Abstract
Osseointegration, the first concept of biosis–abiosis intelligent interface, is primarily explained, and researches on the elucidation of osseointegration mechanism and titanium-tissue interface observation are reviewed to understand a concept to create biosis–abiosis intelligent interface. In addition, current status of surface treatment of metallic materials is reviewed. In particular, a gap between research level progress and commercialization in surface treatments is focused. Mechanical property, durability, and manufacturing process of surface layer formed on titanium by surface treatment, are significant to commercialize the treatment, while most of researches focuses only evaluation of biocompatibility and biofunction.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Excellent biocompatibility and biofunction of ceramics and polymers are expected to show excellent properties as biomaterials; in fact many devices consisting of metals have been substituted by those consisting of ceramics and polymers. In spite of this event, over 70 % of implant devices in medical field including dentistry, especially over 95 % in orthopedics, still consist of metals, and this share is currently maintained, because of their high strength, toughness, and durability.
On the contrary, a disadvantage of using metals as biomaterials is that they are typically artificial materials and have no biofunction. Therefore, metal surface naturally forms a clear interface against living tissue that works as a barrier to conduct biofunctions. To add biocompatibility and biofunction to metals, in other words, to create biosis–abiosis intelligent interface, surface treatment is essential, because biofunction cannot be added during manufacturing processes of metals such as melting, casting, forging, and heat treatment. Surface treatment is a process that changes a material’s surface composition, structure, and morphology, leaving the bulk mechanical properties intact.
This chapter primarily reviews past researches on the interface between titanium and tissue and change in the research trend with era that much help us to understand a concept to create biosis–abiosis intelligent interface. In addition, current status of surface treatment of metallic materials is reviewed to enhance new and superior designs of biosis–abiosis intelligent interface.
2 Biosis–Abiosis Intelligent Interface
When a metallic material is implanted into a human body, immediate reaction occurs between its surface and the living tissues. In other words, immediate reaction at this initial stage straightaway determines and defines a metallic material’s tissue compatibility. An artificial material usually makes clear interface against a biological system, such as cell, bacterial and tissue: The interface works as a barrier for transportation of molecules and conduction of biofunction, as shown in Fig. 5.1a. On the other hand, if we could create unclear and graded interface at which molecules smoothly transport, both material and tissue are integrated together, and biofunctions are conducted, this interface may be defined as biosis–abiosis intelligent interface, as shown in Fig. 5.1b. In addition, this interface is expected to be a field not only for chemically biofunctional conduction, but also for mechanically stress conduction. If so, how to make this biosis–abiosis intelligent interface? Of course, one of the solutions is surface treatment of materials. With surface treatment, tissue compatibility of surface layer could be improved.
Clear interface against cell, bacterial and tissue: The interface works as a barrier for transportation of molecules and conduction of biofunction (a). Unclear and graded interface at which smooth transportation of molecules occurs, both material and tissue are integrated together, and biofunctions are conducted (b)
3 Osseointegration of Titanium
Osseointegration is the first definition of the interface between a metallic material and living tissue. The definition of osseointegration is as follows: The formation of a direct interface between an implant and bone, without intervening soft tissue. No scar tissue, cartilage or ligament fibers are present between the bone and implant surface. The direct contact of bone and implant surface can be verified microscopically [1]. This “osseointegration” concept was immediately accepted by dentists and dental materials researchers in the world to show biocompatible advantage of titanium among metals that makes it possible that titanium occupies major position in dental implant bodies. After percolating the concept of osseointegration, the elucidation of osseointegration mechanism including the investigation on microscopic interface structure between titanium and bone tissue has been actively studied.
4 Mechanism of Osseointegration in Titanium
From the viewpoint of the property of titanium surface, mechanism and process of osseointegration has been discussed. Titanium and some of its alloys are known to be among the best biocompatible materials, and commercially the materials have been successfully used for orthopedic and dental implants. The question is why titanium and its alloys show such good biocompatibility compared with other alloys. The explanation to the question is generally believed to be that titanium passivates in aqueous solutions and that passive film is stable even in a biological system. Therefore, it was first thought that good hard tissue compatibility of titanium is caused by its high corrosion resistance. This hypothesis was false. For example, electric plating of platinum on titanium makes delay bone formation on itself, while the corrosion resistance increased [2]. Therefore, good hard tissue compatibility of titanium is caused not only by its high corrosion resistance but also other causes.
In this regard, the surface layer of titanium is essentially TiO2 before and after autoclaving and anodic oxidation treatment [3, 4]. However, it is questionable whether titanium oxide is stable and does not react with any electrolyte even in biological system. In this question, the mechanisms of passive dissolution of titanium in a model physiological environment were revealed [5]. They explained that dissolution of titanium depends on solution ligands and the surface oxide characteristics. They also revealed preferential molecular adsorption on titanium [6].
Composition of surface oxide film varies according to environmental changes, though the film is macroscopically stable. Passive surfaces co-exist in close contact with electrolytes, undergoing a continuous process of partial dissolution and re-precipitation from the microscopic viewpoint. In this sense, surface composition is always changing according to the environment (Fig. 5.2). The composition and properties of the oxide film regenerated in a biological environment may be different from those in water. When titanium which has been surgically implanted into the human jaw is characterized using Auger electron spectroscopy, its surface oxide film reveals constituents of calcium, phosphorus, and sulfur [7, 8]. By immersing titanium and its alloys in Hanks’ solution and other solutions [9–12] (Fig. 5.3), preferential adsorption of phosphate ions occurs. Even during cell culture on titanium, calcium phosphate is formed on it [13]. Extrapolating from here, it can be assumed that bone formation is faster on titanium implanted in hard tissue simply because the surface oxide film is titanium oxide. The surface oxide film on titanium is not completely oxidized and is relatively reactive; neither calcium nor phosphate stably exists alone on titanium, and calcium phosphate is naturally formed on it; calcium phosphate formed on titanium is stable and protective [14]. Surface oxide films as passive films on valve metals such as Ti are almost amorphous and different from titanium oxide bulk and crystalline ceramics with regard to its chemical property.
The surface oxide is always formed on conventional metallic biomaterials and the surface of the surface oxide is active. Therefore, the oxide surface immediately reacts with water molecules and hydroxyl groups are formed as shown in Fig. 5.4a. The surface hydroxyl groups contain both terminal OH and bridge OH in the equal amounts. Concentration of hydroxyl groups on the unit area of the surface is determined with various techniques. Active surface hydroxyl groups dissociates in aqueous solutions and forms electric charges as shown in Fig. 5.4b [15–18]. Positive or negative charge due to the dissociation is governed by pH of the surrounding aqueous solution: positive and negative charges are balanced and apparent charge is zero at a certain pH. This pH is the point of zero charge (pzc). The pzc is the unique value for an oxide and an indicator which the oxide shows acidic or basic property. For example, in the case of TiO2, the pzc of rutile is 5.3 and that of anatase is 6.2 [15] (Fig. 5.4c). In other words, anatase surface is acidic at smaller pH and basic at larger pH than 6.2. Active surface hydroxyl groups and electric charges formed by the dissociation of the groups play important roles for the bonding with polymers and immobilization of biomolecules. Therefore, the concentration of surface hydroxyl group and pH is important factors for the bonding with polymeric materials and immobilization of biomolecules.
Formation of surface hydroxyl groups on titanium oxide by the adsorption of water molecules (a), dissociation of hydroxyl groups in aqueous solutions including body fluid and showing positive and negative charges according to the environmental pH (b), and point of zero charge (pzc) of various oxide (c)
Proteins adsorption influences cells adhesion. Likewise, proteins denaturalization and fragmentation (which occur due to adsorption) may affect the function of the host body. To characterize proteins adsorbed to metals and metal oxides, various techniques can be used [19], especially that of ellipsometry [20]. To predict proteins adsorption, the wettability test is used where a liquid droplet is applied to the material [21]. Fibrinogen is much more naturally adsorbed on titanium surface than on gold surface, because the dielectric constant, the factor governing electrostatic force, of TiO2 is 80.1 and similar to that of water [22]. Therefore, fibrinogen remains its conformation even after the adsorption on titanium surface.
As described above, many researchers made their effort to elucidate the mechanism of osseointegration by characterization of titanium surface oxide (composition and change of it), surface hydroxyl groups, adsorption of proteins (amount, speed, change in the conformation, and denaturalization), and adhesion, proliferation and differentiation of cells. However, the true mechanism of osseointegration is still not clear.
5 Nanometer-Level Interface Structure
On the other hand, micrometer and nanometer-level observation of the interface between titanium and tissue has been studied. The intact bone-to-titanium interface consists of a fibrous tissue-free boundary zone with a 20–40 nm thick proteoglycan coat immediately adjacent to titanium oxide are revealed [23, 24]. Bundles of collagen appear at a minimum distance of 100–200 nm from the interface. Calcium deposits were sometimes seen in direct contacted (resolution level 30–50 nm) with the titanium oxide. The similar variation in interface ultrastructure within 50–100 nm of titanium surface [25]. The collagen fibrils did not reach the implant surface but were separated from it by an amorphous layer, being 300–500 nm thick which did not decrease in width with time [26]. An electron-dense lamina limitans-like line containing mineral was observed between the amorphous layer and the bone tissue. On the other hand, amorphous proteoglycan layer is not interposed at the interface between bone and titanium was observed [27]. In addition, this lamina limitans seems to consist of osteopontin and α2 HS-glycoprotein [28]. Recently, osteoblast-like cells made direct contact with titanium via a 20–50 nm thin amorphous zone is shown [29]. A 20–50 nm thin amorphous zone, a slender cell layer, and/or a poorly mineralized zone were interposed between bone and titanium. There is apparently a 20–50 nm amorphous layer containing proteoglycan on titanium oxide according to the above studies. Relatively high-resolutional observation using transmission electron microscopy is feasible in the findings regarding structure of the interface. However, it is difficult to make a tissue specimen with metallic material for TEM observation. Therefore, a couple of studies [24, 25] employed a foil and sputter-coated film of titanium instead of bulk material to be easily sectioned with a microtome. That is, the structure at the interface near titanium is unclear, while the observation of the interface is currently continued [30].
6 Surface Treatment
6.1 Change of Research Trend
The above researches on the elucidation of osseointegration mechanism and characterization of structure at the interface, now showed down and research trend moved to surface treatment for bone formation on titanium. Tremendous amount of surface treatment researches has been conducted, while some of the researches are left important matters behind somewhere. In these researches, the control is usually untreated titanium. Therefore, some researchers declare that “titanium is bioinert” to demonstrate the effective results of their surface treatment. Origin of this misunderstanding is that no apatite forms on titanium by SEM-level after immersion in Kokubo’s simulated body fluid (SBF) [31, 32]. Where has the initial definition of “osseointegration” of titanium gone? The true story is as follows: Titanium shows the best bone conduction among metallic materials, while the ability is much lower than bioactive ceramics.
6.2 Surface Treatment
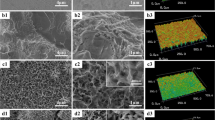
Surface treatment is a process that changes a material’s surface composition, structure, and morphology, leaving the bulk mechanical properties intact. With surface treatment, the tissue compatibility of the surface layer can be improved, as shown in Fig. 5.5. Surface treatment techniques by both dry and wet processes used in research and industry are summarized in Fig. 5.6. Surface treatment techniques are reviewed elsewhere [33, 34].
6.3 Surface Treatment for Bone Formation
Titanium and its alloys, which show good hard tissue compatibility, are used for dental implants and artificial hip joints. However, the hard-tissue compatibility of these materials is lower than that of bioactive ceramics, such as hydroxyapatite and bioactive glasses. Therefore, numerous surface treatment techniques to improve the hard tissue compatibility of titanium have been developed, and some have been commercialized.
In the stems of artificial hip joints and dental implants, the chemical bonding of metal surfaces with bone is not expected. In other words, it is impossible for metals as typical artificial materials to chemically and naturally bond with bone as living tissue, especially in the human body with body fluid. Therefore, the surface morphology is sometimes controlled, and rough and porous surface is formed in titanium. Living tissue, such as bone, is expected to grow into the rough porous surface, and the materials and bone are strongly connected as a result of the so-called anchoring effect. Figure 5.7 shows chemical bonding and a mechanical anchoring connection between bone and material.
6.4 Evolution of Surface Treatment for Bone Formation
Figure 5.8 shows the evolution of surface treatment techniques to improve hard tissue compatibility at the research level:
-
First generation: Grind machining of the surface.
-
Second generation: Grooving, blast, acid etching, anodic oxidation, and laser abrasion.
-
Third generation: Chemical treatment and hydroxyapatite coating.
-
Fourth generation: Immobilization of biofunctional molecules (collagen, bone morphogenetic protein, and peptide).
-
Fifth generation: Coating of stem cells and tissues?
The bone formation of the materials surface is accelerated when biomolecules concerning bone formation are immobilized on the material surface, such as in the fourth generation in Fig. 5.8. Therefore, many studies have achieved good results in this direction. However, to increase the popularity of the immobilization of biofunctional molecules, it is necessary to ensure the safety, quality maintenance during storage, and dry-conditioned durability of the immobilized layer. Therefore, it is difficult for manufacturers to commercialize those research results. Most of commercialized goods are categorized into the second generation, a few belong to the third generation, and there is no prospect for the commercialization of the fourth generation, at present. The commercialization went faster for the second than third generation possibly because materials employing mechanical anchoring are more practical than materials employing chemical bonding with bone.
On researches developing new surface treatment techniques, biocompatibility and biofunction are usually focused, while sometimes mechanical properties, durability, and manufacturing process are left behind, that may delays the utilization of the technique. Most of researchers make the best effort to evaluate biological effects with cell culture and animal test; they hesitate conduct the evaluation of durability. They sometimes do not remember “materials engineering”, while remind only materials chemistry and biological evaluation.
However, immobilization of biomolecules and biofunctional molecules as shown as the fourth generation above is effective tool to add biofunction to metal surface. This subject is reviewed somewhere [35].
7 Conclusions
Metallic materials are widely used in medicine not only for orthopedic implants and dental implants, but also for cardiovascular devices and for other purposes. Metallic biomaterials are always used in close contact with living tissues. Therefore, interactions between material surfaces and living tissues must be well controlled. Metal surface may be biofunctionalized by various surface treatment techniques. These techniques make it possible to apply metals to a scaffold in tissue engineering.
References
Bränemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallĕn O, Ohman A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1–132.
Itakura Y, Tajima T, Ohoke S, Matsuzawa J, Sudo H, Yamamoto S. Osteocompatibility of platinum-plated titanium assessed in vitro. Biomaterials. 1989;10:489–93.
Lausmaa J, Kasemo B, Mattsson H. Surface spectroscopic characterization of titanium implant materials. Appl Surf Sci. 1990;44:133–46.
Lausmaa J, Kasemo B, Mattsson H, Odelius H. Multi-technique surface spectroscopic characterization of electropolished and anodized Ti. Appl Surf Sci. 1990;45:189–200.
Healy KE, Ducheyne P. Hydration and preferential molecular adsorption on titanium in vitro. J Biomed Mater Res. 1992;26:319–38.
Healy KE, Ducheyne P. Hydration and preferential molecular adsorption on titanium in vitro. Biomaterials. 1992;13:553–61.
Espostito M, Lausmaa J, Hirsch JM, Thomsen P. Suface analysis of failed oral titanium implants. J Biomed Mater Res Appl Biomater. 1999;48:559–68.
Hanawa T, Ota M. Characterization of surface film formed on titanium in electrolyte. Appl Surf Sci. 1992;55:269–76.
Hanawa T. Titanium and its oxide film: a substrate for formation of apatite. In: Davies JE, editor. The bone-biomaterial interface. Toronto: University of Toronto Press; 1991. p. 49–61.
Hanawa T, Okuno O, Hamanaka H. Compositional change in surface of Ti-Zr alloys in artificial bioliquid. J Jpn Inst Met. 1992;56:1168–73.
Bruesch P, Muller K, Atrens A, Neff H. Corrosion of stainless-steels in chloride solution-an XPS investigation of passive films bruesch. Appl Phys. 1985;38:1–18.
Sundgren JE, Bodo P, Lundstrom I. Auger electron spectroscopic studies of the interface between human tissue and inplants of titanium and stainless steel. J Colloid Interface Sci. 1986;110:9–20.
Hiromoto S, Hanawa T, Asami K. Composition of surface oxide film of titanium with culturing murine fibroblasts L929. Biomaterials. 2004;25:979–86.
Tsutsumi Y, Nishimura D, Doi H, Nomura N, Hanawa T. Difference in surface reactions between titanium and zirconium in Hanks’ solution to elucidate mechanism of calcium phosphate formation on titanium using XPS and cathodic polarization. Mater Sci Eng C. 2009;29:1702–8.
Parfitt GD. The surface of titanium dioxide. Progr Surf Membr Sci. 1976;11:181–226.
Westall J, Hohl H. A comparison of electrostatic models for the oxide/solution interface. Adv Colloid Interface Sci. 1980;12:265–94.
Healy TW, Fuerstenau DW. The oxide-water interface-Interreaction of the zero point of charge and the heat of immersion. J Colloid Sci. 1965;20:376–86.
Boehm HP. Acidic and basic properties of hydroxylated metal oxide surfaces. Discuss Faraday Soc. 1971;52:264–89.
Ivarsson B, Lundström I. Physical characterization of protein adsorption on metal and metal oxide surfaces. CRC Critic Rev Biocompat. 1986;2:1–96.
Elwing H. Protein absorption and ellipsometry in biomaterial research. Biomaterials. 1998;19:397–406.
Bagnall RD, Arundel PA. A method for the prediction of protein adsorption on implant surfaces. J Biomed Mater Res. 1983;17:459–66.
Sundgren JE, Bodö P, Ivarsson B, Lundström I. Adsorption of fibrinogen on titanium and gold surfaces studied by ESCA and ellipsometry. J Colloid Interface Sci. 1986;113:530–43.
Albrektsson T, Hansson HA, Ivarsson B. Interface analysis of titanium and zirconium bone implants. Biomaterials. 1985;6:97–101.
Albrektsson T, Hansson HA. An ultrastructual characterization of the interface between bone and sputtered titanium or stainless steel surfaces. Biomaterials. 1986;7:201–5.
Linder L, Obrant K, Boivin G. Osseointegration of metallic implants. II. Transmission electron microscopy in the rabbit. Acta Orthop Scand. 1989;60:235–9.
Sennerby L, Thomsen P, Ericson LE. Early tissue response to titanium implants inserted in rabbit cortical bone. J Mater Sci Mater Med. 1993;4:494–502.
Listgarten MA, Buser D, Steinemann SG, Donath K, Lang NP, Weber HP. Light and transmission electron microscopy of the intact interfaces between non-submerged titanium-coated epoxy resin implants and bone or gingiva. J Dent Res. 1992;71:364–71.
Nanci A, McCarthy GF, Zalzal S, Clokie CML, Warshawsky H, McKee MD. Tissue response to titanium implants in the rat tibia: ultrastructural immunocytochemical and lectin-cytochemical characterization of the bone-titanium interface. Cell Mater. 1994;4:1–30.
Murai K, Takeshita F, Ayukawa Y, Kiyoshima T, Suetsugu T, Tanaka T. Light and electron microscopic studies of bone-titanium interface in the tibiae of young and mature rats. J Biomed Mater Res. 1996;30:523–33.
Brunette DM, Tengvall P, Textor M, Thomsen P, editors. Titanium in medicine. Berlin: Springer; 2001.
ISO23317:2007. Implants for surgery. In vitro evaluation for apatite-forming ability of implant materials. Geneva: International Organization for Standardization; 2007.
Kokubo T, Takadama H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials. 2006;27:2907–15.
Hanawa T. An overview of biofunctionalisation of metals in Japan. J R Soc Interface. 2009;6:S361–9.
Hanawa T. Biofunctionalization of titanium for dental implant. Jpn J Dent Sci Rev. 2010;46:93–101.
Hanawa T. Metal-polymer composite biomaterials. In: Dumitriu S, Popa V, editors. Polymeric biomaterials Vol. 1, Structure and function. Boca Raton: CRC; 2013. p. 343–75.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is distributed under the terms of the Creative Commons Attribution Noncommercial License, which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Copyright information
© 2015 The Author(s)
About this paper
Cite this paper
Hanawa, T. (2015). Biofunctionalization of Metallic Materials: Creation of Biosis–Abiosis Intelligent Interface. In: Sasaki, K., Suzuki, O., Takahashi, N. (eds) Interface Oral Health Science 2014. Springer, Tokyo. https://doi.org/10.1007/978-4-431-55192-8_5
Download citation
DOI: https://doi.org/10.1007/978-4-431-55192-8_5
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-55125-6
Online ISBN: 978-4-431-55192-8
eBook Packages: MedicineMedicine (R0)