Abstract
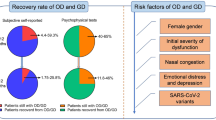
This chapter will consider the viral pathogen that has left an indelible mark on our lives and our world and look at the evidence for how it causes its pathophysiology inside the nose, with specific reference to the sense of smell. Although taste buds are not located in the nasal cavity, the chapter will also consider the mechanisms of action of the virus on the sense of taste due to the inherent associations with smell. Finally, the chapter will consider specific therapeutic implications for those affected by COVID-19-related chemosensory disturbances.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Safiabadi Tali SH, LeBlanc JJ, Sadiq Z, Oyewunmi OD, Camargo C, Nikpour B, et al. Tools and techniques for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)/COVID-19 detection. Clin Microbiol Rev. 2021;34(3)
Yuen E, Gudis DA, Rowan NR, Nguyen SA, Schlosser RJ. Viral infections of the upper airway in the setting of COVID-19: a primer for rhinologists. Am J Rhinol Allergy. 2021;35(1):122–31.
Rockx B, Kuiken T, Herfst S, Bestebroer T, Lamers MM, Oude Munnink BB, et al. Comparative pathogenesis of COVID-19, MERS, and SARS in a nonhuman primate model. Science. 2020;368(6494):1012–5.
McCray PB Jr, Pewe L, Wohlford-Lenane C, Hickey M, Manzel L, Shi L, et al. Lethal infection of K18-hACE2 mice infected with severe acute respiratory syndrome coronavirus. J Virol. 2007;81(2):813–21.
Rocke J, Hopkins C, Philpott C, Kumar N. Is loss of sense of smell a diagnostic marker in COVID-19: A systematic review and meta-analysis. Clin Otolaryngol. 2020;45(6):914–22.
Parma V, Ohla K, Veldhuizen MG, Niv MY, Kelly CE, Bakke AJ, et al. More than smell—COVID-19 is associated with severe impairment of smell, taste, and chemesthesis. Chem Senses. 2020;45(7):609–22.
Lechner M, Liu J, Counsell N, Ta NH, Rocke J, Anmolsingh R, et al. Course of symptoms for loss of sense of smell and taste over time in one thousand forty-one healthcare workers during the Covid-19 pandemic: our experience. Clin Otolaryngol. 2021;46(2):451–7.
Brann DH, Tsukahara T, Weinreb C, Lipovsek M, Van den Berge K, Gong B, et al. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Sci Adv. 2020;6(31)
Pacheco-Herrero M, Soto-Rojas LO, Harrington CR, Flores-Martinez YM, Villegas-Rojas MM, Leon-Aguilar AM, et al. Elucidating the neuropathologic mechanisms of SARS-CoV-2 infection. Front Neurol. 2021;12:660087.
Lim AY, Cheong HK, Oh YJ, Lee JK, So JB, Kim HJ, et al. Modeling the early temporal dynamics of viral load in respiratory tract specimens of COVID-19 patients in Incheon, the Republic of Korea. Int J Infect Dis. 2021;108:428–34.
Wang H, Liu Q, Hu J, Zhou M, Yu MQ, Li KY, et al. Nasopharyngeal swabs are more sensitive than oropharyngeal swabs for COVID-19 diagnosis and monitoring the SARS-CoV-2 load. Front Med-Lausanne. 2020:7.
Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–7.
Vofo G, Brodie R, Gross M. Nasal lavage containing Angiotensin-Converting Enzyme-2 agonist can prevent and reduce viral load in COVID-19. Med Hypotheses. 2020;144
Matschke J, Lutgehetmann M, Hagel C, Sperhake JP, Schroder AS, Edler C, et al. Neuropathology of patients with COVID-19 in Germany: a post-mortem case series. Lancet Neurol. 2020;19(11):919–29.
Solomon IH, Normandin E, Bhattacharyya S, Mukerji SS, Keller K, Ali AS, et al. Neuropathological features of covid-19. New Engl J Med. 2020;383(10):989–92.
Butowt R, von Bartheld CS. Anosmia in COVID-19: underlying mechanisms and assessment of an olfactory route to brain infection. Neuroscientist. 2020;1073858420956905
Lochhead JJ, Thorne RG. Intranasal delivery of biologics to the central nervous system. Adv Drug Deliv Rev. 2012;64(7):614–28.
Bryche B, St Albin A, Murri S, Lacote S, Pulido C, Ar Gouilh M, et al. Massive transient damage of the olfactory epithelium associated with infection of sustentacular cells by SARS-CoV-2 in golden Syrian hamsters. Brain Behav Immun. 2020;89:579–86.
Walsh-Messinger J, Kaouk S, Manis H, Kaye R, Cecchi G, Meyer P, et al. Standardized testing demonstrates altered odor detection sensitivity and hedonics in asymptomatic college students as SARS-CoV-2 emerged locally. medRxiv. 2020;
Lee JC, Nallani R, Cass L, Bhalla V, Chiu AG, Villwock JA. A systematic review of the neuropathologic findings of post-viral olfactory dysfunction: implications and novel insight for the COVID-19 pandemic. Am J Rhinol Allergy. 2021;35(3):323–33.
Mueller A, Rodewald A, Reden J, Gerber J, von Kummer R, Hummel T. Reduced olfactory bulb volume in post-traumatic and post-infectious olfactory dysfunction. Neuroreport. 2005;16(5):475–8.
Rashid RA, Alaqeedy AA, Al-Ani RM. Parosmia due to COVID-19 disease: a 268 case series. Indian J Otolaryngol. 2022;74:2970–7.
Huart C, Philpott C, Konstantinidis I, Altundag A, Whitcroft KL, Trecca EMC, et al. Comparison of COVID-19 and common cold chemosensory dysfunction. Rhinology. 2020;58(6):623–5.
Wang H, Zhou M, Brand J, Huang L. Inflammation and taste disorders: mechanisms in taste buds. Ann N Y Acad Sci. 2009;1170:596–603.
Okada Y, Yoshimura K, Toya S, Tsuchimochi M. Pathogenesis of taste impairment and salivary dysfunction in COVID-19 patients. Jpn Dent Sci Rev. 2021;57:111–22.
Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 2020;92(6):552–5.
Addison AB, Wong B, Ahmed T, Macchi A, Konstantinidis I, Huart C, et al. Clinical Olfactory Working Group consensus statement on the treatment of postinfectious olfactory dysfunction. J Allergy Clin Immunol. 2021;147(5):1704–19.
Hopkins C, Alanin M, Philpott C, Harries P, Whitcroft K, Qureishi A, et al. Management of new onset loss of sense of smell during the COVID-19 pandemic—BRS Consensus Guidelines. Clin Otolaryngol. 2021;46(1):16–22.
Huart C, Philpott CM, Altundag A, Fjaeldstad AW, Frasnelli J, Gane S, et al. Systemic corticosteroids in coronavirus disease 2019 (COVID-19)-related smell dysfunction: an international view. Int Forum Allergy Rhinol. 2021;
Webster KE, MacKeith S, Philpott C, Hopkins C, Burton MJ. Interventions for the treatment of persistent post-COVID-19 olfactory dysfunction. Cochrane Database Syst Rev. 2021;2
Philpott C, Dixon J, Boak D. Qualitative olfactory disorders: patient experiences and self-management. Allergy Rhinol (Providence). 2021;12:21526567211004251.
Philpott CM, Boardman J, Boak D. Patient experiences of postinfectious olfactory dysfunction. ORL J Otorhinolaryngol Relat Spec. 2021;83:299–303.
Liu DT, Sabha M, Damm M, Philpott C, Oleszkiewicz A, Hähner A, et al. Parosmia is associated with relevant olfactory recovery after olfactory training. Laryngoscope. 2021;131:618–23.
Reden J, Mueller A, Mueller C, Konstantinidis I, Frasnelli J, Landis BN, et al. Recovery of olfactory function following closed head injury or infections of the upper respiratory tract. Arch Otolaryngol Head Neck Surg. 2006;132(3):265–9.
Hummel T, Whitcroft KL, Andrews P, Altundag A, Cinghi C, Costanzo RM, et al. Position paper on olfactory dysfunction. Rhinol Suppl. 2017;54(26):1–30.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Philpott, C. (2023). The Nose and the Effects of SARS-CoV-2 Pandemic. In: Swift, A.C., Carrie, S., de Souza, C. (eds) Contemporary Rhinology: Science and Practice. Springer, Cham. https://doi.org/10.1007/978-3-031-28690-2_11
Download citation
DOI: https://doi.org/10.1007/978-3-031-28690-2_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-28689-6
Online ISBN: 978-3-031-28690-2
eBook Packages: MedicineMedicine (R0)