Abstract
Neuroendocrine tumours/neoplasms (NEN) are clinically challenging entities, often due to their late stage at initial diagnosis. Whilst surgery is the cornerstone of curative treatment, many patients are not eligible for a radical surgical approach, and instead other targeted or systemic treatments may be utilised. Neoadjuvant concepts such as downstaging borderline resectable tumours are more established in some adenocarcinomas than in neuroendocrine oncology, yet the diverse armamentarium for the latter offers promise for novel multimodal concepts that may offer prolonged disease control by complementarily targeting micro- and macro-neuroendocrine disease. One promising option, as yet only explored in small case series, is the combination of surgery and peptide receptor radionuclide therapy (PPRT). Here, the authors review the challenges posed by advanced NEN, review the fledgling evidence regarding the combination of PRRT and surgery, and present the case for a wider examination of embedding PRRT and surgery within a multimodal treatment strategy.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
3.1 Introduction
Neuroendocrine tumours (NET)—recently reclassified under the auspices of ‘neuroendocrine neoplasms’ (NEN)—arise from widely distributed neuroendocrine cells and share the capacity to secrete hormones and vasoactive peptides. They encompass distinct tumour entities with variable clinical behaviour, ranging from indolent to highly aggressive. Most commonly they are seen in the gastro-entero-pancreatic (GEP) [1] and bronchopulmonary tracts [2]. The analysis of large registries demonstrates that NET are steadily increasing in incidence and prevalence, with approximately three- to sevenfold increases in the former over the past three decades, and an estimated prevalence of 35/100,000. In the gastrointestinal tract, NEN are the second most common malignancy after colon cancer [3].
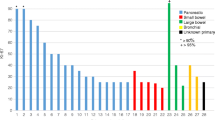
The central management issue of NEN is that at initial diagnosis, lymph node metastases and distant metastases are frequently seen. In a substantial number of patients with initially localised disease, metastases occur later during their clinical course. Depending upon the primary tumour site, 65–95% of NET present with liver metastases [4, 5]. The incidence of hepatic metastases is highest in patients with small bowel NEN (SBNEN) (67–91%) and pancreatic NEN (PanNEN) (28.3–77%) [6, 7], in contrast to patients with well-differentiated appendiceal NEN who display hepatic involvement in under 1% of cases [8] and patients with type I gastric NET or those with small, mainly incidentally discovered rectal NET. In historical series with a very limited spectrum of treatment options, 5-year survival was 13–54% for NEN patients with liver metastases compared with 75–99% for those without hepatic involvement. Experience in Centres of Excellence indicates a 5-year overall survival of 56–83% for metastatic intestinal NEN and 40–60% for pancreatic NEN [9]. In patients with SBNEN, lymph node metastases, in addition to liver metastases, present a therapeutic challenge since they frequently compromise major mesenteric vascularity and encase the mesenteric root, inducing abdominal angina and intestinal ischemia.
3.2 Molecular Imaging of Neuroendocrine Neoplasms
Molecular functional imaging has evolved into representing the cornerstone in diagnosis, staging, treatment selection, and follow-up of NEN. Scintigraphy with 111In-pentetreotide has almost universally been replaced by hybrid positron emission tomography (PET)/computed tomography (CT) with 68Ga-labeled somatostatin analogues (SSA) in the functional imaging of low-grade (G1) and intermediate-grade (G2) NEN [10,11,12,13,14]. Other PET agents utilised for diagnosis of neuroendocrine disease include 18F-FDG (for G2 and high-grade NEN), 18F-DOPA, 11C-5-HTP, GLP1, 64Cu-SSA and 68Ga-labeled somatostatin receptor antagonists [15]. Hybrid PET/magnetic resonance imaging (MRI) appears to be superior to PET/CT in the staging of liver metastases, utilises the same anatomic imaging modality used as the gold standard for diagnosis and follow-up of neuroendocrine liver metastases [16]. Dual imaging with 68Ga-DOTA and 18F-FDG PET/CT is suggested to be performed in tandem in patients with higher-grade NEN to better capture the known heterogeneity of neuroendocrine disease, or if a clinical course indicates sudden change towards more aggressive tumour behaviour.
Meticulous staging of NEN before planned surgery is critical for optimal patient selection and accurate surgical strategy (Fig. 3.1). 68Ga-DOTA-PET/CT has been shown to provide additional information and predicate change in initial surgical planning either in terms of change in surgical strategy or switch to non-surgical treatment in up to one-third of patients [17, 18] (Figs. 3.2 and 3.3).
Findings on 68Ga-DOTATATE PET/CT for a patient with a metastatic small intestinal neuroendocrine neoplasm. This patient underwent resection of the primary tumour (arrow, left image), followed by debulking of liver metastases and then peptide receptor radionuclide therapy. Images provided courtesy of Professor Richard P. Baum and Dr D. Kaemmerer
3.3 Surgical Treatment
Radical surgery with an aim to eliminate the primary tumour including loco-regional lymph node metastases and distant metastases (particularly those in the liver) accounts for the first-line treatment of grade 1 and grade 2 NEN where possible. Surgery may also be a valid option for loco-regionally limited grade 3 NEN, especially in tumours with a Ki67 of ≤55% [19]. Although no randomised controlled trials exist comparing surgical versus non-surgical treatment, there is a large body of evidence generated in retrospective series showing that surgery provides the best long-term outcomes [20,21,22]. The proclivity of NEN to metastasize challenges the surgical approach since surgery as an isolated measure is frequently insufficient. Moreover, it requires embedding within multimodal treatment concepts and the cognisance of the surgeon in dealing with metastasised disease.
All patients with localised SBNET should be considered for curative resection [23, 24]. As up to 50% of SBNET are multifocal and most of them already metastatic to loco-regional lymph nodes at the time of diagnosis, meticulous exploration of the mesentery and palpation of the entire small bowel from Treitz’s ligament to caecum is pivotal [25, 26]. A key issue in the resection of SBNEN is not necessarily the primary tumour per se, but the focus on preserving intestinal integrity whilst selectively resecting mesenteric lymph nodes. Extensive en bloc resections should be avoided as they may lead to short bowel syndrome. In case of multifocal focal tumour manifestation, multi-segmental resections might be required.
Patients with functioning PanNEN, irrespective of size, and those with primary tumours >2 cm are candidates for surgery encompassing typical resections including pancreaticoduodenectomy, distal pancreatectomy and total pancreatectomy, or atypical parenchyma-sparing resections [27]. Peripancreatic lymphadenectomy should be considered an integral part of a pancreatic resection with an exception of parenchyma-sparing procedures for benign insulinoma [28]. The indication for surgery and extent of surgery for multiple endocrine neoplasia (MEN)-1-associated PanNEN is a topic of controversial discussion, ranging from a rather conservative observational approach to extensive pancreatic resection [29, 30]. In general, non-functioning MEN-1-associated PanNEN smaller than 1 cm can be safely observed whilst tumours >2 cm should be resected. Indication for surgery is present in most of the patients with functioning MEN-1 PanNEN. Conflicting data exist also for small (≤2 cm) (nowadays frequently incidentally discovered) sporadic non-functioning PanNEN in asymptomatic patients. The threshold of ≤2 cm has been shown as a reliable selection criterion for surgical versus observational management in some series, whilst in others lymph node metastases and/or liver metastases were seen also in PanNEN less than 2 cm in size [31, 32]. Tumours causing ductal dilatation and G2/G3 PanNEN, even if below this threshold should be considered for resection [33]. In the future, biopsy-based genetic analysis of the primary tumour and novel preoperative risk scores may guide the decision to resect or to observe. Ki67 ≥3% and location of the tumour in the pancreatic head/uncinate process were shown to be associated with lymph node metastases in 21.4% of <2 cm in size PanNET, compared to 3.4% if Ki67 was <3% and the tumour located in the distal pancreas [34].
The role of resection of the primary tumour in presence of non-resectable LM in asymptomatic SBNEN or PanNEN patients is insufficiently defined. Randomised controlled trials comparing cohorts having primary tumour resection with those who were observed only and underwent surgery if symptoms occurred are lacking. Meta-analyses utilising data from retrospective series however indicate survival benefit for patients who had primary tumour resection in this setting [35]. Resecting an intestinal primary may avoid ileus, bowel obstruction, bleeding and desmoplastic reaction, and it may be associated with survival benefit [36]. For patients with asymptomatic PanNEN with non-resectable liver metastases, the recommendation for pancreatic resection is less convincing and burdened by selection bias. Surgery might be beneficial for younger patients free of comorbidities and tumour locations amenable to less extensive pancreatic resections [33].
The surgical treatment of neuroendocrine liver metastases (NE LM) involves resection with curative intention, cytoreductive surgery, or transplantation procedures [5, 37]. Patients with G1/G2 NEN with limited hepatic disease burden and highly selected patients with G3 tumours with Ki67 of ≤55% may be candidates for liver resection with curative intent. Only about 20% of all patients with NE LM are eligible for complete resection of liver deposits. Resection with curative intent is associated with the most favourable outcomes with a median 1-year, 3-year, 5-year, and 10-year overall survival (OS) rates of 94% (range 79–100%), 83% (range 63–100%), 70.5% (range 31–100%), and 42% (range 0–100%), respectively [38]. The wide range of reported overall survival reflects the importance of accurate patient selection. Whilst OS rates are overall favourable, early hepatic disease recurrence seen in approximately 80% of patients within the first three years following hepatectomy is a major clinical drawback [39]. This transforms liver resection with intended “curative” attempt to a de facto palliative treatment of NE LM, even if complete resection is achieved. Debulking surgery may be offered to patients with advanced G1/G2 NE LM unsuitable for radical hepatectomy, or to patients that are symptomatic either due to hepatic tumour bulk or hormone hypersecretion unresponsive to medical treatment [40]. Patients in whom at least 70% extirpation of tumour burden could be attained by parenchyma-sparing debulking procedures may benefit from surgery despite a rather short median liver progression-free survival of 11 months [41]. Liver transplantation is a generally accepted treatment option for highly selected patients with NE LM [42, 43]. Selection criteria for liver transplantation as defined by Mazzaferro et al. from Milan are: patients with low-grade NEN (with or without clinical symptoms), venous drainage of the primary tumour by the portal venous system, age ≤55 years, ≤50% liver involvement, complete resection of primary tumour and any extrahepatic disease prior to transplantation, and stable disease or disease response of at least 6 months before transplantation [44]. Under strict consideration of these selection criteria, 5-year and 10-year survival of 97.2% and 88.8%, respectively was reported [45]. Despite these impressive results and improvements of immunosuppressive protocols for patients transplanted for oncologic conditions, early disease recurrence remains a major clinical issue.
3.4 Surgery in Combination with Peptide Receptor Radionuclide Therapy
Peptide receptor radionuclide therapy (PRRT) with either 90Y-octreotide or 177Lu-DOTATATE or -DOTATOC was introduced into the treatment of metastasised NET in the early 1990s. Efficacy of PRRT in terms of favourable PFS and OS in NEN patients compared to historical controls has been shown in numerous phase I and II phase studies [46,47,48,49] and also prolonged PFS in the recent phase III NETTER-1 trial [50] (for more details please see contributions on peptide receptor radionuclide therapy in this Festschrift). The combination of surgical and medical-targeted therapeutic strategies within multimodal concepts offers an attractive possibility for long-term disease control by comprehensively eliminating macro- and microscopic neuroendocrine disease.
The combination of surgery and PRRT can be used in various clinical scenarios; (a) in neoadjuvant settings in patients with initially unresectable or borderline resectable NEN, (b) in adjuvant settings to minimise the risk of disease recurrence after radical surgery, (c) in palliative settings for treatment of remaining non-resectable disease after surgery, (d) as bridging prior to transplantation, or (e) as an upfront strategy to enhance the efficacy of PRRT by resecting the primary tumour. Such novel concepts have not yet been widely adopted and are mostly limited to single centres with interest and expertise in both advanced surgical procedures and theranostics.
In the first case reports, neoadjuvant Yttrium-90 (90Y) DOTA-PRRT was shown to effectively down-stage initially unresectable NEN including those originating from midgut [51], pancreas [52], rectum [53] and stomach [54]. The concept of staged surgery with neoadjuvant 90Y DOTA-PRRT has also been suggested for initially unresectable neuroendocrine liver metastases in case reports [55] and in small series [56]. In a Polish series of six patients with unresectable NEN, resection was achieved in two patients after tumour size reduction induced by PRRT [51]. In an Italian series comparing postoperative outcomes in patients with resectable/potentially resectable pancreatic NEN deemed at high risk of recurrence treated with or without neoadjuvant PRRT (n = 23 in each group), the incidence of nodal metastases was significantly lower in the PRRT group, and the PFS was significantly longer in the neoadjuvant group compared to the upfront surgery group [57]. Of interest, the risk of pancreatic fistula was lower in the neoadjuvant group compared to the group of patients who underwent upfront surgery. Most likely PRRT induces fibrosis which is known to reduce the risk of developing of pancreatic fistula [58]. A recent study comparing histopathological and immunophenotypic changes in pancreatic NEN after neoadjuvant PRRT revealed that neoadjuvant PRRT is associated with reduced tumour diameter, an increased percentage of stroma, preserved somatostatin receptor subtype 2A expression in most of the cases, and an increased CD163+ M2-polarised macrophage density [59]. Although the body of surgical data in NEN patients who underwent neoadjuvant PRRT is still scarce, postoperative complications do not occur more frequently than in not pre-treated patients. Peptide receptor radionuclide therapy has also a role as a bridging/downstaging procedure prior to liver or intestinal transplantation with an aim to stabilise macroscopical disease and target micrometastases [60]. To maximise the outcomes of neoadjuvant treatment for pancreatic neuroendocrine tumours, combined chemotherapy (Capecitabine/Temozolamide) and PRRT (chemo-PRRT) regimens have been brought into discussion [61].
Resection of the primary tumour in asymptomatic NET patients with unresectable distant metastases is a matter of ongoing debate [62,63,64]. In contrast, surgery for elimination of loco-regional and/or debulking of distant disease followed by PRRT for remaining non-resectable distant metastases appears as a generally accepted approach in patients symptomatic due to local tumour effect [65]. Particularly those with small bowel NEN who are at risk of developing intestinal obstruction, bleeding, and desmoplastic mesenteric and patients with large pancreatic NEN at risk for significant local stomach and superior mesenteric vein compression [66] may benefit from this approach.
Recently, upfront locoregional primary tumour resection has been proposed in patients considered for peptide receptor radionuclide therapy. In a study reported by Bertani et al., patients who underwent upfront surgery showed higher stabilisation or objective response after PRRT and better median PFS (70 vs. 30 months) and OS (112 vs. 65 months) compared to patients who underwent solely PRRT [67]. Similar experience was reported by Kaemmerer et al. who demonstrated prolonged OS in patients who had primary tumour resected prior to PRRT [68].
3.5 Conclusions
Although surgery offers the best chance of disease cure, given the clinical challenges presented by the oft metastatic stage of NEN at initial diagnosis, this cannot be realised for many patients. Therefore, embedding surgery within a multimodal treatment concept alongside PRRT and driven by theranostic principles represents a novel approach that targets macro- and micro-disease that may offer genuine advance in disease control. The combination of surgery and PRRT has only been reported in specialist centres with promising results from small series, but ideally a randomised controlled trial comparing neoadjuvant PRRT versus adjuvant PRRT versus PRRT alone is required to definitively assess this interesting therapeutic strategy. It is incumbent upon the NEN medical community to evaluate such novel treatment combinations to engender a divergence from a single modality focus that is often observed.
References
Clift AK, Kidd M, Bodei L, Toumpanakis C, Baum RP, Oberg K, et al. Neuroendocrine neoplasms of the small bowel and pancreas. Neuroendocrinology. 2019;110(6):444–76.
Fraenkel M, Faggiano A, Valk GD. Epidemiology of neuroendocrine tumors. Front Horm Res. 2015;44:1–23.
Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3(10):1335–42.
Riihimäki M, Hemminki A, Sundquist K, Sundquist J, Hemminki K. The epidemiology of metastases in neuroendocrine tumors. Int J Cancer. 2016;139(12):2679–86.
Frilling A, Modlin IM, Kidd M, Russell C, Breitenstein S, Salem R, et al. Recommendations for management of patients with neuroendocrine liver metastases. Lancet Oncol. 2014;15(1):e8–21.
Panzuto F, Boninsegna L, Fazio N, Campana D, Pia Brizzi M, Capurso G, et al. Metastatic and locally advanced pancreatic endocrine carcinomas: analysis of factors associated with disease progression. J Clin Oncol. 2011;29(17):2372–7.
Miller HC, Drymousis P, Flora R, Goldin R, Spalding D, Frilling A. Role of Ki-67 proliferation index in the assessment of patients with neuroendocrine neoplasias regarding the stage of disease. World J Surg. 2014;38(6):1353–61.
Pawa N, Clift AK, Osmani H, Drymousis P, Cichock A, Flora R, et al. Surgical management of patients with neuroendocrine neoplasms of the appendix: appendectomy or more? Neuroendocrinology. 2017;106(3):242–51.
Pavel M, Baudin E, Couvelard A, Krenning E, Öberg K, Steinmüller T, et al. ENETS consensus guidelines for the management of patients with liver and other distant metastases from neuroendocrine neoplasms of foregut, midgut, hindgut, and unknown primary. Neuroendocrinology. 2012;95(2):157–76.
Sundin A, Arnold R, Baudin E, Cwikla JB, Eriksson B, Fanti S, et al. ENETS consensus guidelines for the standards of care in neuroendocrine tumors: radiological, nuclear medicine and hybrid imaging. Neuroendocrinology. 2017;105(3):212–44.
Deppen SA, Blume J, Bobbey AJ, Shah C, Graham MM, Lee P, et al. 68Ga-DOTATATE compared with 111In-DTPA-octreotide and conventional imaging for pulmonary and gastroenteropancreatic neuroendocrine tumors: a systematic review and meta-analysis. J Nucl Med. 2016;57(6):872–8.
Sadowski SM, Neychev V, Millo C, Shih J, Nilubol N, Herscovitch P, et al. Prospective study of 68Ga-DOTATATE positron emission tomography/computed tomography for detecting gastro-entero-pancreatic neuroendocrine tumors and unknown primary sites. J Clin Oncol. 2016;34(6):588–97.
Hope TA, Bergsland EK, Bozkurt MF, Graham M, Heaney AP, Herrmann K, et al. Appropriate use criteria for somatostatin receptor PET imaging in neuroendocrine tumors. J Nucl Med. 2018;59(1):66–74.
Kulkarni HR, Baum RP. Theranostics with Ga-68 somatostatin receptor PET/CT: Monitoring response to peptide receptor radionuclide therapy. PET Clin. 2014;9(1):91–7.
Ito T, Jensen RT. Molecular imaging in neuroendocrine tumors: recent advances, controversies, unresolved issues, and roles in management. Curr Opin Endocrinol Diabetes Obes. 2017;24(1):15–24.
Hope TA, Pampaloni MH, Nakakura E, VanBrocklin H, Slater J, Jivan S, et al. Simultaneous (68)Ga-DOTA-TOC PET/MRI with gadoxetate disodium in patients with neuroendocrine tumor. Abdom Imaging. 2015;40(6):1432–40.
Ilhan H, Fendler WP, Cyran CC, Spitzweg C, Auernhammer CJ, Gildehaus FJ, et al. Impact of 68Ga-DOTATATE PET/CT on the surgical management of primary neuroendocrine tumors of the pancreas or ileum. Ann Surg Oncol. 2015;22(1):164–71.
Frilling A, Sotiropoulos GC, Radtke A, Malago M, Bockisch A, Kuehl H, et al. The impact of 68Ga-DOTATOC positron emission tomography/computed tomography on the multimodal management of patients with neuroendocrine tumors. Ann Surg. 2010;252(5):850–6.
Merola E, Rinke A, Partelli S, Gress TM, Andreasi V, Kollár A, et al. Surgery with radical intent: is there an indication for G3 neuroendocrine neoplasms? Ann Surg Oncol. 2020;27(5):1348–55.
Falconi M, Eriksson B, Kaltsas G, Bartsch DK, Capdevila J, Caplin M, et al. ENETS consensus guidelines update for the management of patients with functional pancreatic neuroendocrine tumors and non-functional pancreatic neuroendocrine tumors. Neuroendocrinology. 2016;103(2):153–71.
Niederle B, Pape UF, Costa F, Gross D, Kelestimur F, Knigge U, et al. ENETS consensus guidelines update for neuroendocrine neoplasms of the jejunum and ileum. Neuroendocrinology. 2016;103(2):125–38.
Fairweather M, Swanson R, Wang J, Brais LK, Dutton T, Kulke MH, et al. Management of neuroendocrine tumor liver metastases: long-term outcomes and prognostic factors from a large prospective database. Ann Surg Oncol. 2017;24(8):2319–25.
Larouche V, Akirov A, Alshehri S, Ezzat S. Management of small bowel neuroendocrine tumors. Cancer. 2019;11(9):1395.
Pasquer A, Walter T, Hervieu V, Forestier J, Scoazec J-Y, Lombard-Bohas C, et al. Surgical management of small bowel neuroendocrine tumors: specific requirements and their impact on staging and prognosis. Ann Surg Oncol. 2015;22(3):742–9.
Gangi A, Siegel E, Barmparas G, Lo S, Jamil LH, Hendifar A, et al. Multifocality in small bowel neuroendocrine tumors. J Gastrointest Surg. 2018;22(2):303–9.
Lardière-Deguelte S, de Mestier L, Appéré F, Vullierme M-P, Zappa M, Hoeffel C, et al. Toward a preoperative classification of lymph node metastases in patients with small intestinal neuroendocrine tumors in the era of intestinal-sparing surgery. Neuroendocrinology. 2016;103(5):552–9.
Maurizi A, Partelli S, Falconi M. Pancreatic surgery. Front Horm Res. 2015;44:139–48.
Lopez-Aguiar AG, Zaidi MY, Beal EW, Dillhoff M, Cannon JGD, Poultsides GA, et al. Defining the role of lymphadenectomy for pancreatic neuroendocrine tumors: an eight-institution study of 695 patients from the US Neuroendocrine Tumor Study Group. Ann Surg Oncol. 2019;26(8):2517–24.
Norton JA, Jensen RT. Resolved and unresolved controversies in the surgical management of patients with Zollinger-Ellison syndrome. Ann Surg. 2004;240(5):757–73.
Triponez F, Sadowski SM, Pattou F, Cardot-Bauters C, Mirallié E, Le Bras M, et al. Long-term follow-up of MEN1 patients who do not have initial surgery for small ≤2 cm nonfunctioning pancreatic neuroendocrine tumors, an AFCE and GTE study: Association Francophone de Chirurgie Endocrinienne & Groupe d’Etude des Tumeurs Endocrines. Ann Surg. 2018;268(1):158–64.
Chivukula SV, Tierney JF, Hertl M, Poirier J, Keutgen XM. Operative resection in early stage pancreatic neuroendocrine tumors in the United States: are we over- or undertreating patients? Surgery. 2020;167(1):180–6.
Finkelstein P, Sharma R, Picado O, Gadde R, Stuart H, Ripat C, et al. Pancreatic neuroendocrine tumors (panNETs): analysis of overall survival of nonsurgical management versus surgical resection. J Gastrointest Surg. 2017;21(5):855–66.
Sallinen VJ, Le Large TTY, Tieftrunk E, Galeev S, Kovalenko Z, Haugvik SP, et al. Prognosis of sporadic resected small (≤2 cm) nonfunctional pancreatic neuroendocrine tumors – a multi-institutional study. HPB. 2018;20(3):251–9.
Lopez-Aguiar AG, Ethun CG, Zaidi MY, Rocha FG, Poultsides GA, Dillhoff M, et al. The conundrum of < 2-cm pancreatic neuroendocrine tumors: a preoperative risk score to predict lymph node metastases and guide surgical management. Surgery. 2019;166(1):15–21.
Almond LM, Hodson J, Ford SJ, Gourevitch D, Roberts KJ, Shah T, et al. Role of palliative resection of the primary tumour in advanced pancreatic and small intestinal neuroendocrine tumours: a systematic review and meta-analysis. Eur J Surg Oncol. 2017;43(10):1808–15.
Capurso G, Rinzivillo M, Bettini R, Boninsegna L, Fave GD, Falconi M. Systematic review of resection of primary midgut carcinoid tumour in patients with unresectable liver metastases. Br J Surg. 2012;99(11):1480–6.
Frilling A, Clift AK. Surgical approaches to the management of neuroendocrine liver metastases. Endocr Metab Clin N Am. 2018;47(3):627–43.
Saxena A, Chua TC, Perera M, Chu F, Morris DL. Surgical resection of hepatic metastases from neuroendocrine neoplasms: a systematic review. Surg Oncol. 2012;21(3):e131–41.
Mayo SC, de Jong MC, Pulitano C, Clary BM, Reddy SK, Gamblin TC, et al. Surgical management of hepatic neuroendocrine tumor metastasis: results from an international multi-institutional analysis. Ann Surg Oncol. 2010;17(12):3129–36.
Osborne DA, Zervos EE, Strosberg J, Strosberg J, Boe BA, Malafa M, et al. Improved outcome with cytoreduction versus embolization for symptomatic hepatic metastases of carcinoid and neuroendocrine tumors. Ann Surg Oncol. 2006;13(4):572–81.
Morgan RE, Pommier SJ, Pommier RF. Expanded criteria for debulking of liver metastasis also apply to pancreatic neuroendocrine tumors. Surgery. 2018;163(1):218–25.
Fan ST, Le Treut YP, Mazzaferro V, Burroughs AK, Olausson M, Breitenstein S, et al. Liver transplantation for neuroendocrine tumour liver metastases. HPB. 2015;17(1):23–8.
Moris D, Tsilimigras DI, Ntanasis-Stathopoulos I, Beal EW, Felekouras E, Vernadakis S, et al. Liver transplantation in patients with liver metastases from neuroendocrine tumors: a systematic review. Surgery. 2017;162(3):525–36.
Mazzaferro V, Pulvirenti A, Coppa J. Neuroendocrine tumors metastatic to the liver: how to select patients for liver transplantation? J Hepatol. 2007;47(4):460–6.
Mazzaferro V, Sposito C, Coppa J, Miceli R, Bhoori S, Bongini M, et al. The long-term benefit of liver transplantation for hepatic metastases from neuroendocrine tumors. Am J Transplant. 2016;16(10):2892–902.
Bodei L, Kwekkeboom DJ, Kidd M, Modlin IM, Krenning EP. Radiolabeled somatostatin analogue therapy of gastroenteropancreatic cancer. Semin Nucl Med. 2016;46(3):225–38.
Brabander T, van der Zwan WA, Teunissen JJM, Kam BLR, Feelders RA, de Herder WW, et al. Long-term efficacy, survival, and safety of [177Lu-DOTA0,Tyr3]octreotate in patients with gastroenteropancreatic and bronchial neuroendocrine tumors. Clin Cancer Res. 2017;23(16):4617–24.
Baum RP, Kulkarni HR, Singh A, Kaemmerer D, Mueller D, Prasad V, et al. Results and adverse events of personalized peptide receptor radionuclide therapy with 90-Yttrium and 177-Lutetium in 1048 patients with neuroendocrine neoplasms. Oncotarget. 2018;9(24):16932–50.
Sabet A, Dautzenberg K, Haslerud T, Aouf A, Sabet A, Simon B, et al. Specific efficacy of peptide receptor radionuclide therapy with (177)Lu-octreotate in advanced neuroendocrine tumours of the small intestine. Eur J Nucl Med Mol Imaging. 2015;42(8):1238–46.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 trial of177Lu-dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125–35.
Sowa-Staszczak A, Pach D, Chrzan R, Trofimiuk M, Stefańska A, Tomaszuk M, et al. Peptide receptor radionuclide therapy as a potential tool for neoadjuvant therapy in patients with inoperable neuroendocrine tumours (NETs). Eur J Nucl Med Mol Imaging. 2011;38(9):1669–74.
Kaemmerer D, Prasad V, Daffner W, Hörsch D, Klöppel G, Hommann M, et al. Neoadjuvant peptide receptor radionuclide therapy for an inoperable neuroendocrine pancreatic tumor. World J Gastroenterol. 2009;15(46):5867–70.
Ryan J, Akhurst T, Lynch AC, Michael M, Heriot AG. Neoadjuvant 90Yttrium peptide receptor radionuclide therapy for advanced rectal neuroendocrine tumour: a case report. ANZ J Surg. 2017;87(1–2):92–3.
Schmidt MC, Uhrhan K, Fischer T, Schmitz S, Markiefka B, Drzezga A, et al. Complete remission of metastatic neuroendocrine paragastric carcinoma after “neoadjuvant” peptide receptor radionuclide therapy and surgery. Clin Nucl Med. 2015;40(8):667–9.
Stoeltzing O, Loss M, Huber E, Gross V, Eilles C, Mueller-Brand J, et al. Staged surgery with neoadjuvant 90Y-DOTATOC therapy for down-sizing synchronous bilobular hepatic metastases from a neuroendocrine pancreatic tumor. Langenbeck's Arch Surg. 2010;395(2):185–92.
Chiapponi C, Lürssen N, Cremer B, Wahba R, Drebber U, Faust M, et al. Peptide receptor radionuclide therapy as a two-step strategy for initially unresectable liver disease from neuroendocrine tumors: a single-center experience. Endocrine. 2020;70(1):187–93. https://doi.org/10.1007/s12020-020-02341-1.
Partelli S, Bertani E, Bartolomei M, Perali C, Muffatti F, Grana CM, et al. Peptide receptor radionuclide therapy as neoadjuvant therapy for resectable or potentially resectable pancreatic neuroendocrine neoplasms. Surgery. 2017;163(4):761–7.
van Vliet EI, van Eijck CH, de Krijger RR, Nieveen van Dijkum EJ, Teunissen JJ, Kam BL, et al. Neoadjuvant treatment of nonfunctioning pancreatic neuroendocrine tumors with [177Lu-DOTA0,Tyr3]octreotate. J Nucl Med. 2015;56(11):1647–53.
Schiavo Lena M, Partelli S, Castelli P, Andreasi V, Smart CE, Pisa E, et al. Histopathological and immunophenotypic changes of pancreatic neuroendocrine tumors after neoadjuvant peptide receptor radionuclide therapy (PRRT). Endocr Pathol. 2020;31(2):119–31.
Frilling A, Giele H, Vrakas G, Reddy S, Macedo R, Al-Nahhas A, et al. Modified liver-free multivisceral transplantation for a metastatic small bowel neuroendocrine tumor: a case report. Transplant Proc. 2015;47(3):858–62.
Basu S, Parghane RV, Ostwal V, Shrikhande SV. Neoadjuvant strategies for advanced pancreatic neuroendocrine tumors: should combined chemotherapy and peptide receptor radionuclide therapy be the preferred regimen for maximizing outcome? Nucl Med Commun. 2018;39(1):94–5.
Lewis A, Raoof M, Ituarte PHG, Williams J, Melstrom L, Li D, et al. Resection of the primary gastrointestinal neuroendocrine tumor improves survival with or without liver treatment. Ann Surg. 2018;270(6):1131–7.
Citterio D, Pusceddu S, Facciorusso A, Coppa J, Milione M, Buzzoni R, et al. Primary tumour resection may improve survival in functional well-differentiated neuroendocrine tumours metastatic to the liver. Eur J Surg Oncol. 2017;43(2):380–7.
Daskalakis K, Karakatsanis A, Hessman O, Stuart HC, Welin S, Tiensuu Janson E, et al. Association of a prophylactic surgical approach to stage IV small intestinal neuroendocrine tumors with survival. JAMA Oncol. 2018;4(2):183–9.
Frilling A, Weber F, Saner F, Bockisch A, Hofmann M, Mueller-Brand J, et al. Treatment with (90)Y- and (177)Lu-DOTATOC in patients with metastatic neuroendocrine tumors. Surgery. 2006;140(6):968–76; discussion 976-7.
da Silva TN, van Velthuysen MLF, van Eijck CHJ, Teunissen JJ, Hofland J, de Herder WW. Successful neoadjuvant peptide receptor radionuclide therapy for an inoperable pancreatic neuroendocrine tumour. Endocrinol Diabetes Metab Case Rep. 2018;2018:18.
Bertani E, Fazio N, Radice D, Zardini C, Grana C, Bodei L, et al. Resection of the primary tumor followed by peptide receptor radionuclide therapy as upfront strategy for the treatment of G1–G2 pancreatic neuroendocrine tumors with unresectable liver metastases. Ann Surg Oncol. 2016;23:981–9.
Kaemmerer D, Twrznik M, Kulkarni HR, Hörsch D, Sehner S, Baum RP, et al. Prior resection of the primary tumor prolongs survival after peptide receptor radionuclide therapy of advanced neuroendocrine neoplasms. Ann Surg. 2019;274(1):e45–53. https://doi.org/10.1097/SLA.0000000000003237.
Conflict of Interest
Both authors report that they have no conflicts to declare.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Frilling, A., Clift, A.K. (2024). Surgery in Combination with Peptide Receptor Radionuclide Therapy: A Novel Approach for the Treatment of Advanced Neuroendocrine Tumours. In: Prasad, V. (eds) Beyond Becquerel and Biology to Precision Radiomolecular Oncology: Festschrift in Honor of Richard P. Baum. Springer, Cham. https://doi.org/10.1007/978-3-031-33533-4_3
Download citation
DOI: https://doi.org/10.1007/978-3-031-33533-4_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-33532-7
Online ISBN: 978-3-031-33533-4
eBook Packages: MedicineMedicine (R0)