Abstract
As of March 2022, the official figures of the COVID-19 crisis have hit the stunning level of nearly 500 million cases and over 6 million deaths worldwide. However, aside from the death toll that has been directly caused by the SARS-CoV-2 infection, the pandemic has also created huge collateral damage to many essential services in most health systems across the world, thus indirectly causing further casualties. To the credit of the scientific community, extensive international cooperation has allowed to develop effective COVID-19 vaccines in record-breaking times. However, this is not enough and we must now ensure that we will continue to work toward the development of technologies and logistics infrastructures that will allow us to react much more swiftly, effectively and equitably when the next pandemic hits.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
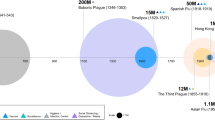
As of March 2022, the official figures of the COVID-19 health crisis have hit the stunning level of nearly 500 million cases and over 6 million deaths worldwide (source https://www.worldometers.info/coronavirus). To paint such a bleak picture as accurately as possible, since the beginning of the pandemic national health authorities have more or less diligently provided the world community with daily information on new cases and deaths within each country, thus allowing the monitoring of surges and declines of infection waves. Such crucial information has clearly been instrumental in the decision making process that has been put in place on a global scale in the effort to curb the problem. However, in early 2022, the Lancet published one of the first studies where the estimated excess mortality (defined as the observed all-cause mortality minus the expected mortality) in each country in the years 2020 and 2021 was calculated relative to pre-pandemic years [1]. Interestingly, the study provided a rather different picture from the official figures in terms of actual COVID-19-related deaths in all countries. Indeed, the study showed that most countries had largely underestimated, albeit to different extents, their reported COVID-19-related deaths, suggesting that the overall death toll of this pandemic around the world could be even three times as high as the official figures suggest. In other terms, the impact of the pandemic has quite clearly been greater than the reported deaths due to COVID-19 alone, some of which caused directly by the SARS-CoV-2 infection and other by collateral (or indirect) consequences. Interestingly, a paper published in Nature Medicine more or less in the same period analyzed the quality and the extent of essential health services such as for instance cancer screening, HIV testing, maternal health services and others in several countries during the COVID-19 pandemic, both in poor and in rich countries [2]. To provide unbiased results, the study analyzed the effect of the pandemic on 31 health services in 10 different countries: two low-income countries (Ethiopia and Haiti), six middle-income countries (Ghana, Laos, Mexico, Nepal South Africa and Thailand) and two high-income countries (Chile and South Korea). The study found that cancer screenings, TB screening and detection and HIV testing were most affected (26–96% declines), while total outpatient visits declined by 9–40%, maternal health services showed a 5–33% disruption and routine childhood vaccinations were also severely disrupted. This general picture is now emerging also by a number of similar studies conducted in all parts of the world. Clearly, as major health services declines are likely to have severe global health consequences, because of the COVID-19 crisis most governments will need to invest in restoring their disrupted health systems and provide their citizens with adequate sanitary infrastructures, in order not to compromise on life expectancy and quality of life. Moreover, what has become clear is that the world needs to prepare for future pandemics and that we must learn from the COVID-19 crisis in order to react swiftly and efficiently when the next pandemic will occur.
Among the top initiatives aimed at preventing the possible catastrophic consequences of future pandemics is the establishment of the Coalition for Epidemic Preparedness Innovations (CEPI). CEPI is a global coalition of public, private, philanthropic and civil society organizations that was set up in Davos (Switzerland) in 2017 with the goal of coordinating and financing vaccine R&D for emerging infectious diseases. The scope of the coalition is to identify priority threats, to build capabilities for rapid response to unknown threats and to move vaccine candidates through preclinical and clinical studies. So far, CEPI has received a global financial commitment from a number of donors, both at the national governments level and at the level of philanthropic organizations such as the Bill and Melinda Gates Foundation and the Wellcome Trust, to name just a few. CEPI is working toward the so-called “100 Days Mission”, whose aim is to put in place the necessary technologies and infrastructures to allow the production of safe and effective vaccines within 100 days of a new epidemic. To this end, CEPI is focusing on several known infectious diseases for which a vaccine could potentially be developed, such as Middle East respiratory syndrome-related coronavirus (MERS-CoV), severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), Nipah virus, Lassa fever, Ebola, Marburg fever, Zika, and Rift Valley fever. Moreover, CEPI aims to develop suitable vaccine technologies and approaches (mostly mRNA-based) against any potential new infectious disease that may arise unexpectedly (“Disease X”). Since its inception, CEPI has helped creating a large number of COVID-19 vaccines and has made billion of doses equitably accessible to most countries via the COVID-19 Vaccines Global Access (COVAX) initiative. Further essential components of the 100 Days Mission are the establishment of an international surveillance network for the early identification of unusual cases of flu, the development and the production of accurate and rapid diagnostic tests and the activation of a global manufacturing network to produce accurate diagnostic tools, therapeutic agents and vaccines on a global scale. In essence, the most important lesson that we must learn from the COVID-19 crisis is that international cooperation is key to reacting swiftly to emerging diseases. In this respect, it is worth mentioning that the first laboratory in the world that identified the SARS-CoV-2 Omicron variant is in Gaborone (Botswana), a laboratory established through a Harvard-Botswana partnership and funded by the NIH and by the government of Botswana.
Population growth, climate change, ecosystem degradation, industrialization, conflicts, mass migrations can all facilitate the (re)-emergence of infectious diseases. Due to the existential threat that these challenges pose on humanity, it is vital that we take a “One Health” approach to achieve optimal health outcomes on a global scale. The One Health concept is not new (it was first developed in the 1960s), but it has lately been re-discovered and widely praised by policy- and decision-makers alike as key to protect our global ecosystem and, ultimately, our own existence. In recognition of the interconnection between humans, animals, plants and the environment, the One Health approach supports the notion that human medicine, public health, veterinary medicine, ecology, ecotoxicology and all related disciplines must come together in an integrated approach to solve global scale problems. Obviously, this can only be achieved when the maximum level of international cooperation is adopted, as shown for the rapid development of effective vaccines against SARS-CoV-2.
In the last two years, since the beginning of the COVID-19 crisis, news and discussions on vaccine development and vaccine efficiency have dominated the public COVID-19 narrative. It is however worth remembering that the whole scientific community, represented also by those scientists who are not directly involved in vaccine development studies, has focused on gathering every possible piece of information to figure out ways to fight against the SARS-CoV-2 virus. In this respect, there are some analogies between the COVID-19 epidemic and the first phase of the HIV-AIDS epidemic in the 1980s, for which it became immediately clear that it would have been difficult to develop a vaccine. In the quest for alternative approaches, the 3D structures of key viral proteins (such as the HIV protease and reverse transcriptase) provided the crucial templates for a structure-based drug discovery approach that led to the development of effective drugs against HIV in a remarkably short time. SARS-CoV-2 is very different from HIV, as it belongs to a wider family of coronaviruses that feature key trimeric proteins (the “spike” proteins) on their surface that enable the virus to attach to a receptor protein that is found on cells of the human respiratory system (the ACE2 receptor). In addition, the virus has two proteases that are very interesting potential targets for drug design. Within a few weeks from the onset of the COVID-19 pandemic, scientific cooperation had already led to the determination of the 3D structure of vital SARS-CoV-2 virus proteins using either X-ray crystallography or cryo-EM. Among these, the main protease [3], the spike protein [4, 5], the viral RNA polymerase [6] and the human ACE2 receptor [7]. These structures allowed the mapping of the interaction of the SARS-CoV-2 spike protein with the ACE2 receptor and, in turn, the mapping of the effects of critical mutations on the SARS-CoV-2 protein. In essence, in a remarkably short time, the scientific community was able to react to the onset of the COVID-19 pandemic and to provide crucial information and technologies that led to a global unprecedented response to the most severe public health crisis of the last 100 years. This clearly indicates that open, participatory and collaborative science is the only way forward to fight not only against future pandemics but also against the multiple existential threats that humanity will have to face in the years to come.
Finally, I would like to end my talk by paying tribute to the late Dr. Paul Farmer, whose premature death this year has left a huge void in the public health arena. The seminal work that Dr. Farmer has done in Haiti, Rwanda and in other developing countries through his “Partners in Health” organization will remain as a testimony of the power of public health approaches that put the health of the entire global community, no one left behind, at the center of the political discourse.
References
H. Wang et al., Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet 399, 1513–1536 (2022)
C. Arsenault et al., COVID-19 and resilience of healthcare systems in ten countries. Nat. Med. 28, 1314–1324 (2022)
Z. Jin et al., Structure of M pro from SARS-CoV-2 and discovery of its inhibitors. Nature 582, 289–293 (2020)
A.C. Walls et al., Structure, function, and antigenicity of the SARS-CoV-2 Spike glycoprotein. Cell 181, 281–292 (2020)
D. Wrapp et al., Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 367, 1260–1263 (2020)
Q. Wang at al., Structural basis for RNA replication by the SARS-CoV-2 Polymerase. Cell 182, 417–428 (2020)
R. Yan et al., Structural basis for bivalent binding and inhibition of SARS-CoV-2 infection by human potent neutralizing antibodies. Cell Res. 31, 517–525 (2021)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this paper
Cite this paper
Parisini, E. (2023). International Cooperation to Tackle Future Pandemics. In: Cotta-Ramusino, P., Lowenthal, M., Maiani, L., Pellecchia, E. (eds) Nuclear Risks and Arms Control - Problems and Progresses in the Time of Pandemics and War. EAC 2022. Springer Proceedings in Physics, vol 291. Springer, Cham. https://doi.org/10.1007/978-3-031-29708-3_6
Download citation
DOI: https://doi.org/10.1007/978-3-031-29708-3_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-29707-6
Online ISBN: 978-3-031-29708-3
eBook Packages: Physics and AstronomyPhysics and Astronomy (R0)