Abstract
Evaluation and comparison of incidence and prevalence of noncommunicable diseases (NCDs) among sexual and gender minorities (SGMs) to cisgender and/or heterosexual populations rest on the belief that SGM populations have unique characteristics that influence the rates. Several theoretical concepts, briefly discussed in this chapter, have been postulated regarding this disparity. These include minority stress theory, fundamental cause theory, compression of morbidity theory, and cumulative disadvantage hypothesis. In each case, and most clearly articulated by the fundamental cause theory, structural stigma, discrimination, and power structures among disadvantaged populations drive these health disparities. In the analyses evaluating health disparities, numerous methodological issues reduce the generalizability of results. Probabilistic-based sampling design is rarely used because the data do not exist. Among the few examples that use this study design, the SGM sample is small or covers multiple years. Another methodological issue is the consistently younger mean age of the SGM participants compared to cisgender and/or heterosexual groups. Across the globe, country-specific cultural norms determine the visibility and value of SGM populations. Moving forward, a hope is that, in the near future, the SGM population will be described as one important group, among others, in assessing the health of each nation.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Noncommunicable diseases
- Sexual minority
- Transgender
- Minority stress theory
- Fundamental cause theory
- Compression of morbidity theory
- Cumulative disadvantage hypothesis
- Chronic stress
- Immune dysregulation
- Methodological issues
4.1 Introduction
Globalization, often narrowly defined as the increasing integration of the world’s economies, has aspects beyond economic factors, including technological, political, social, scientific, and cultural phenomena (Huynen et al., 2005). The sociocultural dimension is particularly germane to the discussion of noncommunicable diseases (NCDs or physical chronic conditions) among sexual and gender minorities (SGMs) that will be discussed in the next chapter. In the twentieth century, scholars in sexuality and nationalism presented alternatives to the beliefs that sexuality is “private,” apolitical, sinful (according to religious authorities), or deviant (according to mental health experts) (Foucault, 1984; Rosario et al., 2002).
One alternative perspective uses the concept of sexual scripts to understand the three interrelated categories of human sexuality: attraction, behavior, and identity (i.e., orientation) (Seidman, 2003). This idea can also be extended to gender scripts, such as ones related to gender as binary, linked to anatomical features, and fixed at birth. This perspective argues that sexual and gender scripts that people use are rooted within each nation’s establishments, such as churches, schools, and laws, and are implemented by socializing agents, such as religious leaders, peers, and the media (Stambolis-Ruhstorfer, 2017). SGMs living in places or within racial/ethnic groups where the scripts associated with SGM identity, behaviors, and/or attraction are nonexistent, associated with allegations of not being legitimate, or depicted as an inherent erotic, racially centric characteristic have ramifications on characterizing the health of SGM people (Carrillo & Fontdevila, 2014; Decena, 2011; Epstein & Carrillo, 2014; Provencher, 2016). Specifically, these scripts reduce the likelihood of describing NCD outcomes for these populations due to receiving low or no priority in scientific and medical research.
Not only is globalization a multidimensional phenomenon, but contemporary global health issues have moved from an emphasis on the health burden tied to infectious disease to that of NCDs. In the twenty-first century, cardiovascular disease, cancer, diabetes mellitus, and chronic respiratory diseases are associated with 71% of all premature deaths worldwide. Among those aged 30–69 years, over 85% of premature deaths linked to these health conditions occur in low- and middle-income countries (Adeyi et al., 2007; Lopez et al., 2006; World Health Organization, 2005, 2018). Extensive evaluation and modeling of mortality patterns by the Global Burden of Disease Study demonstrated that some NCDs topping the list as leading regional contributors of years of lost life (YLLs: a standard metric for mortality studies) also showed considerable intraregional differences based on a composite sociodemographic index as well as between subpopulations; this index is comprised of the geometric mean of income per capita, educational attainment, and total fertility rate in the current year (GBD 2017 Disease and Injury Incidence Prevalence Collaborators, 2018). To illustrate, NCD burden in New Zealand (NZ) has significant variation between indigenous Polynesian people of NZ (i.e., Maori) compared to non-Maori populations (GBD 2017 Disease and Injury Incidence Prevalence Collaborators, 2018). This finding highlights the importance of recognizing that the prevalence of NCDs by region or within countries in which SGM-specific data are unavailable may not accurately represent SGM’s health status in those places.
A parallel metric to capture disease burden is disability-adjusted life year (DALY), which adds both years of life lost (YLLs) and years lived with disability (YLDs) (Murray et al., 2012). This metric was developed in the 1990s specifically to compare national health burden around the world, as it is an acceptable measure of the effects of chronic illness on population health burden (Murray, 1994). As the selected NCDs described in the next chapter contribute to premature death and/or disability, especially in countries with limited health interventions, this metric is particularly valuable. According to the Global Burden of Disease Study, which analyzed and modeled data to describe the burden of both communicable and noncommunicable diseases in 195 countries and territories, NCDs contributed an estimated 54% of the DALYs in 2010, with 25.3% by the selected five NCDs (i.e., cardiovascular diseases (CVD), including strokes, at 11.8%, cancer at 7.6%, diabetes mellitus at 1.9%, asthma at 0.9%, COPD at 3.1%) (Murray, 1994).
4.2 On the Impact of COVID-19
The COVID-19 pandemic links both infections from a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with NCDs. First detected in Wuhan, China in December 2019, the World Health Organization declared COVID-19 a pandemic on March 11, 2020 (Neher et al., 2020; Zhou et al., 2020). A higher risk of severe COVID-19 disease is experienced by two groups of people; adults aged 65 years or older and people with underlying medical conditions, such as those NCDs described in the subsequent chapter (CVD, cancer, diabetes, asthma, and COPD) (Azarpazhooh et al., 2020). Among younger patients diagnosed with COVID-19 (18–49 years), obesity, underlying chronic lung disease (primarily asthma), and diabetes are the most prevalent chronic disorders (Stokes et al., 2020). According to Clark and colleagues, among the global population, countries with older populations, African countries with high HIV/AIDS prevalence, and small island nations with high diabetes prevalence are estimated to be at the highest increased risk for severe COVID-19 illness (Clark et al., 2020). No research has addressed the impact of the COVID-19 pandemic on gender minority populations with NCDs. Some work has been done to characterize reduced access to gender-affirming services, including one study with a global sample of 849 transgender and non-binary people representing Europe (n = 382), Southeast Asia (n = 215), the Americas (n = 81), Eastern Mediterranean (n = 76), Western Pacific (n = 40), and Africa (n = 31). The authors found reduced access to gender-affirming services as well as increased levels of anxiety and depression among their sample (Restar et al., 2021). Unfortunately, at the writing of this chapter, no studies have reported on SGM individuals’ risk for severe COVID-19, though it is possible that multiple syndemic factors may increase this population’s risk of exposure (Cahill et al., 2020).
4.3 Chronic Stress and Immune Dysregulation
Segerstrom and Miller evaluated over 300 studies and concluded that chronic stress was associated with numerous measures of immune dysregulation, such as inflammatory engagement and poor antibody responses (Segerstrom & Miller, 2004). However, inconsistent results using biological markers of stress, such as cortisol or C-reactive protein levels, comparing SGM and non-SGM participants have been published with virtually all of these data from developed countries (Austin et al., 2016; Cohen et al., 2017; DuBois et al., 2017; Huebner & Davis, 2005; Juster et al., 2013, 2015). As noted by Segerstrom and Miller, many studies suffer from methodological limitations in sampling with a variety of biomarkers used to signal stress which adds uncertainty to understanding the stress response (Segerstrom & Miller, 2004).
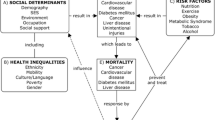
4.4 Factors Contributing to Chronic Illnesses
Since the major causes and/or significant risk factors of the leading NCDs are known, approximately 60% of these deaths are preventable. For example, the Oxford Health Alliance (OHS) developed a conceptual model called “4four60” to support effective communication on the prevention of NCDs. They link four risk factors (poor diet, physical inactivity, tobacco use, and excess alcohol consumption) known to be associated with four leading NCDs (cardiovascular disease, cancer, diabetes, and chronic lung disease) to the contribution of 60% of all global premature deaths (Colagiuri et al., 2007). Both poor diet and physical inactivity in association with these NCDs are often associated with high body mass index (BMI). As a sidenote, BMI is often used as a standardized and convenient method to classify people into weight categories, though numerous limitations have been reported in using this metric (Nuttall, 2015). In a systematic review comparing BMI, waist circumference, and waist-to-height ratio (WHtR) measurements to visceral adipose tissue (VAT) measurement, waist circumference and WHtR were better predictors of VAT than BMI (Browning et al., 2010). Using indexes that account for body fat distribution such as waist-to-hip or WHtR ratio, intra-abdominal fat depot volume, or waist-to-height ratio provides a more accurate means of risk assessment associated with obesity.
Regarding dietary choices, a significant downstream effect of globalization is the unprecedented increase in the global food trade, which has been dominated by large transnational companies (Pang & Guindon, 2004). Global brand names and aggressive marketing strategies have adapted to local environments such that recognition of brand names of popular beverages and fast foods has been especially rapid (Chopra et al., 2002). This situation has contributed to the global epidemic of obesity by replacing traditional diets with fat- and calorie-rich foods (Gakidou et al., 2017). The results from the Global Burden of Disease study on high BMI found 12% of the adult population (603.7 million adults; 95% uncertainty interval: 592.9 to 615.6) were obese worldwide with a consistently higher prevalence of obesity among women. In 2015, high BMI contributed to deaths from any cause worldwide at 7.1% (95% uncertainty interval: 4.9 to 9.6) with obesity-related cardiovascular disease and diabetes as leading causes of these mortality statistics (Afshin et al., 2017). Beyond mere statistics, the threats to population health in many LMICs are occurring on two fronts simultaneously: “In the slums of today’s megacities, we are seeing NCDs caused by unhealthy diets and habits, side by side with undernutrition” according to former Director-General of World Health Organization, Dr. Gro Harlem Brundtland (World Health Organization, 2002, p. x).
Although considerable data have been compiled with recent excellent work by the Global Burden of Disease study (Benziger et al., 2016), sparse data are available to address the question of the burden of NCDs among sexual and gender minority (SGM) populations. SGMs in some parts of the world, where data are available, have a higher prevalence of known risk factors (as detailed by the aforementioned “4for60” model) associated with leading NCDs. For example, in a systematic review of literature, Eliason and colleagues reported that lesbian and bisexual women had a higher prevalence of a BMI over 30 compared to heterosexual women (Eliason et al., 2015); however, of the 20 studies included, only two (Australia and Great Britain) were outside of the USA, thus limiting the global picture. Similarly, some studies in the USA have suggested a higher prevalence of overweight but not obese status among transmasculine individuals compared to cisgender women (Caceres et al., 2019; Reisner et al., 2013).
A fundamental question that remains largely unanswered is whether factors related to SGM status, and perhaps the synergistic or syndemic effects between SGM status and health-related behaviors (e.g., unhealthy weight, smoking, excessive alcohol consumption), are associated with an increased prevalence of NCDs among SGMs (Coulter et al., 2015). For example, in Western countries, the minority stress model is often used to help explain health disparities experienced by SGMs, with similar stressors identified in other counties (Bowling et al., 2018; Kontos et al., 2011; Laćan, 2015; Lobato et al., 2019; Mahdavi, 2019).
To understand this issue, extramural funding and/or intramural funding priorities are critical. Perhaps a systematic bias in selecting grant proposals worthy of funding or considering SGM issues beyond HIV/AIDS research is due to (unconscious) bias. Historically, bias in US National Institutes of Health (NIH) funding (Kaiser, 2011) culminated in NIH mandating justification for studies if women and minority groups (race/ethnicity) were not included. It is not unreasonable to consider bias as a factor in funding focused on SGM issues. The catch-22 of rejections in grant applications, particularly in the USA and other countries in which extramural funding is expected of researchers, is that young researchers will either move on to more fundable opportunities with a non-SGM focus, since successful funding is necessary for tenure and promotion or move out of the research arena entirely.
4.5 Health Disparity Theories
A recent study in Sweden tested another related hypothesis to explain health disparities faced by SGMs, called the fundamental cause theory (Branstrom et al., 2016). In a comparison of advantaged (heterosexuals) and disadvantaged (SGMs) groups, they found the prevalence of high-preventable diseases—ones that could be prevented or effectively treated—was significantly higher among SGMs. They posit that for preventable diseases, disadvantaged groups cannot leverage the resources necessary (i.e., knowledge, prestige, power, or supportive social connections) to achieve healthy outcomes. To bolster this theory, analysis of low-preventable diseases—ones that cannot be effectively prevented or cured—had similar outcomes between the two groups (Branstrom et al., 2016). Although this study provides evidence that a true health disparity for NCDs may exist for the SGM population that cannot be explained by an increased prevalence of established risk factors linked to these NCDs, we are still left with a very difficult construct to assess and compare across countries. Further, the validity of the construct has not been tested, although tangential information partially supports the fundamental cause theory (Branstrom et al., 2016). For example, in Niger, general population patients were typically viewed as passive or without a “voice” by their local nurse, and therefore obtaining services beyond the local health centers rarely occurred. One could extrapolate this characteristic to SGM individuals in which presumably their lower prestige and/or power could limit optimizing their health-seeking behavior (Bossyns & Van Lerberghe, 2004).
National legislation and political rhetoric can also have the effect of reduced privilege and/or power for SGM citizens (see Stigma chapter, Chap. 2), which can create dissonance between one’s personal self and one’s national self and likely engenders a sense of powerlessness. Alternatively, some countries, such as Canada, Spain, and the Netherlands, embrace SGM rights as a key characteristic of national belonging (Stambolis-Ruhstorfer, 2017). However, the intersection of SGM identity and nationalism ideology can also create discordance (“Muslim and gay: seeking identity coherence in New Zealand,” 2016). For SGMs who also identify with other ethnicities, such as a Muslim with family from Iran (known for its extreme anti-gay laws), national rhetoric from any country that supports SGM rights may require its citizens to reject or renounce their ethnic communities in order to gain acceptance; thus, these individuals may experience one aspect of their identity being pitted against another aspect of their identity. These situations could have a negative influence on their health either from a stigmatizing position (i.e., minority stress theory (Meyer, 2003)) or an inability to leverage necessary resources to optimize health (i.e., fundamental cause theory). Regardless of the source of such disparities, it is critical to characterize potential sources that create dissonance so that the health of SGM populations can be better understood and disparities addressed across various healthcare delivery systems.
Two theories have been suggested regarding aging, health disparity, and NCD prevalence. Compression of morbidity theory for health disparities posits that with increasing years lived, the disparity gap narrows since only the hardiest individuals survive (Beckett, 2000; House et al., 2005). On a global scale, countries first need to achieve a more equal comparison of three domains before the hardiest individuals would have the opportunity to survive. One domain is for countries to transition more fully from health outcomes based on injury/violence, infection, and maternal/perinatal/nutritional issues to NCDs, known as the epidemiological transition (Omran, 2005). To illustrate, sub-Saharan Africa (of 48 countries) has the highest under-five mortality rate (1 in 13 births) and modest life expectancy of 61 years (range: 52 years in the Central African Republic to 74 years in Mauritius) versus Australia and New Zealand with the lowest mortality rate (1 in 263 births) and a life expectancy of 82 years (World Bank Group, 2019; United Nations Inter-agency Group for Child Mortality Estimation, 2018). A second domain is achieving a relatively equable performance of the country’s health system to treat medical conditions including NCDs, thereby supporting the potential for an aging population (Gordon-Larsen et al., 2000; Schutte et al., 2018). The third domain encompasses similar NCD risk-attributable burden (i.e., tobacco use, excessive alcohol consumption, obesity, and inactivity) at the population level among the countries (GBD 2017 Disease and Injury Incidence Prevalence Collaborators, 2018). For example, worldwide, the age-standardized prevalence of daily smoking was 25% (95% uncertainty interval 24.2–25.7) for men and 5.4% (5.1–5.7) for women. However, wide variability exists globally, with half the population smoking in Greenland (women at 44% and men at 43%) compared to rare smoking behavior in Sudan (women at 0.4% and men at 1.3%) (Reitsma et al., 2017).
The second theory, the cumulative disadvantage hypothesis, advocates the opposite—a widening of the health disparity gap due to the accumulation of burden over time (Dupre, 2007; Kim & Durden, 2007; Lauderdale, 2001). The concept of chronic stress experienced by SGM individuals over a lifetime translates into the wearing down of biological coping systems and thereby results in an increased prevalence of NCDs per this hypothesis (Schneiderman et al., 2005). As with the first theory, applying this hypothesis on a global scale requires more equable treatment of SGM populations worldwide. As explored in the Stigma chapter (Chap. 2), there is considerable variability in how the people and institutions within any country accept and embrace SGM citizens. Establishing the prevalence of NCDs over the life course among sexual and gender minorities compared to heterosexual groups can provide support for one of these theories within individual countries. From a global perspective, further narrowing of differences among countries on aforementioned health domains as well as capturing data on SGM populations will provide evidence regarding the health of SGMs worldwide.
4.6 Methodological Considerations
Regardless of a potential mechanism(s) underpinning differences in NCD prevalence, systems have to be in place to detect such a potential difference. Much of health research is guided by opportunities either directly through funding initiatives or through agency/organization’s priorities, and a critical component in being selected as a research priority lies in the generalizability of results. Two critical components of the generalizability of results are determined from a sufficient sample size and the use of probability-based sampling of participants. Sexual minorities (SM) comprise 6–14% of the global population (Rahman et al., 2020). The visible (“out”) number of SM individuals comprises a sufficiently large group to warrant inclusion on national NCD surveillance surveys with the caveat that up to 83% of SM individuals, globally, may conceal their identity from most or all others (Pachankis & Branstrom, 2019). This concealment means their perspectives may not be represented in NCD prevalence and incidence statistics and therefore reduces the generalizability of the study results. Alternatively, estimates of the global prevalence of transgender identity range from 0.3 to 0.5% (Gender Identity in US Surveillance (GenIUSS) Group, 2014; Reisner et al., 2016) and vary depending on how transgender identity is defined (Collin et al., 2016; Reisner et al., 2016). According to Collin and colleagues, the prevalence estimates vary by degree of medical intervention with surgical or gender-affirming hormonal therapy (GAHT: i.e., estrogen and testosterone supplementation) or transgender-related diagnoses versus self-reported transgender identity (Collin et al., 2016). For the former, estimates range from 1 to 30 per 100,000 (0.001–0.03%) persons, and the latter is 100–700 per 100,000 (0.1–0.7%) (Collin et al., 2016; Peitzmeier, 2013). Although transgender identity prevalence seems to be increasing over time (Ahmadzad-Asl et al., 2010; Blosnich et al., 2013; Eklund et al., 1988; Kauth et al., 2014; Meier & Labuski, 2013), one limitation in understanding NCD issues among transgender populations is the relatively small sample size that would be captured on any national surveillance study. Unless intentional over-sampling of the transgender population is implemented, a small sample size will limit reporting outcomes among this population in large surveillance studies. Finally, for both the SM and transgender populations, participation in research is voluntary. Therefore, until it is safe and acceptable for individuals to disclose their SGM status, it is unlikely that estimates of NCD prevalence will capture the true state of health among these populations.
A second strong element in the generalizability of study results is the use of probability-based sampling as opposed to convenience sampling. A mantra often used by SGM researchers advocating inclusion of sexual orientation/gender identity (SOGI) questions on surveillance surveys is, “If you don’t ask, you don’t count.” Probability-based sampling requires a list of all eligible participants from which a random sample is selected. Unless these identities are collected in a similar manner as other commonly acquired demographics such as age, marital status, race/ethnicity/nationality, and educational attainment, researchers will be hampered in designing studies that accurately reflect the state of SGM health. For NCD research, these two components are critical for credible research findings. One objective downstream effect of these elements of scientific rigor determines which countries contribute to the SGM research agenda as described in the next chapter.
Another important aspect of SGM research associated with the prevalence of NCDs is age. For transgender health research, virtually no NCD research has been done to explore the health impact of age of medical affirming interventions, GAHT use, and experience of gender dysphoria. Among those who have medical affirming interventions, these three characteristics are likely to vary with age. For example, in a small cohort of transfeminine patients aged 19–66 years who were undergoing gender-affirming surgery in Germany, the reported age of gender dysphoria was between 4 and 63 years. Age of GAHT use for this cohort was not provided for individual participants but was between 18 and 63 years (Zavlin et al., 2019). In general, most NCD findings have been reported without details on these three characteristics (Goodman & Nash, 2018). For SM individuals, status is more fluid across the lifespan without clear patterns of stability at any age cohort (Morgan, 2013). For example, about two-thirds of participants aged 36–50 (n = 762) reported a shift in sexual orientation labels over time (Kinnish et al., 2005), and very little is known about the health impact of changing sexual orientation labels as one ages. In a systematic review of national, international, state, and regional health surveillance data sources that capture SOGI information, Patterson et al. (2017) reported substantial gaps in the SM measurement of older adults. As most NCDs selected for the study are age-dependent, this age discrepancy limits the quality of health surveillance results since extrapolation of younger SM health may not reflect older SM health (Patterson et al., 2017).
4.7 Conclusion
The forces shaping the mere ability to acknowledge, enumerate, and engage SGM populations across the globe are ever-changing and heavily influenced by country-specific cultural norms. Further, a lack of security is felt by many SGMs locally due to structural stigma, outright violence, and discrimination, as well as local laws and political rhetoric, which lends itself to the SGM population remaining difficult to identify. With the pressures of globalization weighing strongly on the burden of NCDs across the globe, it is critical to accurately capture the SGM population’s similarity or divergence from regional NCD patterns. The path forward is fraught with competing tensions that make the gold standards of universal acceptance of this population as well as data collection currently unattainable. In the interim, it behooves researchers across the globe to proactively include SGM populations in their research agenda. The first step is to consistently incorporate answer options to the question on gender that includes gender options beyond male/female as well as asking specifically about sexual orientation (Brown & Herman, 2020; Gender Identity in US Surveillance (GenIUSS) Group, 2014; Sexual Minority Assessment Research Team (SMART), 2009). Ultimately, we return to a concluding point: “If you don’t ask, you don’t count” and a hope that, in the near future, the SGM population will be counted in assessing the health of each nation.
References
Adeyi, O., Smith, O., & Robles, S. (2007). Public policy and the challenge of chronic noncommunicable diseases. The World Bank.
Afshin, A., Forouzanfar, M. H., Reitsma, M. B., Sur, P., Estep, K., Lee, A., et al. (2017). Health effects of overweight and obesity in 195 countries over 25 years. New England Journal of Medicine, 377(1), 13–27. https://doi.org/10.1056/NEJMoa1614362
Ahmadzad-Asl, M., Jalali, A. H., Alavi, K., Naserbakht, M., Taban, M., Mohseninia-Omrani, K., & Eftekhar, M. (2010). The epidemiology of transsexualism in Iran. Journal of Gay & Lesbian Mental Health, 15(1), 83–93. https://doi.org/10.1080/19359705.2011.530580
Austin, A., Herrick, H., & Proescholdbell, S. (2016). Adverse childhood experiences related to poor adult health among lesbian, gay, and bisexual individuals. American Journal of Public Health, 106(2), 314–320. https://doi.org/10.2105/AJPH.2015.302904
Azarpazhooh, M. R., Morovatdar, N., Avan, A., Phan, T. G., Divani, A. A., Yassi, N., et al. (2020). COVID-19 pandemic and burden of non-communicable diseases: An ecological study on data of 185 countries. Journal of Stroke and Cerebrovascular Diseases, 29(9), 105089. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105089
Beckett, M. (2000). Converging health inequalities in later life—An artifact of mortality selection. Journal of Health and Social Behavior, 41(1), 106–119.
Benziger, C. P., Roth, G. A., & Moran, A. E. (2016). The global burden of disease study and the preventable burden of NCD. Global Heart, 11(4), 393–397. https://doi.org/10.1016/j.gheart.2016.10.024
Blosnich, J. R., Brown, G. R., Shipherd, J. C., Kauth, M., Piegari, R. I., & Bossarte, R. M. (2013). Prevalence of gender identity disorder and suicide risk among transgender veterans utilizing veterans’ health administration care. American Journal of Public Health, 103(10), e27–e32. https://doi.org/10.2105/AJPH.2013.301507
Bossyns, P., & Van Lerberghe, W. (2004). The weakest link: Competence and prestige as constraints to referral by isolated nurses in rural Niger. Human Resources for Health, 2(1), 1. https://doi.org/10.1186/1478-4491-2-1
Bowling, J., Dodge, B., Banik, S., Bartelt, E., Rawat, S., Guerra-Reyes, L., et al. (2018). A multi-method study of health behaviours and perceived concerns of sexual minority females in Mumbai, India. Sexual Health, 15(1), 29–38. https://doi.org/10.1071/sh17042
Branstrom, R., Hatzenbuehler, M. L., & Pachankis, J. E. (2016). Sexual orientation disparities in physical health: Age and gender effects in a population-based study. Social Psychiatry and Psychiatric Epidemiology, 51(2), 289–301. https://doi.org/10.1007/s00127-015-1116-0
Brown, T. N., & Herman, J. (2020). Exploring international priorities and best practices for the collection of data about gender minorities: A focus on South America. Accessed 20 Nov 2022. https://williamsinstitute.law.ucla.edu/publications/gender-minority-data-south-am/
Browning, L. M., Hsieh, S. D., & Ashwell, M. (2010). A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 05 could be a suitable global boundary value. Nutrition Research Reviews, 23(2), 247–269. https://doi.org/10.1017/S0954422410000144
Caceres, B. A., Jackman, K. B., Edmondson, D., & Bockting, W. O. (2019). Assessing gender identity differences in cardiovascular disease in US adults: An analysis of data from the 2014-2017 BRFSS. Journal of Behavioral Medicine, 43, 329–338. https://doi.org/10.1007/s10865-019-00102-8
Cahill, S., Grasso, C., Keuroghlian, A., Sciortino, C., & Mayer, K. (2020). Sexual and gender minority health in the COVID-19 pandemic: Why data collection and combatting discrimination matter now more than ever. American Journal of Public Health, 110(9), 1360–1361. https://doi.org/10.2105/AJPH.2020.305829
Carrillo, H., & Fontdevila, J. (2014). Border crossings and shifting sexualities among Mexican gay immigrant men: Beyond monolithic conceptions. Sexualities, 17(8), 919–938. https://doi.org/10.1177/1363460714552248
Chopra, M., Galbraith, S., & Darnton-Hill, I. (2002). A global response to a global problem: The epidemic of overnutrition. Bulletin of the World Health Organization, 80(12), 952–958.
Clark, A., Jit, M., Warren-Gash, C., Guthrie, B., Wang, H. H., Mercer, S. W., et al. (2020). Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: A modelling study. Lancet Global Health, 8(8), e1003–e1017. https://doi.org/10.1016/S2214-109X(20)30264-3
Cohen, S. A., Cook, S. K., Kelley, L., Foutz, J. D., & Sando, T. A. (2017). A closer look at rural-urban health disparities: Associations between obesity and rurality vary by geospatial and sociodemographic factors. Journal of Rural Health, 33(2), 167–179. https://doi.org/10.1111/jrh.12207
Colagiuri, R., Pramming, S., & Leeder, S. R. (2007). The Oxford Health Alliance: A risky business? Medical Journal of Australia, 187(11–12), 652–653. https://doi.org/10.5694/j.1326-5377.2007.tb01461.x
Collin, L., Reisner, S. L., Tangpricha, V., & Goodman, M. (2016). Prevalence of transgender depends on the "case" definition: A systematic review. Journal of Sexual Medicine, 13(4), 613–626. https://doi.org/10.1016/j.jsxm.2016.02.001
Coulter, R. W., Kinsky, S. M., Herrick, A. L., Stall, R. D., & Bauermeister, J. A. (2015). Evidence of syndemics and sexuality-related discrimination among young sexual-minority women. LGBT Health, 2(3), 250–257. https://doi.org/10.1089/lgbt.2014.0063
Decena, C. U. (2011). Tacit subjects: Belonging and same-sex desire among Dominican immigrant men. Duke University Press.
DuBois, L. Z., Powers, S., Everett, B. G., & Juster, R. P. (2017). Stigma and diurnal cortisol among transitioning transgender men. Psychoneuroendocrinology, 82, 59–66. https://doi.org/10.1016/j.psyneuen.2017.05.008
Dupre, M. E. (2007). Educational differences in age-related patterns of disease: Reconsidering the cumulative disadvantage and age-as-leveler hypotheses. Journal of Health and Social Behavior, 48(1), 1–15. https://doi.org/10.1177/002214650704800101
Eklund, P. L., Gooren, L. J., & Bezemer, P. D. (1988). Prevalence of transsexualism in The Netherlands. British Journal of Psychiatry, 152, 638–640. https://doi.org/10.1192/bjp.152.5.638
Eliason, M. J., Ingraham, N., Fogel, S. C., McElroy, J. A., Lorvick, J., Mauery, D. R., & Haynes, S. (2015). A systematic review of the literature on weight in sexual minority women. Women’s Health Issues, 25(2), 162–175. https://doi.org/10.1016/j.whi.2014.12.001
Epstein, S., & Carrillo, H. (2014). Immigrant sexual citizenship: Intersectional templates among Mexican gay immigrants to the USA. Citizenship Studies, 18(3–4), 259–276. https://doi.org/10.1080/13621025.2014.905266
Foucault, M. (1984). The history of sexuality: Volume 1 an introduction (R. Hurley, Trans.). Penguin Random House.
Gakidou, E., Afshin, A., Abajobir, A. A., Abate, K. H., Abbafati, C., Abbas, K. M., et al. (2017). Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet, 390(10100), 1345–1422. https://doi.org/10.1016/S0140-6736(17)32366-8
GBD 2017 Disease and Injury Incidence Prevalence Collaborators. (2018). Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet, 392(10159), 1789–1858. https://doi.org/10.1016/S0140-6736(18)32279-7
Gender Identity in U.S. Surveillance (GenIUSS) Group. (2014). Best practices for asking questions to identify transgender and other gender minority respondents on population-based surveys. Accessed 20 Nov 2022. https://williamsinstitute.law.ucla.edu/wp-content/uploads/geniuss-report-sep-2014.pdf
Goodman, M., & Nash, R. (2018). Examining health outcomes for people who are transgender. Patient-Centered Outcomes Research Institute. https://doi.org/10.25302/2.2019.AD.12114532
Gordon-Larsen, P., McMurray, R. G., & Popkin, B. M. (2000). Determinants of adolescent physical activity and inactivity patterns. Pediatrics, 105(6), E83. https://doi.org/10.1542/peds.105.6.e83
House, J. S., Lantz, P. M., & Herd, P. (2005). Continuity and change in the social stratification of aging and health over the life course: Evidence from a nationally representative longitudinal study from 1986 to 2001/2002 (Americans’ Changing Lives Study). Journals of Gerontology Series B-Psychological Sciences and Social Sciences, 60(Spec No 2), 15–26 . http://doi.org/60/suppl_Special_Issue_2/S15.
Huebner, D. M., & Davis, M. C. (2005). Gay and bisexual men who disclose their sexual orientations in the workplace have higher workday levels of salivary cortisol and negative affect. Annals of Behavioral Medicine, 30(3), 260–267. https://doi.org/10.1207/s15324796abm3003_10
Huynen, M. M., Martens, P., & Hilderink, H. B. (2005). The health impacts of globalisation: A conceptual framework. Globalization and Health, 1(1), 14. https://doi.org/10.1186/1744-8603-1-14
Juster, R. P., Hatzenbuehler, M. L., Mendrek, A., Pfaus, J. G., Smith, N. G., Johnson, P. J., et al. (2015). Sexual orientation modulates endocrine stress reactivity. Biological Psychiatry, 77(7), 668–676. https://doi.org/10.1016/j.biopsych.2014.08.013
Juster, R. P., Smith, N. G., Ouellet, E., Sindi, S., & Lupien, S. J. (2013). Sexual orientation and disclosure in relation to psychiatric symptoms, diurnal cortisol, and allostatic load. Psychosomatic Medicine, 75(2), 103–116. https://doi.org/10.1097/PSY.0b013e3182826881
Kaiser, J. (2011). Biomedical research funding. NIH uncovers racial disparity in grant awards. Science, 333(6045), 925–926. https://doi.org/10.1126/science.333.6045.925
Kauth, M. R., Shipherd, J. C., Lindsay, J., Blosnich, J. R., Brown, G. R., & Jones, K. T. (2014). Access to care for transgender veterans in the Veterans Health Administration: 2006–2013. American Journal of Public Health, 104(Suppl 4), S532–S534. https://doi.org/10.2105/AJPH.2014.302086
Kim, J., & Durden, E. (2007). Socioeconomic status and age trajectories of health. Social Science & Medicine, 65(12), 2489–2502. https://doi.org/10.1016/j.socscimed.2007.07.022
Kinnish, K. K., Strassberg, D. S., & Turner, C. W. (2005). Sex differences in the flexibility of sexual orientation: A multidimensional retrospective assessment. Archives of Sexual Behavior, 34(2), 173–183. https://doi.org/10.1007/s10508-005-1795-9
Kontos, E. Z., Emmons, K. M., Puleo, E., & Viswanath, K. (2011). Determinants and beliefs of health information mavens among a lower-socioeconomic position and minority population. Social Science & Medicine, 73(1), 22–32. https://doi.org/10.1016/j.socscimed.2011.04.024
Laćan, S. (2015). Concealing, revealing, and coming out: Lesbian visibility in Dalibor Matanić’s Fine Dead Girls and Dana Budisavljević’s Family Meals. Studies in European Cinema, 12(3), 229–245. https://doi.org/10.1080/17411548.2015.1094260
Lauderdale, D. S. (2001). Education and survival: Birth cohort, period, and age effects. Demography, 38(4), 551–561. https://doi.org/10.1353/dem.2001.0035
Lobato, M. I., Soll, B. M., Brandelli Costa, A., Saadeh, A., Gagliotti, D. A., Fresan, A., et al. (2019). Psychological distress among transgender people in Brazil: Frequency, intensity and social causation – An ICD-11 field study. Brazilian Journal of Psychiatry, 41(4), 310–315. https://doi.org/10.1590/1516-4446-2018-0052
Lopez, A. D., Mathers, C. D., Ezzati, M., Jamison, D. T., & Murray, C. J. (Eds.). (2006). Global burden of disease and risk factors. Oxford University Press and World Bank.
Mahdavi, P. (2019). The personal politics of private life in The United Arab Emirates (UAE): Sexualities, space, migration and identity politics in motion. Culture, Health & Sexuality, 21(12), 1–13. https://doi.org/10.1080/13691058.2018.1564938
Meier, S. C., & Labuski, C. M. (2013). The demographics of the transgender population. In A. K. Baumle (Ed.), International handbook on the demography of sexuality (pp. 289–327). Springer.
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. https://doi.org/10.1037/0033-2909.129.5.674
Morgan, E. M. (2013). Contemporary issues in sexual orientation and identity development in emerging adulthood. Emerging Adulthood, 1(1), 52–66. https://doi.org/10.1177/2167696812469187
Murray, C. J. (1994). Quantifying the burden of disease: The technical basis for disability-adjusted life years. Bulletin of the World Health Organization, 72(3), 429–445.
Murray, C. J., Vos, T., Lozano, R., Naghavi, M., Flaxman, A. D., Michaud, C., et al. (2012). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. The Lancet, 380(9859), 2197–2223. https://doi.org/10.1016/S0140-6736(12)61689-4
Muslim and gay: seeking identity coherence in New Zealand. (2016). Culture, Health & Sexuality, 18(3), 280–293. https://doi.org/10.1080/13691058.2015.1079927
Neher, R. A., Dyrdak, R., Druelle, V., Hodcroft, E. B., & Albert, J. (2020). Potential impact of seasonal forcing on a SARS-CoV-2 pandemic. Swiss Medical Weekly, 150(1112), w20224. https://doi.org/10.1101/2020.02.13.20022806
Omran, A. R. (2005). The epidemiologic transition: A theory of the epidemiology of population change. 1971. Milbank Quarterly, 83(4), 731–757. https://doi.org/10.1111/j.1468-0009.2005.00398.x
Pachankis, J. E., & Branstrom, R. (2019). How many sexual minorities are hidden? Projecting the size of the global closet with implications for policy and public health. PLoS One, 14(6), e0218084. https://doi.org/10.1371/journal.pone.0218084
Pang, T., & Guindon, G. E. (2004). Globalization and risks to health. EMBO Rep, 5 Spec No, S11–16. https://doi.org/10.1038/sj.embor.7400226
Patterson, J. G., Jabson, J. M., & Bowen, D. J. (2017). Measuring sexual and gender minority populations in health surveillance. LGBT Health, 4(2), 82–105. https://doi.org/10.1089/lgbt.2016.0026
Peitzmeier, S. M. (2013). Promoting cervical cancer screening among lesbians and bisexual women. Accessed 20 Nov 2022. www.fenwayhealth.org/cervicalcancerfocus
Provencher, D. M. (2016). Farid’s impossible “je”: Unequal access to flexible language in the queer Maghrebi French diaspora. Journal of Language and Sexuality, 5(1), 113–139. https://doi.org/10.1075/jls.5.1.05pro
Rahman, Q., Xu, Y., Lippa, R. A., & Vasey, P. L. (2020). Prevalence of sexual orientation across 28 nations and its association with gender equality, economic development, and individualism. Archives of Sexual Behavior, 49(2), 595–606. https://doi.org/10.1007/s10508-019-01590-0
Reisner, S. L., Gamarel, K. E., Dunham, E., Hopwood, R., & Hwahng, S. (2013). Female-to-male transmasculine adult health: A mixed-methods community-based needs assessment. Journal of the American Psychiatric Nurses Association, 19(5), 293–303. https://doi.org/10.1177/1078390313500693
Reisner, S. L., Poteat, T., Keatley, J., Cabral, M., Mothopeng, T., Dunham, E., et al. (2016). Global health burden and needs of transgender populations: A review. Lancet, 388(10042), 412–436. https://doi.org/10.1016/S0140-6736(16)00684-X
Reitsma, M. B., Fullman, N., Ng, M., Salama, J. S., Abajobir, A., Abate, K. H., et al. (2017). Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2013;2015: A systematic analysis from the Global Burden of Disease Study 2015. The Lancet, 389(10082), 1885–1906. https://doi.org/10.1016/S0140-6736(17)30819-X
Restar, A. J., Jin, H., Jarrett, B., Adamson, T., Baral, S. D., Howell, S., & Beckham, S. W. (2021). Characterizing the impact of COVID-19 environment on mental health, gender affirming services and socioeconomic loss in a global sample of transgender and non-binary people: A structural equation modelling. BMJ Global Health, 6(3), e004424. https://doi.org/10.1136/bmjgh-2020-004424
Rosario, M., Schrimshaw, E. W., Hunter, J., & Gwadz, M. (2002). Gay-related stress and emotional distress among gay, lesbian, and bisexual youths: A longitudinal examination. Journal of Consulting and Clinical Psychology, 70(4), 967–975. https://doi.org/10.1037//0022-006x.70.4.000
Schneiderman, N., Ironson, G., & Siegel, S. D. (2005). Stress and health: Psychological, behavioral, and biological determinants. Annual Review of Clinical Psychology, 1, 607–628. https://doi.org/10.1146/annurev.clinpsy.1.102803.144141
Schutte, S., Acevedo, P. N., & Flahault, A. (2018). Health systems around the world – A comparison of existing health system rankings. Journal of Global Health, 8(1), 010407. https://doi.org/10.7189/jogh.08.010407
Segerstrom, S. C., & Miller, G. E. (2004). Psychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychological Bulletin, 130(4), 601–630. https://doi.org/10.1037/0033-2909.130.4.601
Seidman, S. (2003). The social construction of sexuality. Norton.
Sexual Minority Assessment Research Team (SMART). (2009). Best practices for asking questions about sexual orientation on surveys (SMART). Accessed 20 Nov 2022. https://williamsinstitute.law.ucla.edu/publications/smart-so-survey/
Stambolis-Ruhstorfer, M. (2017). The importance of sexuality for research on ethnicity and nationalism. Studies in Ethnicity and Nationalism, 17(1), 44–56. https://doi.org/10.1111/sena.12224
Stokes, E., Zambrano, L., Anderson, K., Marder, E. P., Raz, K. M., Felix, S. E., et al. (2020). Coronavirus disease 2019 case surveillance — United States, January 22–May 30, 2020. MMWR Morbidity and Mortality Weekly Report, 69(24), 759–765. https://doi.org/10.15585/mmwr.mm6924e2
The World Bank Group. (2019). Life expectancy at birth, total (years) by country in 2017. Accessed 20 Nov 2022. https://data.worldbank.org/indicator/sp.dyn.le00.in.
United Nations Inter-agency Group for Child Mortality Estimation. (2018). Levels and trends in child mortality: Report 2018. Accessed 20 Nov 2022. https://www.unicef.org/publications/index_103264.html
World Health Organization. (2002). The World Health Report 2002: Reducing risks, promoting healthy life. Accessed 20 Nov 2022. https://apps.who.int/iris/bitstream/handle/10665/42510/WHR_2002.pdf.
World Health Organization. (2005). Preventing chronic diseases: A vital investment. WHO Global Report. Accessed 20 Nov 2022. https://www.who.int/chp/chronic_disease_report/en/
World Health Organization. (2018). Fact sheet: Noncommunicable diseases. Accessed 20 Nov 2022. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
Zavlin, D., Wassersug, R. J., Chegireddy, V., Schaff, J., & Papadopulos, N. A. (2019). Age-related differences for male-to-female transgender patients undergoing gender-affirming surgery. Sexual Medicine, 7(1), 86–93. https://doi.org/10.1016/j.esxm.2018.11.005
Zhou, P., Yang, X. L., Wang, X. G., Hu, B., Zhang, L., Zhang, W., et al. (2020). A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 579, 270–273. https://doi.org/10.2139/ssrn.3542586
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
McElroy, J.A., Gosiker, B.J. (2024). If You Don’t Ask, You Don’t Count: Elements to Consider in Understanding Global Sexual and Gender Minority Data on Noncommunicable Diseases. In: Hwahng, S.J., Kaufman, M.R. (eds) Global LGBTQ Health. Global LGBTQ Health. Springer, Cham. https://doi.org/10.1007/978-3-031-36204-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-031-36204-0_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-36203-3
Online ISBN: 978-3-031-36204-0
eBook Packages: MedicineMedicine (R0)