Abstract
Lateral pelvic lymph node dissection (LPND) represents a treatment option for patients with locally advanced low rectal cancer and suspected lateral pelvic nodes. Many of these patients could develop locoregional recurrence when treated with total mesorectal excision alone. However, LPND is a technically demanding procedure burdened by a non-negligible risk of intraoperative bleeding and postoperative genitourinary dysfunction. The robotic platform may represent the best option for minimally invasive LPND, providing fine movements, good traction, and stable camera. Indeed, robotic LPND is associated with decreased intraoperative blood loss and lower rates of urinary retention compared to the laparoscopic approach. We present here our standardized technique based on the dissection of three potential fascial planes within the lateral pelvic sidewall: plane A, the innermost, containing the ureter and the hypogastric and pelvic nerves; plane B, the outmost, defined by the external iliac vessels and psoas and obturator internus muscle; plane C, lateral to the internal iliac vessels and their branches. Standard LPND includes the obturator and internal iliac node group.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Rectal cancer
- Locally advanced rectal cancer
- Low rectal cancer
- Robotic surgery
- Minimally invasive surgery
- Lateral pelvic node dissection
- Lymphadenectomy
1 Introduction
The Western and Eastern classification of nodal metastases differ regarding the definition of regional lymph nodes. Historically, lateral pelvic nodes (LPN) in the obturator area were regarded as distant metastases according to the American Joint Committee on Cancer (AJCC) staging system, while the current edition of the AJCC staging manual defines internal iliac nodes as regional lymph nodes [1]. Conversely, the ninth edition of the Japanese guidelines considers all LPN as regional [2]. Interestingly, a study on 3487 Japanese patients with locally advanced low rectal cancer (LARC) who received LPN dissection (LPND) showed that overall and recurrence-free survival was slightly, but not significantly, worse in patients with obturator LPN metastases compared with those with internal iliac LPN metastases. Therefore, the authors proposed obturator LPN metastases as local disease [3]. Standard LPND for LARC includes the removal of the lymphoareolar tissue from both the obturator and internal iliac areas, given that they are the most common sites of LPN metastases [4].
Also, treatment of LARC differs between the East and the West. While Western countries contemplate neoadjuvant chemoradiotherapy (CRT) followed by total mesorectal excision (TME) [5], the Japanese routinely perform prophylactic or therapeutic LPND [2]. These practices are based on the results of large randomized controlled trials, which showed lower locoregional recurrence rates with preoperative radiotherapy (5%) [6, 7] or prophylactic bilateral LPND (7.7%) [8, 9] compared to TME alone (11–13%). Nonetheless, there is evidence that CRT and TME may not be sufficient in the case of suspicious LPN, as the vast majority of locoregional recurrences (54–83%) in these patients is found in the lateral pelvic sidewall [10, 11]. Moreover, LPN metastases are a strong predictor of survival and local recurrence [12]. Since the rate of metastatic LPN in prophylactic LPND is lower than 10% [9], some authors have suggested selective LPND after preoperative CRT for patients with suspicious LPN [11]. Debate still exists on the optimal criteria for the definition of suspicious LPN, but most authors consider the short or long axis of the largest LPN on pre- [11, 13,14,15,16] or post-treatment imaging [13, 17]. An international multicenter study by the Lateral Node Study Consortium re-evaluated the pretreatment MRI of 1216 patients with LARC. They identified a significantly higher risk of local recurrence (19.5%) and lateral local recurrence (15%) at 5 years in patients with LPN equal to or greater than 7 mm in short axis on pretreatment MRI [11]. The indication for LPND at the Colorectal Cancer Center at Kyungpook National University Hospital is an enlarged suspicious lymph node in the pelvic sidewall on pretreatment MRI with a short axis greater than 5 mm, regardless of response to preoperative treatment [18, 19].
LPND is considered by most surgeons a technically demanding procedure. The risk of intraoperative bleeding and postoperative genitourinary dysfunction limited its diffusion in the West [20]. Nonetheless, data from specialized Eastern centers demonstrated that the slight increase in short-term complications and functional morbidity is offset by improved long-term oncological outcomes. Data from the JCOG0212 trial comparing 351 patients receiving open TME plus prophylactic bilateral LPND, with 350 undergoing TME alone, reported increased intraoperative blood loss (576 mL vs. 337 mL, p < 0.001) in the LPND group, but no differences in terms of severe complications and anastomotic leak [21]. Moreover, laparoscopic LPND compared to the open approach showed reduced blood loss, shorter hospital stay, and a higher number of retrieved lymph nodes [22, 23]. The robotic platform represents an optimal option for LPND, providing good traction and counter-traction, high-quality images and stable camera, as well as articulating and precise instruments for fine dissection. In fact, robotic LPND is associated with decreased intraoperative blood loss and lower rate of urinary retention compared to the laparoscopic approach [18]. Moreover, initial evaluation of long-term outcomes showed comparable local recurrence rates and disease-free survival of robotic and laparoscopic LPND [19]. Despite the advantages of the robotic platform, LPND remains technically demanding. Analysis of 100 patients undergoing robotic TME plus LPND showed a learning phase of about 50 cases. Even in the competence phase, urinary dysfunction represented the most frequent complication, although the incidence decreased from the learning to the competence phase (39.4% vs. 16.7%) [24].
Herein we report the details of our technique of LPND using a fourth-generation, four-arm surgical robot (da Vinci Xi, Intuitive Surgical, Sunnyvale, CA).
2 Equipment, Patient Positioning and Operating Room Setup
Recommended equipment:
-
30° down endoscope
-
fenestrated bipolar forceps
-
monopolar curved scissors
-
tip-up grasper.
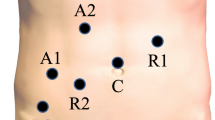
LPND is carried out after completion of rectal dissection and rectal transection and before creation of the anastomosis. Therefore, the patient is in the supine position, with a 15–20° Trendelenburg position and a left lateral tilt (10–15°). The bedside surgeon is on the right of the patient. Two different port setups are possible, depending on the availability of a Uni-Port (Dalim Medical, Korea) or similar single-port devices. Uni-Port is placed in the right-lower quadrant in the future ileostomy site and will accommodate one robotic 8-mm port as well as assistant trocars. As illustrated in Fig. 12.1a, one additional 5-mm assistant port, and four robotic 8-mm ports are placed. Figure 12.1b illustrates trocar setting in the absence of the Uni-Port (four robotic 8-mm ports and two 5-mm assistant ports). Robotic accesses are generally placed along an oblique line. After completion of rectal dissection, left LPND is generally performed first, maintaining the same trocar and instrument setup as for rectal resection. Typically, R1 is used for the tip-up grasper, which we favor for major tractions. The bipolar fenestrated forceps and the monopolar curved scissors are mounted on R2 and R4, respectively, for finer traction and dissection. Bipolar fenestrated forceps can also be used as an energy device to control minor bleeds. R3 holds the 30° endoscope. The bedside surgeon utilizes the laparoscopic accesses to assist with the counter-traction, deliver irrigation and suction, and apply energy devices as needed. For right LPND, the bipolar fenestrated forceps, endoscope, monopolar curved scissors, and tip-up grasper are repositioned in robotic trocars R1 to R4, respectively. For female patients, a 2-0 Prolene suture with straight needle is usually recommended to suspend the uterus anteriorly and the Fallopian tube-ovary complex to the lateral abdominal wall to allow better exposure.
3 Technique/Procedure
3.1 Surgical Anatomy and Dissection
We standardized the surgical steps based on anatomical landmarks of the lateral pelvic sidewall, as previously reported [25]. The lateral pelvic sidewall is defined with three potential fascial planes, as illustrated in Fig. 12.2. The planes are developed in the order of A, B, and C, and they represent the boundaries of standard LPND. Dissection commences at plane A, which is the innermost layer containing the ureter, hypogastric nerve, pelvic splanchnic nerves, and pelvic plexus. Plane B is the outmost layer, defined by the medial aspect of the external iliac vessels and psoas and the obturator internus muscle. Plane C is a potential fascial plane just lateral to the internal iliac vessels and their branches, continuing to the dorsolateral wall of the urinary bladder. The floor is defined by the lumbosacral nerve trunk and a part of the pelvic bone and muscles. All vascular structures are preserved whenever possible, unless encapsulated by metastatic lymph nodes. In that case, en-bloc resection is performed, and vessel division is carried out with LigaSure delivered through the assistant port. Standard LPND usually involves dissection of the obturator and internal iliac nodes. External iliac and common iliac node dissection is performed only in selected cases with highly suspicious metastatic nodes in these areas.
Dissection starts along plane A, which separates the medial side of the internal iliac node group (see Video 12.1 for the detailed procedure). This plane is developed through the avascular space between the ureter and common iliac vessels, and then continued between the internal iliac vessels and the hypogastric nerve, and between the pelvic plexus, pelvic splanchnic nerves, and terminal branches of the internal iliac vessels on the bottom. The ureter near the common iliac artery is gently grasped with the bipolar grasper, retracted medially, and blunt or sharp dissection with the monopolar curved scissors is carried out to separate it within a fascia from the pelvic sidewall. Dissection is then continued caudally and dorsally to separate the thin medial layer containing the hypogastric nerve, the pelvic plexus, and the pelvic splanchnic nerves from the pelvic sidewall. Dissection is carried on until branches of the internal iliac vein are identified on the lateral side, and fibers of the pelvic autonomic nerves on the medial side. Subsequently, plane B is developed. An incision is made along the medial aspect of the external iliac artery to divide lymphoareolar tissue of the obturator node group. The tip-up grasper is used for lateral retraction of the external iliac vessels while dissection is continued downward over the surface of the external iliac vein, psoas muscle, and obturator internus muscle. Occasionally, an obturator accessory vein branches off from the external iliac vein, representing the distal landmark of dissection along this plane. Finally, we make plane C, which is medially bounded by the terminal branches of the anterior division of the internal iliac vessels, dividing the medial aspect of the obturator node group. The branches encountered in a cranial-to-caudal order include the umbilical artery, superior vesical artery, obturator artery, inferior vesical artery, and the internal pudendal artery at its entrance in the Alcock’s canal as the most distal landmark of dissection.
The branches of the internal iliac artery can be grouped based on their direction.
-
Posterior division: iliolumbar, lateral sacral, superior gluteal.
-
Anterior division: obturator, umbilical and primary branch superior vesical, uterine (± vaginal), inferior vesical, middle rectal, inferior gluteal, internal pudendal.
Variations in the anatomy of the branches of the internal iliac artery are common, with the superior vesical artery that may arise directly from the internal iliac artery just distally to the umbilical artery. Caution should be used for dissection of the superior gluteal artery because it runs very close to the sciatic nerve.
3.2 Lymphadenectomy
After all three planes are securely developed, actual lymph node dissection is carried out. First, obturator node dissection starts from the bifurcation of the common iliac vessels to remove all lymphoareolar tissue between planes B and C. Special attention should be directed toward identification and preservation of the obturator nerve and the lumbosacral trunk at the bottom. The tip-up grasper in the third robotic arm is used for distal counter-traction in the bladder area, while the assistant aids with retraction of the external iliac vessels when needed. Bipolar fenestrated forceps with the open jaws technique can help to effectively expose the surgical field and conduct fine dissection. Again, obturator node dissection starts at the bifurcation of the common iliac vessels, where the nodes are separated from the obturator nerve, and continues caudally toward the obturator foramen. Distally, the surface of the bladder is exposed. The distal side of the obturator nerve and artery is exposed, and the lymph nodes are dissected from these structures. The dorsal boundary of dissection is the lumbosacral trunk, which should be carefully dissected without injury. Lymph nodes are also dissected from the lateral aspect of the umbilical artery and internal pudendal vessels and nerve. Dissection of the obturator nodes is completed by removing all lymphoareolar tissue between planes B and C. A suspicious index lymph node can be marked by applying a hem-o-lok.
Then, the internal iliac nodes are dissected between planes A and C and through the distal branches of the internal iliac artery. The assistant grasps the ureter and retracts it medially, while the tip-up grasper pushes the parietal peritoneum upwards and laterally. The most critical area is dissection of the distal internal iliac node group which is an entry of lateral lymphatic flow from the rectum. Complete dissection should be performed along the terminal branches of the internal iliac vessels until identification of the internal pudendal artery, because it is the site most commonly containing metastatic lymph nodes. Dissection starts on the medial side of the internal iliac artery and continues along the medial side of the umbilical artery. The superior vesical artery is then identified and preserved, and dissection is carried on along the terminal branches of the internal iliac vessels until identification of the internal pudendal artery. We then remove remaining lymphoareolar tissue around the inferior vesical artery and the deepest area of the pelvic sidewall. The final appearance of the dissected lateral pelvic sidewall is shown in Fig. 12.3.
The specimens are collected in a plastic bag and extracted through the Uni-Port, if present, or through a periumbilical minilaparotomy on the midline using a plastic wound retractor. Finally, the abdominal cavity is checked for adequate hemostasis and generously irrigated with saline. We routinely use one drain in the pelvis to prevent postoperative lymph collections. The abdomen is carefully desufflated and the port accesses and extraction site are closed. Loop ileostomy is created when deemed necessary.
References
Amin M, Edge SB, Greene F. AJCC cancer staging manual. 8th ed. Springer; 2018.
Hashiguchi Y, Muro K, Saito Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25(1):1–42.
Chen Z, Sasaki K, Murono K, et al. Oncologic status of obturator lymph node metastases in locally advanced low rectal cancer: a Japanese multi-institutional study of 3487 patients. Ann Surg Oncol. 2022;29(7):4210–9.
Kobayashi H, Mochizuki H, Kato T, et al. Outcomes of surgery alone for lower rectal cancer with and without pelvic sidewall dissection. Dis Colon Rectum. 2009;52(4):567–76.
National Comprehensive Cancer Network. NCCN Guidelines – Rectal Cancer (version 3.2022). https://www.nccn.org/professionals/physician_gls/pdf/rectal.pdf.
Kapiteijn E, Marijnen CAM, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001;345(9):638–46.
Van Gijn W, Marijnen CAM, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol. 2011;12(6):575–82.
Tsukamoto S, Fujita S, Ota M, et al. Long-term follow-up of the randomized trial of mesorectal excision with or without lateral lymph node dissection in rectal cancer (JCOG0212). Br J Surg. 2020;107(5):586–94.
Fujita S, Mizusawa J, Kanemitsu Y, et al. Mesorectal excision with or without lateral lymph node dissection for clinical stage II/III lower rectal cancer (JCOG0212). Ann Surg. 2017;266(2):201–7.
Kim TH, Jeong SY, Choi DH, et al. Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol. 2008;15(3):729–37.
Ogura A, Konishi T, Cunningham C, et al. Neoadjuvant (chemo)radiotherapy with total mesorectal excision only is not sufficient to prevent lateral local recurrence in enlarged nodes: Results of the multicenter lateral node study of patients with low ct3/4 rectal cancer. J Clin Oncol. 2019;37(1):33–43.
Sugihara K, Kobayashi H, Kato T, et al. Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum. 2006;49(11):1663–72.
Kawai K, Shiratori H, Hata K, et al. Optimal size criteria for lateral lymph node dissection after neoadjuvant chemoradiotherapy for rectal cancer. Dis Colon Rectum. 2021;64(3):274–83.
Hida K, Nishizaki D, Sumii A, et al. Prognostic impact of lateral pelvic node dissection on the survival of patients in low rectal cancer subgroups based on lymph node size. Ann Surg Oncol. 2021;28(11):6179–88.
Akiyoshi T, Ueno M, Matsueda K, et al. Selective lateral pelvic lymph node dissection in patients with advanced low rectal cancer treated with preoperative chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol. 2014;21(1):189–96.
Kim HJ, Choi GS, Park JS, et al. Optimal treatment strategies for clinically suspicious lateral pelvic lymph node metastasis in rectal cancer. Oncotarget. 2017;8(59):100724–33.
Ogura A, Konishi T, Beets GL, et al. Lateral nodal features on restaging magnetic resonance imaging associated with lateral local recurrence in low rectal cancer after neoadjuvant chemoradiotherapy or radiotherapy. JAMA Surg. 2019;154(9):e192172.
Kim HJ, Choi GS, Park JS, et al. Selective lateral pelvic lymph node dissection: a comparative study of the robotic versus laparoscopic approach. Surg Endosc. 2018;32(5):2466–73.
Song SH, Choi GS, Kim HJ, et al. Long-term clinical outcomes of total mesorectal excision and selective lateral pelvic lymph node dissection for advanced low rectal cancer: a comparative study of a robotic versus laparoscopic approach. Tech Coloproctol. 2021;25(4):413–23.
Georgiou P, Tan E, Gouvas N, et al. Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Lancet Oncol. 2009;10(11):1053–62.
Fujita S, Akasu T, Mizusawa J, et al. Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): Results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol. 2012;13(6):616–21.
Nagayoshi K, Ueki T, Manabe T, et al. Laparoscopic lateral pelvic lymph node dissection is achievable and offers advantages as a minimally invasive surgery over the open approach. Surg Endosc. 2016;30(5):1938–47.
Park JS, Choi GS, Lim KH, et al. Laparoscopic extended lateral pelvic node dissection following total mesorectal excision for advanced rectal cancer: Initial clinical experience. Surg Endosc. 2011;25(10):3322–9.
Kim HJ, Choi GS, Park JS, et al. Stepwise improvement of surgical quality in robotic lateral pelvic node dissection: lessons from 100 consecutive patients with locally advanced rectal cancer. Dis Colon Rectum. 2022;65(4):599–607.
Choi GS, Kim HJ, Park JS, et al. Minimally invasive approach for lateral pelvic node dissection: a standardization based on surgical anatomy. Dis Colon Rectum. 2019;62(12):1550.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
Robotic lateral pelvic lymph node dissection (MP4 560560 kb)
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (http://creativecommons.org/licenses/by-nc-nd/4.0/), which permits any noncommercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if you modified the licensed material. You do not have permission under this license to share adapted material derived from this chapter or parts of it.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Pedrazzani, C., Turri, G., Kim, H.J., Choi, GS. (2024). Robotic Lateral Pelvic Lymph Node Dissection for Advanced Low Rectal Cancer. In: Ceccarelli, G., Coratti, A. (eds) Robotic Surgery of Colon and Rectum. Updates in Surgery. Springer, Cham. https://doi.org/10.1007/978-3-031-33020-9_12
Download citation
DOI: https://doi.org/10.1007/978-3-031-33020-9_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-33019-3
Online ISBN: 978-3-031-33020-9
eBook Packages: MedicineMedicine (R0)