Abstract
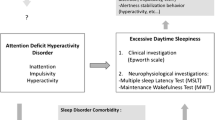
Sleep problems and sleep disorders are common comorbidities in individuals with attention-deficit/hyperactivity disorder (ADHD) across the lifespan. Sleep problems/disorders contribute significantly to the impairment experienced by children and adults with ADHD. Despite the high prevalence of sleep problems/disorders and the impact of these on daytime functioning, screening and assessment of sleep are not often conducted as part of an initial ADHD diagnostic assessment or follow-up assessments. As such, treatment for sleep problems/disorders is often not implemented. In Sect. 10.1 of this chapter, we provide an overview of what is known about sleep and its functions and explore how ADHD and sleep problems/disorders are related. In Sect. 10.2, we provide information about the assessment of sleep problems, including assessment tools and approaches, and how these may be modified for individuals with ADHD. In Sect. 10.3, information about the main sleep disorders in individuals with ADHD is provided, along with best clinical practice for the treatment of these disorders in individuals with ADHD. In Sect. 10.4, we present a case study that highlights sleep problems across childhood, adolescence, and adulthood in an individual with ADHD, along with assessment information. The reader is encouraged to consider a case formulation using a biopsychosocial model and develop a treatment plan using the 4Ps model. This chapter is concluded with the take-away messages about ADHD and sleep problems/disorders.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Aksu, H., Günel, C., Özgür, B. G., Toka, A., & Başak, S. (2015). Effects of adenoidectomy/adenotonsillectomy on ADHD symptoms and behavioral problems in children. International Journal of Pediatric Otorhinolaryngology, 79(7), 1030–1033. https://doi.org/10.1016/j.ijporl.2015.04.018
Alimoradi, Z., Jafari, E., Broström, A., Ohayon, M. M., Lin, C.-Y., Griffiths, M. D., Blom, K., Jernelöv, S., Kaldo, V., & Pakpour, A. H. (2022). Effects of cognitive behavioral therapy for insomnia (CBT-I) on quality of life: A systematic review and meta-analysis. Sleep Medicine Reviews, 64, 101646. https://doi.org/10.1016/j.smrv.2022.101646
Allen, R. P., Burchell, B. J., MacDonald, B., Hening, W. A., & Earley, C. J. (2009). Validation of the self-completed Cambridge-Hopkins questionnaire (CH-RLSq) for ascertainment of restless legs syndrome (RLS) in a population survey. Sleep Medicine, 10(10), 1097–1100. https://doi.org/10.1016/j.sleep.2008.10.007
American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders (3rd ed., revised). American Psychiatric Press.
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (DSM-5-TR). American Psychiatric Association Publishing. https://doi.org/10.1176/appi.books.9780890425787
Angriman, M., & Cortese, S. (2022). Pharmacological and nonpharmacological treatment of insomnias, parasomnias, and circadian rhythm disorders associated with ADHD. In H. Hiscock & E. Sciberras (Eds.), Sleep and ADHD: An evidence-based guide to assessment and treatment (pp. 213–235). Elsevier Academic Press. https://doi-org.ezproxy.library.dal.ca/10.1016/B978-0-12-814180-9.00009-0
Antle, M. C., van Diepen, H. C., Deboer, T., Pedram, P., Pereira, R. R., & Meijer, J. H. (2012). Methylphenidate modifies the motion of the circadian clock. Neuropsychopharmacology, 37, 2446–2455. https://doi.org/10.1038/npp.2012.103
Backhaus, J., Junghanns, K., Broocks, A., Riemann, D., & Hohagen, F. (2002). Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. Journal of Psychosomatic Research, 53(3), 737–740. https://doi.org/10.1016/S0022-3999(02)00330-6
Baglioni, C., Nanovska, S., Regen, W., Spiegelhalder, K., Feige, B., Nissen, C., Reynolds, C. F. I., & Riemann, D. (2016). Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychological Bulletin, 142(9), 969–990. https://doi.org/10.1037/bul0000053
Baird, A. L., Coogan, A. N., Siddiqui, A., Donev, R. M., & Thome, J. (2012). Adult attention-deficit hyperactivity disorder is associated with alterations in circadian rhythms at the behavioural, endocrine and molecular levels. Molecular Psychiatry, 17, 988–995. https://doi.org/10.1038/mp.2011.149
Barclay, N. L., Kocevska, D., Bramer, W. M., Van Someren, E. J. W., & Gehrman, P. (2021). The heritability of insomnia: A meta-analysis of twin studies. Genes, Brain and Behavior, 20(4). https://doi.org/10.1111/gbb.12717
Barker, P. (1988). Basic child psychiatry (5th ed.). University Park Press.
Bassetti, C. L, A,, Kallweit, U,, Vignatelli, L,, Plazzi, G., Lecendreux, M., Baldin, E., Dolenc-Groselj, L., Jennum, P., Khatami, R., Manconi, M., Mayer, G., Partinen, M., Pollmächer, T., Reading, P., Santamaria, J., Sonka, K., Dauvilliers, Y., & Lammers, G. J. (2021). European guideline and expert statements on the management of narcolepsy in adults and children. Eur J Neurol, 28(9), 2815–2830. https://doi.org/10.1111/ene.14888. Epub 2021 Jun 25. PMID: 34173695.
Batool-Anwar, S., Li, Y., De Vito, K., Malhotra, A., Winkelman, J., & Gao, X. (2016). Lifestyle factors and risk of restless legs syndrome: Prospective cohort study. Journal of Clinical Sleep Medicine, 12(02), 187–194. https://doi.org/10.5664/jcsm.5482
Becker, S. P., Sidol, C. A., Van Dyk, T. R., Epstein, J. N., & Beebe, D. W. (2017). Intraindividual variability of sleep/wake patterns in relation to child and adolescent functioning: A systematic review. Sleep Medicine Reviews, 34, 94–121. https://doi.org/10.1016/j.smrv.2016.07.004
Becker, S. P., Epstein, J. N., Tamm, L., Tilford, A. A., Tischner, C. M., Isaacson, P. A., Simon, J. O., & Beebe, D. W. (2019). Shortened sleep duration causes sleepiness, inattention, and oppositionality in adolescents with attention-deficit/hyperactivity disorder: Findings from a crossover sleep restriction/extension study. Journal of the American Academy of Child & Adolescent Psychiatry, 58(4), 433–442. https://doi.org/10.1016/j.jaac.2018.09.439
Becker, S. P., Kapadia, D. K., Fershtman, C. E. M., & Sciberras, E. (2020). Evening circadian preference is associated with sleep problems and daytime sleepiness in adolescents with ADHD. Journal of Sleep Research, 29(1), 1–9. https://doi-org.ezproxy.library.dal.ca/10.1111/jsr.12936
Benz, F., Knoop, T., Ballesio, A., Bacaro, V., Johann, A. F., Rücker, G., Feige, B., Riemann, D., & Baglioni, C. (2020). The efficacy of cognitive and behavior therapies for insomnia on daytime symptoms: A systematic review and network meta-analysis. Clinical Psychology Review, 80, 101873. https://doi.org/10.1016/j.cpr.2020.101873
Berry, R. B., & Wagner, M. H. (2015). Sleep medicine pearls (3rd ed.). Elsevier/Saunders.
Bevans, K. B., Meltzer, L. J., De La Motte, A., Kratchman, A., Viél, D., & Forrest, C. B. (2019). Qualitative development and content validation of the PROMIS pediatric sleep health items. Behavioral Sleep Medicine, 17(5), 657–671. https://doi.org/10.1080/15402002.2018.1461102
Biancardi, C., Sesso, G., Masi, G., Faraguna, U., & Sicca, F. (2021). Sleep EEG microstructure in children and adolescents with attention deficit hyperactivity disorder: A systematic review and meta-analysis. Sleep, 44(7), 1–14. https://doi.org/10.1093/sleep/zsab006
Bijlenga, D., Van Someren, E. J. W., Gruber, R., Bron, T. I., Kruithof, I. F., Spanbroek, E. C. A., & Kooij, J. J. S. (2013). Body temperature, activity and melatonin profiles in adults with attention-deficit/hyperactivity disorder and delayed sleep: A case–control study. Journal of Sleep Research, 22, 607–616. https://doi.org/10.1111/jsr.12075
Bijlenga, D., Vollebregt, M. A., Kooij, J. J. S., & Arns, M. (2019). The role of the circadian system in the etiology and pathophysiology of ADHD: Time to redefine ADHD? ADHD Attention Deficit and Hyperactivity Disorders, 11(1), 5–19. https://doi.org/10.1007/s12402-018-0271-z
Borbély, A. (2022). The two-process model of sleep regulation: Beginnings and outlook. Journal of Sleep Research, 31(4), 1–8. https://doi.org/10.1111/jsr.13598
Bos, S. C., & Macedo, A. F. (2019). Literature review on Insomnia (2010–2016). Biological Rhythm Research, 50(1), 94–163. https://doi.org/10.1080/09291016.2017.1413766
Bragg, S., Benich, J., Christian, N., Visserman, J., & Freedy, J. (2019). Updates in insomnia diagnosis and treatment. The International Journal of Psychiatry in Medicine, 54(4–5), 275–289. https://doi.org/10.1177/0091217419860716
Brevik, E. J., Lundervold, A. J., Halmøy, A., Posserud, M.-B., Instanes, J. T., Bjorvatn, B., & Haavik, J. (2017). Prevalence and clinical correlates of insomnia in adults with attention-deficit hyperactivity disorder. Acta Psychiatrica Scandinavica, 136(2), 220–227. https://doi.org/10.1111/acps.12756
Bruni, O., Angriman, M., Calisti, F., Comandini, A., Esposito, G., Cortese, S., & Ferri, R. (2018). Practitioner review: Treatment of chronic insomnia in children and adolescents with neurodevelopmental disabilities. Journal of Child Psychology and Psychiatry, 59(5), 489–508. https://doi.org/10.1111/jcpp.12812
Bumb, J. M., Mier, D., Noelte, I., Schredl, M., Kirsch, P., Hennig, O., Liebrich, L., Fenske, S., Alm, B., Sauer, C., Leweke, F. M., & Sobanski, E. (2016). Associations of pineal volume, chronotype and symptom severity in adults with attention deficit hyperactivity disorder and healthy controls. European Neuropsychopharmocology, 26(7), 1119–1126. https://doi.org/10.1016/j.euroneuro.2016.03.016
Buysse, D. J. (2014). Sleep health: Can we define it? Does it matter? Sleep, 37(1), 9–17. https://doi.org/10.5665/sleep.3298
Buysse, D. J., Yu, L., Moul, D. E., Germain, A., Stover, A., Dodds, N. E., Johnston, K. L., Shablesky-Cade, M. A., & Pilkonis, P. A. (2010). Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep, 33(6), 781–792. https://doi.org/10.1093/sleep/33.6.781
Byars, K. C., Simon, S. L., Peugh, J., & Beebe, D. W. (2016). Validation of a brief insomnia severity measure in youth clinically referred for sleep evaluation. Journal of Pediatric Psychology, jsw077. https://doi.org/10.1093/jpepsy/jsw077
Carpena, M. X., Bonilla, C., Matijasevich, A., Martins-Silva, T., Genro, J. P., Hutz, M. H., Rohde, L. A., & Tovo-Rodrigues, L. (2021). Sleep-related traits and attention-deficit/hyperactivity disorder comorbidity: Shared genetic risk factors, molecular mechanisms, and causal effects. The World Journal of Biological Psychiatry, 22(10), 778–791. https://doi.org/10.1080/15622975.2021.1907719
Cella, D., Yount, S., Rothrock, N., Gershon, R., Cook, K., Reeve, B., Ader, D., Fries, J. F., Bruce, B., & Rose, M. (2007). The patient-reported outcomes measurement information system (PROMIS). Medical Care, 45(5 Suppl 1), S3–S11. https://doi.org/10.1097/01.mlr.0000258615.42478.55
Chaput, J.-P. (2019). The integration of pediatric sleep health into public health in Canada. Sleep Medicine, 56, 4–8. https://doi.org/10.1016/j.sleep.2018.06.009
Chen, M., Wardlaw, M., & Stein, M. A. (2019). ADHD medications and sleep. In Sleep and ADHD (pp. 151–173). Elsevier. https://doi.org/10.1016/B978-0-12-814180-9.00006-5
Cheng, D. C. Y., Ganner, J. L., Gordon, C. J., Phillips, C. L., Grunstein, R. R., & Comas, M. (2021). The efficacy of combined bright light and melatonin therapies on sleep and circadian outcomes: A systematic review. Sleep Medicine Reviews, 58, 101491. https://doi.org/10.1016/j.smrv.2021.101491
Chervin, R. D., Dillon, J. E., Bassetti, C., Ganoczy, D. A., & Pituch, K. J. (1997). Symptoms of sleep disorders, inattention, and hyperactivity in children. Sleep, 20(12), 1185–1192. https://doi.org/10.1093/sleep/20.12.1185
Chervin, R. D., Ruzicka, D. L., Giordani, B. J., Weatherly, R. A., Dillon, J. E., Hodges, E. K., Marcus, C. L., & Guire, K. E. (2006). Sleep-disordered breathing, behavior, and cognition in children before and after adenotonsillectomy. Pediatrics, 117(4), e769–e778. https://doi.org/10.1542/peds.2005-1837
Chung, K.-F., Lee, C.-T., Yeung, W.-F., Chan, M.-S., Chung, E. W.-Y., & Lin, W.-L. (2018). Sleep hygiene education as a treatment of insomnia: A systematic review and meta-analysis. Family Practice, 35(4), 365–375. https://doi.org/10.1093/fampra/cmx122
Coles, L., Thorpe, K., Smith, S., Hewitt, B., Ruppanner, L., Bayliss, O., O’Flaherty, M., & Staton, S. (2022). Children’s sleep and fathers’ health and wellbeing: A systematic review. Sleep Medicine Reviews, 61, 101570. https://doi.org/10.1016/j.smrv.2021.101570
Coogan, A. N., & McGowan, N. M. (2017). A systematic review of circadian function, chronotype and chronotherapy in attention deficit hyperactivity disorder. ADHD Attention Deficit and Hyperactivity Disorders, 9(3), 129–147. https://doi.org/10.1007/s12402-016-0214-5
Corkum, P., & Coulombe, J. A. (2013). Sleep in the context of ADHD: A review of reviews to determine implications for research and clinical practice. In I. A. R. Wolfson & H. E. Montgomery-Downs (Eds.), The Oxford handbook of infant, child, and adolescent sleep and behavior (pp. 495–514). Oxford University Press.
Corkum, P., Davidson, F., & MacPherson, M. (2011). A framework for the assessment and treatment of sleep problems in children with attention-deficit/hyperactivity disorder. Pediatric Clinics of North America, 58(3), 667–683. https://doi.org/10.1016/j.pcl.2011.03.004
Corkum, P., Lingley-Pottie, P., Davidson, F., McGrath, P., Chambers, C. T., Mullane, J., Laredo, S., Woodford, K., & Weiss, S. K. (2016). Better nights/better days—Distance intervention for insomnia in school-aged children with/without ADHD: A randomized controlled trial. Journal of Pediatric Psychology, 41(6), 701–713. https://doi.org/10.1093/jpepsy/jsw031
Corkum, P., Rigney, G., Howlett, M., & Weiss, S. (2019a). Healthy sleep practices (sleep hygiene) in children with ADHD. In Sleep and ADHD (pp. 119–149). Elsevier. https://doi.org/10.1016/B978-0-12-814180-9.00005-3
Corkum, P., Weiss, S., Hall, W., Brown, C., Chambers, C., Constantin, E., Godbout, R., Hanlon-Dearman, A., Ipsiroglu, O., Reid, G. J., Shea, S., Smith, I. M., Stremler, R., & Witmans, M. (2019b). Assessment and treatment of pediatric behavioral sleep disorders in Canada. Sleep Medicine, 56, 29–37. https://doi.org/10.1016/j.sleep.2018.11.007
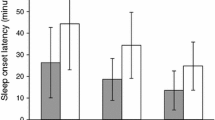
Corkum, P., Begum, E., Rusak, B., Rajda, M., Shea, S., MacPherson, M., Williams, T., Spurr, K., & Davidson, F. (2020). The effects of extended release stimulant medication on sleep in children with ADHD. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 29(1), 33–43.
Cortese, S., Konofal, E., Yateman, N., Mouren, M.-C., & Lecendreux, M. (2006). Sleep and alertness in children with attention-deficit/hyperactivity disorder: A systematic review of the literature. Journal of Sleep and Sleep Disorders Research, 29(4), 504–511.
Cortese, S., Faraone, S. V., Konofal, E., & Lecendreux, M. (2009). Sleep in children with attention-deficit/hyperactivity disorder: Meta-analysis of subjective and objective studies. Journal of the American Academy of Child & Adolescent Psychiatry, 48(9), 894–908. https://doi.org/10.1097/chi.0b013e3181ac09c9
Cortese, S., Brown, T. E., Corkum, P., Gruber, R., O’Brien, L. M., Stein, M., Weiss, M., & Owens, J. (2013). Assessment and management of sleep problems in youths with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 52(8), 784–796. https://doi.org/10.1016/j.jaac.2013.06.001
Cortese, S., Sun, S., Zhang, J., Sharma, E., Chang, Z., Kuja-Halkola, R., Almqvist, C., Larsson, H., & Faraone, S. V. (2018). Association between attention deficit hyperactivity disorder and asthma: A systematic review and meta-analysis and a Swedish population-based study. The Lancet Psychiatry, 5(9), 717–726. https://doi.org/10.1016/S2215-0366(18)30224-4
Cortese, S., Sabé, M., Chen, C., Perroud, N., & Solmi, M. (2022). Half a century of research on attention-deficit/hyperactivity disorder: A scientometric study. Neuroscience and Biobehavioral Reviews, 140, 104769. https://doi.org/10.1016/j.neubiorev.2022.104769
Cox, R. C., & Olatunji, B. O. (2020). Sleep in the anxiety-related disorders: A meta-analysis of subjective and objective research. Sleep Medicine Reviews, 51, 101282. https://doi.org/10.1016/j.smrv.2020.101282
Curcio, G., Ferrara, M., & Gennaro, L. D. (2006). Sleep loss, learning capacity and academic performance. Sleep Medicine Reviews, 10, 323–337. https://doi.org/10.1016/j.smrv.2005.11.001
Davidson, F., Rusak, B., Chambers, C., & Corkum, P. (2018). The impact of sleep restriction on daytime functioning in school-aged children with and without ADHD: A narrative review of the literature. Canadian Journal of School Psychology, 34(3), 188–214. https://doi.org/10.1177/0829573518770593
Davidson, F., Rigney, G., Rusak, B., Chambers, C., Rajda, M., & Corkum, P. (2021). Sleep variables as predictors of treatment effectiveness and side-effects of stimulant medication in newly diagnosed children with ADHD. Journal of Developmental and Behavioral Pediatrics, 42(1), 1–8. https://doi.org/10.1097/DBP.0000000000000866
de Bruin, E. J., Bögels, S. M., Oort, F. J., & Meijer, A. M. (2018). Improvements of adolescent psychopathology after insomnia treatment: Results from a randomized controlled trial over 1 year. Journal of Child Psychology and Psychiatry, 59(5), 509–522. https://doi.org/10.1111/jcpp.12834
Demichelis, O. P., Grainger, S. A., McKay, K. T., Bourdaniotis, X. E., Churchill, E. G., & Henry, J. D. (2022). Sleep, stress and aggression: Meta-analyses investigating associations and causality. Neuroscience & Biobehavioral Reviews, 139, 104732. https://doi.org/10.1016/j.neubiorev.2022.104732
Díaz-Román, A., Mitchell, R., & Cortese, S. (2018). Sleep in adults with ADHD: Systematic review and meta-analysis of subjective and objective studies. Neuroscience and Biobehavioral Reviews, 89, 61–71. https://doi.org/10.1016/j.neubiorev.2018.02.014
Dimakos, J., Gauthier-Gagné, G., Lin, L., Scholes, S., & Gruber, R. (2021). The associations between sleep and externalizing and internalizing problems in children and adolescents with attention-deficit/hyperactivity disorder. Child and Adolescent Psychiatric Clinics of North America, 30(1), 175–193. https://doi.org/10.1016/j.chc.2020.08.001
Drouyer, E., Rieux, C., Hut, R. A., & Cooper, H. M. (2007). Responses of SCN neurons to light and dark adaptation: Relative contributions of melanopsin and rod-cone inputs. Journal of Neuroscience, Society for Neuroscience, 27(36), 9623–9631. https://doi.org/10.1523/JNEUROSCI.1391-07.2007
Durmus, F. B., Arman, A. R., & Ayaz, A. B. (2017). Chronotype and its relationship with sleep disorders in children with attention deficit hyperactivity disorder. Chronobiology International, 34(7), 886–894. https://doi.org/10.1080/07420528.2017.1329207
Dutil, C., Walsh, J. J., Featherstone, R. B., Gunnell, K. E., Tremblay, M. S., Gruber, R., Weiss, S. K., Cote, K. A., Sampson, M., & Chaput, J.-P. (2018). Influence of sleep on developing brain functions and structures in children and adolescents: A systematic review. Sleep Medicine Reviews, 42, 184–201. https://doi.org/10.1016/j.smrv.2018.08.003
Engel, G. L. (1977). The need for a new medical model: A challenge for biomedicine. Science, 196(4286), 129–136. https://doi.org/10.1126/science.847460
England, S. J., Picchietti, D. L., Couvadelli, B. V., Fisher, B. C., Siddiqui, F., Wagner, M. L., Hening, W. A., Lewin, D., Winnie, G., Cohen, B., & Walters, A. S. (2011). L-Dopa improves restless legs syndrome and periodic limb movements in sleep but not attention-deficit-hyperactivity disorder in a double-blind trial in children. Sleep Medicine, 12(5), 471–477. https://doi.org/10.1016/j.sleep.2011.01.008
Faulkner, S. M., Bee, P. E., Meyer, N., Dijk, D.-J., & Drake, R. J. (2019). Light therapies to improve sleep in intrinsic circadian rhythm sleep disorders and neuro-psychiatric illness: A systematic review and meta-analysis. Sleep Medicine Reviews, 46, 108–123. https://doi.org/10.1016/j.smrv.2019.04.012
Filardi, M., Pizza, F., Tonetti, L., Antelmi, E., Natale, V., et al. (2017) Attention impairments and ADHD symptoms in adult narcoleptic patients with and without hypocretin deficiency. PLOS ONE 12(8): e0182085. https://doi.org/10.1371/journal.pone.0182085
Forrest, C. B., Meltzer, L. J., Marcus, C. L., de la Motte, A., Kratchman, A., Buysse, D. J., Pilkonis, P. A., Becker, B. D., & Bevans, K. B. (2018). Development and validation of the PROMIS Pediatric Sleep Disturbance and Sleep-Related Impairment item banks. Sleep, 41(6). https://doi.org/10.1093/sleep/zsy054
Funderburk, J. S., Shepardson, R. L., Wray, J., Acker, J., Beehler, G. P., Possemato, K., Wray, L. O., & Maisto, S. A. (2018). Behavioral medicine interventions for adult primary care settings: A review. Families, Systems & Health, 36(3), 368–399. https://doi.org/10.1037/fsh0000333
Gao, Y., Ge, L., Liu, M., Niu, M., Chen, Y., Sun, Y., Chen, J., Yao, L., Wang, Q., Li, Z., Xu, J., Li, M., Hou, L., Shi, J., Yang, K., Cai, Y., Li, L., Zhang, J., & Tian, J. (2022). Comparative efficacy and acceptability of cognitive behavioral therapy delivery formats for insomnia in adults: A systematic review and network meta-analysis. Sleep Medicine Reviews, 64, 101648. https://doi.org/10.1016/j.smrv.2022.101648
Gardani, M., Bradford, D. R. R., Russell, K., Allan, S., Beattie, L., Ellis, J. G., & Akram, U. (2022). A systematic review and meta-analysis of poor sleep, insomnia symptoms and stress in undergraduate students. Sleep Medicine Reviews, 61, 101565. https://doi.org/10.1016/j.smrv.2021.101565
Gloger, E. M., & Suhr, J. A. (2020). Correlates of poor sleep and subsequent risk of misdiagnosis in college students presenting with cognitive complaints. Archives of Clinical Neuropsychology, 35(6), 692–670. https://doi.org/10.1093/arclin/acaa023
Goll, J. C., & Shapiro, C. M., (2006). Sleep disorders presenting as common pediatric problems. Canadian Medical Association Journal, 174(5), 617. https://doi.org/10.1503/cmaj.1040993
Golden, M. E., Cosottile, M., Meadows, T., Parikh, M. R., & O’Dell, S. M. (2022). Primary care providers’ practices regarding patient sleep: Impact of integrated behavioral health. Families, Systems & Health. https://doi.org/10.1037/fsh0000695
Gradisar, M., Gardner, G., & Dohnt, H. (2011). Recent worldwide sleep patterns and problems during adolescence: A review and meta-analysis of age, region, and sleep. Sleep Medicine, 12(2), 110–118. https://doi.org/10.1016/j.sleep.2010.11.008
Gruber, R., Grizenko, N., & Joober, R. (2007). Delayed sleep phase syndrome, ADHD, and bright light therapy. The Journal of Clinical Psychiatry, 68(02), 337–338. https://doi.org/10.4088/JCP.v68n0221h
Gruber, R., Wiebe, S., Montecalvo, L., Brunetti, B., Amsel, R., & Carrier, J. (2011). Impact of sleep restriction on neurobehavioral functioning of children with attention deficit hyperactivity disorder. Sleep, 34(3), 315–323. https://doi.org/10.1093/sleep/34.3.315
Gruber, R., Fontil, L., Bergmame, L., Wiebe, S. T., Amsel, R., Frenette, S., & Carrier, J. (2012). Contributions of circadian tendencies and behavioral problems to sleep onset problems of children with ADHD. BMC Psychiatry, 12, 212. http://www.biomedcentral.com/1471-244X/12/212
Gudka, S., Haynes, E., Scotney, J., Mukherjee, S., Frenkel, S., Sivam, S., Swieca, J., Chamula, K., Cunnington, D., & Saini, B. (2022). Narcolepsy: Comorbidities, complexities and future directions. Sleep Medicine Reviews, 65, 101669. https://doi.org/10.1016/j.smrv.2022.101669. Epub 2022 Aug 11. PMID: 36037569.
Harris, M. A. (2009). Too soon for dopaminergics in the management of restless legs syndrome in children. Sleep Medicine Reviews, 13(4), 299–300. https://doi.org/10.1016/j.smrv.2009.03.002
Hasan, F., Tu, Y.-K., Yang, C.-M., James Gordon, C., Wu, D., Lee, H.-C., Yuliana, L. T., Herawati, L., Chen, T.-J., & Chiu, H.-Y. (2022). Comparative efficacy of digital cognitive behavioral therapy for insomnia: A systematic review and network meta-analysis. Sleep Medicine Reviews, 61, 101567. https://doi.org/10.1016/j.smrv.2021.101567
Hayes, B., & Bainton, J. (2020). The impact of reduced sleep on school related outcomes for typically developing children aged 11–19: A systematic review. School Psychology International, 41(6), 569–594. https://doi.org/10.1177/0143034320961130
Heaton, K., & Anderson, D. (2007). A psychometric analysis of the Epworth sleepiness scale. Journal of Nursing Measurement, 15(3), 177–188. https://doi.org/10.1891/106137407783095748
Hening, W. (2004). Impact, diagnosis and treatment of restless legs syndrome (RLS) in a primary care population: The REST (RLS epidemiology, symptoms, and treatment) primary care study. Sleep Medicine, 5(3), 237–246. https://doi.org/10.1016/j.sleep.2004.03.006
Hertenstein, E., Trinca, E., Wunderlin, M., Schneider, C. L., Züst, M. A., Fehér, K. D., Su, T., Straten, V. A., Berger, T., Baglioni, C., Johann, A., Spiegelhalder, K., Riemann, D., Feige, B., & Nissen, C. (2022). Cognitive behavioral therapy for insomnia in patients with mental disorders and comorbid insomnia: A systematic review and meta-analysis. Sleep Medicine Reviews, 62, 101597. https://doi.org/10.1016/j.smrv.2022.101597
Hiscock, H., Sciberras, E., Mensah, F., Gerner, B., Efron, D., Khano, S., & Oberklaid, F. (2015). Impact of a behavioural sleep intervention on symptoms and sleep in children with attention deficit hyperactivity disorder, and parental mental health: Randomised controlled trial. BMJ, 350, h68–h68. https://doi.org/10.1136/bmj.h68
Hiscock, H., Mulraney, M., Heussler, H., Rinehart, N., Schuster, T., Grobler, A. C., Gold, L., Bohingamu Mudiyanselage, S., Hayes, N., & Sciberras, E. (2019). Impact of a behavioral intervention, delivered by pediatricians or psychologists, on sleep problems in children with ADHD: A cluster-randomized, translational trial. Journal of Child Psychology and Psychiatry, 60(11), 1230–1241. https://doi.org/10.1111/jcpp.13083. APA PsycInfo.
Horne, J. A., & Östberg, O. (1976). A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. International Journal of Chronobiology, 4, 97–110.
Hornyak, M., Feige, B., Riemann, D., & Voderholzer, U. (2006). Periodic leg movements in sleep and periodic limb movement disorder: Prevalence, clinical significance and treatment. Sleep Medicine Reviews, 10(3), 169–177. https://doi.org/10.1016/j.smrv.2005.12.003
Huhn, A. S., Ellis, J. D., Dunn, K. E., Sholler, D. J., Tabaschek, P., Burns, R., & Strain, E. C. (2022). Patient-reported sleep outcomes in randomized-controlled trials in persons with substance use disorders: A systematic review. Drug and Alcohol Dependence, 237, 109508. https://doi.org/10.1016/j.drugalcdep.2022.109508
Huang, Y.-S., Guilleminault, C., Li, H.-Y., Yang, C.-M., Wu, Y.-Y., & Chen, N.-H. (2007). Attention-deficit/hyperactivity disorder with obstructive sleep apnea: A treatment outcome study. Sleep Medicine, 8(1), 18–30. https://doi.org/10.1016/j.sleep.2006.05.016
Hvolby, A. (2015). Associations of sleep disturbance with ADHD: Implications for treatment. ADHD Attention Deficit and Hyperactivity Disorders, 7(1), 1–18. https://doi.org/10.1007/s12402-014-0151-0
Hysing, M., Heradstveit, O., Harvey, A. G., Nilsen, S. A., Bøe, T., & Sivertsen, B. (2022). Sleep problems among adolescents within child and adolescent mental health services. An epidemiological study with registry linkage. European Child & Adolescent Psychiatry, 31(1), 121–131. https://doi.org/10.1007/s00787-020-01676-4
Ironside, S., Davidson, F., & Corkum, P. (2010). Circadian motor activity affected by stimulant medication in children with attention-deficit/hyperactivity disorder. Journal of Sleep Research, 19(4), 546–551. https://doi.org/10.1111/j.1365-2869.2010.00845.x
Jernelöv, S., Larsson, Y., Llenas, M., Nasri, B., & Kaldo, V. (2019). Effects and clinical feasibility of a behavioral treatment for sleep problems in adult attention deficit hyperactivity disorder (ADHD): A pragmatic within-group pilot evaluation. BMC Psychiatry, 19. https://doi.org/10.1186/s12888-019-2216-2. APA PsycInfo.
Ji, X., & Liu, J. (2016). Subjective sleep measures for adolescents: A systematic review: Subjective sleep measures for adolescents. Child: Care, Health and Development, 42(6), 825–839. https://doi.org/10.1111/cch.12376
Khullar, A. (2012). The role of melatonin in the circadian rhythm sleep-wake cycle. Psychiatric Times, 29(7), 26–32.
Kidwell, K. M., Van Dyk, T. R., Lundahl, A., & Nelson, T. D. (2015). Stimulant medications and sleep for youth with ADHD: A meta-analysis, 136(6), 1144–1153. https://doi.org/10.1542/Peds.2015-1708
Klingman, K. J., Jungquist, C. R., & Perlis, M. L. (2017). Questionnaires that screen for multiple sleep disorders. Sleep Medicine Reviews, 32, 37–44. https://doi.org/10.1016/j.smrv.2016.02.004
Kim, J., Lee, G. H., Sung, S.M., Jung, D. S., & Pak, K. (2020). Prevalence of attention deficit hyperactivity disorder symptoms in narcolepsy: a systematic review. Sleep Medicine, 65, 84–88. https://doi.org/10.1016/j.sleep.2019.07.022. Epub 2019 Aug 3. Erratum in: Sleep Med. 2023 Jul;107:100. PMID: 31739230.
Kocevska, D., Lysen, T. S., Dotinga, A., Koopman-Verhoeff, M. E., Luijk, M. P. C. M., Antypa, N., Biermasz, N. R., Blokstra, A., Brug, J., Burk, W. J., Comijs, H. C., Corpeleijn, E., Dashti, H. S., de Bruin, E. J., de Graaf, R., Derks, I. P. M., Dewald-Kaufmann, J. F., Elders, P. J. M., Gemke, R. J. B. J., et al. (2021). Sleep characteristics across the lifespan in 1.1 million people from the Netherlands, United Kingdom and United States: A systematic review and meta-analysis. Nature Human Behaviour, 5, 113–122. https://doi.org/10.1038/s41562-020-00965-x
Kraus, S. S., & Rabin, L. A. (2012). Sleep America: Managing the crisis of adult chronic insomnia and associated conditions. Journal of Affective Disorders, 138(3), 192–212. https://doi.org/10.1016/j.jad.2011.05.014
Kwon, M., Wang, J., Wilding, G., Dickerson, S. S., & Dean, G. E. (2022). Brief behavioral treatment for insomnia: A meta-analysis. Behavioral Sleep Medicine, 20(6), 674–694. https://doi.org/10.1080/15402002.2021.1982715
Lai, J.-S., Blackwell, C. K., Tucker, C. A., Jensen, S. E., & Cella, D. (2022). Measuring PROMIS® physical activity and sleep problems in early childhood. Journal of Pediatric Psychology, 47(5), 534–546. https://doi.org/10.1093/jpepsy/jsac028
Langberg, J. M., Breaux, R. P., Cusick, C. N., Green, C. D., Smith, Z. R., Molitor, S. J., & Becker, S. P. (2019). Intraindividual variability of sleep/wake patterns in adolescents with and without attention-deficit/hyperactivity disorder. The Journal of Child Psychology and Psychiatry, 60(11), 1219–1229. https://doi.org/10.1111/jcpp.13082
Lecendreux, M. MD and others (2015). Attention-Deficit/Hyperactivity Disorder (ADHD) Symptoms in Pediatric Narcolepsy: A Cross-Sectional Study. Sleep, 38(8), 1285–1295. https://doi.org/10.5665/sleep.4910
Lee, H., Chen, R., Lee, Y., & Lee, C. (2009). Essential roles of CKIδ and CKIε in the mammalian circadian clock. Biological Sciences, 106(50), 21359–21364. https://doi.org/10.1073/pnas.0906651106
Longstreth, W. T. Jr, Koepsell, T. D., Ton, T. G., Hendrickson, A. F., & van Belle, G. (2007). The epidemiology of narcolepsy. Sleep, 30(1), 13–26. https://doi.org/10.1093/sleep/30.1.13. PMID: 17310860.
Lopez, R., Micoulaud-Franchi, J.-A., Camodeca, L., Gachet, M., Jaussent, I., & Dauvilliers, Y. (2020). Association of Inattention, Hyperactivity, and Hypersomnolence in Two Clinic-Based Adult Cohorts. Journal of Attention Disorders, 24(4), 555–564. https://doi.org/10.1177/1087054718775826
Lucas, I., Mulraney, M., & Sciberras, E. (2019). Sleep problems and daytime sleepiness in children with ADHD: Associations with social, emotional, and behavioral functioning at school, a cross-sectional study. Behavioral Sleep Medicine, 17(4), 411–422. https://doi.org/10.1080/15402002.2017.1376207
Lundahl, A., Kidwell, K. M., Van Dyk, T. R., & Nelson, T. D. (2015). A meta-analysis of the effect of experimental sleep restriction on youth’s attention and hyperactivity. Developmental Neuropsychology, 40(3), 104–121. https://doi.org/10.1080/87565641.2014.939183
Lunsford-Avery, J. R., Krystal, A. D., & Kollins, S. H. (2016). Sleep disturbances in adolescents with ADHD: A systematic review and framework for future research. Clinical Psychology Review, 50, 159–174. https://doi.org/10.1016/j.cpr.2016.10.004
Mai, E., & Buysse, D. J. (2008). Insomnia: Prevalence, impact, pathogenesis, differential diagnosis, and evaluation. Sleep Medicine Clinics, 3(2), 167–174. https://doi.org/10.1016/j.jsmc.2008.02.001
Markovich, A. N., Gendron, M. A., & Corkum, P. V. (2015). Validating the children’s sleep habits questionnaire against polysomnography and actigraphy in school-aged children. Frontiers in Psychiatry, 5. https://doi.org/10.3389/fpsyt.2014.00188
Martin, C. A., Papadopoulos, N., Rinehart, N., & Sciberras, E. (2021). Associations between child sleep problems and maternal mental health in children with ADHD. Behavioral Sleep Medicine, 19(1), 12–25. https://doi.org/10.1080/15402002.2019.1696346
Maski, K., Trotti, L. M., Kotagal, S., Robert Auger, R., Rowley, J. A., Hashmi, S. D., & Watson, N. F. (2021). Treatment of central disorders of hypersomnolence: An American Academy of Sleep Medicine clinical practice guideline. Journal of Clinical Sleep Medicine, 17(9), 1881–1893. https://doi.org/10.5664/jcsm.9328
McDonagh, M. S., Holmes, R., & Hsu, F. (2019). Pharmacologic treatments for sleep disorders in children: A systematic review. Journal of Child Neurology, 34(5), 237–247. https://doi.org/10.1177/0883073818821030
McLay, L., Sutherland, D., Machalicek, W., & Sigafoos, J. (2020). Systematic review of telehealth interventions for the treatment of sleep problems in children and adolescents. Journal of Behavioral Education, 29(2), 222–245. https://doi.org/10.1007/s10864-020-09364-8
Meltzer, L. J., Forrest, C. B., de la Motte, A., & Bevans, K. B. (2020). Clinical validity of the PROMIS pediatric sleep measures across populations of children with chronic illnesses and neurodevelopment disorders. Journal of Pediatric Psychology, 45(3), 319–327. https://doi.org/10.1093/jpepsy/jsz088
Merikanto, I., Pesonen, A.-K., Kuula, L., Lahti, J., Heinonen, K., Kajantie, E., & Räikkönen, K. (2017). Eveningness as a risk for behavioural problems in late adolescence. Chronobiology International, 34(2), 225–234. https://doi.org/10.1080/07420528.2016.1267739
Miano, S. (2017). Circadian rhythm disorders in childhood. In S. Nevšímalová & O. Bruni (Eds.), Sleep disorders in children (pp. 253–280). Springer International Publishing. https://doi.org/10.1007/978-3-319-28640-2_12
Micic, G., Lovato, N., Gradisar, M., Ferguson, S. A., Burgess, H. J., & Lack, L. C. (2016). The etiology of delayed sleep phase disorder. Sleep Medicine Reviews, 27, 29–38. https://doi.org/10.1016/j.smrv.2015.06.004
Minz, S., & Pati, A. K. (2021). Morningness-eveningness preference, sleep quality and behavioral sleep patterns in humans—A mini review. Biological Rhythm Research, 52(4), 549–584. https://doi.org/10.1080/09291016.2019.1616889
Modestino, E. J., & Winchester, J. (2013). A retrospective survey of childhood ADHD symptomatology among adult narcoleptics. Journal of Attention Disorders, 17(7), 574–582. https://doi.org/10.1177/1087054713480033. Epub 2013 Apr 2. PMID: 23548870.
Montplaisir, J., Boucher, S., Poirier, G., Lavigne, G., Lapierre, O., & Lespérance, P. (1997). Clinical, polysomnographic, and genetic characteristics of restless legs syndrome: A study of 133 patients diagnosed with new standard criteria. Movement Disorders, 12(1), 61–65. https://doi.org/10.1002/mds.870120111
Morin, C. M., Belleville, G., Bélanger, L., & Ivers, H. (2011). The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep, 34(5), 601–608. https://doi.org/10.1093/sleep/34.5.601
Mulraney, M., Giallo, R., Lycett, K., Mensah, F., & Sciberras, E. (2016). The bidirectional relationship between sleep problems and internalizing and externalizing problems in children with ADHD. Sleep Medicine, 17, 45–51. https://doi.org/10.1016/j.sleep.2015.09.019
National Sleep Foundation. (2020, October 1). How much sleep do you really need? https://www.thensf.org/how-many-hours-of-sleep-do-you-really-need/
Navarro-Bravo, B., Párraga-Martínez, I., López-Torres Hidalgo, J., Andrés-Pretel, F., & Rabanales-Sotos, J. (2015). Group cognitive-behavioral therapy for insomnia: A meta-analysis. [Terapia cognitivo-conductual grupal para el tratamiento del insomnio: metaanálisis]. Anales de Psicología, 31(1), 8–18. https://doi.org/10.6018/analesps.31.1.168641
Nixon, G. M. (2019). Treatment of medical (sleep breathing disorders, restless legs syndrome, periodic limb movement disorder, and narcolepsy) sleep problems in ADHD. In H. Hiscock & E. Sciberras (Eds.), Sleep and ADHD: An evidence-based guide to assessment and treatment (2019-25191-010; pp. 237–255). Elsevier Academic Press; APA PsycInfo. https://doi.org/10.1016/B978-0-12-814180-9.00010-7
Nováková, M., Paclt, I., Ptáček, R., Kuželová, H., Hájek, I., & Sumová, A. (2011). Salivary melatonin rhythm as a marker of the circadian system in healthy children and those with attention-deficit/hyperactivity disorder. Chronobiology International, 28(7), 630–637. https://doi.org/10.3109/07420528.2011.596983
Oosterloo, M., Lammers, G. J., Overeem, S., de Noord, I., & Kooij, J. J. S. (2006). Possible confusion between primary hypersomnia and adult attention-deficit/hyperactivity disorder. Psychiatry Research, 143(2-3), 293–297. https://doi.org/10.1016/j.psychres.2006.02.009
Ottoni, G. L., Antoniolli, E., & Lara, D. R. (2012). Circadian preference is associated with emotional and affective temperaments. Chronobiology International, 29(6), 786–793. https://doi.org/10.3109/07420528.2012.679329
Owens, J. A., & Dalzell, V. (2005). Use of the ‘BEARS’ sleep screening tool in a pediatric residents’ continuity clinic: A pilot study. Sleep Medicine, 6(1), 63–69. https://doi.org/10.1016/j.sleep.2004.07.015
Owens, J. A., Spirito, A., & McGuinn, M. (2000). The Children’s Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep, 23(8), 1–9. https://doi.org/10.1093/sleep/23.8.1d
Palagini, L., Biber, K., & Riemann, D. (2014). The genetics of insomnia – Evidence for epigenetic mechanisms? Sleep Medicine Reviews, 18(3), 225–235. https://doi.org/10.1016/j.smrv.2013.05.002
Peppard, P. E., Young, T., Barnet, J. H., Palta, M., Hagen, E. W., & Hla, K. M. (2013). Increased prevalence of sleep-disordered breathing in adults. American Journal of Epidemiology, 177(9), 1006–1014. https://doi.org/10.1093/aje/kws342
Picchietti, M. A., & Picchietti, D. L. (2010). Advances in pediatric restless legs syndrome: Iron, genetics, diagnosis and treatment. Sleep Medicine, 11(7), 643–651. https://doi.org/10.1016/j.sleep.2009.11.014
Rezaie, L., Fobian, A. D., McCall, W. V., & Khazaie, H. (2018). Paradoxical insomnia and subjective–objective sleep discrepancy: A review. Sleep Medicine Reviews, 40, 196–202. https://doi.org/10.1016/j.smrv.2018.01.002
Riemann, D., Baglioni, C., Bassetti, C., Bjorvatn, B., Dolenc Groselj, L., Ellis, J. G., Espie, C. A., Garcia-Borreguero, D., Gjerstad, M., Gonçalves, M., Hertenstein, E., Jansson-Fröjmark, M., Jennum, P. J., Leger, D., Nissen, C., Parrino, L., Paunio, T., Pevernagie, D., Verbraecken, J., et al. (2017). European guideline for the diagnosis and treatment of insomnia. Journal of Sleep Research, 26(6), 675–700. https://doi.org/10.1111/jsr.12594
Rigney, G., Ali, N. S., Corkum, P. V., Brown, C. A., Constantin, E., Godbout, R., Hanlon-Dearman, A., Ipsiroglu, O., Reid, G. J., Shea, S., Smith, I. M., Van der Loos, H. F. M., & Weiss, S. K. (2018). A systematic review to explore the feasibility of a behavioural sleep intervention for insomnia in children with neurodevelopmental disorders: A transdiagnostic approach. Sleep Medicine Reviews, 41, 244–254. https://doi.org/10.1016/j.smrv.2018.03.008
Rigney, G., Keys, E., Johnson, M., Paul, J., & Corkum, P. V. (2021). Sleep problems. In J. Allen, D. Hawes, & C. Essau (Eds.), Family intervention for specific child and adolescent mental health problems (pp. 191–206). Cambridge, Cambridge University Press. https://doi.org/10.1017/9781108682053.016
Roach, M., Juday, T., Tuly, R., Chou, J. W., Jena, A. B., & Doghramji, P. P. (2021). Challenges and opportunities in insomnia disorder. International Journal of Neuroscience, 131(11), 1058–1065. https://doi.org/10.1080/00207454.2020.1773460
Roenneberg, T. (2012). What is chronotype?: Preface. Sleep and Biological Rhythms, 10(2), 75–76. https://doi.org/10.1111/j.1479-8425.2012.00541.x
Roth, T., & Zinsenheim, J. (2009). Sleep in adults with ADHD and the effects of stimulants. Primary Psychiatry, 16(12), 32–37.
Rybak, Y. E., McNeely, H. E., Mackenzie, B. E., Jain, U. R., & Levitan, R. D. (2006). An open trial of light therapy in adult attention-deficit/hyperactivity disorder. The Journal of Clinical Psychiatry, 67(10), 1527–1535. https://doi.org/10.4088/JCP.v67n1006
Sadeh, A., Pergamin, L., & Bar-Haim, Y. (2006). Sleep in children with attention-deficit/hyperactivity disorder: A meta-analysis of polysomnographic studies. Sleep Medicine Reviews, 10(6), 381–398. https://doi.org/10.1016/j.smrv.2006.03.004
Salanitro, M., Wrigley, T., Ghabra, H., de Haan, E., Hill, C. M., Solmi, M., & Cortese, S. (2022). Efficacy on sleep parameters and tolerability of melatonin in individuals with sleep or mental disorders: A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 139, 104723. https://doi.org/10.1016/j.neubiorev.2022.104723
Saletin, J. M., Jackvony, S., Rodriguez, K. A., & Dickstein, D. P. (2018). A coordinate-based meta-analysis comparing brain activation between attention deficit hyperactivity disorder and total sleep deprivation. Sleep, 42(3), 1–9. https://doi.org/10.1093/sleep/zsy251
Sateia, M. J. (2014). International classification of sleep disorders-Third edition. Chest, 146(5), 1387–1394. https://doi.org/10.1378/chest.14-0970
Schinkelshoek, M. S., de Wit, K., Bruggink, V., Fronczek, R., & Lammers, G. J. (2020). Daytime sleep state misperception in a tertiary sleep centre population. Sleep Medicine, 69, 78–84. https://doi.org/10.1016/j.sleep.2019.12.026
Schreck, K. A. (2010). Sleep disorders the forgotten variable in behavior assessment: A guide for practitioners. Journal of Behavioral Health and Medicine, 1(1), 65–78. https://doi.org/10.1037/h0100542
Sciberras, E. (2022). Sleep in individuals with ADHD: Prevalence, impacts, causes, and treatments. In S. C. Stanford & E. Sciberras (Eds.), New discoveries in the behavioral neuroscience of attention-deficit hyperactivity disorder (Vol. 57, pp. 199–220). Springer International Publishing. https://doi.org/10.1007/7854_2022_336
Sedky, K., Bennett, D. S., & Carvalho, K. S. (2014). Attention deficit hyperactivity disorder and sleep disordered breathing in pediatric populations: A meta-analysis. Sleep Medicine Reviews, 18(4), 349–356. https://doi.org/10.1016/j.smrv.2013.12.003
Sen, T., & Spruyt, K. (2020). Pediatric sleep tools: An updated literature review. Frontiers in Psychiatry, 11, 317. https://doi.org/10.3389/fpsyt.2020.00317
Shahid, A., Wilkinson, K., Marcu, S., & Shapiro, C. M. (2012). STOP, THAT, and one hundred other sleep scales. Springer Science + Business Media.
Shen, C., Luo, Q., Chamberlain, S. R., Morgan, S., Romero-Garcia, R., Du, J., Zhao, X., Touchette, É., Montplaisir, J., Vitaro, F., Boivin, M., Tremblay, R. E., Zhao, X.-M., Robaey, P., Feng, J., & Sahakian, B. J. (2020). What is the link between attention-deficit/hyperactivity disorder and sleep disturbance? A multimodal examination of longitudinal relationships and brain structure using large-scale population-based cohorts. Biological Psychiatry, 88(6), 459–469. https://doi.org/10.1016/j.biopsych.2020.03.010
Shephard, E., Zuccolo, P. F., Idrees, I., Godoy, P. B. G., Salomone, E., Ferrante, C., Sorgato, P., Catão, L. F. C. C., Goodwin, A., Bolton, P. F., Tye, C., Groom, M. J., & Polanczyk, G. V. (2022). Systematic review and meta-analysis: The science of early-life precursors and interventions for attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 61(2), 187–226. https://doi.org/10.1016/j.jaac.2021.03.016
Silber, M. H., Buchfuhrer, M. J., Earley, C. J., Koo, B. B., Manconi, M., Winkelman, J. W., Earley, C. J., Becker, P., Berkowski, J. A., Buchfuhrer, M. J., Clemens, S., Connor, J. R., Ferré, S., Hensley, J. G., Jones, B. C., Karroum, E. G., Koo, B., Manconi, M., Ondo, W., et al. (2021). The management of restless legs syndrome: An updated algorithm. Mayo Clinic Proceedings, 96(7), 1921–1937. https://doi.org/10.1016/j.mayocp.2020.12.026
Snitselaar, M. A., Smits, M. G., & Spijker, J. (2016). Prevalence of restless legs syndrome in adult ADHD and its subtypes. Behavioral Sleep Medicine, 14(5), 480–488. https://doi.org/10.1080/15402002.2015.1018386
Snitselaar, M. A., Smits, M. G., van der Heijden, K. B., & Spijker, J. (2017). Sleep and circadian rhythmicity in adult ADHD and the effect of stimulants: A review of the current literature. Journal of Attention Disorders, 21(1), 14–26. https://doi.org/10.1177/1087054713479663
Speth, T. (2019). Impact of cumulative sleep restriction on sleep physiology in children with and without attention-deficit/hyperactivity disorder (ADHD). Dalhousie University. https://dalspace.library.dal.ca/bitstream/handle/10222/75455/Speth-Tamara-PhD-PSYO-April-2019.pdf?sequence=1&isAllowed=y
Spruyt, K., & Gozal, D. (2011). Pediatric sleep questionnaires as diagnostic or epidemiological tools: A review of currently available instruments. Sleep Medicine Reviews, 15(1), 19–32. https://doi.org/10.1016/j.smrv.2010.07.005
Sung, V., Hiscock, H., Sciberras, E., & Efron, D. (2008). Sleep problems in children with attention-deficit/hyperactivity disorder: Prevalence and the effect on the child and family. Archives of Pediatrics & Adolescent Medicine, 162(4), 336. https://doi.org/10.1001/archpedi.162.4.336
Tahmasian, M., Aleman, A., Andreassen, O. A., Arab, Z., Baillet, M., Benedetti, F., Bresser, T., Bright, J., Chee, M. W. L., Chylinski, D., Cheng, W., Deantoni, M., Dresler, M., Eickhoff, S. B., Eickhoff, C. R., Elvsåshagen, T., Feng, J., Foster-Dingley, J. C., Ganjgahi, H., et al. (2021). ENIGMA-sleep: Challenges, opportunities, and the road map. Journal of Sleep Research, 30(6). https://doi.org/10.1111/jsr.13347
Tan-MacNeill, K. M., Smith, I. M., Jemcov, A., Keeler, L., Chorney, J., Johnson, S., Weiss, S. K., Begum, E. A., Brown, C. A., Constantin, E., Godbout, R., Hanlon-Dearman, A., Ipsiroglu, O., Reid, G. J., Shea, S., & Corkum, P. V. (2020). Barriers and facilitators to treating insomnia in children with autism spectrum disorder and other neurodevelopmental disorders: Parent and health care professional perspectives. Research in Developmental Disabilities, 107, 103792. https://doi.org/10.1016/j.ridd.2020.103792
Tarakçıoğlu, M. C., Kadak, M. T., Gürbüz, G. A., Poyraz, B. Ç., Erdoğan, F., & Aksoy, U. M. (2018). Evaluation of the relationship between attention deficit hyperactivity disorder symptoms and chronotype. Archives of Neuropsychiatry, 55(1), 54–58. https://doi.org/10.29399/npa.18168
Tomaso, C. C., Johnson, A. B., & Nelson, T. D. (2021). The effect of sleep deprivation and restriction on mood, emotion, and emotion regulation: Three meta-analyses in one. Sleep: Journal of Sleep and Sleep Disorders Research, 44(6), 1–30. https://doi.org/10.1093/sleep/zsaa289
Tonetti, L., Natale, V., & Randler, C. (2015). Association between circadian preference and academic achievement: A systematic review and meta-analysis. Chronobiology International, 32(6), 792–801. https://doi.org/10.3109/07420528.2015.1049271
Tonetti, L., Conca, A., Giupponi, G., Filardi, M., & Natale, V. (2018). Circadian activity rhythm in adult attention-deficit hyperactivity disorder. Journal of Psychiatric Research, 103, 1–4. https://doi.org/10.1016/j.jpsychires.2018.05.002
Tseng, P.-T., Cheng, Y.-S., Yen, C.-F., Chen, Y.-W., Stubbs, B., Whiteley, P., Carvalho, A. F., Li, D.-J., Chen, T.-Y., Yang, W.-C., Tang, C.-H., Chu, C.-S., Yang, W.-C., Liang, H.-Y., Wu, C.-K., & Lin, P.-Y. (2018). Peripheral iron levels in children with attention-deficit hyperactivity disorder: A systematic review and meta-analysis. Scientific Reports, 8(1), 788. https://doi.org/10.1038/s41598-017-19096-x
van Andel, E., Bijlenga, D., Vogel, S. W. N., Beekman, A. T. F., & Kooij, J. J. S. (2021). Effects of chronotherapy on circadian rhythm and ADHD symptoms in adults with attention-deficit/hyperactivity disorder and delayed sleep phase syndrome: A randomized clinical trial. Chronobiology International, 38(2), 260–269. https://doi.org/10.1080/07420528.2020.1835943. APA PsycInfo.
van Andel, E., ten Have, M., Bijlenga, D., Beekman, A. T. F., de Graaf, R., & Sandra Kooij, J. J. (2022). Combined impact of ADHD and insomnia symptoms on quality of life, productivity, and health care use in the general population. Psychological Medicine, 52(1), 36–47. https://doi.org/10.1017/S0033291720001592
Van der Heijden, K. B., Smits, M. G., Van Someren, E. J. W., & Gunning, W. B. (2005). Idiopathic chronic sleep onset insomnia in attention-deficit/hyperactivity disorder: A circadian rhythm sleep disorder. Chronobiology International, 22(3), 559–570. https://doi.org/10.1081/CBI-200062410
Van der Heijden, K. B., Smits, M. G., Van Someren, E. J. W., Ridderinkhof, K. R., & Gunning, W. B. (2007). Effect of melatonin on sleep, behavior, and cognition in ADHD and chronic sleep-onset insomnia. Journal of the American Academy of Child & Adolescent Psychiatry, 46(2), 233–241. https://doi.org/10.1097/01.chi.0000246055.76167.0d
van Geijlswijk, I. M., Korzilius, H. P. L. M., & Smits, M. G. (2010). The use of exogenous melatonin in delayed sleep phase disorder: A meta-analysis. Sleep, 33(12), 1605–1614. https://doi.org/10.1093/sleep/33.12.1605
van Straten, A., van der Zweerde, T., Kleiboer, A., Cuijpers, P., Morin, C. M., & Lancee, J. (2018). Cognitive and behavioral therapies in the treatment of insomnia: A meta-analysis. Sleep Medicine Reviews, 38, 3–16. https://doi.org/10.1016/j.smrv.2017.02.001
Van Veen, M. M., Kooij, J. J. S., Boonstra, A. M., Gordijn, M. C. M., & Van Someren, E. J. W. (2010). Delayed circadian rhythm in adults with attention-deficit/hyperactivity disorder and chronic sleep-onset insomnia. Biological Psychiatry, 67(11), 1091–1096. https://doi.org/10.1016/j.biopsych.2009.12.032
Vogel, S. W. N., Bijlenga, D., Benjamins, J. S., Beekman, A. T. F., Kooij, J. J. S., & Van Someren, E. J. W. (2017). Attention deficit hyperactivity disorder symptom severity and sleep problems in adult participants of the Netherlands sleep registry. Sleep Medicine, 40, 94–102. https://doi.org/10.1016/j.sleep.2017.09.027
Vriend, J. L., Davidson, F. D., Corkum, P. V., Rusak, B., Chambers, C. T., & McLaughlin, E. N. (2013). Manipulating sleep duration alters emotional functioning and cognitive performance in children. Journal of Pediatric Psychology, 38(10), 1058–1069. https://doi.org/10.1093/jpepsy/jst033
Waldon, J., Begum, E., Gendron, M., Rusak, B., Andreou, P., Rajda, M., & Corkum, P. (2016). Concordance of actigraphy with polysomnography in children with and without attention-deficit/hyperactivity disorder. Journal of Sleep Research, 25(5), 524–533. https://doi.org/10.1111/jsr.12402
Walters, A. S., Mandelbaum, D. E., Lewin, D. S., Kugler, S., England, S. J., & Miller, M. (2000). Dopaminergic therapy in children with restless legs/periodic limb movements in sleep and ADHD. Pediatric Neurology, 22(3), 182–186. https://doi.org/10.1016/S0887-8994(99)00152-6
Wang, Y., Peng, S., Liu, T., Zhang, Y., Li, H., Li, X., Tao, W., & Shi, Y. (2020). The potential role of clock genes in children attention-deficit/hyperactivity disorder. Sleep Medicine, 71, 18–27. https://doi.org/10.1016/j.sleep.2020.02.021
Weiss, M. D., Ivabebko, A., & McBridfe, N. M. (2019). Assessing sleep problems in ADHD. In H. Hiscock & E. Sciberras (Eds.), Sleep and ADHD. An evidence-based guide to assessment and treatment (1st ed.). Elsevier Academic Press.
Wells, M. E., & Vaughn, B. V. (2012). Poor sleep challenging the health of a nation. The Neurodiagnostic Journal, 52(3), 233–249. https://doi.org/10.1080/21646821.2012.11079859
Wiggs, L. D. (2019). Epidemiology and etiology of behavioral insomnias, circadian rhythm disorders, and parasomnias in ADHD. In H. Hiscock & E. Sciberras (Eds.), Sleep and ADHD: An evidence-based guide to assessment and treatment (2019-25191-003; pp. 63–93). Elsevier Academic Press; APA PsycInfo. https://doi.org/10.1016/B978-0-12-814180-9.00003-X
Womack, S. D., Hook, J. N., Reyna, S. H., & Ramos, M. (2013). Sleep loss and risk-taking behavior: A review of the literature. Behavioral Sleep Medicine, 11(5), 343–359. https://doi.org/10.1080/15402002.2012.703628
Wu, J., Gu, M., Chen, S., Chen, W., Ni, K., Xu, H., & Li, X. (2017). Factors related to pediatric obstructive sleep apnea–hypopnea syndrome in children with attention deficit hyperactivity disorder in different age groups. Medicine, 96(42), e8281. https://doi.org/10.1097/MD.0000000000008281
Yilbas, B., Ozturk, H. I., & Karadeniz, P. G. (2022). The relationship of chronotypes with food addiction, impulsivity, and attention deficit hyperactivity disorder symptoms in a sample of undergraduate university students. Chronobiology International, 39(10), 1389–1398. https://doi.org/10.1080/07420528.2022.2109483
Yoon, S. Y. R., Jain, U., & Shapiro, C. (2012). Sleep in attention-deficit/hyperactivity disorder in children and adults: Past, present, and future. Sleep Medicine Reviews, 16(4), 371–388. https://doi.org/10.1016/j.smrv.2011.07.001
Zhang, Y., Ren, R., Yang, L., Zhang, H., Shi, Y., Shi, J., Sanford, L. D., Lu, L., Vitiello, M. V., & Tang, X. (2022). Comparative efficacy and acceptability of psychotherapies, pharmacotherapies, and their combination for the treatment of adult insomnia: A systematic review and network meta-analysis. Sleep Medicine Reviews, 65, 101687. https://doi.org/10.1016/j.smrv.2022.101687
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Corkum, P., Bertrand, M., Ilie, A., Rajda, M. (2023). ADHD and Sleep Problems. In: Matson, J.L. (eds) Clinical Handbook of ADHD Assessment and Treatment Across the Lifespan. Autism and Child Psychopathology Series. Springer, Cham. https://doi.org/10.1007/978-3-031-41709-2_10
Download citation
DOI: https://doi.org/10.1007/978-3-031-41709-2_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-41708-5
Online ISBN: 978-3-031-41709-2
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)