Abstract
Background: Overweight and obesity have been linked with several objective and subjective measures of health. However, results are mixed and this relationship seems to vary across populations, genders and age categories. This paper investigates the relationship between categories of the Body Mass Index (underweight, normal weight, overweight, obesity and severe obesity) and satisfaction with health.
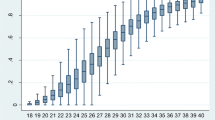
Methods: Data come from eleven waves of the Swiss Household Panel (2004–2014). Analyses are based on 7151 men and 8142 women aged between 18 and 75. Satisfaction with health was measured on a ten-point scale. Pooled OLS, random and fixed effects were estimated.
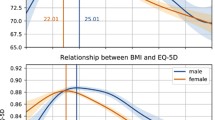
Results: Overall, departures from the normal weight range seemed to decrease the individual satisfaction with health. Obesity and severe obesity appeared to have the strongest impact on satisfaction with health and this is particularly so in the case of women.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
According to the World Health Organization (WHO 2016), worldwide the prevalence of obesity has more than doubled since 1980 and in 2014 600 million people were obese. In many countries, childhood obesity is increasing at an even higher rate than adult obesity, what would probably lead to a further increase in the prevalence of obesity, given that obese children are more likely to become obese adults (Singh et al. 2008; Reilly and Kelly 2011).
In Switzerland obesity rates are low compare to most OECD countries, but they have increased significantly in the last twenty years: in 1992, 31.3% of the Swiss population was overweight or obese, and this increased to 41,2 % in 2012 (Schneider and Venetz 2014). According to the most recent estimates of the Swiss Survey on Health, in 2012 41% of the Swiss population aged over 15 years appear to be overweight or obese (Federal Office of Public Health (FOPH) 2014).
Obesity, defined as excessive body fat and typically measured using the Body Mass Index (BMI) (WHO 2016), can impair health. There is robust evidence suggesting that obesity is an important risk factors for a set of health problems and diseases such as diabetes, cardiovascular diseases, hypertension, respiratory problems, musculoskeletal diseases and some forms of cancer (Hu 2008; WHO 2016; Imai et al. 2008). Interestingly, the link between obesity and health has been confirmed in studies using a variety of different health indicators, such as measures of health related quality of life (Garner et al. 2011; Ford et al. 2001), measures of functional health (Ford et al. 2001; Imai et al. 2008) or self-assessed health (Cullinan and Gillespie 2016; Imai et al. 2008). Obesity has also been associated with poor mental health and depression (Ford et al. 2001; Imai et al. 2008; Luppino et al. 2010) and this is not surprising given the fact that obese person tend to suffer from prejudices and discrimination in several life domains and might suffer from low self-esteem (Puhl and Heuer 2009). Weight-related stigma seems to be particularly relevant for women, who tend to suffer the most from being obese and are more discriminated than their male counterparts (Puhl and Heuer 2009; Puhl and Brownell 2003; Hebl and Turchin 2005; Wadsworth and Pendergast 2014). These cultural reasons, together with possible physiological reasons, might explain why in some studies obesity appears to have worse health related consequences for women rather than for men (Garner et al. 2012; Wang et al. 2012).
Overweight, concof the Swiss population was overweight or obese,erning around 1,8 billion adults worldwide (WHO 2016), has also been linked to health-related conditions, but the evidence is more mixed and, in the majority of studies, overweight does not appear to increase mortality risk (rather, some studies suggested a protective role of overweight, at least in men and in the elderly) (Cullinan and Gillespie 2016; Garner et al. 2012; Lantz et al. 2010; Berrington de Gonzalez et al 2010; Flegal et al. 2007; Imai et al. 2008).
The relationship between BMI and health, hence, does not seem to be a strictly linear one. This is particularly so because several studies reported underweight to be a risk factor for health and premature mortality as well (Garner et al. 2012; Flegal et al. 2007; Imai et al. 2008; Ford et al. 2001). Again, this relationship seems to vary across age categories and gender: for instance, Garner et al. (2012) found underweight to be protective in terms of health related quality of life for young women. Despite the great deal of evidence about the link between obesity/BMI and health, the causal nature of this relationship is still disputed. There is a huge literature -comprising observational, intervention and genetic epidemiological studies using mendelian randomization (MR) - that has investigated this issue (Corbin and Timpson 2016). Every approach presents some limits in its ability to assess the causal link between obesity (or BMI) and health outcomes (confounding bias, reversed causality) and even the instrumental variable approach can be criticized because it ultimately relies on assumptions that are difficult to test (Cameron and Trivedi 2009). Moreover, results are mixed, though some MR studies (in which genetic variation is used as an instrumental variable) have found evidence of causal effects of obesity on several physical and mental health outcomes (Corbin and Timpson 2016).
This study specifically focuses on the relationship between BMI and satisfaction with health. Satisfaction with health belongs to the group of subjective measures of health that can encompass aspects of both physical and mental health, reflecting a complex process of internalized reckoning. In the health literature subjective measures of health, such as Self-Assessed Health (SAH), are widely used. Despite being a very simple measure of health, SAH is extremely powerful and appears to be related to several objective measures of health, such as morbidity and functional limitations, and it is able to predict mortality above and beyond the individual objective health status (Benyamini 2011; Benjamins et al. 2004; Idler and Benyamini 1997; Jylha 2009). The negative association between obesity and SAH has been found to hold true for adults as well as for adolescents (Imai et al. 2008; Krause and Lampert 2015; Vingilis et al. 2002), and in several countries, like Switzerland, Ireland and the USA (Cullinan and Gillespie 2016; Prosper et al. 2009; Marques-Vidal et al. 2012). However, this relationship has not been found in countries such as Portugal and Greece (Darviri et al. 2012; Marques-Vidal et al. 2012) and in specific subpopulations such as Latino immigrants living in the USA (Macmillan et al. 2011).
Moreover, the association of BMI with SAH appears to vary significantly across ages and sexes (Imai et al. 2008), although not in all studies: for instance, Cullinan and Gillespie (2016) did not find substantial differences among genders concerning the impact of obesity on SAH.
Variation in results might reflect real differences, due to the specific population under study and its cultural specificities. However, methodological shortcomings might also be partly responsible for mixed findings. Indeed, previous studies in this field have mostly used cross-sectional data and were not able to adequately control for potential confounders. One notable exception is the study by Cullinan and Gillespie (2016) who adopted the instrumental variable approach to assess the effect of obesity and overweight (underweight was not considered) on SAH in a nationally representative sample of Irish people. The authors concluded that obesity (and particularly severe obesity) negatively impacts SAH, whereas overweight does not seem to affect SAH.
The present study aimed to investigate the relationship between BMI and satisfaction with health in Switzerland, using longitudinal studies and applying panel data regression models that partly allow to control for unobserved heterogeneity.
Data and Variables
For our analysis we used data from the Swiss Household Panel (SHP), a representative longitudinal study of household and individuals, supported by the Swiss National Science Foundation, which began in 1999 with a sample of 5074 households containing 12,931 household members.Footnote 1 More precisely, we used the eleven waves from 2004 to 2014. We selected 103,861 observations nested into 22,815 individuals, aged 18–75. The dependent variable — satisfaction with health— was measured on a scale ranging from 0 (not at all satisfied) to 10 (completely satisfied). Despite its ordinal nature, following Ferrer-i-Carbonell and Frijters (2004) we considered satisfaction with health as a cardinal variable in order to facilitate interpretation of the estimated parameters. Our main focus was BMI that was coded into five categories, according to the thresholds set by the World Health Organization, as follows: underweight (BMI < 18.50), normal weight (BMI > 18.50 to 24.99), overweight (BMI >24.99 to 29.99), obesity class I (BMI >29.99 to 34.99), obesity class II and III (BMI > 34.99), also called “severe obesity”. In the regression models, normal weight was the category of reference.
All models included a set of control variables, that have been proven to affect health and, in many cases, BMI as well: age, age squared, gender, a set of social relationship indicators such as civil status dummies (single, married, separated, divorced, widow), number of children in the family, size of household, death of closely related person (dummy), termination of close relationship (dummy), conflicts with or among related persons (dummy) (Umberson and Karas Montez 2010; Umberson et al. 2006); social status indicators such as the logarithm of net total annual household income, work status (employed, unemployed, not in labour force), and education dummies (less than secondary education, secondary education, tertiary education) (Marmot and Wilkinson 2006; McLaren 2007), physical activity (dummy) (Wanner et al. 2017), regional dummies (Lake Geneva, Middleland, North-West Switzerland, Zurich, East Switzerland, Central Switzerland, Ticino) (Ogna et al. 2014) and wave dummies (2004–2014). Since previous studies found gender differences in the association between self-rated health and BMI, descriptive analysis (see Table 2.1) and regression models (see Table 2.2) were carried out separately for men and women.
Analytic Strategies
In order to investigate the existence and the nature of the relationship between health and BMI categories, we adopted different analytical strategies, with the aim of exploiting the strength of panel data and understanding to which extend unobserved individual heterogeneity could introduce a bias in the parameter estimates. More precisely, we estimated three types of regression models —pooled OLS, random effect (RE) and fixed effect (FE) models— as follows:
Where SWH it was the satisfaction with health score of respondent i at time t; X it was a vector of K time-varying BMI dummies; Z it and W i represented, respectively, a vector of Q time-varying and R time-constant characteristics, that we considered as control variables. Finally, \( {\alpha}_i \)was a time-invariant individual-specific effect; \( {\psi}_t \) corresponded to wave effects and \( {\varepsilon}_{it} \) was the idiosyncratic error term.
Firstly, we estimated OLS pooled regression models with clustered standard errors and subsequently random effect models (RE) that enabled us to study the effect of both time-constant and time-varying covariates. These analytical strategies allowed us to take into account differences across individuals and to control for time invariant variables. It is important to underline that since BMI is an endogenous variable, these models would give biased results, as they unrealistically assume the causal variable to be uncorrelated with the error term (Cameron and Trivedi 2009).
If variables of interest showed enough intra-individual variation, fixed effect models (FE) were also implemented. FE yields an unbiased estimate of the causal parameter by erasing the influence of time constant unobserved variables (Cameron and Trivedi 2009). This means that this estimation method allowed us to control for crucial unobservable differences in time constant individual characteristics like personality, dispositions or genetic traits that are known to be important determinants of satisfaction with health. In order to test if RE was more appropriate than FE, or vice versa, we ran a Hausman Test.
Empirical Results
Effects of BMI on satisfaction with health, obtained by applying OLS, RE and FE estimators, are reported in Table 2.2.
Overall, we could see that the sign of the coefficients were consistent and in line with the literature, although, as expected, there appeared to be a shrink in the size of estimates moving from the OLS to RE and from RE to the FE specifications.
The OLS estimates suggest that individuals with normal weight enjoyed a better health status than individuals belonging to others categories. Those with the lowest level of satisfaction with health were severely obese individuals (i.e. obesity class II and III), followed by obese individuals (obesity class I) and overweight individuals. This appeared to be true for both men and women, though these effects appeared to be more pronounced among women. Indeed, among men severe obesity reduced satisfaction with health by 0.791 points (on a 10 point-scale), among women the reduction reached 1 point.
Overweight also appeared to decrease the level of satisfaction with health, and particularly so for women. Being underweight was also associated with lower levels of satisfaction with health, but the coefficient for men did not reach statistical significance and it was only significant at the 1% level in women.
Looking at the OLS estimates for the chosen control variables, we could see that getting married (for women), secondary and tertiary education, family income, physical activity, Swiss nationality (for women) and living in Ticino (for men) were positively associated with satisfaction with health. On the contrary, ageing, getting married (for women) unemployment, inactivity, the death of a closely related person, the termination of a close relationship, the conflicts with or among related persons were negatively correlated with satisfaction with health.
RE estimates tell us roughly the same story, even though it is important to emphasize a remarkable reduction in the size of the parameter estimates. More precisely, the negative effect of obesity class II and III decreased from −0.791 to −0.565 in the male sample and from −1.002 to −0.865 in the female one. For the obesity class I the size of the effect changed from −0.438 to −0.332 for male and from −0.676 to −0.497 for female.
Finally, FE parameter estimates tell us a slightly different story. For men, the effect of the BMI categories decreased in size and lost statistical significance. For women, we observed that the size of the estimates of interest decreased, while maintaining statistical significance. This means that a change in a woman’s BMI leads to a change in satisfaction with health, whereas the same conclusion does not apply to men. Women belonging to obesity class II and III showed the lowest level of satisfaction with health (0.521 point less than normal weight woman), followed by women belonging to obesity class I (−0.237), underweight (−0.157) and overweight (−0.088) women. These results might reflect the fact that weight related stigma is stronger for women and obese women tend to suffer more because of their weight status (Puhl and Heuer 2009; Puhl and Brownell 2003; Hebl and Turchin 2005; Wadsworth and Pendergast 2014) and are consistent with what has been found in some studies (Garner et al. 2012; Wang et al. 2012), albeit not in all.
A Hausman model selection test was run in order to understand whether the FE estimator was more efficient than the RE. According to this test, the FE should be preferred over the RE model in that time constant unobserved characteristics were likely to be associated with our BMI dummies.
Overall, these results suggested that, even after controlling for a range of individual, socioeconomic and lifestyle related variables, departures from normal weight had statistically significant negative impact on women’s satisfaction with health. More precisely, we could see a dose-response relationship, whereby being obese had a stronger negative effect than being overweight and being severely obese had a stronger effect than being obese. The effect of underweight on women’s satisfaction with health was less pronounced but still statistically significant (in line with results from Imai et al. 2008). Working on Canadian women, Garner et al. (2012) found a protective effect of underweight on women’s self-assessed health, at least at younger ages, but this might reflect cultural difference in the value attributed to thinness. This difference could also be due to the fact that FE models applied in this study are not fully able to tackle the issue of reversed causality.
Conclusion
Obesity is an important risk factor for a number of diseases (cardiovascular diseases, type 2 diabetes, hypertension, some cancers, musculoskeletal disorders, etc.) and obese individuals often face discrimination and stigmatization in important domains of life and tend to report lower level of self-esteem and mental health (Hu 2008; WHO 2016; Puhl and Heuer 2009; Hebl and Turchin 2005).
Hence, the association between obesity and subjective measures of health is not surprising, since this kind of subjective measures are likely to capture aspect of both physical and mental health. However, the role of overweight and underweight is less clear and studies investigating the relationship between BMI and health have provided mixed results.
Cultural as well as methodological reasons can explain these differences. The strength of the social penalty associated with overweight and obesity can vary over population sub-groups and across societies. Moreover, previous studies in this field have not generally addressed nor taken into account the issue of endogeneity and reverse causality (with the exception of Cullinan and Gillespie 2016).
In this work, we exploited the power of panel data and appropriate analytic strategies to overcome this limitation. Working with data coming from the Swiss Household Panel (waves 2004–2015), we modelled the relationship between BMI and satisfaction with health using pooled OLS, random effects and fixed effects. Since the impact of BMI has been shown to vary between genders, we estimated separate models for women and men.
Overall, our results confirmed the non-linearity in the relationship between BMI and health.
Estimates from pool OLS and RE models showed that women and men belonging to BMI categories different from normal weight had a significantly lower level of satisfaction with health. These effects were more pronounced for women than for men.
FE estimates —that allow removing the time constant individual heterogeneity— showed that any departures from normal weight appeared to be associated with lower levels of satisfaction with health in women, but not in men. These results support previous findings showing gender differences in the association between BMI and health (Imai et al. 2008; Ford et al. 2001; Garner et al. 2012).
In every model, obese and severely obese individuals appeared to be the ones with the lowest level of satisfaction with health. Given that the prevalence of obesity is rising worldwide, these results calls for action. The pathways through which obesity impacts on health satisfaction need to be further explored. However, gender differences in empirical results suggest that stigma plays a crucial role. Interventions to tackle the stigma issue are needed together with actions to counteract the obesity epidemic.
References
Benjamins, M. R., Hummer, R. A., Eberstein, I., & Nam, C. B. (2004). Self-reported health and adult mortality risk: An analysis of cause-specific mortality. Social Science & Medicine, 59, 1297–1306.
Benyamini, Y. (2011). Why does self-rated health predict mortality? An update on current knowledge and a research agenda for psychologist. Psychology & Health, 26, 1407–1413.
Berrington de Gonzalez, A., Hartge, P., Cerhan, J. R., Flint, A. J., Hannan, L., & MacInnis, R. J. (2010). Body-mass index and mortality among 1.46 million white adults. The New England Journal of Medicine, 363(23), 2211–2219.
Cameron, C., & Trivedi, P. K. (2009). Microeconometrics using stata. College Station: Stata Press.
Corbin, L. J., & Timpson, N. J. (2016). Body mass index: Has epidemiology started to break down causal contributions to health and disease? Obesity, 24, 1630–1638. https://doi.org/10.1002/oby.21554.
Cullinan, J., & Gillespie, P. (2016). Does overweight and obesity impact on self-rated health? Evidence using instrumental variables ordered Probit models. Health Economics, 25(10), 1341–1348.
Darviri, C., Fouka, G., Gnardellis, C., Artemiadis, A. K., Tigani, X., & Alexopoulos, E. C. (2012). Determinants of self-rated health in a representative sample of a rural population: A cross-sectional study in Greece. International Journal of Environmental Research and Public Health, 9(3), 943–954.
Ferrer-i-Carbonell, A., & Frijters, P. (2004). How important is methodology for the estimates of the determinants of happiness? The Economic Journal, 114, 641–659.
Flegal, K. M., Graubard, B. I., Williamson, D. F., & Gail, M. H. (2007). Cause-specific excess deaths associated with underweight, overweight, and obesity. The Journal of the American Medical Association, 298(17), 2028–2037.
Ford, E. S., Moriarty, D. G., Zack, M. M., Mokdad, A. H., & Chapman, D. P. (2001). Self-reported body mass index and health-related quality of life: Findings from the behavioral risk factor surveillance system. Obesity Research, 9(1), 21–31.
Garner, R. E., Feeny, D. H., Thompson, A., Bernier, J., McFarland, B. H., Huguet, N., Kaplan, M. S., Orpana, H., Ross, N. A., & Blanchard, C. (2012). Bodyweight, gender, and quality of life: A population-based longitudinal study. Quality of Life Research, 21(5), 813–825.
Hebl, M. R., & Turchin, J. M. (2005). The stigma of obesity: What about men? Basic Applied Social Psychology, 27(3), 267–275.
Hu, F. B. (2008). Obesity epidemiology. New York: Oxford University Press.
Idler, E. L., & Benyamini, Y. (1997). Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior, 38, 21–37.
Imai, K., Gregg, E. W., Chen, Y. J., Zhang, P., de Rekeneire, N., & Williamson, D. F. (2008). The association of BMI with functional status and self-rated health in US adults. Obesity, 16(2), 402–408.
Jylha, M. (2009). What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Social Science and Medicine, 69, 307–316.
Krause, L., & Lampert, T. (2015). Relation between overweight/obesity and self-rated health among adolescents in Germany. Do socio-economic status and type of school have an impact on that relation? International Journal of Environmental Research and Public Health, 12(2), 2262–2276.
Lantz, P. M., Golberstein, E., House, J. S., & Morenoff, J. (2010). Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of U.S. adults. Social Science & Medicine, 70(10), 1558–1566.
Luppino, F. S., de Wit, L. M., Bouvy, P. F., Stijnen, T., Cuijpers, P., Penninx, B. W., & Zitman, F. G. (2010). Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry, 67(3), 220–229.
Macmillan, R., Duke, N., Oakes, J. M., & Liao, W. (2011). Trends in the association of obesity and self-reported overall health in 30 years of the integrated health interview series. Obesity, 19(5), 1103–1105.
Marmot, M., & Wilkinson, R. (Eds.). (2006). Social determinants of health. New York: Oxford University Press.
Marques-Vidal, P., Ravasco, P., & Paccaud, F. (2012). Differing trends in the association between obesity and self-reported health in Portugal and Switzerland. Data from national health surveys 1992-2007. BMC Public Health, 12, 588.
McLaren, L. (2007). Socioeconomic status and obesity. Epidemiologic Reviews, 29, 29–48.
Ogna, A., Forni Ogna, V., Bochud, M., Paccaud, F., Gabutti, L., & Burnier, M. (2014). Prevalence of obesity and overweight and associated nutritional factors in a population-based Swiss sample: An opportunity to analyze the impact of three different European cultural roots. European Journal of Nutrition, 53(5), 1281–1290.
Prosper, M., Moczulski, V. L., & Qureshi, A. (2009). Obesity as a predictor of self-rated health. American Journal of Health Behavior, 33(3), 319–329.
Puhl, R. M., & Brownell, K. D. (2003). Psychological origins of obesity stigma: Toward changing a powerful and pervasive Bias. Obesity Reviews, 4, 213–227.
Puhl, R. M., & Heuer, C. A. (2009). The stigma of obesity: A review and update. Obesity, 17(5), 941–964.
Reilly, J. J., & Kelly, J. (2011). Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. International Journal of Obesity, 35(7), 891–898.
Schneider, H., & Venetz, W. (2014). Cost of obesity in Switzerland in 2012. Final report. Swiss Federal Office of Public Health.
Singh, A. S., Mulder, C., Twisk, J. W. R., Van Mechelen, W., & Chinapaw, M. J. M. (2008). Tracking of childhood overweight into adulthood: A systematic review of the literature. Obesity Reviews, 9(5), 474–488.
Umberson, D., & Karas Montez, J. (2010). Social relationships and health: A flashpoint for health policy. Journal of Health and Social Behavior, 51(Suppl), S54–S66.
Umberson, D., Williams, K., Powers, D., Liu, H., & Needham, B. (2006). You make me sick: Marital quality and health over the life course. Journal of Health and Social Behavior, 47(1), 1–16.
Vingilis, E. R., Wade, T. J., & Seeley, J. S. (2002). Predictors of adolescent self-rated health. Analysis of the National Population Health Survey. Canadian Journal of Public Health, 93(3), 193–197.
Wadsworth, T., & Pendergast, P. M. (2014). Obesity (sometimes) matters: The importance of context in the relationship between obesity and life satisfaction. Journal of Health and Social Behavior, 55(2), 196–214.
Wang, R., Wu, M. J., Ma, X. Q., Zhao, Y. F., Yan, X. Y., Gao, Q. B., & He, J. (2012). Body mass index and health-related quality of life in adults: A population based study in five cities of China. European Journal of Public Health, 22(4), 497–502.
Wanner, M., Richard, A., Martin, B., Faeh, D., & Rohrmann, S. (2017). Associations between self-reported and objectively measured physical activity, sedentary behavior and overweight/obesity in NHANES 2003–2006. International Journal of Obesity, 41(1), 186–193.
World Health Organization (WHO). (2016). Obesity and overweight. Fact sheet N.311 Available at http://www.who.int/mediacentre/factsheets/fs31/en/.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
<SimplePara><Emphasis Type="Bold">Open Access</Emphasis> This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.</SimplePara> <SimplePara>The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.</SimplePara>
Copyright information
© 2018 The Author(s)
About this chapter
Cite this chapter
Lucchini, M., Della Bella, S. (2018). Body Mass Index and Satisfaction with Health in Contemporary Switzerland. In: Tillmann, R., Voorpostel, M., Farago, P. (eds) Social Dynamics in Swiss Society. Life Course Research and Social Policies, vol 9. Springer, Cham. https://doi.org/10.1007/978-3-319-89557-4_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-89557-4_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-89556-7
Online ISBN: 978-3-319-89557-4
eBook Packages: Social SciencesSocial Sciences (R0)