Abstract
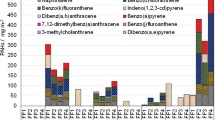
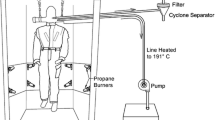
Firefighting as an occupation involves exposure to many chemical hazards, including many known and suspected carcinogens. These exposures often occur at intense exposure levels despite the availability of self-contained breathing apparatus (SCBA), which cannot be used indefinitely. Skin absorption is significant for many chemical hazards. The source of the most toxic chemical exposures routinely encountered in firefighting is generally combustion, including lignocellulosic material (wood and paper) but particularly of synthetic polymers, which make available chlorine for halogenation of many combustion products, producing, among other toxic chemical products, dioxins and furans. Other products of combustion include: polycyclic aromatic hydrocarbons, some of which are known carcinogens; volatile organic compounds, including benzene, a potent carcinogen, and halogenated hydrocarbon compounds more familiar as solvents, some of which are also known or suspected carcinogens; 1,3-butadiene, a carcinogen; formaldehyde, also a carcinogen; and nitroarenes, some of which are carcinogens, predominantly from diesel emissions. Fine particulate matter is produced by both fire and diesel exhaust. The acute toxicity of carbon monoxide and cyanide are well known. Other hazardous materials, such as asbestos and polychlorinated biphenyl compounds (PCBs) may be encountered during in particular situations. Halogenated flame retardants are a newly emerging class of chemical hazard. A brief introduction to toxicology is appended to the chapter.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Laitinen J, Makela M, Mikkola J, Huttu I. Firefighters’ multiple exposure assessments in practice. Toxicol Lett. 2012;213:129–33.
Booze TF, Reinhardt TE, Quiring SJ, Ottmar RD. A screening-level assessment of the health risks of chronic smoke exposure for wildland firefighters. J Occup Environ Hyg. 2004;1:296–305.
Eliopulos E, Armstrong BK, Spickett JT, Heyworth F. Mortality of fire fighters in Western Australia. Br J Ind Med. 1984;41:183–7.
Fabian TZ, Gandhi P. Smoke characterization project: Technical report. Northbrook, IL: Underwriters Laboratories, Inc.; 2007.
Daniels RD, Kubale TL, Yiin JH, et al. Mortality and cancer incidence in a pooled cohort of US firefighters from San Francisco, Chicago and Philadelphia (1950–2009). Occup Environ Med. 2014;71(6):388–97.
Hesterberg TW, Long CM, Bunn WB, Lapin CA, McClellan RO, Valberg PA. Health effects research and regulation of diesel exhaust: an historical overview focused on lung cancer risk. Inhalation toxicology. 2012;24 Suppl 1:1–45.
Diesel and Gasoline Engine Exhausts and Some Nitroarenes. World Health Organization, 2013
Shaw SD, Berger ML, Harris JH, et al. Persistent organic pollutants including polychlorinated and polybrominated dibenzo-p-dioxins and dibenzofurans in firefighters from Northern California. Chemosphere. 2013;91:1386–94.
Humblet OBL, Rimm E, Mittleman MA, Hauser R. Dioxins and cardiovascular disease mortality. Environ Health Perspect. 2012;116:1443–8.
Jin CF, Sun YH, Islam A, Qian Y, Ducatman A. Perfluoroalkyl acids including perfluorooctane sulfonate and perfluorohexane sulfonate in firefighters. J Occup Environ Med. 2011;53:324–8.
Chiu WA, Jinot J, Scott CS, et al. Human health effects of trichloroethylene: key findings and scientific issues. Environ Health Perspect. 2013;121:303–11.
Cocco P, Vermeulen R, Flore V, et al. Occupational exposure to trichloroethylene and risk of non-Hodgkin lymphoma and its major subtypes: a pooled IinterLlymph analysis. Occup Environ Med. 2013;70:795–802.
Hansen J, Sallmen M, Selden AI, et al. Risk of cancer among workers exposed to trichloroethylene: analysis of three Nordic cohort studies. J Natl Cancer Inst. 2013;105:869–77.
Karami S, Bassig B, Stewart PA, et al. Occupational trichloroethylene exposure and risk of lymphatic and haematopoietic cancers: a meta-analysis. Occup Environ Med. 2013;70:591–9.
Mandel JH, Kelsh M, Mink PJ, Alexander DD. Trichloroethylene exposure and non-Hodgkin’s lymphoma: supportive evidence. Occup Environ Med. 2008;65:147–8.
McLaughlin JKBW. A critical review of epidemiology studies of trichloroethylene and perchloroethylene and risk of renal-cell cancer. Int Arch Occup Environ Health. 1997;70:222–31.
McNeil C. TCE, designated a known carcinogen, now the focus of ongoing research. J Natl Cancer Inst. 2013;105:1518–9.
Rusyn I, Chiu WA, Lash LH, Kromhout H, Hansen J, Guyton KZ. Trichloroethylene: Mechanistic, epidemiologic and other supporting evidence of carcinogenic hazard. Pharmacol Ther. 2014;141:55–68.
Vlaanderen J, Straif K, Pukkala E, et al. Occupational exposure to trichloroethylene and perchloroethylene and the risk of lymphoma, liver, and kidney cancer in four Nordic countries. Occup Environ Med. 2013;70:393–401.
Purdue M, Bakke B, Stewart P, DeRoos AJ, Schenk M, Lynch CF, Bernstein L, Morton LM, Cerhan JR, Severson RK, Cozen W, Davis S, Rothman N, Hartge P, Colt JD. A case-control study of occupational exposure to trichloroethylene and non-Hodgkin lymphoma. Environ Health Perspect. 2011;119:232–8.
Guidotti TL, Clough VM. Occupational health concerns of firefighting. Annu Rev Public Health. 1992;13:151–71.
Brandt-Rauf PW, Cosman B, Fallon Jr LF, Tarantini T, Idema C. Health hazards of firefighters: acute pulmonary effects after toxic exposures. Br J Ind Med. 1989;46:209–11.
Bolstad-Johnson DM, Burgess JL, Crutchfield CD, Storment S, Gerkin R, Wilson JR. Characterization of firefighter exposures during fire overhaul. AIHAJ. 2000;61:636–41.
Austin CC, Dussault G, Ecobichon DJ. Municipal firefighter exposure groups, time spent at fires and use of self-contained-breathing-apparatus. Am J Ind Med. 2001;40:683–92.
Austin CC, Wang D, Ecobichon DJ, Dussault G. Characterization of volatile organic compounds in smoke at municipal structural fires. J Toxicol Environ Health A. 2001;63:437–58.
Austin CC, Wang D, Ecobichon DJ, Dussault G. Characterization of volatile organic compounds in smoke at experimental fires. J Toxicol Environ Health A. 2001;63:191–206.
Jankovic J, Jones W, Burkhart J, Noonan G. Environmental study of firefighters. Ann Occup Hyg. 1991;35:581–602.
Ruokojarvi P, Aatamila M, Ruuskanen J. Toxic chlorinated and polyaromatic hydrocarbons in simulated house fires. Chemosphere. 2000;41:825–8.
Gold A, Burgess WA, Clougherty EV. Exposure of firefighters to toxic air contaminants. Am Ind Hyg Assoc J. 1978;39:534–9.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Appendix: A Primer on Toxicology
Appendix: A Primer on Toxicology
Toxicology is a sophisticated and complicated science, grounded in biochemistry and physiology. This section is a short introduction to toxicology, provided so that references on individual toxic chemicals may be easier to follow by anyone concerned, whether physician, lawyer, human resources staff, hearing officer, judge, or legislator. This section should be unnecessary for experts, however. Experts, of course, should go to the primary literature whenever possible and should know all or most of this material already.
The most authoritative and convenient references available for individual chemicals are the Toxicological Profiles developed for the Agency for Toxic Substances and Disease Control. These publications are available in hardcopy or without cost on-line (http://www.atsdr.cdc.gov/toxprofiles/index.asp). Each Toxicological Profile summarizes the world literature on a particular chemical exposure , objectively and comprehensively. If they have a fault, however, it is that they tend to be too complete and sometimes include studies that are not particularly helpful. They also do not always explain the significance of the information. Overall, however, they are exceptionally well written and produced. Reading them can be a chore for someone who does not have a background in toxicology. Fortunately each one comes with a summary in nontechnical language in front. To get the most out of them or any such resource, however, it helps to know the principles of toxicology.
Toxicology is the science of how the human body handles and responds to chemicals. The part that has to do with how the body is exposed to chemicals and how they are handled is called “toxicokinetics”. It can be thought of as “what the body does to the chemical”. The part about how the body responds to the chemical is called “toxicodynamics.” It can be thought of as “what the chemical does to the body.”
Toxicity occurs as a result of the effect of the chemical on the body and the body’s response to it. Toxicity can range from barely detectable to death . When toxicity results in a set of symptoms and signs, called a “toxidrome”, that is characteristic of a particular chemical exposure , it is called “poisoning”, but toxicologists do not use this word as freely as it is used in regular language. (They prefer “toxicity.”) Once a chemical substance encounters the body and enters that route of exposure, it may cause local problems at the site of entry, for example lung injury due to smoke inhalation , or it may enter the body (absorption ), be carried somewhere else (distribution), and may cause problems elsewhere in the body. This is called “systemic toxicity.”An important example of systemic toxicity for firefighters is carbon monoxide , because carbon monoxide does not injure the lung at all, but it enters the body through the lung and has effects on many other organs.
A toxic effect may be “acute”, meaning occurring quickly. In toxicology, “acute” does not mean intense, as it may in common language. Carbon monoxide causes acute effects . A toxic effect may be “chronic”, meaning that the outcome evolves over a longer time. Cancer is a chronic effect.
Toxicokinetics
“Toxicokinetics” describes what happens when the chemical gets taken into the body. Toxicologists often refer to all chemical substances not normally present in the body as “xenobiotics.” These can be chemical pollutants, drugs, venoms and natural poisons, cosmetics and personal care products, and even nutrients. The acute toxic effect of a xenobiotic is proportional to the concentration and for most is determined by concentration in the blood. This in turn depends in part on the rate of absorption and entry into the blood.
How a chemical reaches the body is called the “pathway of exposure ” and the means by which it enters the body is called the “route of entry.” There are only so many routes of entry into the human body: breathing it in, getting it on skin or mucous membranes, or swallowing it; everything else is artificial and applies more in the lab than in real-world exposures, such as getting an injection.
For a gas or a particle of smoke coming off of a fire, the “pathway” is being carried on air and the route of exposure is inhalation , because the gas or particle is breathed into the lung . For skin contact, the pathway might be deposition of soot onto a surface which is then touched and the route of exposure is skin contact.
There are four phases that describe what happens to a xenobiotic in the body: absorption (how a xenobiotic gets into the body), distribution (how it is delivered to various parts of the body by the bloodstream and other means), metabolism (the chemical biotransformation of the xenobiotic), and excretion. Figure 5.3 illustrates these four steps. The latter two steps, metabolism and excretion, combined, constitute “elimination,” because they describe the removal of the xenobiotic from the body.
Principles of toxicokinetics: the passage of a chemical through the body. (Adapted from Guidotti TL. Principles of occupational toxicology (Chap. 7). In: Zenz C, Nickerson B, Horvath EP, eds. Occupational Medicine: Principles and Practical Applications, 3rd edn. Chicago, Mosby-Year Book, 1994, pp. 70–84.)
Absorption
Xenobiotics may enter the body through any of several routes of entry, of which the most important for firefighters is inhalation . Inhalation is most important for firefighters but skin contact plays a small secondary role as a pathway for volatile organic compounds. Ingestion is comparatively unimportant for firefighting-related exposures.
For firefighters, by far the most common and the most important “route of exposure ” is inhalation , when the chemical is airborne and breathed into the lungs. There is hardly any barrier between the air in the lung and the bloodstream, so chemicals in the form of a gas that are inhaled enter the circulation very quickly and completely. Inhalation delivers a lot of the substance to the blood stream quickly, leading to a high but short peak concentration. An example relevant to firefighters is carbon monoxide , which enters the bloodstream from the lungs very quickly, attaches to haemoglobin in red cells in the blood almost instantaneously, and is carried throughout the body within seconds. After that, other processes take over to determine blood concentration. In the case of carbon monoxide, the molecule detaches itself from haemoglobin slowly, over hours.
The lung has some means to protect itself. There are many “host defense mechanisms” that serve to protect a person (or an animal) from the effects of chemical exposures and to reduce absorption . Particle clearance from the lung is especially important, with special particles (alveolar macrophages) that engulf and remove inhaled particles, and a special mechanisms called the “mucociliary escalator” that bring up particles from the deep lung through moving a thin mobile layer of mucus upward. A soluble particle may be broken down by the alveolar macrophage which may release its constituent chemicals into the bloodstream.
Exposure by inhalation results in relatively efficient absorption of gases and a quick peak concentration of blood if the gas can penetrate to the deep lung . Whether the gas will penetrate efficiently depends on its solubility in water, reflecting clearance rates in the bronchial tree. Particles, on the other hand, are subject to a number of host-defense mechanisms in the respiratory tract that limit the efficiency of penetration to the alveolar level. Once there, their size prevents them from passing directly into the bloodstream and they must dissolve or be digested by macrophages (defense cells that engulf bacteria and particles and that try to digest them) before their constituent chemical contents can be absorbed and enter the bloodstream. Particles may contribute to systemic toxicity if they are composed of a soluble material, such as lead or polycyclic aromatic hydrocarbons . Particles at nanoscale (on the order of 100 nm or so) often have very different characteristics than larger particles of the same composition and tend to be much more toxic.
Absorption into the bloodstream after skin exposure is relatively slow and incomplete. Turnout gear is largely protective, preventing most skin contact. Some small concentrations of volatile xenobiotics such as solvent chemicals can be detected in the breath of firefighters who are fully protected by the inhalation route with SCBA and wearing turnout gear . This shows that despite some skin absorption does take place, even with protective clothing, but not much.. Skin is also the local target organ for skin carcinogens, such as polycyclic aromatic hydrocarbons . Skin can be penetrated quickly by chemicals that dissolve easily in fats (“lipid-soluble”) and this can facilitate the penetration of other chemicals as well. Within the context of firefighting, skin exposure is generally more likely to be important as a cause of local problems of the skin, including irritation and skin cancer , rather than as a route of exposure for systemic toxicity.
The third common route of exposure , ingestion, which is less important for firefighters than the other two. Ingestion is an important route of exposure for water and food and occasionally in special situations where food or a cigarette is contaminated by something on a person’s hands.
Distribution
Once the xenobiotic is absorbed and enters the bloodstream, it is transported to the capillary level in tissues of the body where it becomes available for uptake by the target organ. After one pass through the circulation, the xenobiotic is uniformly mixed in arterial blood, regardless of its route of entry. The peripheral tissues are therefore presented with an increasing concentration of xenobiotic in the blood which peaks and then declines, as the xenobiotic is distributed to tissues throughout the body, removed and stored in whatever tissue depots may accumulate the xenobiotic (sometimes this depot consists of proteins in the blood itself), and then eliminated by metabolism or excretion.
Uptake of a xenobiotic from the plasma by an organ depends on the blood flow to the organ and the affinity of the tissue for the material. In most cases, delivery of a xenobiotic depends on the blood supply to a tissue relative to its weight. The liver and kidneys each receive massive fractions of the cardiac output and are therefore presented with circulating xenobiotics in quantity.
Special transport mechanisms exist at the cellular level for some xenobiotics. As mentioned above in the context of absorption into the body, absorption of a xenobiotic from the bloodstream into the tissue depends importantly on the solubility of the xenobiotic in fat (how “lipophilic” it is). Lipophilic agents will accumulate in lipid-rich organs such as the nervous system or in liver. Organs with a lipid (fat) content accumulate much larger concentrations of highly lipophilic xenobiotics, such as organohalide pesticides or the PCBs, than occurs in plasma or in other organs. One important implication of storage in fatty tissues is that accumulation in breast tissue results in subsequent excretion into breast milk, which is the major route of exposure to a variety of xenobiotics for infants who breast feed. Where the physicochemical properties of the organ attract and bind metals, as in bone and kidney , a metal or semimetal xenobiotic will be sequestered and will accumulate over time.
Entry into some tissues is restricted by special barriers to passage, such as the blood-brain barrier and the placenta. These barriers generally keep out more toxic classes of xenobiotics and permit passage of nutrients and xenobiotics that resemble nutrients. The brain also receives a disproportionate fraction of the cardiac output but is partly protected by the blood-brain barrier; this barrier works well for most polar xenobiotics but is permeable to lipophilic compounds.
Metabolism
Many xenobiotics are substrates for intracellular enzyme systems. There are many biochemical pathways and enzyme systems that metabolize xenobiotics, either as a primary function or as an incidental function to another role. From the standpoint of evolutionary biology, it is thought that most of these mechanisms of metabolism developed to detoxify and excrete harmful substances ingested in foods (especially natural toxins from plants and those in spoiled or putrefied foodstuffs) or to metabolize and therefore control levels of endogenous chemical compounds (such as steroid hormones).
These enzyme systems transform the xenobiotic in a series of steps from the original compound to a series of stable metabolites, often through unstable intermediate compounds. For many xenobiotics there are many pathways of metabolism, resulting in numerous metabolites. These transformations may have the effect of either “detoxifying” the xenobiotic by rendering the agent toxicologically inactive, or of “activating” the xenobiotic by converting the native agent into a metabolite that is more active in producing the same or another toxic effect. (By convention, a metabolite that is activated or unstable is often indicated with an asterisk.) An active xenobiotic may be transformed into an inactive metabolite, effectively removing the agent from the body in its toxicologically active form. The metabolism of xenobiotics ranges widely in scope, from highly specialized biochemical pathways, such as the biotransformation of cyanide , to complex and alternative pathways with several steps, such as occurs with benzene . For most important organic compounds, such s the polycyclic aromatic hydrocarbons (PAHs ), however, there is a pattern to biotransformation.
In general, the enzyme systems available for the metabolism of organic xenobiotics such as the PAHs usually consist of two phases, especially in the very important “mixed function oxidase” (MFO) system. Phase I involves converting lipid-soluble, water-insoluble compounds into water-soluble products that are more easily excreted in urine or bile. This often results in activation, and results in a metabolite capable of interacting with macromolecules, such as DNA. Activation of a procarcinogen, for example, into a carcinogen may be the initial step in the early stages of carcinogenesis. Phase II involves the removal or conversion of chemical groups in such a way as to render the molecule more polar and therefore more easily excretable by the kidney (and less easily diffused back across the renal tubular epithelium after filtration). In the process, the activated xenobiotic metabolite from Phase I usually becomes inactivated. This process frequently involves “conjugation,” the attachment of a chemical group (such as sulfonate or glucuronic acid) that makes the molecule much more hydrophilic (water soluble). This makes it much easier for the body to excrete the xenobiotic through the kidney or liver and eliminate it from the body.
Some enzyme pathways, such as those in the MFO system, have the effect of activating xenobiotics so that the metabolite is more toxic than the original chemical. Most, however, detoxify the chemical and clear it from the tissue and bloodstream and so contribute to its elimination.
The most complicated metabolic pathways are those for organic compounds. Metals may also be metabolized, however. The methylation of mercury and arsenic, especially, plays a major role in their toxicity. The methylation pathway of arsenic is species- specific and the reason why arsenic is a carcinogen in humans but not in animals.
Excretion
The xenobiotic or its metabolites would remain and accumulate within the body if there were no mechanisms for excretion. Elimination is the term used for removal of the xenobiotic, especially from the bloodstream, by excretion or metabolism or sequestration (storage).
The kidney is the major route of excretion for most xenobiotics. The liver, besides being an important metabolizing organ, secretes some xenobiotics, including heavy metals such as lead and mercury, into bile, which passes into the small intestine, through the large intestine and out in feces. Sometimes, metabolites that are excreted in bile will be reabsorbed in the small intestine and will recirculate, a phenomenon called “enterohepatic circulation.” Enterohepatic circulation causes many xenobiotics and metabolites, such as mercury and many organochlorines, to persist in the body much longer than they would otherwise.
Xenobiotics and their metabolites are also eliminated by various minor routes. Some gases leave the body by passing directly from the bloodstream into air in the lungs and are exhaled. Lipophilic xenobiotics, such as organochlorines, may also be excreted in breast milk, which is potentially a consideration for exposure of the child but is usually not a significant route of elimination from the mother. Water-soluble agents are filtered through sweat glands much as they are in the kidney , but this is not an important route of elimination. It is not true that a person can be “detoxified” from toxic substances by sweating in a sauna, steam bath, or sweat lodge.
Toxicodynamics
There are as many potential mechanisms of toxic effects as there are reactions in biochemistry and functions in physiology, there are a few processes that have special characteristics that affect their behavior, such as inflammation (particularly important in lung disorders) and the causation of cancer (carcinogenesis).
Carcinogenesis is a complicated process. The body is constantly bombarded by carcinogenic chemicals and other influences. Carcinogenic chemicals that make it through the body’s defences alter DNA and other molecules in the body continually but mostly nothing happens. Infrequently, at random, there is an event resulting in damage to DNA that does matter. This event causes a mutation or other defect that changes the cell’s control mechanisms but the cell can still divide and grow. The process proceeds stepwise, with each step controlled by a more or less a random event. Each step and the total sequence takes time, which is called “latency .” For environmental cancers, the latency of a cancer from the time of first exposure to detection of the tumor typically takes many years (generally 15 or more) or decades. (There are exceptions in which latency is shorter, for example, leukemia .) Unless stopped at a given step or the cell shuts down, this leads to a clone of abnormal cells that can form a tumor, can invade surrounding normal tissue, and can metastasize elsewhere in the body (often through the bloodstream).
Cancer is a disorder of genetically-determined control of cell division and growth which, once it begins, proceeds by its own biological determinants. While cancer can arise in any living tissue (although it is rare in many) and manifest itself in many tissue types, the actual number of genetic defects is limited, probably to only a few dozen. In theory, in the future it may be possible to assess causation of cancers much more accurately by looking at the genomics of the cancer of a particular tissue type rather than its site. Because the underlying cellular event occurs at random, cancer occurs at random in the susceptible population. One person may get it and the next person will not, purely by chance. However, increasing exposure to a carcinogen increases the probability that it will occur in an individual and increases the number of cancers that can be observed in the population. Epidemiologists use this association to identify probable causes of cancer.
The central principle in toxicodynamics is the relationship between exposure to the xenobiotic and the adverse response on the body. This relationship, called the “dose-response” or “exposure-response” relationship is the most fundamental idea in toxicology: the more of a toxic chemical one is exposed to, the greater the effect. Toxicologists often quote one of the great scientists of the late Middle Ages, Paracelsus, who was the first to recognize that “the dose makes the poison.” Everything is toxic if the dose is high enough, including water. (Water intoxication, and the seizures it causes, is very rare and more often the result of an endocrine or psychiatric disturbance.) However, at a low enough level, everything is “safe,” even the most potent poisons known. (Botulinum toxic and ricin remain lethal down to exceedingly low dosage levels but even they have levels below which there is no effect.)
There are three distinct varieties of the exposure -response relationship that need to be separated out. These are:
-
The toxicological dose-response relationship, which refers to the principle that the response at a tissue or cellular level is proportionate to the amount of the agent delivered to the tissue; the other exposure -response relationships build on this one
-
The clinical dose- or exposure -response relationship, which refers to the principle that in a given individual (human or animal), different symptoms and signs may appear as different effects predominate with increasing exposure; this is what we want to know for an individual
-
The epidemiological exposure -response relationship, which refers to the principle that in a population of individuals, the cases of disease or toxicity become more frequent with increasing exposure; this is what we want to know if we are concerned about whether cancer is caused by a chemical.
In this chapter, and in most handbooks of hazardous substances, we are most concerned with the clinical exposure -response relationship. This type of exposure-response relationship describes what one would see in an individual with increasing exposure, which symptoms and signs would apper, and in the end what the toxidrome of severe toxicity (poisoning) would look like.
The epidemiological exposure response relationship relates exposure levels to the frequency of the response in a population, based on the number of people showing a sign characteristic of the outcome (such as a symptom) or the entire toxidrome (which in epidemiology is called a “case definition”). This is the essential approach used in environmental epidemiology and yields what is usually called the “epidemiological” exposure-response relationship, with increasing count or rate associated with increasing exposure. In epidemiology, one is interested in how frequently a response is associated with a given level of exposure in a population. Recognized cases (based on the toxidrome, or some simplified “case definition”, such as cancer type) are counted as cases, and if there is an association (and if it is causal) the frequency of cases should increase with increasing exposure. An increasing number of cases cross this threshold and are observed with increasing exposure, yielding the “epidemiologic” exposure-response relationship, which relates magnitude of exposure to frequency of disease, not severity. This relationship is particularly important for disorders that are “stochastic” (arising on a probabilistic basis) rather than showing gradations of severity as a result of exposure, such as cancer, immune-mediated disorders, and infectious disease .
Occupational toxicologists are very concerned that exposure to complex mixtures, such as fire smoke . Mixtures have the potential for numerous interactions and for producing unpredictable effects. Some xenobiotics are well known interact with others to produce disproportionate effects. For example, many chemicals in air hitch a ride onto particles (by adsorbing onto their surface) and penetrate more deeply into the lung than they wood otherwise. The classic example of a positive interaction (often called “synergism) is the combination of cigarette smoke (and possibly other forms of smoke ) with asbestos : for cigarette smoke, the risk of lung cancer is a multiple of the risk from asbestos alone, not just the simple addition of the same risk as from the smoke alone. Other xenobiotics do not seem to interact and exert their actions in an additive way. Absence of an interaction is more likely when the pollutants are all members of the same class or have relevant chemical properties in common. For example, the combined effect of different PAHs that cause cancer is additional cancer, not a synergistic risk.
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Guidotti, T.L. (2016). Toxic Hazards. In: Guidotti, T. (eds) Health Risks and Fair Compensation in the Fire Service. Risk, Systems and Decisions. Springer, Cham. https://doi.org/10.1007/978-3-319-23069-6_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-23069-6_5
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-23068-9
Online ISBN: 978-3-319-23069-6
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)