aspirin to disrupt bone metastasis in mice. J Cell Biochem 104:1311–1323
Sugimoto S, Lin X, Lai J, Okazaki M, Das NA, Li W, Krupnick AS, Chen R, Jeong SS, Patterson GA, Kreisel D, Gelman AE (2009) Apyrase treatment prevents ischemia-reperfusion injury in rat lung isografts. J Thorac Cardiovasc Surg 138:752–7759
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Science+Business Media B.V.
About this chapter
Cite this chapter
Tilley, S., Volmer, J., Picher, M. (2011). Therapeutic Applications. In: Picher, M., Boucher, R. (eds) Purinergic Regulation of Respiratory Diseases. Subcellular Biochemistry, vol 55. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-1217-1_9
Download citation
DOI: https://doi.org/10.1007/978-94-007-1217-1_9
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-1216-4
Online ISBN: 978-94-007-1217-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)