Abstract
According to the World Health Organization, acute lower respiratory tract infection (ALRI) is the fourth leading cause of death worldwide, responsible for approximately 3.1 million (5.5%) of the 56 million estimated deaths per year. Human respiratory syncytial virus (RSV) is recognized as the most important cause of ALRI in infants worldwide. It is estimated that every year 33.8 million new cases of RSV-related ALRIs occur and cause approximately 200,000 deaths in children younger than 5 years; of note, 99% of these deaths occur in developing countries. Usually primary infections occur during the first 2 years of life and are symptomatic, causing from mild upper respiratory tract illness to severe ALRI, and in some cases pneumonia and bronchiolitis may occur simultaneously. Recurrent infections throughout life are common but normally cause milder upper respiratory tract illness. Several studies also associated severe RSV infections during infancy with permanent lung function reduction in adulthood, with higher risk of asthma. The seasonality of the virus varies but it is often detected throughout the year. In South America the highest incidence occurs in the months of January to June. Despite the clinical importance and the disease burden associated with RSV, there is neither specific treatment nor vaccines widely accepted and available nowadays.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- HRSV
- Respiratory syncytial virus
- Respiratory viruses
- Molecular diagnostic
- Molecular epidemiology
- Virus replication
- HRSV genotype
- Virus resistance
- Palivizumab
1 Introduction
Acute respiratory infections (ARIs) are the most frequent infectious disease in humans, and the great majority of respiratory infections observed in medical practice around the world are of viral etiology [3, 34, 80]. During the period of 2000 to 2003, an estimate of 10,600,000 children under the age of 5 years died every year, and ARIs were responsible for nearly 19% of these deaths. Most of these fatalities were caused by bronchitis and pneumonia associated with viral infections [14, 57, 106, 119]. Viral respiratory infections are also associated with high morbidity in this age group worldwide. For example, 35% of hospitalized children in Brazil, 35% in Belgium, 22% in Italy, and 59% in the UK attending pediatric services were the result of viral respiratory infections [78, 84, 85, 87, 98].
Currently, the following viruses shall be considered causes of acute respiratory illness in children: human respiratory syncytial virus (HRSV); parainfluenza virus types 1, 2, 3, and 4 (PIV1, PIV2, PIV3, PIV4); influenza virus types A, B, C (IA, IB, IC); adenoviruses (ADV) ; coronaviruses HCoV-OC43, HCoV-229E, HCoV-HKU1, and HCoV-NL64; human rhinovirus (HRV) ; some subtypes of enterovirus (HEV-68); human metapneumovirus (hMPV) ; human bocavirus (HBoV) ; and WU and KI polyomavirus (Fig. 12.1). However, some viruses present high rates of co-detection, as is the case of rhinovirus, enterovirus, human coronavirus and bocavirus, and polyomavirus, being questioned for its significance in the etiology of these infections [10, 45, 49, 64, 89, 91, 96, 114].
Clinical association with major symptoms of disease and respiratory viruses. In South America, studies conducted in different regions of the country indicate the importance of viruses as etiological agents of low respiratory infection (LRI) . These studies revealed the presence of different respiratory viruses in children and adults, such as human respiratory syncytial virus (HRSV), influenza A and B, HPIV, HAdV, HRV, hMPV, hBoV, and HCoV; the percentage of cases among children for some type of respiratory viruses ranged between 28.75% and 75%, whereas positivity in adults was 61.8% for at least one of the viruses studied [11, 15, 35, 39, 40, 85, 105, 111, 116]
The seasonality of respiratory viruses is described in several studies, with some viral infections taking place throughout the year, such as influenza virus, with a predominance in the winter months [96], and others occurring chiefly in the late fall, winter, or early spring, such as HPIV, hMPV, HCoV, and HRSV [85, 99, 105, 114]. Adenoviruses are found worldwide and can circulate sporadically, endemically, or epidemically in the winter, spring, and early summer [103, 105].
Despite the great number of viral agents involved in respiratory infections and their importance, the HRSV is the leading cause of acute respiratory infections and one of the leading causes of hospitalization and death among children under 5 years of age worldwide. Each year, respiratory syncytial virus (RSV) infections lead to 2,100,000 outpatient attendances and 57,257 hospitalizations of children less than 5 years of age in the U.S. Additionally, RSV is responsible for 177,000 hospitalizations with 14,000 deaths among adults over 65 years of age [24].
Newborns, premature infants, and those with chronic lung disease are at greater risk of developing severe disease by infection with HRSV [48]. Despite their importance, there is no vaccine prophylaxis against HRSV infection or effective antiviral therapy available. Currently, in Latin America, only palivizumab (Pz) (Synagis; MedImmune, Gaithersburg, MD, USA) is being used in the prophylaxis and therapy of these infections [68].
2 History of the HRSV
In 1955, an outbreak of respiratory illness characterized by coughing, sneezing, and mucopurulent discharge was described in a colony of 20 chimpanzees at the Walter Reed Army Institute of Research (WRAIR) (Washington, DC, USA). During that episode, the RSV was isolated for the first time from a swab from the throat of a female chimpanzee and then called the chimpanzee coryza agent (CCA) [82]. Viral isolation was performed in liver cells, later being inoculated in various laboratory animals, mice, hamsters, rabbits, rats, and chimpanzees, the latter being the only ones to develop specific symptoms.
One of the attendants of the chimpanzees became sick and developed symptoms similar to those of the animals. Although the attempt at isolation of human respiratory syncytial virus was unsuccessful, an increase in antibody titer by complement fixation against CCA was detected. Parallel seroprevalence studies conducted in a human general population revealed the presence of antibodies to a new CCA agent in teenagers and adults.
The following year, Chanock and colleagues isolated a virus similar to the CCA of a child with pneumonia and another with croup, in Baltimore [25, 26]. The agent was named human respiratory syncytial virus, HRSV, to reflect its ability to form syncytia in cell culture and its tropism for the human respiratory tract.
Serological studies carried out at the time indicated that the majority of children in Baltimore had been infected with HRSV before 4 years of age. Similar investigations in diverse parts of the world indicated that the HRSV was associated with diseases of the lower respiratory tract [33]. Currently, HRSV is recognized as the viral agent more frequently related to cases of bronchiolitis and pneumonia during infancy and preschool age. About 95% of the children have the first HRSV infection in the first 2 years of life, and the peak incidence occurs in the first few months [3]. Approximately 40% of children develop symptoms of lower respiratory tract involvement during the first infection. Although reinfections are common during a lifetime, the clinical symptoms in older children and adults are less severe [55].
Some groups of patients are at risk of developing serious illness resulting from the lower respiratory tract infection by HRSV; these include children younger than 6 months of age, premature infants, immunodeficient children, and children with chronic lung disease or congenital heart disease [33]. There are also studies relating the HRSV to severe infections in the elderly [44, 117].
3 Classification
The human respiratory syncytial virus (HRSV) is a member of the order Mononegavirales (mono, from Greek, meaning “single, simple”; nega, from Latin, meaning “RNA negative polarity”; virales, from Latin, meaning virus), classified within the Pneumoviridae family and the genus Orthopneumovirus. Other members of the Orthopneumovirus genus are the bovine respiratory syncytial virus (BRSV) and the pneumonia virus of mice (murine pneumonia virus) [125].
4 Structure
The virion is pleomorphic with a diameter of 150–300 nm and is composed of an internal nucleocapsid of helical symmetry and an envelope derived from the host cytoplasmic membrane; viral glycoproteins that protrude from the envelope as 11- to 20-nm projections, separated by intervals of 6–10 nm, are involved in the processes of adherence and penetration of the virus. The viral genome is composed of a single-stranded RNA molecule, not segmented, and with negative polarity. Each infectious particle contains only one functional copy of the genome (Fig. 12.2) [33].
5 Genomic Organization
The virus contains a single-stranded negative-sense RNA genome with 15,222 nucleotides (nt), with molecular weight of 5 × 106 Da, which serves as a template for transcription of messenger RNAs (mRNAs) , encoding for 11 proteins. The genome transcription takes place in the 5′ → 3′ direction. The 3′-region of the genomic RNA consists of a region of 44 nucleotides that presumably contains the viral promoter [81]. The first 30 nt in this region are highly susceptible to inactivation by the insertion or deletion of nucleotides. This region is followed by 10 genes that encode 11 proteins, in the following order: NS1, NS2, N, P, M, SH, G, F, M2, L. The last gene, L, is followed by a region that is more tolerant to the insertion or deletion of nucleotides [81].
The first nine genes are separated by inter-gene regions ranging from 1 to 52 nt in size, which apparently do not have an important role in the modulation of gene expression and show little conservation among isolates [31, 71]. The beginning of each gene contains a conserved signal (gene start signal) composed of nine nucleotides, 3′-CCCCGUUUA, except for the L gene, which presents the following differences as underlined: 3′-CCCUGUUUUA. The genes end with a semi-conserved sign (gene end signal) composed of 12 or 13 nucleotides whose sequence is 3′-UCAAUNAAAUUU, which drives the end of transcription and polyadenylation. The last two genes, M2 and L, have in common 68 nt. Consequently, the gene L has the initiation of the transcript inside the M2 gene [33]. The M2 has two ORFs (open reading frames), which give rise to proteins M2-1 and M2-2. The organization of the gene of HRSV is schematized in Fig. 12.3.
Organization of the gene in the genome of HRSV. The genome is 15,225 nucleotides long, a single-stranded RNA with negative polarity. It has 10 genes encoding 11 proteins . The M2 gene has two products: a nucleocapsid-associated transcription factor (M2-1) and another protein involved in genome replication (M2-2)
6 Proteins
In cells infected with HRSV, 11 proteins have been identified. Of these, 2 are nonstructural proteins, NS1 and NS2, present in abundance in the cells, but in small amounts in the virion. The others are structural proteins, M (matrix) and M2-1(transcriptiol elongation factor) proteins, N (nucleoprotein), P (phosphoprotein), L (large polymerase), and M22 nucleocapsid viral proteins, and 3 are surface glycoproteins G (attachment), F (fusion), and SH (small hydrophobic) [33]. The glycoproteins F and G are highly accessible to neutralizing antibodies, resulting in numerous changes in response to the host immune pressure [34] and therefore are the most studied.
The NS1 (molecular weight PM, 15.5 kDa) and NS2 (PM, 27 kDa) proteins have, respectively, 139 and 124 amino acids , and the genes that encode these have 532 and 503 nucleotides, respectively. Their functions are not well understood, but it is presumed that they are related to the structural regulation of RNA synthesis, the morphogenesis of the virion, or the interaction with the host cells [33].
The proteins P, L, and N are associated with genomic RNA and nucleocapsid, forming the ribonucleoprotein complex, considered as the minimum unit necessary for transcription and replication of the virus. The P protein is highly phosphorylated and acidic and has a key role in the regulation of the transcription and replication process. It has 241 amino acids and a molecular weight of 35 kDa, and the gene that encodes it has 914 nucleotides. The nucleoprotein N has 391 amino acids and a molecular weight of 43.4 kDa, and the gene that encodes it has 1203 nucleotides and is the main structural protein of the nucleocapsid, closely associated with the genomic RNA. The L protein, consisting of 2165 amino acids with a molecular weight of 250 kDa, is the largest viral protein. The gene that encodes the L protein has 6578 nucleotides [33].
The M proteins (PM, 27 kDa) and M2-1 (PM, 22 kDa) are internal and not glycosylated, possessing, respectively, 194 and 256 amino acids, and the genes that encode them have 958 and 961 nucleotides, respectively. The M protein mediates the association of nucleocapsid with the viral envelope [33], and the M2-1 acts on the elongation during transcription [32].
The SH protein is a small molecule (amino acids and 64 PM, 7.5 kDa), which is inserted in the cytoplasmic membrane of the host cell via a hydrophobic sequence, ranging from 14 to 41 amino acids. The function of this protein has not yet been clarified ; however, because it is integrated in the membrane, it is assumed to be involved in adsorption, penetration, and denudation of the virus [33].
The glycoprotein F has 574 amino acids with a molecular weight of 70 kDa, and the gene that encodes it has 1903 nucleotides. Identified as a fusion protein, it is responsible for the attachment of the viral envelope with the plasma membrane of the host cell, releasing nucleocapsid directly within the cytoplasm. Also, it is responsible for the fusion of the cell infected with neighbor cells, favoring the formation of the syncytium [33].
The F protein is synthesized as an inactive precursor called F0, which consists of two domains, F2 (1–130 amino acids) and F1 (137–574 amino acids), and also has a cleaved peptide (131–136 amino acids). The F1 subunit is anchored to the membrane. The F1 subunit is relatively well preserved and is greatly affected in its function by deletions or substitutions of amino acids [33].
The glycoprotein G is a type II protein, which is anchored to the membrane next to its amino-terminal portion by a hydrophobic domain, non-cleaved, signal anchor type, that extends from residues 38 to 66 [73]. The G protein is 289 to 342 amino acids in length, depending on the viral strain. The G gene is composed of 918 to 1062 (group A) or 921 to 981 (group B) nucleotides [43, 102, 108].
The glycoprotein G is the viral attachment engaged in the adsorption of virus, and it has been shown that antibodies against the G glycoprotein inhibited the binding of virus to the cells [72]. The glycoprotein G is of special interest for showing the largest variability between the viral isolates [4, 52, 67] and can support large deletions or multiple amino acid substitutions without loss of function [43, 102]. This variability among strains of HRSV is a signature feature that can alter the pathogenicity and adaptation of the virus and contribute to the ability of the virus to cause repeated infections and outbreaks by escaping the immune system. The glycoproteins F and G are the most important proteins involved in a protective immune response [8, 66], and antibodies against them show strong neutralization activity in vitro [2, 123].
7 Replication
The cell receptor specific for the glycoprotein G was first identified by Krusat and Streckert [70], who showed that preincubation of the virus with heparin inhibited the infection in cell culture and that the G protein binds heparin. These results suggest that heparin or other glycosaminoglycans (GAGs) similar to heparin, present on the cell surface, are involved in the binding of the virus to the cell. The binding site of the glycoprotein G to the heparin (or another GAG) was mapped between the 184 and 198 amino acids of the protein G for group A and among the 183 to 197 amino acids for group B. Martinez et al. [77] confirmed that the presence of these receptors is critical for the binding of the virus.
The virus enters into the cell through fusion with the cell membrane. After penetration, the viral envelope remains as part of the cell membrane. The nucleocapsid is released into the cytoplasm and begins the process of transcription of the viral genome by the viral polymerase. The genes are transcribed in sense 3′ → 5′ with a sign promoting to the 3′-side [33]. The peak of the synthesis of mRNAs occurs 16 h after infection, and the peak of proteins occurs at 18–20 h [6, 33]. In addition to the transcription and translation of proteins, another important step is the replication of the viral genome, which produces an intermediate positive (+ ssRNA), which will serve as a template to generate more copies of the viral genome (ssRNA). All the replication process takes place in the cytoplasm [33].
The maturation of the virus occurs in the first instance, with the combination of proteins N and P to the genomic RNA and subsequent addition of other auxiliary proteins to the nucleocapsid. The surface glycoproteins are inserted into the cytoplasmic membrane of the host cell . In the next step the matrix protein interacts by noncovalent forces to the cytoplasmic tails of the surface glycoprotein. The assembled internal structures of the virus interact with this surface and drive the budding, with the release of the virus, when the virus acquires the lipoprotein envelope [69].
8 Genetic Variability
The variability of the G protein is concentrated in the extracellular domain, where two variable regions have a high content of serine and threonine, between 69 to 164 and 207 to 298 amino acids , with approximately 56% divergence between groups A and B [66, 67]. Interspersing this region of high variability, there is a conserved region with a small segment of 13 amino acids (164–176) and four cysteine residues (C173, C176, C182, C186), which are well preserved in all samples of HRSV [97, 118], suggesting that this region is responsible for binding the virus to a cell receptor. However, data about the region for genotypes that emerged after 2010 are currently lacking.
The genotyping of HRSV-A and HRSV-B is based on the variability of the G-protein gene. For HRSV A, 11 genotypes were reported and designated as GA1, GA2, GA3, GA4, GA5, GA6, and GA7 [92, 93], SAA1 (South Africa, A1) [115], and more recently, NA1, NA2, NA3, and NA4 [102]. For HRSV-B, 17 genotypes have been described and designated as GB1, GB2, GB3, and GB4 [93], SAB1, SAB3 [115], BA1–BA6 (Argentina) [109], BA7–BA10 (Japan) [38], and B11 (Korea) [7]. Interestingly, strains belonging to genotype BA of HRSV-B exhibited duplication of 60 nucleotides (nt) in the second variable region protein gene G, but were not associated with more severe clinical manifestations [38, 108]. In Brazil, the only genotypes circulating currently from HRSV-A are NA2, NA3, and ON1 and BA genotyping from HRSV-B.
In 2012, Eshaghi et al. [43] detected in group A one repetition of 72 nucleotides (GTCAAGAGGAAACCCTCCACTCAACCACCTCCGAAG GCTATCTAAGCCCATCACAAGTCTATACAACATCCG) in the C-terminal portion of the gene (G), being the largest duplication described in this group. This new genotype was called ON1 and was found in 10% of HRSV isolates. In 2013 this ON1 genotype was found in 75% of all isolates in Brazil [42, 80], and in 2015 the ON1 genotype had attained natural dominance and become the predominant genotype circulating in different areas of the world [107]. This area is specifically targeted for neutralizing antibodies, and these types of changes of structure can lead to changes in immunogenicity and pathogenicity of the virus. However, additional studies are still required to explore the pathogenicity, transmissibility, and replication of this new variant .
9 Epidemiology
In the 1990s several studies of molecular epidemiology were conducted based on partial sequences of genes G and SH and a restriction map of the N gene, enabling reaching some important conclusions about HRSV circulation:
-
1.
The existence of several genotypes circulating concurrently in a single outbreak, with a predominance of one or two genotypes which tend to decrease in subsequent outbreaks until its disappearance [17, 19, 20, 27, 28, 30, 65, 75, 92, 93].
-
2.
The genotypes of HRSV have worldwide distribution, and strains isolated in distinct communities and in different years may be more related to strains isolated in the same locality in two consecutive days, demonstrating a pattern of temporal and not necessarily geographic circulation [18, 50].
-
3.
Within each strain (genotype) occurs a progressive buildup of amino acid changes [21].
-
4.
Antigenic changes detected with a panel of anti-G monoclonal antibodies can be correlated with the position of the viruses in the phylogenetic trees [50].
-
5.
The synonymous nucleotide substitutions have a uniform distribution over the G gene, and non-synonymous substitutions are accumulated in the two variable regions of the gene G [21, 50].
However, there are studies in which a minimal temporal variation in the gene encoding the G protein has been reported. A study performed in Cuba revealed the movement of extremely homogeneous samples during the 1994–1995 outbreaks, with a difference of just five nucleotides when compared to the sample long since isolated in 1956 [113].
The significance of the antigenic variation of HRSV groups in epidemiology is not yet clear. The antigenic dimorphism, although at modest rates, seems to contribute to the high incidence of reinfections during the first years of life. However, several reinfections in children involving viruses of the same group have been reported [60, 83]. In addition, there is no indication that reinfection with a heterologous group induces more serious clinical signs than reinfection with homologous samples [110].
The two groups (A and B) have been circulating concurrently in many epidemics for more than 20 years [12, 65], in diverse regions of the world, and with incidences that vary from year to year. Studies conducted in El Salvador, Santa Fe, and Buenos Aires in Argentina revealed the presence of both groups during outbreaks with prevalence of group A [23, 63, 121].
In some localities , such as Rochester and Boston in the U.S., Sapporo in Japan, and Rio de Janeiro, Porto Alegre, and Ribeirão Preto in Brazil, in addition to the co-circulation of the groups, the prevalence of groups A and B may switch over the years or show a balance of the frequencies of both groups [29, 56, 58, 104, 112].
Differences in pathogenicity between the two groups are not clear. Hall et al. [56] and Imaz et al. [63] verified increased severity in children infected with group A, although Zelaya et al. [121] found greater severity in children infected with group B. Other authors did not observe significant differences in pathogenicity between the groups [29, 104].
In a study carried out in Bogota, Colombia, a total of 13,488 samples of children hospitalized with a diagnosis of respiratory infection were tested for RSV during 5 years and 4,559 (33.8%) were found positive. The average age of patients analyzed in the study was 9.2 ± 8.5 months, and 71.7% of cases of HRSV infection occurred in the period from March to May, whereas 50% of the bronchiolitis cases were diagnosed from April to June during the years of the study [47].
In Chile, HRSV are detected as a single pathogen at 74/124 (58.7%) samples of nasopharyngeal aspirate of patients, and 28/124 (22.6%) samples were co-detected with HRV. Hospitalization was necessary in 77% of positive cases of HRSV (57/74), and 44.6% of these cases were considered serious; 53.6% (15/28) of cases coinfected by both viruses were hospitalized, too, but this coinfection does not increase the severity of illness [74].
In Brazil, many studies have already been carried out to investigate the etiology of acute respiratory diseases [12]. During the period of 2003–2009, nasopharyngeal aspirates were examined in more than 2000 children less than 5 years old, and HRSV were found in at least 42% of positivity between respiratory viruses identified in children hospitalized with acute respiratory disease [85, 105].
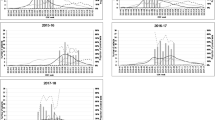
In countries in southern Latin America such as Argentina and Uruguay, outbreaks of HRSV occur predominantly during the winter months [22, 61]. In tropical and subtropical climates , the outbreaks are not always well defined, although in Ceara, located in the northeast of Brazil, HRSV caused yearly seasonal epidemics, generally from February until July (Moura et al. 2013). In Brazil, in the cities of Rio de Janeiro and São Paulo, HRSV outbreaks start in autumn (ranging from March to April) and extend until winter (July–August), with peak incidence occurring usually in May (Table 12.1) [85, 105].
Fortunately, fatalities from infection by HRSV are uncommon, and estimates indicate that the number of deaths is around 200–500 a year, 80% of which are of children under 1 year of age. However, mortality may increase significantly in children who present some background that predisposes to more serious diseases, such as congenital heart diseases and lung diseases , and premature infants, in which mortality by HRSV infection is around 10%, 5.5%, and 4.6%, respectively [41, 100]. High mortality rates may also be observed in individuals with immunodeficiency, congenital or induced by chemotherapy against cancer [54] or from organ transplants, especially in the first 20 days after the transplant [94]. Among bone marrow transplant recipients, the mortality of those who become infected with HRSV can reach 45% [14, 57].
A study conducted in the U.S. revealed the occurrence of 14,000 to 62,000 annual hospitalizations of the elderly with pneumonia associated with HRSV, at a cost of approximately 150,000,000–680,000,000 dollars to the health system and causing about 1,500–6,700 deaths per year (5–20 deaths/100,000) [124].
10 Laboratory Diagnosis
The laboratory diagnosis of HRSV can be carried out by the direct detection of viruses, viral antigens, or the viral genome or, indirectly, based on the detection of specific antibodies. For the routine clinical laboratory diagnosis using respiratory secretions as biological samples, the procedures may include viral isolation in cell culture, antigen detection by immunofluorescence or enzyme-linked immunosorbent assay, and viral RNA detection by reverse transcriptase (RT)-polymerase chain reaction (PCR). The best samples are those obtained by aspiration or washing nasopharyngeal secretions [76, 79]. The viral particle present in the secretions is highly labile, and the samples should be kept refrigerated during transportation to the laboratory and processing before inoculation in cell cultures .
The isolation in cell culture , regarded as the gold standard, can be carried out in a wide variety of human and animal cell lines, but HEp-2 and HeLa cells are the most used [110; Perini et al. 2007]. The cytopathic effect usually appears within 3–7 days after inoculation and is characterized by the presence of large syncytia resulting from cell fusion (Fig. 12.4). Nevertheless, as viral isolation in cell culture is difficult, the diagnosis of infection is most often accomplished by detection of HRSV antigens in nasopharyngeal epithelial cells by immunofluorescence (Fig. 12.5) or enzyme-linked immunosorbent assay, faster methods that do not require the presence of infectious viral particles. These last two methods require the adequate preparation of the specimens by removing excess mucus. Finally, success of the immunofluorescence technique, aside from well-trained personnel and well-prepared samples, requires a minimum number of infected cells to enable a correct diagnosis [110].
Hughes et al. [62] compared the three diagnostic techniques for HRSV: isolation in cell culture , direct and indirect immunofluorescence (IFA), and enzyme-linked immunosorbent assay (ELISA) . Both immunofluorescence-based methods detected more positive samples (showed higher sensitivity) than viral isolation. However, 15% of the samples found positive by viral isolation were negative by immunofluorescence, demonstrating the need for the use of at least two diagnostic methods.
The RT-PCR technique has been used both for the diagnosis [51, 59, 117] and for typing a sample to group A or B [53, 122]. It is considered a highly sensitive technique, especially useful in the diagnosis of infections, in which both the sample amount and the viral load in the sample are small, as is the case of samples taken from the elderly [117]. In the past decade, the molecular methods were considered as a gold standard, because of their specificity and ability of simultaneous detection of different viruses [90]. The advances in real time-RT-PCR (quantitative (q)RT-PCR) specificity and sensitivity for the detection of HRSV in clinical samples became more suitable for diagnosis in clinical laboratories [46].
The rapid antigen detection tests (RADTs) are dipstick-based immunoassays that allow for the rapid, qualitative detection of RSV antigen (viral fusion protein) directly from nasopharyngeal swab, nasopharyngeal aspirate, or nasal/nasopharyngeal wash specimens from symptomatic pediatric patients. The RADTs provide a result in 15 min, compared to approximately 90 min for a conventional IFA test and 2–3 h for ELISA [80]. Rapid tests may also be used as a point-of-care assay. These methods, although effective, may present several drawbacks, including price and skilled personnel. All these issues pose a challenge to hospitals and pediatric clinics to apply the best medical management for monitoring or treatment of children with suspected infection.
Serological diagnoses can be made through neutralization assays, complement fixation, or determination of class-specific immunoglobulins (IgG, IgM) by ELISA or immunofluorescence techniques. The diagnosis is based on the increase in antibody titer between acute and convalescent titers, performed in serum or saliva [110, 120]. The serology offers limited value in the diagnosis of primary infection in children less than 6 months of age because 40% of these cases present no increase in antibody titer. However, in infants and adults, the serology is regarded as a good indicator of reinfections [55]. The serology, therefore, is not the most appropriate method for diagnosis of infection by HRSV, having, however, great importance in clinical and epidemiological studies [36].
11 Treatment and Prevention
Ribavirin (1-β-d-ribofuranosyl-1,2,4-triazole-3-carboxamide), a nucleoside analogue of the guanosine, licensed since 1986, is the treatment of choice for RSV. Its use is indicated in the form of aerosol for the treatment of serious diseases caused by HRSV. Although several studies have demonstrated the effectiveness of ribavirin in inhibiting replication of the virus and the improvement of clinical conditions, resulting in a decrease in the need for supplemental oxygen and mechanical ventilation in children with lower respiratory tract infection, chronic lung disease, and infection in immunocompromised individuals, lately there has been controversy about the benefits of its use. Since 1989, several studies have appeared indicating that the use of ribavirin has minimal effect on disease outcome caused by HRSV, not showing evidence of decreased duration of hospitalization or the need of supporting therapy, in addition to the high cost and extended treatment (12 h or more of inhalation) [13, 37].
Several drug candidates have been studied in the past decades, including several inhibitors, targeting different HRSV proteins. Despite these efforts, until the present time there has been no antiviral drug approved for treatment (Heylen et al. 2017).
Development of an RSV vaccine has been hampered by the incidence of enhanced respiratory disease (ERD) following vaccination with formalin-inactivated RSV in the 1960s. Since its failure, multiple live virus vaccines have been developed, as well as other vaccine platforms, including virus-like particles, peptide-based vaccines, protein subunit vaccines, and plasmid DNA-based vaccines. Many of these vaccines have been evaluated in animals, and a few have been studied in humans. None, however, has shown sufficient promise to move toward licensure. It is clear that a better understanding of virus and host factors that contribute to both disease and protective immunity is still necessary to develop safe and effective RSV vaccines.
Alternative approaches to identify vaccine-relevant epitopes include the identification of neutralizing RSV protein epitopes to which a protective immune response can be safely generated and the development of modern pre- and post-RSV fusion (F) protein subunits. One obstacle to developing an RSV vaccine has been the difficulty in inducing long-term protective immunity, as evidenced by the repeated infections throughout life and the incomplete protection afforded to recipients of immune prophylaxis. In addition, an immunogenic approach targeted to a single neutralizing epitope mapped to the site A region may generate a focused immune response against RSV F, but in general, the polyclonal response generated by site A-based vaccines has been characterized by poor binding to intact RSV F protein, modest in vitro neutralization, and no evidence of protection to RSV challenges in vivo.
Palivizumab (Pz) (Synagis; MedImmune) is a humanized IgG monoclonal antibody that neutralizes HRSV through interaction with the HRSV F glycoprotein. Pz is the only FDA-approved prophylaxis against HRSV infection [5, 101]. Five monthly Pz injections spanning the annual HRSV epidemic period have been shown to reduce hospitalizations among high-risk children in the U.S. However, the quasi-species nature of RNA viruses allows rapid emergence of escape mutants to the immune pressure . The increasing use of Pz in high-risk children and immunocompromised patients provides opportunities for Pz-resistant mutants to arise and persist among humans [1, 9, 86, 88, 123]. However, little is known of these mutations in patients who did not use Pz.
References
Adams O, Bonzel L, Kovacevic A, Mayatepek E, Hoehn T, Vogel M (2010) Palivizumab-resistant human respiratory syncytial virus infection in infancy. Clin Infect Dis 51(2):185–188
Anderson LJ, Bingham P, Hierholzer JC (1988) Neutralization of respiratory syncytial virus by individual and mixtures of F and G protein monoclonal antibodies. J Virol 62(11):4232–4238
Anderson LJ, Parker RA, Strikas RL (1990) Association between respiratory syncytial virus outbreaks and lower respiratory tract deaths of infants and young children. J Infect Dis 161(4):640–646
Anderson LJ, Hierholzer JC, Tsou C, Hendry RM, Fernie BF, Stone Y, Mcintosh K (1985) Antigenic characterization of respiratory syncytial virus strains with monoclonal antibodies. J Infect Dis 151:626–633
Anon (1998) Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk in infants. Pediatrics 102:531–537
Arslanagic E, Matsumoto M, Suzuki K, Nerome K, Tsutsumi H, Hung T (1996) Maturation of respiratory syncytial virus within HEp-2 cell cytoplasm. Acta Virol 40(4):209–214
Baek YH, Choi EH, Song MS, Pascua PN, Kwon HI, Park SJ, Lee JH, Woo SI, Ahn BH, Han HS, Hahn YS, Shin KS, Jang HL, Kim SY, Choi YK (2012) Prevalence and genetic characterization of respiratory syncytial virus (RSV) in hospitalized children in Korea. Arch Virol 157(6):1039–1050
Beeler JA, Coelingh van Wyke K (1989) Neutralization epitopes of the F glycoprotein of respiratory syncytial virus: effect of mutation upon fusion function. J Virol 63:2941–2950
Boivin G, Caouette G, Frenette L, Carbonneau J, Ouakki M, Serres G (2008) Human respiratory syncytial virus and other viral infections in infants receiving palivizumab. J Clin Virol 42(1):52–57
Boivin G, De Serres G, Côte S, Gilca R, Abed Y, Rochette L, Bergeron MG, Dery EP (2003) Human metapneumovírus infection in hospitalized children. Emerg Infect Dis 9(6):634–640
Bonfim CM, Nogueira ML, Simas PV, Gardinassi LG, Durigon EL, Rahal P, Souza FP (2011) Frequent respiratory pathogens of respiratory tract infections in children attending daycare centers. J Pediatr (Rio) 87(5):439–444
Botosso VF, Zanotto PM, Ueda M, Arruda E, Gilio AE, Vieira SE, Stewien KE, Peret TC, Jamal LF, Pardini MI, Pinho JR, Massad E, Sant'anna OA, Holmes EC, Durigon EL, VGDN Consortium (2009) Positive selection results in frequent reversible amino acid replacements in the G protein gene of human respiratory syncytial virus. PLoS Pathog 5(1):e1000254
Bricks LF (2000) Prevention of respiratory syncytial virus infections. Rev Hosp Clin Fac Med SP 56:79–90
Bryce J, Boschi-Pinto C, Shibuya K, Black RE (2005) Who estimates the causes of death in children. Lancet 365(23):1147–1152
Bueno IA, Riccetto AG, Morcillo AM, Arns CW, Baracat EC (2012) Respiratory syncytial vírus, infants and intensive therapy. Braz J Infect Dis 16(1):86–89
Cane PA (2001) Molecular epidemiology of respiratory syncytial virus. Rev Med Virol 11:103–116
Cane PA, Matheus DA, Pringle CR (1991) Identification of variable domains of the attachment (G) protein of subgroup A respiratory syncytial virus. J Gen Virol 72:2091–2096
Cane PA, Matthews DA, Pringle CR (1992) Analysis of relatedness of subgroup A respiratory syncytial viruses isolated worldwide. Virus Res 25:15–22
Cane PA, Matthews DA, Pringle CR (1994) Analysis of respiratory syncytial virus strain variation in successive epidemics in one city. J Clin Microbiol 32:1–4
Cane PA, Pringle CR (1991) Respiratory syncytial virus heterogeneity during an epidemic: analysis by limited nucleotide sequencing (SH gene) and restriction mapping (N gene). J Gen Virol 72:349–357
Cane PA, Prince CR (1995) Evolution of subgroup a respiratory syncytial virus: Evidence for progressive accumulation of amino acid changes in the attachment protein. J Virol 69:2918–2925
Carballal G, Videla CM, Espino MA, Savy V, Uez O, Sequeira MD, Knez V, Requeijo PV, Posse CR, Miceli I (2001) Multicentered study of viral acute lower respiratory infections in children from four cities of Argentina, 1993–1994. J Med Virol 64:164–174
Carballal G, Videla CM, Sequeira MD, Mistchenko A, Requeijo PV, Arbiza J (2000) Respiratory syncytial virus: changes in prevalence of subgroups A and B among Argentinian children, 1990–1996. J Med Virol 61:275–279
CDC-Centers for Disease Control and Prevention (2014) Respiratory syncytial virus circulation in the United States, July 2012–June 2014. MMWR 62:141–144
Chanock RM, Roizman B, Myers R (1957) Recovery from infants with respiratory illness of virus related to chimpanzee coryza agent. I. isolation, properties and characterization. Am J Hyg 66:281–290
Chanock RM, Finberg L (1957) Recovery from infants with respiratory illness of a virus related to chimpanzee coryza agent (CCA). II. Epidemiological aspects of infection in infants and young children. Am J Hyg 66:291–300
Choi E, Lee H (2000) Genetic diversity and molecular epidemiology of the G protein of subgroups A and B of respiratory syncytial virus isolated over 9 consecutive epidemics in Korea. J Infect Dis 181:1547–1556
Christensen LS, Larsen LB, Johansen J, Andersen EA, Wejse C, Klug B, Hornsleth A (1999) The fluctuating pattern of various genome types of respiratory syncytial virus in copenhagen and some other locations in Denmark. APMIS 107:843–850
Cintra OA, Owa MA, Machado AA, Cervi MC, Figueiredo LT, Rocha GM et al (2001) Occurrence and severity of infections caused by subgroup A and B respiratory syncytial virus in children in southeast Brazil. J Med Virol 65(2):408–412
Wb C, Ej L, Wm S (1998) Genetic variability among group A and group B respiratory syncytial virus in a children’s hospital. J Clin Microbiol 36:35552–35557
Collins PL, Dickens LE, Buckler-White A, Olmsted RA, Spriggs MK, Camargo E et al (1986) Nucleotide sequences for the gene junctions of human respiratory syncytial virus reveal distinctive features of intergenic structure and gene order. Proc Natl Acad Sci U S A 83(13):4594–4598
Collins PL, Hill MG, Camargo E, Grosfeld H, Chanock RM, Murphy BR (1995) Production of infectious human respiratory syncytial virus from cloned cDNA confirms an essential role for the transcription elongation factor from the 5′ proximal open reading frame of the M2 mRNA in gene expression and provides a capability for vaccine development. Proc Natl Acad Sci U S A 92(25):11563–11567
Collins PL, McIntosh K, Chanock RM (1996) Respiratory syncytial virus. In: Fields BN, Knipe DM, Howley PM (eds) Fields virology, 3rd edn. Lippincott-Raven, Philadelphia, pp 1313–1351
Collins PL, Chanock RM, Murphy FBR (2001) Respiratory syncytial vírus. In: Fields BN (ed) Fields virology, 4th edn. Lippincott-Raven, Philadelphia/New York
Costa LF, Yokosawa J, Mantese OC, Oliveira TF, Silveira HL, Nepomuceno LL, Moreira LS, Dyonisio G, Rossi LM, Oliveira RC, Ribeiro LZ, Queiróz DA (2006) Respiratory vírus in children younger than five years old with acute respiratory disease from 2001 to 2004 in Uberlândia, MG, Brazil. Mem Inst Oswaldo Cruz 101(3):301–306
Cox MJ, Azevedo RS, Cane PA, Massad E, Medley GF (1998) Seroepidemiological study of respiratory syncytial virus in São Paulo state, Brazil. Med Virol 55:234–239
Crowe JE (2002) Respiratory syncytial virus vaccine development. Vaccine 20:S32–S37
Dapat IC, Shobugawa Y, Sano Y, Saito R, Sasaki A, Suzuki Y, Kumaki A, Zaraket H, Dapat C, Oguma T, Yamaguchi M, Suzuki H (2010) New genotypes within respiratory syncytial virus group B, genotype BA in Niigata, Japan. J Clin Microbiol 48(9):3423–3427
Debur MC, Vidal LR, Stroparo E, Nogueira MB, Almeida SM, Takahashi GA, Rotta I, Pereira LA, Silveira CS, Delfraro A, Nakatani SM, Skraba I, Raboni SM (2010 Dec) Impact of human metapneumovirus infection on in and outpatients for the years 2006-2008 in Southern Brazil. Mem Inst Oswaldo Cruz 105(8):1010–1018
Durigon GS, Oliveira DB, Vollet SB, Storni JG, Felício MC, Finelli C, Piera J, Magalhães M, Caldeira RN, Barbosa ML, Durigon EL, Berezin EN (2010) Hospital-acquired human bocavirus in infants. J Hosp Infect 76(2):171–173
Durigon GS, Oliveira DB, Felicio MC, Finelli C, Pereira MF, Storni JG et al (2015) Poor outcome of acute respiratory infection in young children with underlying health condition in Brazil. Int J Infect Dis 34:3–7
Colmanetti TC, Oliveira DBL, Botosso VF, Thomazelli LM, Pinez CMN, Crema D, Mesquita FS, Vieira SE, Gilio AE, Martinez MB, Durigon EL (2015) Naturally dominance of RSV, a N276S mutation in protein palivizumab binding site in new genotypes oni-1 and na1-2-3. Presented at Clinical Virological Symposium.2015
Eshaghi A, Duvvuri VR, Lai R, Nadarajah JT, Li A, Patel SN, Low DE, Gubbay JB (2012) Genetic variability of human respiratory syncytial virus A strains circulating in Ontario: a novel genotype with a 72 nucleotide G gene duplication. PLoS One 7(3):e32807
Falsey AR (2005) Respiratory syncytial virus infection in elderly and high-risk adults. Exp Lung Res 31(1):77
Forster J, Ihorst G, Rieger CH, Stephan V, Frank HD, Gurth H, Berner R, Rohwedder A, Werchau H, Schumacher M, Tsai T, Petersen G (2004) Prospective population-based study of viral lower respiratory tract infection in children under 3 years of age. Eur J Pediatr 163:709–716
Fry AM, Chittaganpitch M, Baggett HC, Peret TC, Dare RK, Sawatwong P et al (2010) The burden of hospitalized lower respiratory tract infection due to respiratory syncytial virus in rural Thailand. PLoS One 5(11):e15098
Gamba-Sanchez N, Rodriguez-Martinez CE, Sossa-Briceno MP (2016) Epidemic activity of respiratory syncytial virus is related to temperature and rainfall in equatorial tropical countries. Epidemiol Infect 144(10):2057–2063
Garcia CG, Bhore R, Soriano-Fallas A, Trost M, Chanson R, Ramilo O, Mejias A (2010) A Risk factors in children hospitalized with RSV bronchiolitis versus non-RSV bronchiolitis. Pediatrics 126(6):e1453–e1460
Garcia MLG, Gabin MO, Rey CC, Alvarez MIG, Ruiz JA, Sierra AA, Breña PP (2001) Infecciones virales de vias respiratórias inferiors en lactentes hospitalizados: etiología, características clínicas y factores de riesgo. An Esp Pediatr 55:101–107
Garcia O, Martin M, Dopazo J, Arbiza J, Frabasile S, Russsi J, Hortal M, Perez-Brena P, Martinez I, Garcia-Barreno B, Melero JA (1994) Evolutionary pattern of human respiratory syncytial virus (subgroup A): cocirculating lineages and correlation of genetic and antigenic changes in the G glicoprotein. J Virol 68:5448–5459
Gilbert LL, Dakhama A, Bone BM, Thomas EE, Hegele RG (1996) Diagnosis of viral respiratory tract infections in children by using a reverse transcription-PCR panel. J Clin Microbiol 34:140–143
Gimenez HB, Hardman N, Keir HM, Cash P (1986) Antigenic variation between human respiratory syncytial virus isolates. J Gen Virol 67(pt 5):863–870
Gottschalk J, Zbinden R, Kaempf L, Heinzer I (1996) Discrimination of respiratory syncytial virus subgroups A and B by reverse transcription-PCR. J Clin Microbiol 34:41–43
Hall CB, Keith RP, Macdonald NE, Gala CL, Menegus ME, Suffin SC, Cohen HJ (1986) Respiratory syncytial viral infection in children with compromised immune function. N Engl J Med 315:77–81
Hall CB, Walsh EE, Long CE, Schnabel KC (1991) Immunity to and frequency of reinfection with respiratory syncytial virus. J Infect Dis 163:693–698
Hall CB, Walsh EE, Schnabel KC, Long CE, Mcconnochie KM, Hildreth SW, Anderson LJ (1990) Occurrence of groups A and B of respiratory syncytial virus over 15 years: associated epidemiologic and clinical characteristics in hospitalized and ambulatory children. J Infect Dis 162:1283–1290
Harrington RD, Hackman EC, Storch GA, Osborne B, Gleaves CA, Benson A, Meyers JD (1992) An outbreak of respiratory syncytial virus in a bone marrow transplant center. J Infect Dis 153:291–297
Hendry RM, Pierik LT, Mcintosh K (1989) Prevalence of respiratory syncytial virus subgroups over six consecutive outbreaks: 1981–1987. J Infect Dis. 160:185–190
Henkel JH, Aberle SW, Kundi M, Popow-Kraupp T (1997) Improved detection of respiratory syncytial virus in nasal aspirates by seminested RT-PCR. J Med Virol 53:366–371
Hierholzer JC, Tannock GA, Hierholzer CM, Coombs RA, Kennett ML, Phillips PA, Gust ID (1994) Subgrouping of respiratory syncytial virus strains from Australia and Papua New Guinea by biological and antigenic characteristics. Arch Virol 136:133–147
Hortal M, Suarez A, Deleon C, Estevan M, Mogdasy MC, Russi JC, Contera M, Meny M (1994) Etiology and severity of community acquired pneumonia in children from Uruguay: a 4-year study. Rev Inst Med Trop São Paulo 36:255–264
Hughes JH, Mann DR, Hamparian VV (1988) Detection of virus respiratory syncytial virus in clinical specimens by viral culture, direct and indirect immunofluorescence, and enzyme immunoassay. J Clin Microbiol 26:588–591
Imaz MS, Sequeira MD, Videla C, Veronessi I, Cociglio R, Zerbini E, Carballal G (2000) Clinical and epidemiological characteristics of respiratory syncytial virus subgroups A and B infections in Santa Fe, Argentina. J Med Virol 61:76–80
Iwane MK, et al., New Vaccine Surveillance Network (2004) Population-based surveillance for hospitalizations associated with respiratory syncytial vírus, influenza vírus e parainfluenza víruses among young children. Pediatrics 113:1758–1764
Johansen J, Christensens LS, Hornsleth A, Klug B, Hansn KS, Nir M (1997) Restriction pattern variability of respiratory syncytial virus during three consecutive epidemics in Denmark. APMIS 105:303–308
Johnson PR Jr, Olmsted RA, Prince GA, Murphy BR, Alling DW, Walsh EE, Collins PL (1987) Antigenic relatedness between glycoproteins of human respiratory syncytial virus subgroups A and B: evaluation of the contributions of F and G glycoproteins to immunity. J Virol 61:3163–3166
Johnson PR, Spriggs MK, Olmsted RA, Collins PL (1987) The G glycoprotein of human respiratory syncytial viruses of subgroups A and B: extensive sequence divergence between antigenically related proteins. Proc Natl Acad Sci U S A 84(16):5625–5629
Kfouri RA, Wagner NH (2011) Infecção pelo virus Sincicial Respiratório. In: Neto VA (ed) Imunizações: atualizações, orientações e segestões. Segmento Farma, São Paulo
Kingsbury DW (1990) Paramyxoviridae and their replication. In: Fields BN (ed) Fields virology. Lippincott-Raven, Philadelphia, pp 945–962
Krusat T, Streckert HJ (1997) Heparin-dependent attachment of respiratory syncytial virus (RSV) to host cells. Arch Virol 142(6):1247–1254
Kuo L, Fearns R, Collins PL (1996) The structurally diverse intergenic regions of respiratory syncytial virus do not modulate sequential transcription by a dicistronic minigenome. J Virol 70(9):6143–6150
Levine SR, Klaiber-Franco R, Paradiso PR (1987) Demonstration that glycoprotein G is the attachment protein of respiratory syncytial virus. J Gen Virol 68:2521–2524
Lichtenstein DL, Roberts SR, Wertz GW, Ball LA (1996) Definition and functional analysis of the signal/anchor domain of the human respiratory syncytial virus glycoprotein. J Gen Virol 77(pt 1):109–118
Luchsinger V, Ampuero S, Palomino MA, Chnaiderman J, Levican J, Gaggero A, Larrañaga CE (2014) Comparison of virological profiles of respiratory syncytial virus and rhinovirus in acute lower tract respiratory infections in very young Chilean infants, according to their clinical outcome. J Clin Virol 61(1):138–144
Lukic-Grlic A, Cane PA, Bace A, Pringle CR, Mlinaric-Galinovic G, Popow-Kraupp T (1998) Antigenic and genomic diversity of central European respiratory syncytial virus strains. Arch Virol 143(7):1441–1447
Mackie PLK, Madge PJ, Getty S, Paton JY (1991) Rapid diagnosis of respiratory syncytial virus by using pernasal swabs. J Clin Microbiol 29:2653–2655
Martinez I, Valdes O, Delfraro A, Arbiza J, Russi J, Melero JA (1999) Evolutionary pattern of the G glycoprotein of human respiratory syncytial virus from antigenic group B: the use of alternative codons and lineage diversification. J Gen Virol 80:125–130
Massin MM, Montesanti J, Gerard P, Lepage (2006) Spectrum and frequency of illness presenting to a pediatric emergency department. Acta Clin Belg 61:161–165
Masters HB, Weber KO, Groothuis JR, Wren CG, Lauer BA (1987) Comparison of nasopharyngeal washing and swab specimens for diagnosis of respiratory syncytial virus by EIA, FAT, and cell culture. Diagn Microbiol Infect Dis 8:101–105
Mesquita FS, Oliveira DBL, Crema D, Botosso VF, Pinez CMN, Colmanetti TC, Thomazelli, LM, Gilio AE, Martinez MB, Durigon EL (2017) Rapid antigen detection test for respiratory syncytial virus (RSV) diagnosis as a diagnostic tool for use in pediatrics. J Pediatr (Rio J). 2016 Nov 25. pii: S0021-7557(16)30287-X. doi: 10.1016/j.jped.2016.06.013. [Epub ahead of print]
Mink MA, Stec DS, Collins PL (1991) Nucleotide sequences of the 3′ leader and 5′ trailer regions of human respiratory syncytial virus genomic RNA. Virology 186:615–624
Morris JA Jr, Blount RE, Savage RE (1956) Recovery of cytopathogenic agent from chimpanzees with coryza. Proc Soc Exp Med 92:544–550
Mufson MA, Belshe RB, Örvell C, Norrby E (1987) Subgroups characteristics of respiratory syncytial virus strains recovered from children with two consecutive infections. J Clin Microbiol 25:1535–1539
Nicholson KG, McNally T, Silverman M, Simons P, Stockton JD, Zambon MC (2006) Rates of hospitalisation for influenza, respiratory syncytial vírus and human metapneumovírus among infants and young children. Vaccine 24:102–108
Oliveira DBL, Durigon EL, Carvalho ACL, Leal AL, Souza TS, Thomazelli LM, Moraes CTP, Vieira SE, Al G, Stewien KE (2009) Epidemiology and genetic variability of human metapneumovírus during a 4-year-long study in Southeastern Brazil. J Med Virol 81:915–921
Oliveira DBL, Iwane MK, Prill MM, Weinberg GA, Williams JV, Griffind MR, Szilagyi PG, Edwards KM, Staat MA, Hall CB, Durigon EL, Erdman DD (2015) Molecular characterization of respiratory syncytial viruses infecting children reported to have received palivizumab immunoprophylaxis. J Clin Virol 65:26–31
Olszewska W, Zambon M, Openshaw PJM (2002) Development of vaccines against common colds. Br Med Bull 62:99–111
Papenburg J, Carbonneau J, Hamelin ME, Isabel S, Bouhy X, Ohoumanne N, Déry P, Paes BA, Corbeil J, Bergeron MG, De Serres G, Boivin G (2012) Molecular evolution of respiratory syncytial virus fusion gene Canada, 2006–2010. Emerg Infect Dis 18:120–124
Pavia AT (2011) Viral infections of the lower respiratory tract: old viruses, new viruses, and the role of diagnosis. Clin Infect Dis 52(suppl 4):S284–S289
Pecchini R, Rogério P, Berezin EN, Calahani Felício MC, Passos SD, de Souza MCO et al (2008) Incidence and clinical characteristics of the infection by the respiratory syncytial virus in children admitted in Santa Casa de São Paulo Hospital. Braz J Infect Dis 12(6):476–479
Peng D, Zhao D, Liu J, Wang X, Yang K, Xicheng H et al (2009) Multipathogen infections in hospitalized children with acute respiratory infections. Virol J 6(1):155–161
Peret TC, Hall CB, Hammond GW, Piedra PA, Storch GA, Sullender WM et al (2000) Circulation patterns of group A and B human respiratory syncytial virus genotypes in 5 communities in North America. J Infect Dis. 181(6):1891–1896
Peret TC, Hall CB, Schnabel KC, Golub JA, Anderson LJ (1998) Circulation patterns of genetically distinct group A and B strains of human respiratory syncytial virus in a community. J Gen Virol 79:2221–2229
Pohl C, Green M, Wald ER, Ledesma-Medina J (1992) Respiratory syncytial virus infections in pediatric liver transplant recipients. J Infect Dis 165:166–169
Pontoriero AV, Baumeister EG, Campos AM, Savy VL, Lin YP, Hay A (2003) Antigenic and genomic relation between human influenza víruses that circulated in Argentina in the period 1995–1999 and the corresponding vaccine components. J Clin Virol 28(2):130–140
Robinson JL, Lee BE, Bastien N, Li Y (2005) Seasonality and clinical features of human metapneumovírus infection in children in northern Alberta. J Med Virol 76:98–105
Sanz MC, Kew OM, Anderson LJ (1994) Genetic heterogeneity of the attachment glycoprotein G among group A respiratory syncytial viruses. Virus Res 33(3):203–217
Sauro A, Barone F, Blasio G, Russo L, Santillo L (2006) Do influenza and acute respiratory infective diseases weigh heavily on general practitioners’ daily practice? Eur J Gen Pract 12:34–36
Shao X, Guo X, Esper F, Weibel C, Kahn JS (2007) Seroepidemiology of group I human coronaviruses in children. J Clin Virol 40(3):207–213
Shay D, Holman RC, Roosevelt GE, Clarke MJ, Anderson LJ (2001) Bronchiolitis-associated mortality and estimates of respiratory syncytial virus -associated deaths among US children, 1979–1997. J Infect Dis 183:16–22
Shadman KA, Wald ER (2011) A review of palivizumab and emerging therapies for respiratory syncytial virus. Expert Opin Biol Ther 11:1455–1467
Shobugawa Y, Saito R, Sano Y, Zaraket H, Suzuki Y, Kumaki A, Dapat I, Oguma T, Yamaguchi M, Suzuki H (2009) Emerging genotypes of human respiratory syncytial virus subgroup A among patients in Japan. J Clin Microbiol 47(8):2475–2482
Spencer MJ, Cherry JD (1987) Adenoviral infections. In: Feigin RD, Cherry JD (eds) Textbook of pediatric infectious diseases, 2nd edn. Elsevier, Philadelphia, pp 1688–1708
Straliotto SM, Nestor SM, Siqueira MM (2001) Respiratory syncytial virus groups A and B in Porto Alegre, Brazil, from 1990 to 1995 and 1998. Mem Inst Oswaldo Cruz 96(2):155–158
Thomazelli LM, Vieira SE, Leal AL, Silva TS, Oliveira DB, Golono MA, Gillio AE, Stewien KE, Erdman DD, Durigon EL (2007) Surveillance of eight respiratory víruses in clinical samples of pediatric patients in southeast Brazil. J Pediatr 83(5):422–428
Tregoning JS, Schwarze J (2010) Respiratory viral infections in infants: causes, clinical symptoms, virology, and immunology. Clin Microbiol Rev 23(1):74–98
Trento A, Abrego L, Rodriguez-Fernandes R, Gonzales-Sanches MI, Gonzales-Martines F, Delfraro A, Pascale JM, Arbiza J, Melero JA (2015) Conservation of G protein epitopes in respiratory syncytial virus (group a) despite broad genetic diversity: is antibody selection involved in virus evolution?. J Virol. piiJVI.00467–15
Trento A, Galiano M, Videla C, Carballal G, García-Barreno B, Melero JA, Palomo C (2003) Major changes in the G protein of human respiratory syncytial virus isolates introduced by a duplication of 60 nucleotides. J Gen Virol 84(pt 11):3115–3120
Trento A, Viegas M, Galiano M, Videla C, Carballal G, Mistchenko AS, Melero JA (2006) Natural history of human respiratory syncytial virus inferred from phylogenetic analysis of the attachment (G) glycoprotein with a 60-nucleotide duplication. J Virol 80(2):975–984
Tristram DA, Welliver RC (1996) Respiratory syncytial virus. In: Diagnostic procedure for viral, rickettsial and chlamydial infections, 7th edn. American Public Health Association, Washington, DC
Tsuchiya LRRV, Costa LMD, Raboni SM, Nogueira MB, Pereira LA, Rotta I, Takahashi GRA, Coelho M, Siqueira MM (2005) Viral respiratory infection in Curitiba, Southern Brazil. J Infect 51:401–407
Tsutsumi H, Onuma M, Suga K, Honjo T, Chiba Y, Chiba S, Ogra PL (1988) Occurrence of respiratory syncytial virus subgroup A and B strains in Japan, 1980 to 1987. J Clin Microbiol 26:1171–1174
Valdez O, Martinez I, Valdivia A, Cancio R, Savón C, Goyenechea A, Melero J (1998) Unusual antigenic and genetic characteristics of human respiratory syncytial virus isolated in Cuba. J Virol 72:7589–7592
van den Hoogen BG, van Doornum GJ, Fockens JC, Cornelissen JJ, Beyer WE, de Groot R, Osterhaus AD, Fouchier RA (2003) Prevalence e clinical symptoms of human metapneumovírus infection in hospitalized patients. J Infect Dis 188:1571–1577
Venter M, Madhi SA, Tiemessen CT, Schoub BD (2001) Genetic diversity and molecular epidemiology of respiratory syncytial virus over four consecutive seasons in South Africa: identification of new subgroup A and B genotypes. J Gen Virol. 82(pt 9):2117–2124
Se V, Stewien KE, Queiróz DAO, Durigon EL, Torok TJ, Anderson LJ, Miyao CR, Hein N, Botosso VF, Pahl MM, Gilio AE, Ejzenberg B, Okay Y (2001) Clinical patterns and seasonal trends in respiratory syncytial vírus hospitalizations in São Paulo, Brazil. Rev Inst Med Trop São Paulo 43:125–131
Walsh EE, Falsey AR, Swinburne IA, Formica MA (2001) Reverse transcription polymerase chain reaction (RT–PCR) for diagnosis of respiratory infection in adults: use of single-tube “hanging droplet” nested PCR. J Med Virol 63:259–263
Wertz GW, Collins PL, Huang Y, Gruber C, Levine S, Ball LA (1985) Nucleotide sequence of the G protein gene of human respiratory syncytial virus reveals an unusual type of viral membrane protein. Proc Natl Acad Sci U S A 82(12):4075–4079
Williams BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C (2002) Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis 2:25–32
Wilson SD, Roberts K, Hammond K, Ayres JG, Cane PC (2000) Estimation of incidence of respiratory syncytial virus infection in schoolchildren using salivary antibodies. J Med Virol 61:81–84
Zelaya EAC, Petterson CA, Forsgren M, Orvell C, Strannegard O (1994) Respiratory syncytial virus infection in hospitalized patients and healthy children in El Salvador. Am J Trop Med Hyg 51:577–584
Zheng H, Peret TC, Randoph VB, Crowley JC, Anderson LJ (1996) Strain-specific reverse transcriptase PCR assay: means to distinguish candidate vaccine from wilde-type strains of respiratory syncytial virus. J Clin Microbiol 34:334–337
Zhu Q, McAuliffe JM, Patel NK, Palmer-Hill FJ, Yang CF, Liang B et al (2011) Analysis of respiratory syncytial virus preclinical and clinical variants resistant to neutralization by monoclonal antibodies palivizumab and/or motavizumab. J Infect Dis 203:674–682
Web Sites
CDC- Center for Disease Control and Prevention (2014) Respiratory syncytial virus circulation in the United States, July 2012-Jun 2014. MMWR 62:141–144. Accessed [Feb 2016]
ICTV. International Committee on Taxonomy of Viruses. Available from: http://www.ictvonline.org/virusTaxonomy.asp . [Mar 2015]. Available from: http://www.ictvonline.org/virusTaxonomy.asp. [3 Mar 2016]
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Durigon, E.L., Botosso, V.F., de Oliveira, D.B.L. (2017). Human Respiratory Syncytial Virus: Biology, Epidemiology, and Control. In: Ludert, J., Pujol, F., Arbiza, J. (eds) Human Virology in Latin America. Springer, Cham. https://doi.org/10.1007/978-3-319-54567-7_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-54567-7_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-54566-0
Online ISBN: 978-3-319-54567-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)