Abstract
Mobile apps are an important source of data, but also an important tool for applying models. The goal of this chapter is to provide a short overview of relevant app development background including data collection tools, as well as provide a literature review on mobile clinical decision support systems. Regulatory issues will be touched upon to create awareness for this important topic.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Operating Systems
Two major operating systems are important for mobile apps: iOS (Apple) and Android (Google) , a total market share of 99% (iOS 54% and Android 45% in May 2018, measured in USA). (Mobile Operating System Market Share United States Of America|StatCounter Global Stats [21]) These two operating systems are not compatible, which means that programming for both requires a different approach. Developing native iOS apps is done using the programming language Objective-C or Swift, and native Android apps are developed in Java or Kotlin. As these languages, and more importantly the operating system-specific frameworks, are fairly different, hybrid app development has become increasingly popular. Hybrid apps are essentially “web apps” (mobile web pages) that are wrapped in a native binary (the file that is downloaded from the App Store or Google Play) and can access native device features such as the camera or the accelerometer. The main advantage is that the app only needs to be developed and maintained once. Potential disadvantages are a lack of native look and feel (which is important from a usability perspective), and a lack of access to features that are not available in the hybrid framework (such as health- and research-frameworks as explained in Chap. 1). A hybrid framework that is very popular at the time of writing is Ionic (www.ionicframework.com), which is open source and available free of charge. Alternatives that can sometimes even offer a native look and feel for the app’s graphical user interface (e.g. Titanium Appcelerator) often come at a price.
2 Collecting Health Data
Apple HealthKit and Google Fit are operating system-specific frameworks for users to collect and organize health data on their mobile device. With the addition of ResearchKit in 2015, Apple created an innovative open-source approach towards easily collecting data from large cohorts that give informed consent and provide data completely from the app. Successful applications have been described in Parkinson, asthma and spine disease [4, 5, 35]. An Android alternative for ResearchKit is the open-source initiative ResearchStack.org. Such frameworks open completely new ways to acquire scientific data, but require a shift in thinking from the researcher’s perspective from classic data collection methods to digital tools and correlated new opportunities (e.g. finger tapping task for Parkinson patients in a mobile app or uploading videos of walking patterns for deep learning applications).
3 Mobile Clinical Decision Support Systems
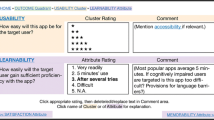
From the perspective of applications, mobile devices are excellent tools to implement decision support systems. A systematic review of the literature was performed to assess the current evidence on this topic. MEDLINE has been searched using the PubMed website and medical subject headings (MeSH) in combination with free text search. The combination (“Decision Support Systems, Clinical”[Mesh]) AND “Computers, Handheld”[Mesh], (“Decision Support Systems, Clinical”[Mesh]) AND smartphone and (“Decision Support Systems, Clinical”[Mesh]) AND “Cell Phones”[Mesh] revealed a total of 183 hits after removing duplicates. These were screened based on title and abstract. The inclusion criteria were: English, mobile, clinical decision support system, patient-related outcome parameters (including caregiver or guideline adherence), and focus on implementing guidelines. Exclusion criteria were: no abstract, no outcome parameters, case study, focus on telemonitoring, or focus on (implementation) strategy. From this screening, 30 articles were included for full text screening. After full text screening, 7 articles were included for a qualitative synthesis of the literature on clinical decision support systems (mCDSS). Reasons for excluding articles based on full text screening are given in Table 12.1. An evidence table summarizing the included studies is presented in Table 12.2.
Samore (2005) performed a randomized clinical trial (RCT) in 12 rural communities represented by a total of 334 general physicians using a Palm OS based mCDSS with a cradle-based database synchronisation. The primary outcome was antimicrobial usage in acute respiratory tract infection. In the mCDSS group there was a 9% decrease in (false positive) prescriptions compared to a 1% decrease in the control group (p = 0.03) [27].
Sintchenko (2005) performed a prospective trial with historical cohorts amongst an unspecified number (at least 12) of intensive care unit physicians and residents, using a Pocket PC platform with HL7-compatible web-based database synchronisation. The primary outcome was antibiotic use and patient outcome on the ICU. Use of the mCDSS resulted in a 17.5% decrease in defined daily doses per 1000 patient days (p = 0.04) and a 13% decreased length of stay on the intensive care unit (p = 0.02) [28].
Berner (2006) performed a RCT amongst 68 internal medicine residents using a Palm OS based mCDSS. The primary outcome was NSAID-related gastrointestinal risk assessment in drug prescriptions. The study compares the ratio of unsafe prescriptions in the mCDSS group (0.23) to the control group (0.45), which is statistically significant (p < 0.05). However, the same rates at baseline are 0.27 and 0.29 for the mCDSS and control group respectively. Apparently in the control group the number of unsafe prescriptions increased compared to baseline, therefore clinically relevant conclusions are hard to draw from these data [2].
Lee (2009) performed a RCT amongst 20 nurses with a total of 1874 patient encounters, using a Palm OS based mCDSS. The primary outcome was the proportion of obesity-related diagnoses. The mCDSS led to a more than 10% increase in (true positive) diagnoses compared to the control group (p < 0.001) [19].
Roy (2009) performed a cluster RCT in 20 emergency departments with a total of 1645 patients, using a Palm OS based mCDSS. The primary outcome was pulmonary embolism diagnosis, and use of the mCDSS led to a 19.3% increase in correct diagnosis compared to the control group (95% CI: 2.9–35.6%; p = 0.023) [25].
Snooks (2014) performed a cluster RCT amongst paramedics. A total of 17 out of 42 paramedics used the mCDSS for 54 out of 436 (12.4%) of the participants. The mCDSS was presented on a tablet PC forming part of the electronic patient record. The primary outcome was fall emergency referrals in the elderly population. The mCDSS led to 9.6% referrals compared to 5.0% in the control group (odds ratio 2.04; 95% CI: 1.12–3.72) [29].
Spat (2016) performed an open, noncontrolled intervention study in 30 patients with type 2 diabetes mellitus in which a mCDSS for insulin dosing was provided to an interdisciplinary team of engineers, physicians and nurses. The mCDSS was a mobile app developed for both iOS and Android. The primary outcome was glucose serum levels. In comparison with a historic control group, there was a statistically significant decrease in hypoglycaemia (1.3% vs 3.0%; p = 0.01) [31].
Based on the available scientific literature it is safe to say that there is level I evidence that mCDSS can be beneficial in guideline implementation for diagnostic and therapeutic purposes. Adoption of mobile devices capable of data connectivity has increased throughout the years and availability should be not a problem nowadays, in particular in combination with a so-called “bring your own device ” strategy.
Most of the excluded articles after full text screening were concerned with app usage, implementation strategy and usability issues. Recurring concerns on implementation are good institutional support, good wireless data connectivity and sufficient technology skills by the end user [6, 13, 22]. A validated rating scale (Attitudes toward Handheld Decision Support Software Scale (H-DSS)) could be used to assess physician attitudes about handheld decision support systems ([23] but no recent articles mentioned the use of this tool. Another application of mCDSS is the opportunity to alert healthcare workers of relevant information immediately when it becomes available. In a prospective study by Etchells, the provision of real-time clinical alerts and decision support for critical laboratory abnormalities did not improve clinical management or decrease adverse events [12]. [12] A different study evaluating opioid prescribing in pharmacopoeietic apps found that multiple programs fail to prominently display drug safety information. This may be an impediment to safe prescribing and may represent a missed opportunity to improve prescribing practices (Lapoint et al. 2013) [17].
A methodological challenge for future studies will be to evaluate outcome at a patient level. Many CDSS studies measure outcome on a healthcare provider level, whether that is correct diagnosis, drug usage or guideline adherence. Indirectly such outcome parameters should be translatable to improved patient outcome, but this has not been measured directly. Obviously in a clinical setting where many parameters influence patient outcome, isolating the influence of the mCDSS is difficult and may require rather large study cohorts.
For the future, more complex models underlying mCDSS can be implemented. For example, Apple’s CoreML technology allows for applying machine learning models in iOS apps. Using the “coremltools” converter, or “turicreate” for modelling, Python-based models can be easily converted to CoreML-format for implementation in a mobile app. XCode 10 even allows to create machine learning models directly from within the development environment.
4 Software as a Medical Device
In May 2020, the new medical device regulations (MDR 2017/745 of the European Parliament) will become the standard for medical devices, including software applications such as mobile apps. The new Regulations contain a series of important improvements to modernise the current system. Among them are: (Regulatory framework – Growth – European Commission [24])
-
stricter ex-ante control for high-risk devices via a new pre-market scrutiny mechanism with the involvement of a pool of experts at EU level
-
the reinforcement of the criteria for designation and processes for oversight of Notified Bodies
-
the inclusion of certain aesthetic devices which present the same characteristics and risk profile as analogous medical devices under the scope of these Regulations
-
the introduction of a new risk classification system for in vitro diagnostic medical devices in line with international guidance
-
improved transparency through the establishment of a comprehensive EU database on medical devices and of a device traceability system based on Unique Device Identification
-
the introduction of an “implant card” containing information about implanted medical devices for a patient
-
the reinforcement of the rules on clinical evidence, including an EU-wide coordinated procedure for authorisation of multi-centre clinical investigations
-
the strengthening of post-market surveillance requirements for manufacturers
-
improved coordination mechanisms between EU countries in the fields of vigilance and market surveillance
Mobile apps that are considered as a medical device will still need CE (Conformité Européenne) marking , but cannot be registered as a risk class 1 device anymore. As a consequence, self-certification will not be possible, and a notified body is required – a far more expensive necessity.
5 Conclusion
Overall, these are exciting times for mCDSS applications. There is level 1 evidence for their effectiveness, and new opportunities both for collecting data and implementing machine learning models in a mobile app create new horizons for scientific research and improving quality of health and healthcare.
References
Alexander GL. A descriptive analysis of a nursing home clinical information system with decision support. Perspect Health Inf Manag. 2008;5:12.
Berner ES, Houston TK, Ray MN, Allison JJ, Heudebert GR, Chatham WW, et al. Improving ambulatory prescribing safety with a handheld decision support system: a randomized controlled trial. J Am Med Inform Assoc. 2006;13(2):171–9. https://doi.org/10.1197/jamia.M1961.
Bochicchio GV, Smit PA, Moore R, Bochicchio K, Auwaerter P, Johnson SB, et al. Pilot study of a web-based antibiotic decision management guide. J Am Coll Surg. 2006;202(3):459–67. https://doi.org/10.1016/j.jamcollsurg.2005.11.010.
Bot BM, Suver C, Neto EC, Kellen M, Klein A, Bare C, et al. The mPower study, Parkinson disease mobile data collected using ResearchKit. Sci Data. 2016;3:160011. https://doi.org/10.1038/sdata.2016.11.
Chan Y-FY, Bot BM, Zweig M, Tignor N, Ma W, Suver C, et al. The asthma mobile health study, smartphone data collected using ResearchKit. Sci Data. 2018;5:180096–11. https://doi.org/10.1038/sdata.2018.96.
Charani E, Kyratsis Y, Lawson W, Wickens H, Brannigan ET, Moore LSP, Holmes AH. An analysis of the development and implementation of a smartphone application for the delivery of antimicrobial prescribing policy: lessons learnt. J Antimicrob Chemother. 2013;68(4):960–7. https://doi.org/10.1093/jac/dks492.
Chin EF, Sosa M-E, O’Neill ES. The N-CODES project moves to user testing. Comput Inform Nurs. 2006;24(4):214–9.
Clauson KA, Polen HH, Peak AS, Marsh WA, DiScala SL. Clinical decision support tools: personal digital assistant versus online dietary supplement databases. Ann Pharmacother. 2008;42(11):1592–9. https://doi.org/10.1345/aph.1L297.
Cricelli I. Use of personal digital assistant devices in order to access, consult and apply a corpus of clinical guidelines and decision-based support documentation like the Italian SPREAD guidelines on stroke disease. Neurol Sci. 2006;27(S3):s238–9. https://doi.org/10.1007/s10072-006-0626-7.
DI Pietro TL, Nguyen HA, Doran DM. Usability evaluation. Comput Inform Nurs. 2012;30(8):440–8. https://doi.org/10.1097/NXN.0b013e31824af6c0.
Divall P, Camosso-Stefinovic J, Baker R. The use of personal digital assistants in clinical decision making by health care professionals: a systematic review. Health Informatics J. 2013;19(1):16–28. https://doi.org/10.1177/1460458212446761.
Etchells E, Adhikari NKJ, Wu R, Cheung M, Quan S, Mraz R, et al. Real-time automated paging and decision support for critical laboratory abnormalities. BMJ Qual Saf. 2011;20(11):924–30. https://doi.org/10.1136/bmjqs.2010.051110.
Garrett B, Klein G. Value of wireless personal digital assistants for practice: perceptions of advanced practice nurses. J Clin Nurs. 2008;17(16):2146–54. https://doi.org/10.1111/j.1365-2702.2008.02351.x.
Gupta RK, McEvoy MD. Initial experience of the American Society of Regional Anesthesia and Pain Medicine Coags regional smartphone application. Reg Anesth Pain Med. 2016;41(3):334–8. https://doi.org/10.1097/AAP.0000000000000391.
Johansson PE, Petersson GRI, Nilsson GC. Personal digital assistant with a barcode reader – a medical decision support system for nurses in home care. Int J Med Inform. 2010;79(4):232–42. https://doi.org/10.1016/j.ijmedinf.2010.01.004.
Lapinsky SE, Wax R, Showalter R, Martinez-Motta JC, Hallett D, Mehta S, et al. Prospective evaluation of an internet-linked handheld computer critical care knowledge access system. Crit Care. 2004;8(6):R414–21. https://doi.org/10.1186/cc2967.
Lapoint J, Perrone J, Nelson LS. Electronic pharmacopoeia: a missed opportunity for safe opioid prescribing information? J Med Toxicol. 2013;10(1):15–8. https://doi.org/10.1007/s13181-013-0351-6.
Laporta R, Anandam A, El-Solh AA. Screening for obstructive sleep apnea in veterans with ischemic heart disease using a computer-based clinical decision-support system. Clin Res Cardiol. 2012;101(9):737–44. https://doi.org/10.1007/s00392-012-0453-1.
Lee N-J, Chen ES, Currie LM, Donovan M, Hall EK, Jia H, et al. The effect of a mobile clinical decision support system on the diagnosis of obesity and overweight in acute and primary care encounters. ANS Adv Nurs Sci. 2009;32(3):211–21. https://doi.org/10.1097/ANS.0b013e3181b0d6bf.
Leung GM, Johnston JM, Tin KYK, Wong IOL, Ho L-M, Lam WWT, Lam T-H. Randomised controlled trial of clinical decision support tools to improve learning of evidence based medicine in medical students. BMJ (Clinical Research Ed). 2003;327(7423):1090. https://doi.org/10.1136/bmj.327.7423.1090.
Mobile Operating System Market Share United States of America|StatCounter Global Stats. Mobile Operating System Market Share United States of America|StatCounter Global Stats. n.d. Retrieved June 22, 2018, from http://gs.statcounter.com/os-market-share/mobile/united-states-of-america
Payne KF, Weeks L, Dunning P. A mixed methods pilot study to investigate the impact of a hospital-specific iPhone application (iTreat) within a British junior doctor cohort. Health Informatics J. 2013;20(1):59–73. https://doi.org/10.1177/1460458213478812.
Ray MN, Houston TK, Yu FB, Menachemi N, Maisiak RS, Allison JJ, Berner ES. Development and testing of a scale to assess physician attitudes about handheld computers with decision support. J Am Med Inform Assoc. 2006;13(5):567–72. https://doi.org/10.1197/jamia.M2096.
Regulatory framework – Growth – European Commission. Regulatory framework – Growth – European Commission. n.d. Retrieved June 22, 2018, from https://ec.europa.eu/growth/sectors/medical-devices/regulatory-framework_en
Roy P, Durieux P, Gillaizeau F, Legall C, Armand-Perroux A, Martino L, et al. A computerized handheld decision-support system to improve pulmonary embolism diagnosis: a randomized trial. Ann Intern Med. 2009;151(10):677–86. https://doi.org/10.1059/0003-4819-151-10-200911170-00003.
Rubin MA, Bateman K, Donnelly S, Stoddard GJ, Stevenson K, Gardner RM, Samore MH. Use of a personal digital assistant for managing antibiotic prescribing for outpatient respiratory tract infections in rural communities. J Am Med Inform Assoc. 2006;13(6):627–34. https://doi.org/10.1197/jamia.M2029.
Samore MH, Bateman K, Alder SC, Hannah E, Donnelly S, Stoddard GJ, et al. Clinical decision support and appropriateness of antimicrobial prescribing: a randomized trial. JAMA. 2005;294(18):2305–14. https://doi.org/10.1001/jama.294.18.2305.
Sintchenko V, Iredell JR, Gilbert GL, Coiera E. Handheld computer-based decision support reduces patient length of stay and antibiotic prescribing in critical care. J Am Med Inform Assoc. 2005;12(4):398–402. https://doi.org/10.1197/jamia.M1798.
Snooks HA, Carter B, Dale J, Foster T, Humphreys I, Logan PA, et al. Support and Assessment for Fall Emergency Referrals (SAFER 1): cluster randomised trial of computerised clinical decision support for paramedics. PLoS One. 2014;9(9):e106436. https://doi.org/10.1371/journal.pone.0106436.
Snooks H, Cheung W-Y, Close J, Dale J, Gaze S, Humphreys I, et al. Support and Assessment for Fall Emergency Referrals (SAFER 1) trial protocol. Computerised on-scene decision support for emergency ambulance staff to assess and plan care for older people who have fallen: evaluation of costs and benefits using a pragmatic cluster randomised trial. BMC Emerg Med. 2010;10(1):268. https://doi.org/10.1186/1471-227X-10-2.
Spat S, Donsa K, Beck P, Höll B, Mader JK, Schaupp L, et al. A mobile computerized decision support system to prevent hypoglycemia in hospitalized patients with type 2 diabetes mellitus. J Diabetes Sci Technol. 2016;11(1):20–8. https://doi.org/10.1177/1932296816676501.
Stephens MB, Waechter D, Williams PM, Williams AL, Yew KS, Strayer SM. Institutional support for handheld computing: clinical and educational lessons learned. Med Ref Serv Q. 2010;29(1):28–36. https://doi.org/10.1080/02763860903485035.
Van Belle VMCA, Van Calster B, Timmerman D, Bourne T, Bottomley C, Valentin L, et al. A mathematical model for interpretable clinical decision support with applications in gynecology. PLoS One. 2012;7(3):e34312–0. https://doi.org/10.1371/journal.pone.0034312.
Yu F, Houston TK, Ray MN, Garner DQ, Berner ES. Patterns of use of handheld clinical decision support tools in the clinical setting. Med Decis Mak. 2007;27(6):744–53. https://doi.org/10.1177/0272989X07305321.
Zens M, Woias P, Suedkamp NP, Niemeyer P. “Back on track”: a mobile app observational study using Apple’s ResearchKit framework. JMIR Mhealth and Uhealth. 2017;5(2):e23–13. https://doi.org/10.2196/mhealth.6259.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2019 The Author(s)
About this chapter
Cite this chapter
Kubben, P. (2019). Mobile Apps. In: Kubben, P., Dumontier, M., Dekker, A. (eds) Fundamentals of Clinical Data Science. Springer, Cham. https://doi.org/10.1007/978-3-319-99713-1_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-99713-1_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-99712-4
Online ISBN: 978-3-319-99713-1
eBook Packages: MedicineMedicine (R0)