Abstract
Background: Currently, there are no recommended assessment protocols for monitoring possible effects of head injury in snowsports athletes who are in competition and training. Objective: This project evaluated the Sport Concussion Assessment Tool 2 (SCAT2) for concussion assessment in a snowsport athlete group. In addition, the project determined the effectiveness of enhancing the SCAT2 protocol by using accelerometer smartphone technology in the balance assessment component of the test battery, with a view to an enhanced protocol for assessment of changes in human motor performance post-concussion injury. Methods: The research team recruited 22 athletes from the New South Wales Institute of Sport and the Olympic Winter Institute Australia snowsport athlete squads who were undertaking baseline sport science testing during the Australian 2012 and 2013 winter seasons. Results: Overall correlation between the SCAT 2 over two separate occasions was moderate/strong (Pearson’s r = 0.58, p = 0.006). Examination of the subcategories within the SCAT2 indicated that the overall correlation was being mediated by the strong correlation of the subset “Symptom Score.” The subset “Balance Score” did not correlate across test occasions (r = 0.42, p = 0.054). There were no other significant correlations across the two occasions of testing. Those who had reported a major head impact history, signified by damage to their helmet during the impact, were significantly older (21.5, SD 4.6 years) than the group not reporting a major head impact (17.5, SD 2.6 years). Two of the instrumented balance test measures, one in the double-leg stance and one in the single-leg stance protocol, showed a significant difference between the “major helmet impact” and “no helmet impact” groups warranting further investigation in a larger sample.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Snowsports are popular winter sports in Australia and have a strong appeal to young and beginner participants. As in any sport, there is a risk of injury, including head injury. Internationally, it has been suggested that traumatic brain injury (TBI) is the leading cause of death in snowsports [1, 2]. Results from an Australian study of patients presenting to the Canberra Hospital with a snowsport-related head injury found that the incidence of head injuries was 1.8 per 1,000,000 skier days (n = 25) with snowboarders having three times the incidence of head injuries of skiers [3]. As with the broader population, snowsport athletes are also at risk of concussion and head injury though at a higher incidence and severity [4, 5]. Thus, there is a need for an effective mechanism to assess any cumulative effects of repeated head impacts or injuries on cognitive and motor performance.
Helmets are proposed to protect against snowsport head injuries [6,7,8,9,10]. An Australian study in Victoria indicated that usage has increased, with children more likely to wear helmets than adults (67% cf. 16% in 2008), however usage was declining [11]. While it has been demonstrated that helmets may reduce the severity of minor injuries in snowsports [11], there continues to be debate about their effectiveness in all circumstances, hence discussion continues about their usefulness. This is consistent with the “Consensus Statement On Concussion In Sport” (CSCS), which states that there is “no good clinical evidence that currently available protective equipment will prevent concussion” [12, 13] though in snowsports helmets may reduce other head and facial injuries. Further, increased helmet usage has not resulted in the expected benefit of less reported head injuries [4]. Yet they are required by FIS for all events [14] but manufactured at similar test standards as recreational helmets where it has been suggested that helmets may not be effective in an impact with a solid object at speeds greater than 23 km/h [2].
The CSCS defines concussion as “a complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces” [12, 13]. Research has been conducted on footballers and ice hockey players related to repeated “mild-impact” and the risk of post-concussion syndrome [15], and there have been efforts to achieve some consensus about how to prevent and manage sport-related concussions [12, 13]. Yet, to date there is no research that reports and monitors the incidence of concussion injury in either athlete or recreational snowsport participants.
The CSCS suggests that “a detailed concussion history is of value” including baseline data gathering prior to a sporting season. A structured concussion history should include specific questions as to previous symptoms of a concussion: not just the perceived number of past concussions. It is also worth noting that dependence upon the recall of concussive injuries by team members or coaches has been demonstrated to be “unreliable” [16]. To this end, the Sport Concussion Assessment Tool 2 (SCAT2) was developed as the recommended tool for assessment of concussion in sport. The SCAT2 is a tool for assessing symptoms and signs reported by the concussed athlete. The SCAT2 score does not independently determine the diagnosis of concussion, nor the athlete’s return-to-play status. The SCAT2 protocol is designed for use to determine a pre-injury baseline and to assess readiness for return-to-play in sports such as the football codes and motor sports. The SCAT2 scoring system incorporates scores for the fields, (1) Symptoms and (2) Cognitive and Physical Evaluation, that includes cognitive assessment, physical signs, balance and coordination, the Glasgow coma scale, and the Maddocks Score.
This project focused on the reliability of the SCAT2 as a baseline test across seasons and on the standing balance assessment component of the SCAT2 test, as the protocol uses a relatively coarse balance assessment approach. The static component of the test uses a hands-on-hips, single-leg stance for 20 s test, with the test scored as the number of times the participant makes movements with the hands away from hips, touches down with one leg, etc. to recover balance, taken as a measure of change in postural sway. With the advances in smart phone technology [17], including the addition of accelerometer systems, the capacity to discover much finer grades of change in sway posture may enhance the sensitivity of the test to detect changes in sway that are indicative of low-level cumulative change in neurologic function. This additional and refined information may then lead to the design of more sensitive SCAT tools.
2 Objectives
As there are currently no recommended assessment protocols for monitoring possible effects of head injury in snowsport athletes who are involved in both competition and training, this project had three objectives:
-
1.
To evaluate the SCAT2 for concussion assessment in a snowsport athlete group
-
2.
To determine the effectiveness of enhancing the SCAT2 protocol using accelerometer smartphone technology in the static “balance assessment” component of the SCAT test
-
3.
To inform the design of an enhanced protocol for assessment of changes in motor performance post-concussion injury: towards an improved SCAT
3 Materials/Methods
Athletes involved in snowsport programs with the New South Wales Institute of Sport and the Olympic Winter Institute of Australia who were competing regionally through to World Cup events were invited to participate in this project. Those who had a significant health issue or those who may have been pregnant did not participate in this study. 22 athletes, 12 male, and 10 female, across a range of snowsport activities (moguls, snowboard cross, and skier cross), volunteered to participate in this project. All were familiarized with the protocol prior to commencing.
Upon consenting to participate, athletes completed the SCAT2 questionnaire sections. A structured concussion history was taken, which included specific questions as to previous symptoms of a concussion, and a question about the number of severe impacts to the head region. A severe impact was indicated where they reported damage to their helmet as a result of an impact, which is one objective measure where medical diagnosis is not available. The clinical history collected included information about all previous head, face, or cervical spine injuries, as these may also have clinical relevance. As part of the clinical history, details regarding protective equipment employed at the time of injury were also gathered, both for recent and old injuries.
Parallel with the SCAT2 protocol, balance was further assessed via:
-
1.
Accelerometer Data Pro smartphone app, a smartphone application that allows recording of acceleration data via a tri-axial accelerometer on an iPhone 3
-
2.
And the “gold standard,” Kistler static force platform, which is commonly used in biomechanics applications for assessment of body sway and accelerations
All measures were undertaken concurrently for all balance tests. The smartphone was worn on the waist in a conforming belt and the participant stood on the force plate (Fig. 1). The suitability of the smartphone accelerometer technology for this application has been demonstrated previously [18]. Accelerometer data was analyzed by determining differences in the standard deviation of the vector sum of accelerations and force platform data via differences in center of pressure area between each balance activity.
Data collection occurred according to the following schedule:
Time 1: Preseason, 2012, (SCAT2A) baseline evaluations and obtaining athlete histories in line with recommendations of the “Consensus Statement on Concussion in Sport,” evaluations involving:
-
Administering the SCAT questionnaire component
-
Concurrently assessing the static balance component of the SCAT via the Accelerometer Data Pro on a smart phone device and the Kistler static force platform
Time 2: Beginning of following winter season (2013) again as described in T1 above (SCAT2B).
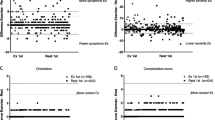
Mean center of pressure and peak frequency measures for the force platform and accelerometer data were determined in each of the x, y, and z planes for each of the standard balance posture tests comprising the balance assessment protocol in the SCAT2 (Fig. 1). Correlations were determined between the overall SCAT2 data scores, and all subsets of the SCAT2 data as well as the mean center of pressure and peak frequency measures for the accelerometer and force platform data.
To determine any difference between those who reported an episode of a major head impact and those who did not, the data was separated into two categories; “those who reported a major head impact history” (n = 8) and those “without a major head impact history” (n = 14). Independent samples t-tests were undertaken on these data to assess any between-group differences.
4 Results
T-tests were undertaken on the data both within-group, comparing participant trials across the data collection period, from pre-test to post-test, and between-group across the snowsport versus control participant groups, in order to determine any differences between the groups using the SCAT2 protocol. Additional test data obtained, where any participant received a head impact during the trial period, was also assessed in the manner described above to determine any impact on sensitivity obtained by including the force or accelerations data in the protocol. 22 participants were assessed over two occasions (Table 1).
Overall correlation between the SCAT2 over the two separate occasions (2012 season SCAT2A and 2013 season SCAT2B) was moderate/strong, with a Pearson’s r of 0.58, p < 0.01. Examination of the subcategories within the SCAT2 indicated that the overall tool correlation was being mediated by the strong correlation of the subset “Symptom Score,” with the Symptom Score A correlating with Symptom Score B Pearson’s r = 0.7, p < 0.01. The subset “Balance Score” did not correlate significantly across the two test occasions Pearson’s r = 0.42, p = 0.054). There were no other significant correlations across the two occasions of testing.
Independent samples t-tests were undertaken to assess any between-group differences between those who reported an episode of a major head impact (n = 8) and those who did not (n = 14). Those who reported a major head impact (21.5, SD 4.6 years) were found to be significantly older than the group not reporting a major head impact (17.5, SD 2.6 years), difference = 4 years older, p = 0.017. However, there was no significant difference between the groups with and without a major head impact in terms of their number of years of experience on either the snowboard or on skis. Those individuals who reported more years of experience snowboarding were more likely to be significantly associated with an episode of damaging a helmet (p = 0.043). However, greater amount of skiing experience was not significantly associated with major damage to a helmet (p = 0.087). Further, there was no significant difference on symptom scores, immediate memory scores or concentration scores between the major head impact and no head impact groups (Tables 2 and 3).
Only two of the measures derived from the instrumented balance test showed a significant difference between the “major helmet impact” and “no helmet impact” groups. These were the single-leg stance force platform CoP measure in the mediolateral “x” plane (p < 0.01) and the double-leg stance accelerometer Normalized Mean Peak Score measure in the mediolateral “x” plane (p < 0.05).
5 Discussion
Based on the results reported here, the symptom component of the SCAT2 is reliable over a 12-month period in snowsports athletes. However, the static balance test component of the SCAT2 protocol, which comprises a visual assessment of errors in the tasks; bilateral feet together stance, single-leg stance and tandem-stance, did not achieve a significant correlation between test scores over the same time period. The SCAT2 tool, although reliable in terms of reported levels of symptom patterns over the test retest period, was not sensitive to differences between participants when they were subdivided into those who had suffered a significant head impact versus those who had not. This result is consistent with previous published work on the SCAT2 that identifies variability in baseline scores in adolescent athletes related to gender, age, and self-reported concussion history [19]. Similarly, this supports the study by Guskiewicz et al. [20] who suggest that there is no evidence to support the use of the composite score for the SCAT2 but that each component of the SCAT scored independently can contribute to concussion assessment.
When participants were separated into those who had suffered a head impact of significant force to damage their helmet and those who had not, the greatest risk for a major head impact seems to occur after the age of 17.5 years. This coincides with the participants entering full adult competition when the pressure to perform at the edge of their capacity is heightened potentially increasing risk-taking combined with an age-related slowing in reaction times from mid-twenties onward [21] which may increase the risk of head injury. Although there was a significantly greater incidence of snowboarders than skiers reporting breaking a helmet, neither snowboarders nor skiers who also broke a helmet had an associated higher incidence of major head impacts. Based on the data in this study, a helmet breakage event is not necessarily equivalent to a severe head impact. This result may cautiously be interpreted as suggesting that the helmet is effectively attenuating a forceful head impact, through the destruction of the helmet.
Two of the instrumented balance assessments, the single-leg stance force platform center of pressure measure in the mediolateral “x” plane and the double-leg stance accelerometer normalized mean peak frequency score measure in the mediolateral “x” plane were significantly different between those receiving a broken helmet during a fall and those who did not experience breaking a helmet and should be considered for further evaluation in a larger sample of participants. This result suggests that accelerometer systems in current smart phone devices may be sensitive to changes in aspects of balance following head impacts and warrants further research. A number of previous research reports indicate changes in postural sway measures occurring following recent concussions, for example, within 48 h post-injury [22] and up to 30 days post-injury [23]. The finding of a difference in a measure of postural sway extending out to months across a season is however consistent with recent reports of changes in performance characteristics and increased lower limb injury rates extending across seasons in concussed athletes [24, 25]. This suggests that the concussion injury may produce residual changes in the balance control systems of the athlete that may result in a higher risk of injury following their return to sport.
Based upon the insights gleaned from this and prior research, further research is warranted to understand both the contributing factors to head injuries and the effect of head impacts on snowsport participants, to inform appropriate and effective snowsport safety strategies. This includes:
-
Exploring contributing factors to head injuries such as balance, proprioception, hydration, and risk-taking (e.g., [26,27,28,29]).
-
Additional research to determine the effectiveness of concussion assessment tools, such as the SCAT 2 and SCAT3, in the immediate post-injury period to allow effective monitoring of return to sport protocols.
-
Instrumented balance assessment needs to be further evaluated as a tool in acute concussion evaluation in snowsports athletes.
While this research has been able to add to the overall understanding of a potential tool, the SCAT2, for the evaluating the effect of snowsport head impacts, there are a number of limitations to the research design. The size of the cohort available of high performance athletes in this mix of sports in Australia is determined by practical considerations that limit the number of athletes available for testing at any one time. The small numbers available mean that the resulting power to detect differences between groups will be less than that achievable with larger sample sizes. However, this can be addressed by collecting data across a series of seasons to increase sample size over time. The self-report mechanism for determining “major head impacts” is not as effective as a formal medically diagnosed concussion episode. However at the level at which these athletes are competing they are acutely aware of episodes that remove them from training or competition for a period of time. This categorization in this study was able to produce significant differences between groups where the categorization regarding a “broken helmet” was not.
The key insights from this research are that:
-
The symptom component of the SCAT2 is reliable over a 12-month period in snowsport athletes.
-
The balance test component of the SCAT2 protocol, which comprises a visual assessment of errors in the tasks, bilateral feet together stance, single-leg stance, and tandem-stance, did not achieve a significant correlation over the same time period.
-
The SCAT2 tool was not sensitive to differences between participants who had suffered a significant head impact versus those who had not.
-
Two of the instrumented balance assessment measures were significantly different when the group was separated into those who had sustained a helmet damaging fall and those who had not and should be considered for further evaluation in a larger sample of participants.
-
Devices such as the accelerometers in smartphones need to be further evaluated to determine their usefulness in detection of motor function changes post-head impact.
-
The greatest risk for a significant head impact occurs after the age of 17.5 years.
-
Helmet breakage is not an effective analogue of equivalence for a severe head impact.
References
Levy AS, Hawkes AP, Hemminger LM, Knight S (2002) An analysis of head injuries among skiers and snowboarders. J Trauma 53(4):695–704
Shealy JE, Johnson RJ, Ettlinger CF (2008) The science behind helmets. Ski Canada 37(2):50–53
Siu TLT, Chandran KN, Newcombe RL, Fuller JW, Pik JHT (2004) Snow sports related head and spinal injuries: an eight-year survey from the neurotrauma centre for the Snowy Mountains, Australia. J Clin Neurosci 11(3):236–242
Dickson TJ, Trathen S, Terwiel FA, Waddington G, Adams R (2017) Head injury trends and helmet use in skiers and snowboarders in Western Canada, 2008–09 to 2012–13: an ecological study. Scand J Med Sci Sports 27(2):236–244. doi:10.1111/sms.12642
Steenstrup SE, Bere T, Bahr R (2014) Head injuries among FIS World Cup alpine and freestyle skiers and snowboarders: a 7-year cohort study. Br J Sports Med 48(1):1–6
Cusimano MD, Kwok J (2010) The effectiveness of helmet wear in skiers and snowboarders: a systematic review. Br J Sports Med 44:781–786. doi:10.1136/bjsm.2009.070573
Hagel BE, Pless IB, Goulet C, Platt RW, Robitaille Y (2005a) The effect of helmet use on injury severity and crash circumstances in skiers and snowboarders. Accid Anal Prev 37(1):103–108
Hagel BE, Pless IB, Goulet C, Platt RW, Robitaille Y (2005b) Effectiveness of helmets in skiers and snowboarders: case-control and case crossover study. Br Med J 330(7486):281. doi:10.1136/bmj.38314.480035.7C
McCrory P (2002) Editorial: the role of helmets in skiing and snowboarding. Br J Sports Med 36(5):314. doi:10.1136/bjsm.36.5.314
Mueller BA, Cummings P, Rivara F, Brooks MA, Terasaki RD (2008) Injuries of the head, face, and neck in relation to Ski helmet use. Epidemiology 19(2):270–276
Cundy TP, Systermans BJ, Cundy WJ, Cundy PJ, Briggs NE, Robinson JB (2010) Helmets for snow sports: prevalence, trends, predictors and attitudes to use. J Trauma 69(6):1486–1490
McCrory P, Meeuwisse W, Johnston K, Dvorak J, Aubry M, Molloy M, Cantu R (2009) Consensus statement on concussion in sport—the 3rd International Conference on concussion in sport, held in Zurich, November 2008. J Clin Neurosci 16(3):755–763
McCrory P, Meeuwisse WH, Aubry M, Cantu B, Dvořák J, Echemendia RJ, Engebretsen L, Johnston K, Kutcher JS, Raftery M, Sills A, Benson BW, Davis GA, Ellenbogen RG, Guskiewicz K, Herring SA, Iverson GL, Jordan BD, Kissick J, McCrea M, McIntosh AS, Maddocks D, Makdissi M, Purcell L, Putukian M, Schneider K, Tator CH, Turner M (2013) Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med 47(5):250–258. doi:10.1136/bjsports-2013-092313
Fédération Internationale de Ski (FIS) (2011) Specficiations for competition equipment and commercial markings: edition 2011/12. Equipment, FIS
Bigler ED (2008) Neuropsychology and clinical neuroscience of persistent post-concussive syndrome. J Int Neuropsychol Soc 14(1):1–22. doi:10.1017/S135561770808017X
Sulheim S, Holme I, Ekeland A, Bahr R (2006) Helmet use and risk of head injuries in alpine skiers and snowboarders. J Am Med Assoc 295(8):919–924
Curaudeau GA, Sharma N, Rovin RA (2011) Development of an iPhone application for sideline concussion testing. Neurosurg Focus 31(5):E4. doi:10.3171/2011.8.FOCUS11186
Amick RZ, Patterson JA, Jorgensen MJ (2013) Sensitivity of tri-axial accelerometers within mobile consumer electronic devices: a pilot study. Int J Appl 3(2):97–100
Valovich McLeod TC, Bay RC, Lam KC, Chhabra A (2012) Representative baseline values on the Sport Concussion Assessment Tool 2 (SCAT2) in adolescent athletes vary by gender, grade, and concussion history. Am J Sports Med 40(4):927–933
Guskiewicz KM, Register-Mihalik J, McCrory P, McCrea M, Johnston K, Makdissi M, Dvořák J, Davis G, Meeuwisse W (2013) Evidence-based approach to revising the SCAT2: introducing the SCAT3. Br J Sports Med 47(5):289–293. doi:10.1136/bjsports-2013-092225
Woods DL, Wyma JM, Yund EW, Herron TJ, Reed B (2015) Age-related slowing of response selection and production in a visual choice reaction time task. Front Hum Neurosci 9:193
Cavanaugh JT, Guskiewicz KM, Giuliani C, Marshall S, Mercer V, Stergiou N (2005) Detecting altered postural control after cerebral concussion in athletes with normal postural stability. Br J Sports Med 39(11):805–811
Slobounov S, Cao C, Sebastianelli W, Slobounov E, Newell K (2008) Residual deficits from concussion as revealed by virtual time-to-contact measures of postural stability. Clin Neurophysiol 119(2):281–289
Brooks MA, Peterson K, Biese K, Sanfilippo J, Heiderscheit BC, Bell DR (2016) Concussion increases odds of sustaining a lower extremity musculoskeletal injury after return to play among collegiate athletes. Am J Sports Med 44(3):742–747
Wasserman EB, Abar B, Shah MN, Wasserman D, Bazarian JJ (2015) Concussions are associated with decreased batting performance among major league baseball players. Am J Sports Med 43(5):1127–1133
Dickson TJ (2008) Behaviors and attitudes towards snowsport safety in Australia. J ASTM Int 5(4):Jai101433. doi:10.1520/JAI101433
Han J, Waddington G, Anson J, Adams R (2015) Level of competitive success achieved by elite athletes and multi-joint proprioceptive ability. J Sci Med Sport 18(1):77–81
Ruedl G, Burtscher M, Wolf M, Ledochowski L, Bauer R, Benedetto KP, Kopp M (2015) Are self-reported risk-taking behavior and helmet use associated with injury causes among skiers and snowboarders? Scand J Med Sci Sports 25(1):125–130. doi:10.1111/sms.12139
Waddington GS, Dickson TJ, Trathen S, Adams RD (2010) Hydration packs modify professional skiers’ hydration levels in all day skiing: a randomised controlled trial. J ASTM Int 7(10):JAI102818. doi:10.1520/JAI102818
Acknowledgements
This project could not have been undertaken without the support of John Marsden, Chief Sport Scientist for the Olympic Winter Institute Australia, and NSW Institute of Sport who facilitated the coordination of access to the OWIA and NSWIS athletes. Grateful acknowledgement is given to the NSW Sporting Injuries Committee who provided the overall funding support for the project.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
This chapter is distributed under the terms of the Creative Commons Attribution-Noncommercial 2.5 License (http://creativecommons.org/licenses/by-nc/2.5/) which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
The images or other third party material in this chapter are included in the work’s Creative Commons license, unless indicated otherwise in the credit line; if such material is not included in the work’s Creative Commons license and the respective action is not permitted by statutory regulation, users will need to obtain permission from the license holder to duplicate, adapt or reproduce the material.
Copyright information
© 2017 The Author(s)
About this paper
Cite this paper
Waddington, G., Trathen, S., Dickson, T.J., Adams, R., Rumore, A. (2017). A Sport Concussion Assessment Tool (SCAT2) for Use in Snowsports: Can the Balance Component of the Tool Be Improved?. In: Scher, I., Greenwald, R., Petrone, N. (eds) Snow Sports Trauma and Safety. Springer, Cham. https://doi.org/10.1007/978-3-319-52755-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-52755-0_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-52754-3
Online ISBN: 978-3-319-52755-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)