Abstract
Overzealous fluid administration and capillary leaks may lead to overhydration or tissue edema. The deleterious effects of tissue edema involve disruption of tissue and endothelial glycocalyx, impeding capillary and lymphatic drainage, and causing cellular hypoxia and organ dysfunction. Evidence suggests that a progressive, cumulative positive fluid balance in patients with sepsis is an independent risk factor for organ failure and death. A combination of clinical, laboratory tests (such as hematocrit, brain natriuretic peptide, and serum electrolytes), radiological (point-of-care ultrasound or imaging) and advanced hemodynamic monitor may be used to diagnose and monitor overhydration. Various strategies to avoid and correct overhydration include fluid restriction and deresuscitation. Recent evidence supports the feasibility and safety of fluid restriction after initial resuscitation. Deresuscitation is defined as the active removal of excessive fluid using pharmacological or non-pharmacological measures and was coined during the 2011 International Fluid Academy meeting. A combination of diuretics, ultrafiltration, and fluid restriction, can be used for deresuscitation along with adequate monitoring to prevent hypoperfusion.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara IFA Commentary (SG)Fluid accumulation of more than 10% is associated with higher morbidity and mortality. However, fluid accumulation is a continuum, and a single threshold value does not encompass everyone. It is a state of pathological overhydration with worse patient outcomes. Organ dysfunction with fluid accumulation is defined as fluid accumulation syndrome. IV fluids should be regarded as drugs, and stewardship focusing on 4D’s (Drug, dose, duration, and de-escalation) is recommended to mitigate the problem of fluid accumulation. IV fluid prescription should consider four indications (resuscitation, maintenance, replacement, and nutrition) and the conceptual model of ROSE (resuscitation, optimization, stabilization, and evacuation). De-escalation and de-resuscitation are strategies to avoid fluid accumulation. Recent evidence supports the feasibility of fluid restriction during resuscitation. De-escalation means discontinuation or reducing IV fluids to prevent fluid accumulation. De-resuscitation is an active fluid removal to treat fluid accumulation causing organ dysfunction. Tools such as negative passive leg raising test, extravascular lung water and bioelectrical impedance, and venous congestion on point-of-care ultrasound are promising to guide de-resuscitation. Diuretics with or without hyper-oncotic albumin are the first step in de-resuscitation. Mechanical fluid removal (ultrafiltration) can be considered in case of diuretic failure or contraindication. The end-point of de-resuscitation are either goal-based (fluid balance, physiological or clinical improvement) or safety concerns.
The goal of fluid resuscitation is to improve tissue perfusion. However, overzealous resuscitation measures may lead to fluid overload and tissue edema, further worsening tissue and organ damage. The fluid overload state is compounded further by poorly planned maintenance fluid therapy and often avoidable ‘fluid creep’. Pathophysiology and clinical features of several fluid accumulation syndromes are described in this chapter in great detail. Below we will list some interventions that can be performed to prevent and treat FAS.
Avoid fluid accumulation: Key is to prevent fluid accumulation without allowing tissue hypoperfusion. We suggest the following strategies to achieve this goal.
-
Avoid large fluid boluses. Fluid bolus as small as 4 ml/kg body weight has shown to be adequate for intravascular volume expansion [1].
-
Further fluid boluses should be guided by patient phenotype e.g. history of large fluid loss or poor fluid intake in preceding days, obvious harm of further fluid administration e.g. pulmonary edema or B-profile in the anterior chest).
-
Fluid responsiveness must be checked before additional fluid boluses and fluid should not be administered if the patient is not fluid responsiveness. However, the converse may not be true [2].
-
Early initiation of vasopressors has been shown to reduce cumulative fluid balance in vasodilatory shock like septic shock [3]. Vasopressors (especially norepinephrine) should be administered along with fluid boluses in patients with diastolic blood pressure <50 mmHg or diastolic shock index >2.3 and after initial fluid volume of not more than 1–2 l of crystalloid [4–6].
-
Hyperoncotic albumin boluses have shown to reduce cumulative fluid volume during fluid resuscitation [7, 8]. However, additional data and cost-benefit ratio must be considered before the widespread adoption of this strategy.
-
Patients should be reassessed frequently during fluid resuscitation to look for improvement in tissue perfusion, as well as for any harmful consequences of administered fluid. In both situations, further fluid boluses must be stopped. In the ANDROMEDA-SHOCK trial, resuscitation targeting capillary refill time (CRT) as the end-point of tissue perfusion goal was shown to lower resuscitation volume compared to lactate guided resuscitation [9].
-
Maintenance fluid and fluid creep contribute to over 60% of administered fluid in critically ill patients [10]. Whenever possible maintenance fluid infusion should be either avoided or limited to the minimal volume. Similarly, ‘fluid creep’ should be actively looked into and whenever feasible patient can be switched to an oral (enteral) formulation or the drug should be diluted in a smaller volume.
-
Moderately hypotonic (sodium concentration 54 mmol/L) maintenance fluid infusion produces lower cumulative fluid balance compared to isotonic (sodium concentration 154 mmol/L) maintenance fluid [11]. Hence, if maintenance fluid is deemed to be necessary, the choice of fluid should be moderately hypotonic.
De-resuscitate when necessary: De-resuscitation is a strategy to remove accumulated fluid forcefully, in an otherwise hemodynamically stable patient with clinical evidence of fluid overload. The aim of de-resuscitation is to treat and/or prevent end-organ damage resulting from fluid overload without producing hypovolemia and organ ischemia. The following questions need to be raised and answered during the process of de-resuscitation [12].
-
When to start? Patient must be hemodynamically stable on no or minimal dose of vasopressors before considering de-resuscitation. He or she should not be requiring additional boluses or fluid or there should not be any ongoing fluid loss requiring replacement. Clinical and objective evidence of fluid overload should be present with reasonable suspicion of organ damage (or impending one) directly resulting from the fluid accumulation. Evidence of fluid overload has been described in great detail in the chapter.
-
How to initiate? Active removal of fluid can be achieved either by judicious use of diuretics or by ultrafiltration [continuous renal replacement therapy (CRRT) or slow low efficiency hemodialysis (SLED)]. Mechanisms of action and pharmacological effects of different diuretic agents have been discussed in the chapter. Discussion on CRRT and SLED techniques are beyond the scope of this book. Some relevant points on the subject are given below.
-
Berthelsen and colleagues suggested is to start de-resuscitation process with a 40 mg IV bolus of furosemide followed by an infusion titrated to a maximum dose of 40 mg/h [13]. Other loop diuretics such as torsemide may be considered in place of furosemide. Interestingly, in a large study on diuretic strategies in patients with acute decompensated heart failure, continuous infusion of furosemide was not shown to be of any additional advantage compared to bolus doses [14].
-
In a recent study, addition of intravenous acetazolamide 500 mg once daily in addition to standard loop diuretic regimen, was shown to achieve better decongestion and produce more diuresis and natriuresis compared to loop diuretic alone, in patients with acute decompensated heart failure [15]. Broader application of this combination strategy in general intensive care unit patients needs further evaluation.
-
Ultrafiltration using CRRT or SLED may be considered as alternative options in patients with inadequate response to diuretics or in anuric patients or in patients requiring renal replacement therapy for some other reason or in patients who developed serious adverse effects to furosemide or torsemide [12].
-
Adding hyperoncotic (20 or 25%) albumin to the diuretic and/or ultrafiltration regimen, in addition to maintaining intravascular volume, has been shown to produce synergistic effect [16]. In an elegant study, Greg Martin et al. randomized hemodynamically stable, hypoproteinemic patients who are on mechanical ventilator for ARDS to either furosemide with albumin (100 ml boluses of 20% albumin every 8-h) or furosemide with placebo for 72 h [16]. Addition of albumin was shown to produce larger negative fluid balance and lesser episodes of hypotension, in addition to a significant improvement in oxygenation. Alternatively, hyperoncotic albumin may be administered as a continuous infusion at 10–20 ml/h [12].
-
Addition of positive end-expiratory pressure (PEEP) matching intra-abdominal pressure (IAP), in addition to albumin plus diuretics (or ultrafiltration) (PAL strategy—PEEP, albumin and lasix or furosemide), had shown to be associated with greater negative fluid balance and greater reduction in extravascular lung water index (EVLWI) and IAP compared to control subjects [17]. PAL strategy also showed improved clinical outcomes (improved oxygenation, shorter ICU length of stay) without compromising cardiovascular or renal function.
-
-
How to monitor? Patients should be monitored closely for evidence of hypovolemia and/or hypoperfusion and adequacy of fluid removal [12].
-
One suggested goal is to achieve a net negative fluid balance of at least 1 mL/kg IBW/hour [13].
-
Patients should also be monitored for serious adverse effects of diuretics e.g. thrombocytopenia, agranulocytosis, pancreatitis, Steven Johnsons syndrome, toxic epidermal necrolysis, etc.
-
Patients should also be monitored for any electrolyte abnormalities (e.g. hypokalemia, dysnatremia, hypomagnesemia or hypophosphatemia) and cardiac arrhythmias related to it.
-
-
When to stop? De-resuscitation should be stopped, if the patient fulfills any of the following conditions.
-
Hemodynamic instability or obvious evidence of hypovolemia; in which case, fluid removal must be suspended and fluid may be re-administered judiciously. Fluid removal may be re-initiated at a lower rate, once hypovolemia or hypoperfusion is mitigated [12].
-
On achievement of de-resuscitation goal—negative or zero fluid balance.
-
Suggested Reading
-
1.
Aya H, Rhodes A, Grounds RM, Cecconi M. Minimal volume for a fluid challenge in postoperative patients. Crit Care. 2015;19(Suppl 1):P189.
-
2.
Ghosh S. Concept of fluid responsiveness. Fluid challenge. In: Handbook of intravenous fluids. Springer, Singapore, 2022. https://doi.org/10.1007/978-981-19-0500-1_9.
-
3.
Macdonald SPJ, Keijzers G, Taylor DM, Kinnear F, Arendts G, Fatovich DM et al. Restricted fluid resuscitation in suspected sepsis associated hypotension (REFRESH): a pilot randomised controlled trial. Intensive Care Med. 2018;44:2070–8.
-
4.
Karpati PCJ, Rossignol M, Pirot M, Cholley B, Vicaut E, Henry P et al. High incidence of myocardial ischemia during postpartum hemorrhage. Anesthesiology. 2004;100:30–6.
-
5.
Ospina-Tascón GA, Teboul JL, Hernandez G, Alvarez I, Sánchez-Ortiz AI, Calderón-Tapia LE et al. Diastolic shock index and clinical outcomes in patients with septic shock. Ann Intensive Care. 2020;10:41.
-
6.
Roberts RJ, Miano TA, Hammond DA, Patel GP, Chen JT, Phillips KM et al. Evaluation of vasopressor exposure and mortality in patients with septic shock. Crit Care Med. 2020;48:1445–53.
-
7.
Margarson MP, Soni NC. Changes in serum albumin concentration and volume expanding effects following a bolus of albumin 20% in septic patients. Br J Anaesth. 2004;92:821–6.
-
8.
Mårtensson J, Bihari S, Bannard-Smith J, Glassford NJ, Lloyd-Donald P, Cioccari L et al. Small volume resuscitation with 20% albumin in intensive care: physiological effects: The SWIPE randomised clinical trial. Intensive Care Med. 2018;44:1797–1806.
-
9.
Hernández G, Ospina-Tascón GA, Damiani LP, Estenssoro E, Dubin A, Hurtado J et al. Effect of a resuscitation strategy targeting peripheral perfusion status vs serum lactate levels on 28-day mortality among patients with septic shock: the ANDROMEDA-SHOCK randomized clinical trial. JAMA. 2019;321:654–64.
-
10.
Van Regenmortel N, Verbrugghe W, Roelant E, Van den Wyngaert T, Jorens PG. Maintenance fluid therapy and fluid creep impose more significant fluid, sodium, and chloride burdens than resuscitation fluids in critically ill patients: a retrospective study in a tertiary mixed ICU population. Intensive Care Med. 2018;44:409–17.
-
11.
Van Regenmortel N, Hendrickx S, Roelant E, Baar I, Dams K, Van Vlimmeren K et al. 154 compared to 54 mmol per liter of sodium in intravenous maintenance fluid therapy for adult patients undergoing major thoracic surgery (TOPMAST): a single-center randomized controlled double-blind trial. Intensive Care Med. 2019;45:1422–32.
-
12.
Ghosh S. Four phases of fluid resuscitation. In: Handbook of intravenous fluids. Springer, Singapore, 2022. https://doi.org/10.1007/978-981-19-0500-1_10.
-
13.
Berthelsen RE, Perner A, Jensen AK, Rasmussen BS, Jensen JU, Wiis J, Behzadi MT, Bestle MH. Forced fluid removal in intensive care patients with acute kidney injury: the randomised FFAKI feasibility trial. Acta Anaesthesiol Scand. 2018;62:936–44.
-
14.
Felker GM, Lee KL, Bull DA, Redfield MM, Stevenson LW, Goldsmith SR et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011;364:797–805.
-
15.
Mullens W, Dauw J, Martens P, Verbrugge FH, Nijst P, Meekers E et al. Acetazolamide in acute decompensated heart failure with volume overload. N Engl J Med. 2022;387:1185–95.
-
16.
Martin GS, Moss M, Wheeler AP, Mealer M, Morris JA, Bernard GR. A randomized, controlled trial of furosemide with or without albumin in hypoproteinemic patients with acute lung injury. Crit Care Med. 2005;33:1681–7.
-
17.
Cordemans C, De Laet I, Van Regenmortel N, Schoonheydt K, Dits H, Martin G, Huber W, Malbrain ML. Aiming for a negative fluid balance in patients with acute lung injury and increased intra-abdominal pressure: a pilot study looking at the effects of PAL-treatment. Ann Intensive Care. 2012;2(Suppl 1):S15.
This chapter will discuss the harms of excessive IV fluids administration and overhydration. Various strategies can be employed to avoid and monitor overhydration. Fluid restriction during resuscitation and active removal of excessive fluid, also known as deresuscitation, are the strategies employed to manage overhydration. We will review the recent evidence on fluid restriction and deresuscitation. With the help of a case, we will review the judicious fluid administration, methods of monitoring overhydration, and safe deresuscitation strategy in case of overhydration.
FormalPara Case VignetteA 26-year-old man was admitted to the ICU after general seizures, syncope, non-palpable blood pressure, and a suspicion of ventricular tachycardia whilst in the Emergency Room. The emergency room physician (successfully) applied a DC shock to convert to regular sinus rhythm. Afterward the patient was alert and cooperative and he was transferred to the ICU for overnight monitoring. The next day his need for supplemental oxygen increased from 2 l via nasal cannula to 15 l administered with a non-rebreathing mask. The patient was in respiratory distress with a respiratory rate of 34 breaths/min. After the failure of non-invasive ventilation, he was intubated and mechanically ventilated within 24 h after ICU admission, illustrating the dramatic chain of events. After intubation, the patient was in profound shock and resuscitated with 3 consecutive boluses of 4 ml/kg balanced crystalloids. Despite fluids and low dose pressors, he remained hypotensive with increasing lactate and poor P/F ratio (<100). Transpulmonary thermodilution monitoring was started. The initial hemodynamic profile showed a normal cardiac index (CI) of 3.5 L/min m2 (normal range 3–5), a relatively low intravascular filling status with a GEDVI of 757 ml/m2 (normal range 680–800), a very low global ejection fraction GEF of 13% (normal range 25–35) in combination with severe capillary leak and high extravascular lung water index (EVLWI) of 12 ml/kg predicted body weight (normal range 3–7). At the same time; however, the patient seemed to be preload responsive with a high pulse pressure variation (PPV) of 19% (normal range <10). Heart rate was regular at 119 beats/min with a MAP of 55 mmHg. The CVP remained at 16 mmHg. His response to a passive leg raising (PLR) maneuver was positive (15% increase in CI and MAP) confirming that he was volume responsive despite the fact that he was in pulmonary edema (EVLWI 12) with a critical oxygenation status at the time (P/F ratio of 57, at IPAP of 34 cmH2O and PEEP of 15 cmH2O).
Questions
-
Q1. What does this case scenario illustrate?
-
The patient was given a further small volume dose of fluids in combination with an increasing dose of vasopressors. The following day, his CI increased to 5.7 L/min m2, GEDVI increased to 900 ml/m2 but also EVLWI had increased to 19 ml/kg PBW. The high EVLWI was suggestive of hyperpermeability edema in view of the high pulmonary vascular permeability index (PVPI) of 2.9 (normal range 1–2.5).
-
Q2. What is the best treatment at this stage?
Introduction
The administration of intravenous (IV) crystalloid solutions is widely regarded as the initial step in resuscitating the hypotensive critically ill ‘septic’ patient, with evidence of inadequate organ perfusion. Recent evidence suggests that overzealous administration of IV fluids, especially in the setting of sepsis with poor source control and capillary leak, may lead to fluid overload and subsequent fluid accumulation syndrome (FAS) [1].
Tissue edema is not just of cosmetic concern, it impairs oxygen and metabolite diffusion, disrupts the endothelial glycocalyx architecture, impedes capillary blood flow and lymphatic drainage and disturbs intercellular interactions. All these effects may contribute to the progression of organ dysfunction and failure. These effects are particularly pronounced in encapsulated organs, such as the liver and kidneys, which lack the capacity to accommodate additional volume without an increase in interstitial pressure, resulting in compromised organ blood flow. Furthermore, large-volume resuscitation increases intraabdominal pressure (IAP) which further compromises end-organ (e.g. renal and hepatic) perfusion. This has led to new insights into polycompartment syndrome and more specifically, the cardio-abdominal-renal syndrome (CARS), hepato-abdominal pulmonary syndrome (HAPS) and the hepato-abdominal-renal syndrome (HARS) [2, 3].
Kelm et al. demonstrated that the majority (67%) of patients resuscitated with an early goal directed protocol, had clinical evidence of fluid accumulation after day 1, with 48% showing persistent signs of fluid overload by day 3 [4]. Multiple studies have demonstrated that a positive fluid balance is independently associated with impaired organ function and an increased risk of death [1].
This was neatly demonstrated in a retrospective study performed by Murphy and co-workers in septic patients [5]. It demonstrated that achieving just 2 consecutive negative fluid balance targets within the first week of an ICU stay (late conservative fluid management), was associated with improved organ function and survival. This has also been replicated in other reports [6, 7]. This dynamic time effect and impact of fluids was also illustrated by other data and has been referred to as the ebb and flow phases of shock. In 1932, Cuthbertson characterized the ebb phase as ‘ashen facies, a thready pulse and cold clammy extremities…’, while during the flow phase ‘the patient warms up, cardiac output increases and the surgical team relaxes…’ [8]. Recent data suggests that a substantial number of ICU patients will not enter the flow phase spontaneously after initial resuscitation or EGDT. In order to avoid fluid accumulation and the associated organ edema and dysfunction, these patients may require therapeutic interventions in order to trigger the transition from ebb phase to flow phase [9]. However, it remains largely unknown whether strategies that target a neutral or even negative fluid balance after the initial resuscitative phase are associated with improved clinical outcomes in humans.
The use of the correct definitions, as repeated in this chapter, may limit the deleterious effects of inappropriate fluid prescription and fluid accumulation [10]. We will focus on the deleterious effects of hyper- or overhydration (a better term for fluid overload) and fluid accumulation and will discuss restrictive and liberal fluid management strategies, as well as the different monitoring tools we can use to guide late goal-directed fluid removal, also termed deresuscitation [11]. The term deresucitation was coined in 2011 during the first International Fluid Academy Day (IFAD) meeting in Antwerp (https://www.fluidacademy.org/memberresources/item/extended-overview.html, congress proceedings page A30—Fig. 25.1) and later on in 2014, defined as active fluid removal in patients with fluid overload using drugs and/or ultrafiltration (UF) [1]. Recently a concise overview has been published [12].
Definitions
The introductory chapter contains a full compendium with a list of definitions and terms. Below, we will briefly discuss those terms related to fluid overload [13,14,15].
Classification of fluid dynamics: With respect to the different phases of fluid resuscitation (early vs. late), one can classify the dynamics of fluid management by combining early adequate (EA) or early conservative (EC) and late conservative (LC) or late liberal (LL) fluid management. Based on this theoretical concept, four distinct strategies can be defined: EALC, EALL, ECLC, ECLL. The EALC and ECLC groups carry the best prognosis.
Cumulative fluid balance: The sum of fluid accumulated by calculating the sum of daily fluid balances over a set period of time. Usually, the first week of a patient’s ICU stay is taken into account for prognostication.
Daily Fluid Balance: The difference between all fluids given to a patient during a 24-h period, and their combined output.
De-escalation: Reduction of the dose or speed of administration of fluid therapy following clinical improvement of the patient.
Deresuscitation (see also Late Goal-Directed Fluid Removal): Correction of fluid accumulation or fluid overload, by actively removing excess fluids using pharmacological and non-pharmacological methods.
Ebb phase: The initial phase of septic shock when the patient shows hyperdynamic circulatory shock, with decreased systemic vascular resistance due to vasodilation, increased capillary permeability, and severe absolute or relative intravascular hypovolemia.
Edema: Peripheral and generalized edema (anasarca) is not merely cosmetic, but harmful to the patient E:I ratio: the ECW/ICW ratio is normally below 1 (0.7–0.8). An increase in ICW% will result in a decrease in E:I ratio and is seen in heart failure, liver cirrhosis, and chronic renal failure patients, especially in the early stages. A decrease in ICW% will result in a decrease in E:I ratio and is generally due to osmotic factors. Finally, an increase in ECW% will also increase the E:I ratio. This occurs due to fluid shifts from the intra to extracellular space, or from the capillary leak, which results in second (interstitial) and third-space fluid accumulation and/or edema.
Flow phase: This refers to the phase of septic shock after initial stabilization, where the patient will mobilize excess fluid spontaneously; a classic example is when a patient enters a polyuric phase during recovery from acute kidney injury (AKI).
Fluid accumulation: A pathologic state of overhydration/volume overload, associated with clinical impact which may vary by age, comorbidity, and phase of illness. It describes a continuum and may occur with concomitant intravascular hypovolemia, normovolemia, and hypervolemia. It may or may not be associated with clinical or imaging signs of edema. No specific threshold of fluid balance alone can define fluid accumulation across all individuals.
Fluid accumulation syndrome: Any degree of fluid accumulation or fluid overload with a negative impact on end-organ function, which may or may not be associated with global increased permeability syndrome.
Fluid Creep: The unintentional and unmeasured fluid volumes administered in the process of delivering medication and nutrition through enteral and parenteral routes [16]. In patients with severe burns, this includes the administration of fluids in excess of any requirements calculated by the Parkland Formula [17].
Fluid overload (see overhydration): An increase in total body fluid (both water and electrolytes) in excess of physiologic requirements. This term has sometimes been used interchangeably with volume overload [18], which generally refers to expansion of the extracellular fluid volume.
Preload responsiveness: The state in which a patient will respond to fluid administration by an increase in stroke volume of 15%. This term should replace the traditional misnomer of ‘fluid responsiveness’.
Global increased permeability syndrome (GIPS): Some patients will not enter the ‘flow’ phase spontaneously and will remain in a persistent state of increased permeability and a tendency to fluid accumulation. This is referred to as ‘the third hit of shock’. It is defined by a positive cumulative fluid balance with organ failure, in the presence of capillary leak (e.g. increased EVLWI, PVPI, CLI, E:I ratio)
Hypervolemia: The opposite of hypovolemia, defined by intravascular overfilling.
Late Conservative Fluid Management (LCFM): Two consecutive days of negative fluid balance within the first week of the ICU stay; this is a strong and independent predictor of survival [5].
Late Goal-Directed Fluid Removal (LGFR): Active fluid removal by means of diuretics or renal replacement therapy with net ultrafiltration.
Overhydration (see also fluid overload and fluid accumulation): A state of positive fluid balance or where there is excess water in the body. Overhydration may be accompanied by a normal, low or high intravascular or interstitial fluid status, with or without (peripheral or lung) edema. An increase in intravascular fluid status will eventually also lead to increased interstitial fluid by hydrostatic pressure (i.e. cardiogenic edema). Dividing the cumulative fluid balance in liters by the patient’s baseline body weight and multiplying by 100% defines the percentage of fluid accumulation. Overhydration or hyperhydration at any stage can be classified as mild (5%), moderate (5–10%) or severe (>10%) fluid accumulation. Historically, it is often defined as increase in body weight relative to admission body weight
-
(Fluid intake during observation period)—(fluid losses during observation period)/pre-ICU body weight ×100 or
-
Actual increase in body weight (Pre-ICU admission body weight/body weight at the timepoint of fluid overload assessment ×100) or
-
Increase in fluid balance (cumulative fluid balance (in L)/pre-ICU body weight × 100) or increase in volume excess (calculated by BIA/pre-ICU body weight × 100) [19].
Positive Fluid Balance: A state in which fluid intake exceeds fluid output. An increase in net fluid balance with accumulation of excess fluids in body tissues and weight gain and in some cases, peripheral edema.
Pathophysiology
We often give too much IV fluid and in particular, too much non-physiological salt. Once within the body, such non-physiological excesses are very difficult to remove and can result in many adverse situations for our patients. There are extremes—increased fluid load can cause major electrolyte swings, whereas dehydration, left unchecked, can lead to poor organ perfusion.
Sick patients have ‘leaky capillaries’ and in this situation, even careful IV fluid administration can lead to fluid overload and resultant complications (ileus, poor mobility following peripheral edema, pressure sores, pulmonary edema, poor wound healing and anastomotic breakdown).
We have a situation whereby fluid has escaped from its beneficial site within the circulating volume, flooding the extracellular compartment, where it offers no physiological value. What these patients require, after sensible fluid challenges and identification of ‘non-response’ (better described as being ‘volume intolerant/preload un-responsive’). This is where the role of early therapy may now be prudent (i.e. noradrenaline).
Fluid administration potentially triggers a vicious cycle, where interstitial edema induces organ dysfunction, which in turn perpetuates fluid accumulation. It is now well-established that fluid overload in septic patients is associated with edema development and worse outcomes. Fluid overload affects all organ functions from head to toe. GIPS can hence be defined as fluid overload in combination with new-onset organ failure, in the setting of persistent capillary leak (Fig. 25.2).
Potential adverse consequences of fluid overload on end-organ function. Adapted from Malbrain et al. with permission [20]. APP abdominal perfusion pressure, IAP intra-abdominal pressure, IAH intra-abdominal hypertension, ACS abdominal compartment syndrome, CARS cardio-abdominal-renal syndrome, CO cardiac output, CPP cerebral perfusion pressure, CS compartment syndrome, CVP central venous pressure, GEDVI global enddiastolic volume index, GEF global ejection fraction, GFR glomerular filtration rate, ICG-PDR indocyaninegreen plasma disappearance rate, ICH intracranial hypertension, ICP intracranial pressure, ICS intracranial compartment syndrome, IOP intra-ocular pressure, MAP mean arterial pressure, OCS ocular compartment syndrome, PAOP pulmonary artery occlusion pressure, pHi gastric tonometry, RVR renal vascular resistance, SV stroke volume
The following list describes the potential detrimental effects of fluid overload on end-organ function:
-
Central nervous system: impaired cognition, delirium, increased intracranial, intra-orbital, and intra-ocular pressure, cerebral edemaand diminished cerebral perfusion pressure. A study of 35 brain injured pigs, with and without hemorrhagic shock, were randomized to Liberal (LR) vs restrictive fluid (HLS). Cerebral edema formation, as indicated by cortical water content (gravity), was studied after 24 h. The study showed that the volume of fluid infused and the fluid balance did affect the ICP, but the amount of Na infused did not [21]. In a retrospective study of 28 severe burn and trauma patients, 8 out of 28 patients required orbital decompression because of increased intra-orbital pressure, related to the amount of fluids administered [22].
-
Respiratory system: pulmonary edema, pleural effusions, increased chest wall elastance, decreased dynamic and static respiratory compliance, increased extravascular lung water index, increased pulmonary vascular permeability index, hypercarbia, hypoxia, low P/F ratio, decreased lung volumes (mimicking restrictive lung disease cf. increased intra-abdominal pressure), prolonged ventilation, difficult weaning, and increased work of breathing. In the FACTT trial, 1000 patients with acute lung injury were randomized to receive either conservative vs. liberal fluid treatment. Patients in the conservative arm had a significantly less positive cumulative fluid balance after 1-week, improved lung function and shorter duration of mechanical ventilation [6].
-
Cardiovascular system: myocardial edema, pericardial effusion, conduction disturbance, impaired contractility, diastolic dysfunction, increased filling pressures (central venous and pulmonary artery occlusion pressure), diminished venous return (cf. increased IAP), decreased stroke volume and cardiac output, myocardial depression, decreased stroke volume and pulse pressure variation, venous congestion, low (global) ejection fraction, increased volumetric preload indicators (e.g. global end-diastolic volume index), and cardio-abdominal-renal interactions [23]. A study in 25 dogs examining the effect of induced myocardial edema (via progressive pulmonary artery banding), showed an inversion relationship between interstitial fluid pressure and cardiac compliance [24].
-
Renal system: renal interstitial edema, increased renal venous and interstitial pressure, decreased renal blood flow and glomerular filtration rate, increased renal vascular resistance, renal venous congestion, increased or decreased (hemodiluation) creatinine, increased uremia, salt and water retention, and local renal compartment syndrome. A study in 296 critically ill patients treated with RRT, showed that patients with fluid overload at RRT initiation had double the crude 90-day mortality compared to those without. Fluid overload was associated with increased risk for 90-day mortality even after adjustments [25].
-
Gastrointestinal system: gut and bowel edema, diminished bowel contractility, increased ileus and malabsorption, diminished hepatosplanchnic perfusion (low ICG-PDR), ascites formation, increased intra-abdominal pressure and decreased abdominal perfusion pressure, abdominal hypertension, abdominal compartment syndrome, increased intestinal permeability and bacterial translocation [26].
-
Hepatic system: diminished liver perfusion, decreased lactate clearance, hepatic venous congestion, local hepatic compartment syndrome.
-
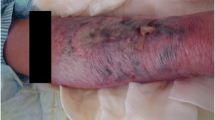
Abdominal wall and skin: tissue edema, poor wound healing, increased wound infections and pressure ulcers, decreased abdominal and chest wall compliance.
Particular attention should be paid to patients at high risk of overhydration e.g. those with cardiac, renal, hepatic failure, and nutritional disorders.
Liberal Versus Restrictive Fluid Regimens
As intravascular underfilling and hypovolaemia are the most prevalent reversible causes of shock, a ‘liberal’ fluid approach with repetitive administration of intravenous fluid boluses until the patient no longer responds with improvement in cardiovascular dynamics (i.e. without increase in mean arterial pressure, central venous pressure, urine output, or cardiac output), is common [27]. This approach is proposed in many international guidelines for the initial management of sepsis such as the NICE, GIFTASUP, ESICM, and SCCM [28, 29]. However, there is no strong rationale for this approach, as the physiological effects of fluid boluses given in ICU appear to be small and short-lived.
Administration of large volumes of intravenous crystalloid fluids often leads to accumulation of a positive fluid and sodium balance. Fluid accumulation and overhydration in critically ill patients, defined by a 10% increase in cumulative fluid balance from baseline body weight, is consistently associated with worse outcomes. This has been shown in broad populations of children and adults with sepsis, acute kidney injury, acute respiratory failure as well as general critical illness. However, this association may not indicate a causal relationship, since severely ill patients are more prone to receiving larger volumes of IV fluids. An interesting question is whether the deleterious effects are related to fluid or sodium accumulation, or both. It is clear that overhydration has extended effects on vascular integrity and permeability, and may trigger ongoing inflammation leading to a vicious cycle (GIPS). Hemodilution, venous congestion, decreased perfusion pressures, increased compartmental pressures (especially in the abdomen and thorax) and interstitial edema further impact on oxygen delivery and diffusion to the tissues. Finally, this may damage the endothelial glycocalyx, a fragile barrier by which fluid is maintained within the intravascular space. Rapid fluid boluses of salt solutions have worse effects on glycocalyx integrity, compared to slow infusion of albumin, the latter having a protective effect.
The FACCT trial, studying 1000 patients with acute lung injury, showed that although there was no significant difference in the primary outcome of 60-day mortality, a conservative strategy of fluid management improved lung function and shortened the duration of mechanical ventilation and intensive care, without increasing non-pulmonary organ failure [6].
As stated above, Murphy and colleagues showed that early adequate fluid therapy in combination with late conservative fluid management, carried the best prognosis in a retrospective study of 212 patients with ALI complicating septic shock [5].
A recent systematic review involving a total of 19577 critically ill patients [1] found that the cumulative fluid balance after 1 week of ICU stay was 4.2 l more positive in non-survivors compared to the survivors (95% CI 2.7–5.6, p < 0.0001). A restrictive fluid regimen resulted in a less positive cumulative fluid balance of 5.6 l (95% CI 3.3–7.7, p < 0.0001) compared to controls with liberal fluid regimen, after 1 week of ICU stay. Restrictive fluid management was associated with a reduction in ICU mortality from 33.2% to 24.7% when compared to patients treated with a more liberal fluid management strategy (OR of 0.42; 95% CI 0.32–0.55, p < 0.0001).
Silversides et al. showed in a recent meta-analysis in adults and children with acute respiratory distress syndrome, sepsis or systemic inflammation (formerly called SIRS), that a conservative or deresuscitative fluid strategy results in an increased number of ventilator-free days and a decreased length of ICU stay compared with a liberal strategy or standard care, although the effect on mortality remained uncertain [30].
The CLASSIC pilot study examined the feasibility of a protocol restricting fluids in 151 patients after initial resuscitation for septic shock [31]. The protocol successfully reduced volumes of resuscitation fluids compared with a standard care protocol. The patient-centred outcomes pointed towards a benefit of fluid restriction, however the trial was underpowered.
In a retrospective cohort study RADAR, investigating the role of active deresuscitation after resuscitation, Silversides et al. found that a negative fluid balance achieved with deresuscitation on day 3 of ICU stay, was associated with improved outcomes [32]. The authors concluded that avoiding and / or minimizing maintenance fluid intake and drug diluents, in combination with deresuscitative measures, represent a potentially beneficial therapeutic strategy that merits investigation in randomized trials.
Although we must also advise caution against the development of hypovolemia (and hypernatremia) and the potential danger of hypoperfusion resulting from aggressive deresuscitation. Indeed, the argument in favour of restrictive fluid therapy is at present mainly based on small physiological observations and studies, and there are, on the other hand, also studies showing the potential harmful effects of restrictive fluid strategy in critically ill patients.
The use of a conservative fluid management approach has been called into question by the long-term follow-up of a subset of survivors of the Fluid and Catheter Treatment Trial (FACTT) [33]. A post-hoc analysis showed that cognitive function was markedly impaired in the conservative fluid group compared with the liberal fluid group, with an adjusted odds ratio of 3.35. Cognitive impairment was defined as impairment in memory, verbal fluency, or executive function. Although all these were more common in the conservative fluid management group, only the deterioration in executive function reached statistical significance (p = 0.001) [33].
The best daily target fluid balance needs a balanced view, especially in light of the results of the RELIEF study [34]. In this pragmatic trial, 3000 patients at increased risk for complications during major abdominal surgery, were randomized between a restrictive vs. more liberal fluid strategy. The authors found that whilst a restrictive regimen was not associated with a higher rate of disability-free survival than a liberal fluid regimen, it was associated with a higher rate of acute kidney injury, more RRT and more surgical site infections.
The RADAR-2 pilot study in 180 critically ill patients showed that a strategy of conservative fluid administration and active deresuscitation is feasible, reduces fluid balance compared with usual care but may cause benefit or harm [35]. Deciding when to start and stop deresuscitation is key to improving patient outcomes; research is ongoing to identify the best parameters to guide fluid removal in critically ill patients.
Results of the CLASSIC trial have been published. The study enrolled 1554 critically ill patients (770 were assigned to the restrictive-fluid group and 784 to the standard-fluid group). Primary outcome data were available for 1545 patients (99.4%) [36]. Patients received a median of 3 liters of intravenous fluid before they underwent randomization and were enrolled within 3 h after admission to the ICU. In the ICU, the restrictive-fluid group received a median of 1798 ml of intravenous fluid (interquartile range, 500 to 4366); the standard-fluid group received a median of 3811 ml (interquartile range, 1861–6762). At 90 days, mortality was the same in both groups as were the number of serious adverse events that occurred at least once. Although underpowered, this study supports a strategy of limiting any post-resuscitation fluid to patients who are either preload responsive or volume tolerant, using dynamic indices of preload responsiveness, as was recommended previously by other available data from the FEAST [37] and FACTT trials [33].
More recently the CLOVERS trial showed that among patients with sepsis-induced hypotension, the use of the restrictive fluid strategy did not result in a significant difference in mortality before discharge home by day 90 when compared to the liberal fluid strategy [38]. The CLOVERS study enrolled 1563 patients, with 782 assigned to the restrictive fluid group and 781 to the liberal fluid group. Resuscitation therapies varied between the groups, with less intravenous fluid given to the restrictive fluid group compared to the liberal fluid group (difference of medians, −2134 ml; 95% confidence interval [CI], −2318 to −1949). The restrictive fluid group also had more prevalent and longer duration of vasopressor use. Death from any cause before discharge home by day 90 occurred in 14.0% of patients in the restrictive fluid group and 14.9% in the liberal fluid group (estimated difference, −0.9% points; 95% CI, −4.4 to 2.6; P = 0.61). The number of serious adverse events reported was similar in both groups.
While waiting for the results of the full RADAR-2 trial, prevention of fluid accumulation and de-escalation of fluid therapy remain the most effective strategies to avoid deresuscitation [12, 35, 39].
Monitoring Hypervolemia and Guiding Deresuscitation
The renewed concept of ‘fluid stewardship’ [10], analogous to antibiotic stewardship, focusses on the 4 D’s (drug, dose, duration, and de-escalation), the 4 questions (when to start and when to stop fluid therapy, and when to start and when to stop fluid removal), the 4 indications (resuscitation, maintenance, replacement, and nutrition), and the conceptual ROSE model describing 4 fluid phases (resuscitation, optimization, stabilization, and evacuation [13]. Figure 25.3 illustrates the 4 dynamic fluid phases and gives some suggestions regarding triggers and safety limits in each phase.
The 4 phases conceptual model and deleterious effects of fluid accumulation syndrome. Graph showing the four-hit model of shock with evolution of patients’ cumulative fluid volume status over time during the five distinct phases of resuscitation: Resuscitation (R), Optimization (O), Stabilization (S), and Evacuation (E) (ROSE), followed by a possible risk of Hypoperfusion in case of too aggressive deresuscitation. On admission patients are often hypovolemic, followed by normovolemia after fluid resuscitation (escalation or EAFM, early adequate fluid management), and possible fluid overload, again followed by a phase returning to normovolemia with de-escalation via achieving zero fluid balance or late conservative fluid management (LCFM) and followed by late goal directed fluid removal (LGFR) or deresuscitation. In case of hypovolemia, O2 cannot get into the tissue because of convective problems, in case of hypervolemia O2 cannot get into the tissue because of diffusion problems related to interstitial and pulmonary edema, gut edema (ileus and abdominal hypertension). Adapted from Malbrain et al. with permission, according to the Open Access CC BY Licence 4.0 [13]. * volumetric preload indicators such as GEDVI, LVEDAI, or RVEDVI are preferred over barometric ones such as CVP or PAOP. ** vasopressor can be started or increased to maintain MAP/APP above 55/45 during deresuscitation phase. # can only be measured via Swan-Ganz pulmonary artery catheter (PAC) and became obsolete. APP abdominal perfusion pressure (APP = MAP-IAP), BIA bio-electrical impedance analysis, CI cardiac index, CLI capillary leak index (serum CRP divided by serum albumin), COP colloid oncotic pressure, CVP central venous pressure, EAFM early adequate fluid management, ECW/ICW extracellular/intracellular water, EVLWI extravascular lung water index, FAS fluid accumulation syndrome, GEDVI global end-diastolic volume index, GIPS global increased permeability syndrome, IAP intra-abdominal pressure, ICG-PDR indocyanine green plasma disappearance rate, IVCCI inferior vena cava collapsibility index, LCFM late conservative fluid management, LGFR late goal-directed fluid removal, LVEDAI left ventricular end-diastolic area index, MAP mean arterial pressure, PAOP pulmonary artery occlusion pressure, PF PaO2 over FiO2 ratio, PLR passive leg raising, PPV pulse pressure variation, PVPI pulmonary vascular permeability index, RVEDVI right ventricular end-diastolic volume index, ScvO2 central venous oxygen saturation, SSCG surviving sepsis campaign guidelines, SvO2 mixed venous oxygen saturation, SVV stroke volume variation, VE volume excess (from baseline body weight), VExUS venous congestion by ultrasound
Clinical Signs of Hypervolemia
The absence of thirst may indicate potential overhydration, but is not very specific. Clinical signs of overhydration should be sought during physical examination, as there is a ubiquitous bias in the direction of hypovolaemia detection. These include vital signs such as increased blood pressure (mean, systolic pressure, diastolic pressure, and pulse pressure), decreased pulse rate, increased central and jugular venous pressure, and absence of orthostatic hypotension and absence of preload responsiveness. Other signs are altered mental status, increased hepatojugular reflux, orthopnea, second and third space fluid accumulation, altered capillary refill time (usually less than 2 s), increased skin turgor, altered peripheral temperature, peripheral pitting edema and anasarca, and a positive daily and cumulative fluid balance. Also, the presence of pulmonary rales or crackles are rather non-specific signs. Many of these signs are subtler, and may not be routinely looked for. Deresuscitation should not solely be based on these non-specific signs. Daily weighing of patients in the ICU is very useful, but unfortunately not routinely used. Increased urine output (regularly checked in ICU patients) can be present (e.g. in polyuric phase after acute tubular necrosis), but depends on many variables and therapeutic interventions. Some advocate the use of a furosemide stress test to identify the risk for acute kidney injury (AKI), or the readiness for deresuscitation. Figure 25.4 summarizes the clinical signs and symptoms related to hypervolemia and fluid accumulation.
Clinical signs and symptoms related to hypervolemia and fluid accumulation. CVP central venous pressure, DAP diastolic arterial blood pressure, FR preload responsiveness, GRV gastric residual volume, HJR hepato-jugular reflux, HR heart rate, JVP jugular venous pressure, MAP mean arterial blood pressure, Na sodium, PLR passive leg raising, RSB rapid shallow breathing, SAP systolic arterial blood pressure, SMA superior mesenteric artery
Laboratory Signs and Biomarkers
Laboratory parameters, although useful, cannot provide independent biomarkers of volume status (Fig. 25.5). Arterial blood gas analysis can be readily obtained and provides a quick estimation of hemoglobin and pO2. There are reports regarding the relationship between hypervolemia and hemoglobin or hematocrit levels, and it is widely accepted that in states of overhydration, hemoglobin levels will be lower than normal due to the effects of hemodilution [40]. In case of fluid overload, extravascular lung water may also increase. This will be discussed further (related to either hyperpermeability or hydrostatic pulmonary edema), resulting in hypoxia, which in combination with anemia may further contribute to the imbalance between oxygen delivery and consumption. This process of hemodilution is however, subject to confounders (e.g., anemia, blood loss, toxic effect of infection). Renal function can be significantly impaired in states of hypervolemia. The impact of temporary decreased renal perfusion due to venous congestion appears to rely predominantly on the pre-existing physiological condition of the kidneys. Plasma sodium is of specific interest in volume regulation. It is easily measured by point-of-care tests and is strongly associated with volume status. Many patients with hypervolemia and a net fluid gain will develop hyponatremia. However, when the different baroreceptors of the body sense hypervolemia, the secretion of antidiuretic hormone by the pituitary gland is decreased.
Laboratory, imaging, hemodynamic and organ function signs and symptoms related to hypovolemia and hypoperfusion. Total body water accounts for 70% of body weight. Overt signs and symptoms of hypovolemia occur when circulating blood volume is reduced by more than 50%. AKI acute kidney injury, APP abdominal perfusion pressure, BIA bio-electrical impedance analysis, BNP brain natriuretic peptide, BVI blood volume index, CARS cardio-abdominal-renal syndrome, CBV circulating blood volume, CI cardiac index, CLI capillary leak index, COP colloid oncotic pressure, CRP C-reactive protein, CVP central venous pressure, ECW extracellular water, EIT electrical impedance tomography, EEO end-expiratory occlusion, EVLWI extravascular lung water index, FR preload responsiveness, GEDVI global end-diastolic volume index, GEF global ejection fraction, GIPS global increased permeability syndrome, HR heart rate, IAP intra-abdominal pressure, ICW intracellular water, IVC inferior vena cava, IVCCI inferior vena cava collapsibility index, LVOT left ventricular outflow tract, MAP mean arterial blood pressure, Na sodium, P/F ratio pO2 over FiO2 ratio, PAOP pulmonary artery occlusion pressure, PLR passive leg raising, PPV pulse pressure variation, PVPI pulmonary vascular permeability index, Qs/Qt shunt fraction, RAAS renin angiotensin aldosterone system, RPP renal perfusion pressure, RVEDVI right ventricular end-diastolic volume index, RVEF right ventricular ejection fraction, ScvO2 mixed central venous oxygen saturation, SPV systolic pressure variation, SVV stroke volume variation, TBW total body water, TTE transthoracic echocardiography, US ultrasound, VExUS venous excess by ultrasonography score, V/Q ventilation/perfusion, VTI velocity time integral, Vt/Vd dead space ventilation
As a consequence, there will be less retention of water, resulting in increase in sodium levels. Sodium values are also confounded by medication (e.g. diuretics), the type of fluids administered (e.g. saline solutions for resuscitation), the phase of fluid therapy (e.g. use of hypertonic lactated saline for deresuscitation), adrenal activity (renin angiotensin aldosterone system), and choice of replacement fluid (isotonic vs hypotonic). Hypervolemic hyponatremia in cirrhosis patients is characterized by a pronounced deficit of free water excretion and leads to inappropriate water retention in comparison with the sodium concentration. This imbalance results in an expanded extracellular volume and dilutional hyponatremia. Plasma osmolality (normal around 287 mOsm/kg) can be decreased in cases of hypervolemia, although the body will try to regulate osmolality within normal limits. Overhydration may result in extracellular fluid accumulation and also cellular hydration depending on the type of accumulating fluids. Osmolality is mainly influenced by the non-soluble fraction of the extra-cellular fluid compartment, namely elevated concentrations of serum lipids or proteins. Many medications (e.g. diuretics, mannitol) will affect the osmolality. The plasma colloid oncotic pressure (COP) is normally around 20–25 mmHg. In overhydrated patients with sepsis, the COP value may decrease below 16 mmHg. COP values are related to left ventricular filling pressures and may help in the differential diagnosis of pulmonary edema. COP is increased in hydrostatic edema and associated with increased filling pressures, whereas in hyperpermeability edema, COP is usually decreased. As such, COP measurement can be used for the differential diagnosis of pulmonary edema (hydrostatic vs hyperpermeability). Overhydrated patients may also show lower total protein and decreased albumin levels. The measurement of BNP levels can be a useful adjunct when in doubt as to the potential cause of hypervolemia. Low BNP levels have a high negative predictive value for the exclusion of heart failure as a diagnosis. On the other hand, high BNP levels can be non-specific for volume or fluid overload. The ANP-over-BNP ratio may be indicative of chronic congestive heart failure and fluid overload.
We often look at urine output as a marker of fluid requirement, however patients who are unwell, have suffered trauma, or have undergone surgery often have a reduced urine output due to increased sodium retention (and thus water), by the kidneys. This is an evolutionary stress response geared to the preservation of intravascular volume, in order to maintain vital organ perfusion during such stress states. Stress-induced (‘inappropriate’) anti-diuretic hormone secretion, as well as intrinsic vasopressor hormone secretion, leads to a state of sodium retention and potassium loss in the urine. The patient becomes edematous, hypokalemic and hypernatremia over time, if left unchecked. If normal saline has been given as a resuscitation fluid or maintenance fluid, the potential situation of hyperchloremic metabolic acidosis can ensue, on top of these other electrolyte imbalances.
Radiological and Imaging Signs
Fluid accumulation can be characterized by an abnormal chest X-ray that shows cardiomegaly, dilated upper lobe vessels, interstitial edema, enlarged pulmonary artery, alveolar edema, prominent superior vena cava, increased cardiothoracic ratio (>0.55), presence of Kerley-B lines or pleural effusion (Fig. 25.5). The utility of lung ultrasound offers a greater diagnostic sensitivity and specificity profile over plain radiography of the chest. Moreover, portable chest X-ray, reduces the sensitivity of findings of volume overload, with pleural effusions regularly being missed if the film is performed supine or in intubated patients [41]. Abdominal ultrasound may show 2nd and 3rd space fluid accumulation with edematous abdominal wall, bowel edema, or presence of ascites [42]. Transthoracic cardiac ultrasound may also be highly useful demonstrating increased E/e′ on tissue Doppler imaging and the absence of left ventricular outflow tract (LVOT) velocity time integral (VTI) variations. Care must be taken over reliance upon on the spot IVC measurements to ascertain volaemic status. Extremes of measurement may be more useful. If there is a complete collapse, in conjunction with an empty, hyperdynamic LV, then the patient is likely to be hypovolaemic. The converse is also true, where a plethoric IVC >2.5 cm is present, with little to no collapse at all, pointing to hypervolemia. There may be other causes of an enlarged IVC to exclude however; large PE, cardiac tamponade, severe tricuspid regurgitation, high PEEP, presence of autoPEEP, increased IAP, noninvasive ventilation, assisted spontaneous breathing, right ventricular dysfunction, right ventricular infarction, low tidal volume or respiratory tidal variation, mechanical obstruction [43]. Low IVCCI (<25%) has been quoted as a useful parameter, but only in ventilated patients and the short axis view is the preferred, more reliable measurement modality. Increased left atrium volume (LA >34 ml/m2) and lung ultrasound, may show B-lines and comet tail artifacts [44, 45]. The importance of venous congestion in the development of organ failure (and especially AKI), in fluid overload, can possibly explain the greatest improvement of renal function after medical treatment for advanced heart failure. This is particularly the case in patients with the echocardiographic signs of right ventricular dysfunction on the inferior vena cava, the portal, hepatic, and renal veins [46, 47] (Table 25.1). To analyse and objectively measure this, the VExUS score (venous excess by ultrasonography) has been suggested (Fig. 25.6) [47].
Advanced Hemodynamic Monitoring
These clinical, biochemical, and radiological parameters are rather non-specific. Hemodynamic assessment of fluid accumulation syndrome includes the absence of preload responsiveness, with a negative passive leg raise test (Fig. 25.7) or end-expiratory occlusion test. Also low functional hemodynamic parameters (PPV, SVV), low systolic pressure variation with normal delta up and delta down, increased MAP, SAP, and DAP, and barometric preload indicators (CVP or PCWP), increased volumetric preload parameters (like global or right ventricular end diastolic volume index; Fig. 25.5).
The passive leg raising (PLR) test can also be used to assess the absence of preload responsiveness. In order to perform a correct PLR test, one should not touch the patient in order to avoid sympathetic activation. The PLR is performed by turning the bed from the starting position (head of bed elevation 30–45°) to the Trendelenburg position. The PLR test results in an autotransfusion effect via the increased venous return from the legs and the splanchnic mesenteric pool. Monitoring of stroke volume is required as a positive PLR test is defined by an increase in SV by at least 10%. See text for an explanation. Adapted from Hofer C, Cannesson M. with permission [49]
In critically ill patients treated with renal replacement therapy (RRT), the absence of preload dependence pre-RRT, as assessed by a negative PLR test, was found to be a predictor that fluid removal during RRT would not induce hemodynamic instability [50]. Volumetric preload parameters are superior to barometric parameters, especially if ITP, IAP or PEEP are increased, but correction of these parameters by measures of ejection fraction, can further improve their ability to assess changes in preload over time, as was shown in an heterogeneous group of critically ill patients [51]. The impact of FAS on organ function can be assessed by examining thyroid and adrenal function, looking for signs for polycompartment syndrome (increased IAP, ICP, low APP), gastric distension, gastroparesis or increased GRV, increased EVLWI, PVPI, drop in P/F ratio and ORI, decreased ICG-PDR, and presence of AKI or CARS. With a cut-off value of 3, the pulmonary vascular permeability index (PVPI), calculated by transpulmonary thermodilution, allows to discriminate hydrostatic from hyperpermeability pulmonary [52]. In the future, some new and less invasive technologies will become readily available at the bedside. For example bio-electrical impedance analysis with calculation of TBW, ECW/ICW ratio, EVF/IVF ratio, volume excess [19] and BIVA hyperhydration [53], calculation of blood volume index with dye densitometry [54] or total circulating BV with albumin marked isotope dilution [55], or ventilation perfusion (mis)match with EIT [56].
Use of a protocol including BV analysis resulted in a 66% reduction in mortality, a 20% reduction in LOS, 36 h earlier treatment decisions, 44% change in treatment strategy [55]. Fluid overload, defined as a 5% increase in volume excess (measured with BIA) from baseline body weight, was associated with increased mortality in a retrospective study of 101 critically ill patients [19].
How to Perform Deresuscitation?
While more restrictive use of fluid, together with earlier use of vasopressors if needed, may reduce fluid administration, it is unlikely that fluid overload can be entirely avoided using this strategy [27]. Fluid intake in ICU comes from a range of sources, many obligate such as drug diluents and nutrition. A recent study showed that this ‘fluid creep’ accounts for as much as 33% of all fluid intake compared to around 7% for resuscitation fluids [16]. As well as restriction of fluid resuscitation, avoidance of fluid overload is therefore likely to require deresuscitation, with active fluid removal using diuretics or ultrafiltration [1], an approach that likely shortens the duration of mechanical ventilation and ICU stay [30]. Measures to remove excess fluid include drugs and UF, combined with fluid restriction.
Provided some kidney function is preserved, diuretics are usually tried first, either as monotherapy or in combination. The options include loop diuretics (furosemide, bumetanide), carbonic anhydrase inhibitor (acetazolamide), mineralocorticoid receptor antagonist (spironolactone), thiazides or thiazide-like drugs (indapamide). In case of low serum albumin levels (<30 g/L) or low serum total protein levels (<60 g/L) co-administration of hyperoncotic albumin 20% can be added for synergistic effect along with diuretics and may promote hemodynamic stability [57]. Increased EVLWI and failure to lower EVLWI resulted in poor outcomes in 123 critically ill patients with increased mortality and longer duration of ventilation. A drop in EVLWI was associated with late conservative fluid management and being preload responsive (less positive cumulative fluid balance) [58]. The combination of PEEP (in cmH2O, set at the level of IAP in mmHg), followed by albumin 20% (up to albumin levels of 30 g/L) and furosemide (or PAL-treatment) resulted in a negative cumulative fluid balance, a reduction of EVLWI and IAP, with improved clinical outcomes in a matched cohort of 114 critically ill patients with hyperpermeability pulmonary edema [59]. In 11 critically ill patients, RRT with 1.9 l net fluid removal was able to lower IAP, EVLWI, and GEDVI significantly [60] (Table 25.2).
Case Vignette
-
Q1. Does this patient have overhydration?
-
A1. Yes, moderate overhydration.
-
Overhydration (or hyperhydration) = body weight relative to admission body weight/pre-ICU body weight × 100
-
(4.9/67) × 100 = 7.3%
-
Q2. Would you consider fluid removal in this patient (deresuscitation), and how?
-
A2. Yes, given indicators of overhydration. An initial attempt with diuretics along with hyperoncotic albumin (if serum albumin is <30 g/L) can be attempted to induce diuresis. Using RRT for ultrafiltration can be tried in case of AKI or non-responder to diuretics.
Conclusions
No patient should suffer the effects of cellular dysfunction and ultimately multi-organ dysfunction, as a result of excessive IV fluid administration. Armed with an understanding of fluid physiology, one can see why oliguria is a poor marker of overall volaemic status. Physiological oral fluids should always be first line, unless circumstances absolutely disallow it.
The best fluid is probably the one that has not been given…(unnecessarily) [11]
Back to the case vignette; where we followed a patient, who developed shock within 18 h of ICU admission. Despite initial normal (and thus adequate) filling pressures, further fluid resuscitation was needed to overcome the ebb phase (this was guided by functional hemodynamic parameters, passive leg raising test and volumetric preload indices). However, at the very early stage of shock despite the fact that the patient was preload responsive, lung water was already increased. This is the classic example of a therapeutic dilemma which is a condition in which each therapeutic option (either fluid administration or fluid removal), may cause potential harm. Fluids are a double-edged sword. After initial further fluid resuscitation, diuretics were initiated after 24 h to help the patient transgress to the flow phase because of respiratory failure due to capillary leak, as evidenced by increased extravascular lung water. Based on barometric preload indicators, most physicians would be reluctant to start initial fluid resuscitation, therefore advanced monitoring may be indicated, especially in situations with changes in preload, afterload or contractility. This case nicely demonstrates the biphasic clinical course from ebb to flow during shock as well as the inability of traditional filling pressures, to guide us through these different phases. It also illustrates the four crucial questions that need to be solved in order not to cause harm. Therefore, it is important to know and understand:
-
1.
When to start giving fluids (low GEF/GEDVI, high PPV and positive PLR, increased lactate)
-
2.
When to stop giving fluids (high GEF/GEDVI, low PPV, negative PLR, normalized lactate)
-
3.
When to start removing fluids (high EVLWI, high PVPI, raised IAP, low APP defined as MAP minus IAP, positive cumulative fluid balance, absence of preload responsiveness).
-
4.
When to stop fluid removal (low ICG-PDR, low APP, low ScvO2, neutral to negative cumulative fluid balance, hypovolemia with hypoperfusion).
However, one must realize that the thresholds for the above-mentioned parameters are dynamic targets with dynamic goals (from early adequate goal-directed therapy, over late conservative fluid management towards late goal-directed fluid removal). And above all, one must always bear in mind that unnecessary fluid loading may be harmful. If the patient does not need fluids, don’t give them, and remember—the best fluid may be the one that has not been given to the patient!
Take Home Messages
-
Tissue edema in ICU patients results from overzealous fluid administration and/or capillary leaks and may lead to worse outcomes.
-
Overhydration affects multiple organs and is independently linked to organ failure and mortality.
-
The clinical, laboratory, and radiological signs of overload are non-specific.
-
Hemodynamic tools like the absence of fluid responsiveness by negative PLR, EEO, low functional hemodynamic variables (SVV, SPV, PPV), increased volumetric (GEDV, RVEDV) or barometric preload indicators (CVP, PAWP) can be used to diagnose and monitor overhydration.
-
Evidence supports the feasibility and safety of restrictive fluid administration during resuscitation.
-
Deresuscitation defined as an active removal of excessive fluid using diuretics and/or ultrafiltration, combined with fluid restriction may be considered in selected patients with overhydration.
References
Malbrain ML, Marik PE, Witters I, Cordemans C, Kirkpatrick AW, Roberts DJ, Van Regenmortel N. Fluid overload, de-resuscitation, and outcomes in critically ill or injured patients: a systematic review with suggestions for clinical practice. Anaesthesiol Intensive Ther. 2014;46(5):361–80.
Malbrain M, Wilmer A. The polycompartment syndrome: towards an understanding of the interactions between different compartments! Intensive Care Med. 2007;33(11):1869–72.
Malbrain ML, Roberts DJ, Sugrue M, De Keulenaer BL, Ivatury R, Pelosi P, Verbrugge F, Wise R, Mullens W. The polycompartment syndrome: a concise state-of-the-art review. Anaesthesiol Intensive Ther. 2014;46(5):433–50.
Kelm DJ, Perrin JT, Cartin-Ceba R, Gajic O, Schenck L, Kennedy CC. Fluid overload in patients with severe sepsis and septic shock treated with early goal-directed therapy is associated with increased acute need for fluid-related medical interventions and hospital death. Shock. 2015;43(1):68–73.
Murphy CV, Schramm GE, Doherty JA, Reichley RM, Gajic O, Afessa B, Micek ST, Kollef MH. The importance of fluid management in acute lung injury secondary to septic shock. Chest. 2009;136(1):102–9.
Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354(24):2564–75.
Alsous F, Khamiees M, DeGirolamo A, Amoateng-Adjepong Y, Manthous CA. Negative fluid balance predicts survival in patients with septic shock: a retrospective pilot study. Chest. 2000;117(6):1749–54.
Malbrain MLNG, Van Regenmortel N. Fluid overload is not only of cosmetic concern (part I): exploring a new hypothesis. ICU Manage. 2012;12:30–3.
Cordemans C, De Laet I, Van Regenmortel N, Schoonheydt K, Dits H, Huber W, Malbrain MLNG. Fluid management in critically ill patients: the role of extravascular lung water, abdominal hypertension, capillary leak and fluid balance. Ann Intensive Care. 2012;2(Suppl 1):S1.
Malbrain ML, Mythen M, Rice TW, Wuyts S. It is time for improved fluid stewardship. ICU Manage Pract. 2018;18(3):158–62.
Malbrain M, Van Regenmortel N, Owczuk R. It is time to consider the four D’s of fluid management. Anaesthesiol Intensive Ther. 2015;47:S1–5.
Malbrain M, Martin G, Ostermann M. Everything you need to know about deresuscitation. Intensive Care Med. 2022;48(12):1781–6.
Malbrain M, Van Regenmortel N, Saugel B, De Tavernier B, Van Gaal PJ, Joannes-Boyau O, Teboul JL, Rice TW, Mythen M, Monnet X. Principles of fluid management and stewardship in septic shock: it is time to consider the four D’s and the four phases of fluid therapy. Ann Intensive Care. 2018;8(1):66.
Chow RS. Terms, definitions, nomenclature, and routes of fluid administration. Front Vet Sci. 2020;7:591218.
Malbrain M, Langer T, Annane D, Gattinoni L, Elbers P, Hahn RG, De Laet I, Minini A, Wong A, Ince C, et al. Intravenous fluid therapy in the perioperative and critical care setting: executive summary of the International Fluid Academy (IFA). Ann Intensive Care. 2020;10(1):64.
Van Regenmortel N, Verbrugghe W, Roelant E, Van den Wyngaert T, Jorens PG. Maintenance fluid therapy and fluid creep impose more significant fluid, sodium, and chloride burdens than resuscitation fluids in critically ill patients: a retrospective study in a tertiary mixed ICU population. Intensive Care Med. 2018;44(4):409–17.
Cartotto R, Zhou A. Fluid creep: the pendulum hasn’t swung back yet! J Burn Care Res. 2010;31(4):551–8.
Vincent JL, Pinsky MR. We should avoid the term “fluid overload”. Crit Care. 2018;22(1):214.
Cleymaet R, Scheinok T, Maes H, Stas A, Malbrain L, De Laet I, Schoonheydt K, Dits H, van Regenmortel N, Mekeirele M, et al. Prognostic value of bioelectrical impedance analysis for assessment of fluid overload in ICU patients: a pilot study. Anaesthesiol Intensive Ther. 2021;53(1):10–7.
Malbrain MLNG, Van Regenmortel N, Saugel B, De Tavernier B, Van Gaal P-J, Joannes-Boyau O, Teboul J-L, Rice TW, Mythen M, Monnet X. Principles of fluid management and stewardship in septic shock: It is time to consider the four D’s and the four phases of fluid therapy. Ann Intensive Care. 2018;8(1):66.
Ramming S, Shackford SR, Zhuang J, Schmoker JD. The relationship of fluid balance and sodium administration to cerebral edema formation and intracranial pressure in a porcine model of brain injury. J Trauma. 1994;37(5):705–13.
Singh CN, Klein MB, Sullivan SR, Sires BS, Hutter CM, Rice K, Jian-Amadi A. Orbital compartment syndrome in burn patients. Ophthal Plast Reconstr Surg. 2008;24(2):102–6.
Verbrugge FH, Dupont M, Steels P, Grieten L, Malbrain M, Tang WH, Mullens W. Abdominal contributions to cardiorenal dysfunction in congestive heart failure. J Am Coll Cardiol. 2013;62(6):485–95.
Desai KV, Laine GA, Stewart RH, Cox CS Jr, Quick CM, Allen SJ, Fischer UM. Mechanics of the left ventricular myocardial interstitium: effects of acute and chronic myocardial edema. Am J Physiol Heart Circ Physiol. 2008;294(6):2428–34.
Vaara ST, Korhonen AM, Kaukonen KM, Nisula S, Inkinen O, Hoppu S, Laurila JJ, Mildh L, Reinikainen M, Lund V, et al. Fluid overload is associated with an increased risk for 90-day mortality in critically ill patients with renal replacement therapy: data from the prospective FINNAKI study. Crit Care. 2012;16(5):R197.
Reintam Blaser A, Starkopf J, Moonen PJ, Malbrain M, Oudemans-van Straaten HM. Perioperative gastrointestinal problems in the ICU. Anaesthesiol Intensive Ther. 2018;50(1):59–71.
Silversides JA, Perner A, Malbrain M. Liberal versus restrictive fluid therapy in critically ill patients. Intensive Care Med. 2019;45(10):1440–2.
Padhi S, Bullock I, Li L, Stroud M, National Institute for H, Care Excellence Guideline Development G. Intravenous fluid therapy for adults in hospital: summary of NICE guidance. BMJ. 2013;347:f7073.
Powell-Tuck J, Gosling P, Lobo D, Allison S, Carlson G, Gore M, Lewington A, Pearse R, Mythen M. Summary of the British consensus guidelines on intravenous fluid therapy for adult surgical patients (GIFTASUP). J Intensive Care Soc. 2009;10(1):13–5.
Silversides JA, Major E, Ferguson AJ, Mann EE, McAuley DF, Marshall JC, Blackwood B, Fan E. Conservative fluid management or deresuscitation for patients with sepsis or acute respiratory distress syndrome following the resuscitation phase of critical illness: a systematic review and meta-analysis. Intensive Care Med. 2017;43(2):155–70.
Hjortrup PB, Haase N, Bundgaard H, Thomsen SL, Winding R, Pettila V, Aaen A, Lodahl D, Berthelsen RE, Christensen H, et al. Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the CLASSIC randomised, parallel-group, multicentre feasibility trial. Intensive Care Med. 2016;42(11):1695–705.
Silversides JA, Fitzgerald E, Manickavasagam US, Lapinsky SE, Nisenbaum R, Hemmings N, Nutt C, Trinder TJ, Pogson DG, Fan E, et al. Deresuscitation of patients with iatrogenic fluid overload is associated with reduced mortality in critical illness. Crit Care Med. 2018;46(10):1600–7.
Mikkelsen ME, Christie JD, Lanken PN, Biester RC, Thompson BT, Bellamy SL, Localio AR, Demissie E, Hopkins RO, Angus DC. The adult respiratory distress syndrome cognitive outcomes study: long-term neuropsychological function in survivors of acute lung injury. Am J Respir Crit Care Med. 2012;185(12):1307–15.
Myles PS, Bellomo R, Corcoran T, Forbes A, Peyton P, Story D, Christophi C, Leslie K, McGuinness S, Parke R, et al. Restrictive versus liberal fluid therapy for major abdominal surgery. N Engl J Med. 2018;378(24):2263–74.
Silversides JA, McMullan R, Emerson LM, Bradbury I, Bannard-Smith J, Szakmany T, Trinder J, Rostron AJ, Johnston P, Ferguson AJ, et al. Feasibility of conservative fluid administration and deresuscitation compared with usual care in critical illness: the role of active deresuscitation after resuscitation-2 (RADAR-2) randomised clinical trial. Intensive Care Med. 2022;48(2):190–200.
Meyhoff TS, Hjortrup PB, Wetterslev J, Sivapalan P, Laake JH, Cronhjort M, Jakob SM, Cecconi M, Nalos M, Ostermann M, et al. Restriction of intravenous fluid in ICU patients with septic shock. N Engl J Med. 2022;386(26):2459–70.
Maitland K, Kiguli S, Opoka RO, Engoru C, Olupot-Olupot P, Akech SO, Nyeko R, Mtove G, Reyburn H, Lang T, et al. Mortality after fluid bolus in African children with severe infection. N Engl J Med. 2011;364(26):2483–95.
Shapiro NI, Douglas IS, Brower RG, Brown SM, Exline MC, Ginde AA, Gong MN, et al. Early restrictive or liberal fluid management for sepsis-induced hypotension. N Engl J Med. 2023;388(6):499–510.
Meyhoff TS, Hjortrup PB, Moller MH, Wetterslev J, Lange T, Kjaer MN, Jonsson AB, Hjortso CJS, Cronhjort M, Laake JH, et al. Conservative vs liberal fluid therapy in septic shock (CLASSIC) trial-protocol and statistical analysis plan. Acta Anaesthesiol Scand. 2019;63(9):1262–71.
Perel A. Iatrogenic hemodilution: a possible cause for avoidable blood transfusions? Crit Care. 2017;21(1):291.
Claure-Del Granado R, Mehta RL. Fluid overload in the ICU: evaluation and management. BMC Nephrol. 2016;17(1):109.
Perez-Calatayud AA, Carrillo-Esper R, Anica-Malagon ED, Briones-Garduno JC, Arch-Tirado E, Wise R, Malbrain M. Point-of-care gastrointestinal and urinary tract sonography in daily evaluation of gastrointestinal dysfunction in critically ill patients (GUTS protocol). Anaesthesiol Intensive Ther. 2018;50(1):40–8.
Via G, Tavazzi G, Price S. Ten situations where inferior vena cava ultrasound may fail to accurately predict fluid responsiveness: a physiologically based point of view. Intensive Care Med. 2016;42(7):1164–7.
Malbrain M, De Tavernier B, Haverals S, Slama M, Vieillard-Baron A, Wong A, Poelaert J, Monnet X, Stockman W, Elbers P, et al. Executive summary on the use of ultrasound in the critically ill: consensus report from the 3rd course on acute care ultrasound (CACU). Anaesthesiol Intensive Ther. 2017;49(5):393–411.
Lichtenstein DA, Malbrain M. Lung ultrasound in the critically ill (LUCI): a translational discipline. Anaesthesiol Intensive Ther. 2017;49(5):430–6.
Testani JM, Khera AV, St John Sutton MG, Keane MG, Wiegers SE, Shannon RP, Kirkpatrick JN. Effect of right ventricular function and venous congestion on cardiorenal interactions during the treatment of decompensated heart failure. Am J Cardiol. 2010;105(4):511–6.
Beaubien-Souligny W, Rola P, Haycock K, Bouchard J, Lamarche Y, Spiegel R, Denault AY. Quantifying systemic congestion with Point-Of-Care ultrasound: development of the venous excess ultrasound grading system. Ultrasound J. 2020;12(1):16.
Rola P, Miralles-Aguiar F, Argaiz E, Beaubien-Souligny W, Haycock K, Karimov T, Dinh VA, Spiegel R. Clinical applications of the venous excess ultrasound (VExUS) score: conceptual review and case series. Ultrasound J. 2021;13(1):32.
Hofer CK, Cannesson M. Monitoring fluid responsiveness. Acta Anaesthesiol Taiwanica. 2011;49(2):59–65.
Monnet X, Cipriani F, Camous L, Sentenac P, Dres M, Krastinova E, Anguel N, Richard C, Teboul JL. The passive leg raising test to guide fluid removal in critically ill patients. Ann Intensive Care. 2016;6(1):46.
Malbrain M, De Potter TJR, Dits H, Reuter DA. Global and right ventricular end-diastolic volumes correlate better with preload after correction for ejection fraction. Acta Anaesthesiol Scand. 2010;54(5):622–31.
Monnet X, Anguel N, Osman D, Hamzaoui O, Richard C, Teboul JL. Assessing pulmonary permeability by transpulmonary thermodilution allows differentiation of hydrostatic pulmonary edema from ALI/ARDS. Intensive Care Med. 2007;33(3):448–53.
Samoni S, Vigo V, Resendiz LI, Villa G, De Rosa S, Nalesso F, Ferrari F, Meola M, Brendolan A, Malacarne P, et al. Impact of hyperhydration on the mortality risk in critically ill patients admitted in intensive care units: comparison between bioelectrical impedance vector analysis and cumulative fluid balance recording. Crit Care. 2016;20:95.
Nishioka M, Ishikawa M, Hanaki N, Kashiwagi Y, Miki H, Miyake H, Tashiro S. Perioperative hemodynamic study of patients undergoing abdominal surgery using pulse dye densitometry. Hepato-Gastroenterology. 2006;53(72):874–8.
Yu M, Pei K, Moran S, Edwards KD, Domingo S, Steinemann S, Ghows M, Takiguchi S, Tan A, Lurie F, et al. A prospective randomized trial using blood volume analysis in addition to pulmonary artery catheter, compared with pulmonary artery catheter alone, to guide shock resuscitation in critically ill surgical patients. Shock. 2011;35(3):220–8.
de Castro MT, Sato AK, de Moura FS, de Camargo E, Silva OL, Santos TBR, Zhao Z, Moeller K, Amato MBP, Mueller JL, et al. A review of electrical impedance tomography in lung applications: theory and algorithms for absolute images. Annu Rev Control. 2019;48:442–71.
Martin GS, Moss M, Wheeler AP, Mealer M, Morris JA, Bernard GR. A randomized, controlled trial of furosemide with or without albumin in hypoproteinemic patients with acute lung injury. Crit Care Med. 2005;33(8):1681–7.
Cordemans C, de Iaet I, van Regenmortel N, Schoonheydt K, Dits H, Huber W, Malbrain ML. Fluid management in critically ill patients: the role of extravascualr lung water, abdominal hypertension, capillary leak and fluid balance. Ann Intensive Care. 2012;2(Suppl 1):S1.
Cordemans C, De Laet I, Van Regenmortel N, Schoonheydt K, Dits H, Martin G, Huber W, Malbrain ML. Aiming for a negative fluid balance in patients with acute lung injury and increased intra-abdominal pressure: a pilot study looking at the effects of PAL-treatment. Ann Intensive Care. 2012;2(Suppl 1):S15.
De Laet I, Deeren D, Schoonheydt K, Van Regenmortel N, Dits H, Malbrain M. Renal replacement therapy with net fluid removal lowers intra-abdominal pressure and volumetric indices in critically ill patients. Ann Intensive Care. 2012;2:S20.
Acknowledgements
Parts of this chapter were published previously as open access under the Creative Commons Attribution 4.0 International Licence (CC BY 4.0) [1, 12, 20]. The European Commission announced it has adopted CC BY 4.0 and CC0 to share published documents, including photos, videos, reports, peer-reviewed studies, and data. The Commission joins other public institutions around the world that use standard, legally interoperable tools such as Creative Commons licenses and public domain tools to share a wide range of content they produce. The decision to use CC aims to increase the legal interoperability and ease of reuse of authors own materials.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Malbrain, M.L.N.G., Wilkinson, J., Malbrain, L., Nasa, P., Wong, A. (2024). Fluid Accumulation and Deresuscitation. In: Malbrain, M.L., Wong, A., Nasa, P., Ghosh, S. (eds) Rational Use of Intravenous Fluids in Critically Ill Patients. Springer, Cham. https://doi.org/10.1007/978-3-031-42205-8_25
Download citation
DOI: https://doi.org/10.1007/978-3-031-42205-8_25
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-42204-1
Online ISBN: 978-3-031-42205-8
eBook Packages: MedicineMedicine (R0)