Abstract
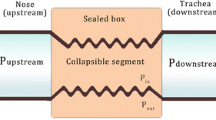
The upper airways are part of the respiratory system. The nose, lips and trachea are essential contributors to overall respiratory resistance and the conditioning of the inspired air. They play a crucial role during noninvasive ventilation (NIV), and their patency can determine success or failure. Their involvement represents a substantial difference from invasive ventilation, where the endotracheal tube bypasses the upper airways and the endotracheal tube cuff closes. During NIV, on the other hand, the airways play an essential role and determine with their characteristics the efficiency of the ventilation delivered and the ventilator’s settings. NIV can, in turn, influence their tone and their calibre. Their physiology has been the subject of multiple studies evaluating patency and collapse factors. Pathological states and the sleep-wake rhythm influence patency and collapse. Different models can explain the behaviour of the upper airways, including the “balance of forces” or the balance between the suction pressure of the airways during inspiration and the dilator tone of the upper airways. In this chapter, all these aspects will be analysed, which, as anticipated, are of fundamental importance in applying the NIV.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
Abbreviations
- ARF:
-
Acute respiratory failure
- EMG:
-
Electromyography
- GG:
-
Genioglossal activity
- NIV:
-
Noninvasive ventilation
- OSA:
-
Obstructive sleep apnoea
References
Strohl KP, Butler JP, Malhotra A. Mechanical properties of the upper airway. Compr Physiol. 2012;2(3):1853–72.
Carley DW, Farabi SS. Physiology of sleep. Diabetes Spectr. 2016;29(1):5–9. https://doi.org/10.2337/diaspect.29.1.5.
Ayappa I, Rapoport DM. The upper airway in sleep: physiology of the pharynx. Sleep Med Rev. 2003;7(1):9–33.
Passos UL, Genta PR, Marcondes BF, Lorenzi-Filho G, Gebrim EMMS. State-dependent changes in the upper airway assessed by multidetector CT in healthy individuals and during obstructive events in patients with sleep apnea. J Bras Pneumol. 2019;45(4):e20180264. Published 2019 Aug 15
Mete A, Akbudak İ. Functional anatomy and physiology of airway. In: Erbay R, editor. Tracheal intubation. IntechOpen; 2018.
Schwab RJ, Gefter WB, Pack AI, Hoffman EA. Dynamic imaging of the upper airway during respiration in normal subjects. J Appl Physiol. 1993;74(4):1504–14.
Hogg JC, Paré PD, Hackett TL. The contribution of small airway obstruction to the pathogenesis of chronic obstructive pulmonary disease. [published correction appears in Physiol rev. 2018 Jul 1;98(3):1909]. Physiol Rev. 2017;97(2):529–52.
Roy B, Samson N, Moreau-Bussière F, Ouimet A, Dorion D, Mayer S, Praud J-P. Mechanisms of active laryngeal closure during noninvasive intermittent positive pressure ventilation in nonsedated lambs. J Appl Physiol. 2008;105:1406–12.
Butler JE, Hudson AL, Gandevia SC. The neural control of human inspiratory muscles. Prog Brain Res. 2014;209:295–308.
Malhotra A, Fogel RB, Edwards JK, Shea SA, White DP. Local mechanisms drive genioglossus activation in obstructive sleep apnea. Am J Respir Crit Care Med. 2000;161(5):1746–9.
Fogel RB, Malhotra A, Shea SA, Edwards JK, White DP. Reduced genioglossal activity with upper airway anesthesia in awake patients with OSA. J Appl Physiol. 2000;88(4):1346–54.
Oliven R, Cohen G, Somri M, Schwartz AR, Oliven A. Relationship between the activity of the genioglossus, other peri-pharyngeal muscles and flow mechanics during wakefulness and sleep in patients with OSA and healthy subjects. Respir Physiol Neurobiol. 2020;274:103362.
Moreau-Bussière F, Samson N, St-Hilaire M, Reix P, Lafond JR, Nsegbe É, Praud J-P. Laryngeal response to nasal ventilation in nonsedated newborn lambs. J Appl Physiol. 2007;17:2149–57.
Rodenstein DO, Dooms G, Thomas Y, et al. Pharyngeal shape and dimensions in healthy subjects, snorers, and patients with obstructive sleep apnoea. Thorax. 1990;45:722–7.
Navalesi P, Costa R. New modes of mechanical ventilation: proportional assist ventilation, neurally adjusted ventilatory assist, and fractal ventilation. Curr Opin Crit Care. 2003;9(1):51–8.
Piquilloud L, Tassaux D, Bialais E, Lambermont B, Sottiaux T, Roeseler J, Laterre PF, Jolliet P, Revelly JP. Neurally adjusted ventilatory assist (NAVA) improves patient-ventilator interaction during non-invasive ventilation delivered by face mask. Intensive Care Med. 2012;38(10):1624–31.
Vignaux L, Vargas F, Roeseler J, Tassaux D, Thille AW, Kossowsky MP, Brochard L, Jolliet P. Patient-ventilator asynchrony during non-invasive ventilation for acute respiratory failure: a multicenter study. Intensive Care Med. 2009;35(5):840–6.
Cheng S, Butler JE, Gandevia SC, Bilston LE. Movement of the human upper airway during inspiration with and without inspiratory resistive loading. J Appl Physiol. 2010;110:69.
Bertrand PM, Futier E, Coisel Y, Matecki S, Jaber S, Constantin JM. Neurally adjusted ventilatory assist vs pressure support ventilation for noninvasive ventilation during acute respiratory failure: a crossover physiologic study. Chest. 2013;143(1):30–6.
Carron M, Freo U, BaHammam AS, et al. Complications of non-invasive ventilation techniques: a comprehensive qualitative review of randomized trials. Br J Anaesth. 2013;110:896–914.
Girault C, Briel A, Benichou J, et al. Interface strategy during noninvasive positive pressure ventilation for hypercapnic acute respiratory failure. Crit Care Med. 2009;37:124–31.
Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374:250–9.
Sassoon C. Triggering of the ventilator in patient-ventilator interactions. Respir Care. 2011;56:39–51.
Moretti M, Cilione C, Tampieri A, Fracchia C, Marchioni A, Nava S. Incidence and causes of non-invasive mechanical ventilation failure after initial success. Thorax. 2000;55:819–25.
Lemyze M, Mallat J, Nigeon O, et al. Rescue therapy by switching to total face mask after failure of face mask-delivered noninvasive ventilation in do-not intubate patients in acute respiratory failure. Crit Care Med. 2013;41:481.
Crimi C, Noto A, Princi P, et al. A European survey of noninvasive ventilation practices. Eur Respir J. 2010;36:362–9.
Fraticelli AT, Lellouche F, L’Her E, et al. Physiological effects of different interfaces during noninvasive ventilation for acute respiratory failure. Crit Care Med. 2009;37:939–45.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Fiorentino, G., Lanza, M., Annunziata, A. (2023). Relationship Between Mask Interface and Upper Airway Anatomy and Physiology. In: Esquinas, A.M., De Vito, A., Barbetakis, N. (eds) Upper Airway Disorders and Noninvasive Mechanical Ventilation. Springer, Cham. https://doi.org/10.1007/978-3-031-32487-1_11
Download citation
DOI: https://doi.org/10.1007/978-3-031-32487-1_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-32486-4
Online ISBN: 978-3-031-32487-1
eBook Packages: MedicineMedicine (R0)