Abstract
Over several decades the perception and therefore description of articular cartilage changed substantially. It has transitioned from being described as a relatively inert tissue with limited repair capacity, to a tissue undergoing continuous maintenance and even adaption, through a range of complex regulatory processes. Even from the narrower lens of biomechanics, the engagement with articular cartilage has changed from it being an interesting, slippery material found in the hostile mechanical environment between opposing long bones, to an intriguing example of mechanobiology in action. The progress revealing this complexity, where physics, chemistry, material science and biology are merging, has been described with increasingly sophisticated computational models. Here we describe how these computational models of cartilage as an integrated system can be combined with the approach of structural reliability analysis. That is, causal, deterministic models placed in the framework of the probabilistic approach of structural reliability analysis could be used to understand, predict, and mitigate the risk of cartilage failure or pathology. At the heart of this approach is seeing cartilage overuse and disease processes as a ‘material failure’, resulting in failure to perform its function, which is largely mechanical. One can then describe pathways to failure, for example, how homeostatic repair processes can be overwhelmed leading to a compromised tissue. To illustrate this ‘pathways to failure’ approach, we use the interplay between cartilage consolidation and lubrication to analyse the increase in expected wear rates associated with cartilage defects or meniscectomy.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Over the past ~40 years, incredible advances have been made in cartilage biology. We are thinking about the finding that transient compressive stiffness arises from low hydraulic conductivity of cartilage and collagen network stiffness, how the equilibrium cartilage compressive stiffness arises primarily from repulsion between negatively charged aggrecan, the interplay between the aggrecan compression and the collagen tension to maintain normal cartilage stiffness, and how turnover of these ECM components is regulated by chondrocytes via chemical, electromechanical and mechanical signals [1,2,3,4,5,6,7,8]. These insights, often gained by patient work on individual processes or isolated molecules, have been integrated to present a compelling story of how this tissue functions in both the short term (to an individual loading) and the long-term (to repeated cyclic loadings), and potential pathways to pathology [8]. With the insight made possible by understanding this integrated system, we are only just beginning to develop rational strategies to intervene at the tissue scale to maintain or reverse cartilage damage.
Meanwhile great advances have also occurred in imaging and computational biomechanics, genetics and genetic manipulations that may soon enable patient (or cohort) specific data to be incorporated into cartilage treatment strategies [9, 10]. How best to do this is still in its infancy, and so largely an open question, but it holds such promise. Our belief is that this way forward will no doubt be computational (i.e. based on deterministic quantitative mechanistic models of cartilage tissue turnover in response to its mechanical and chemical environment), but will also necessarily include statistical aspects (e.g. variable loadings and model tissue parameters over time and/or population). More to our point, we believe the concepts of risk analysis borrowed from reliability engineering, provides a promising framework to shepherd our hard-won understanding of cartilage biology into the clinic [11, 12]. Here we will expand on these ideas. In doing so we will necessarily review some cartilage biology. However, the focus will be on identifying strategies cartilage uses to maintain and repair itself, and the pathways to cartilage ‘failure’, however failure may be defined. This approach promises to enable the risk associated with various ‘disease pathways’ in an individual or patient cohort to be rationally quantified, and then managed.
2 Articular Cartilage, an Extraordinary Tissue
Articular cartilage faces extraordinary mechanical challenges during daily physical activities. For example, knee cartilages in adults experience contact forces up to 5 times the body weight during stair climbing [13], leading to contact stresses up to 18 MPa. To get this loading in perspective, we note that a large stiletto heel exerts about 10 MPa pressure on the ground, and this contact stress is well-known for damaging some wooden floors—while cartilage tissue repeatedly experiences stresses that are almost twice as great. Probably due to this harsh mechanical environment, cartilage is an avascular tissue with a sparse chondrocyte to extracellular matrix (ECM) distribution, which limits its repair capacity. All tissues that normally repair quickly have abundant blood supplies, while in contrast, cartilage relies solely on diffusion/advection of nutrients and oxygen from synovial fluid that bathes its contact surface, with the subchondral bone- cartilage interface generally considered impermeable in healthy joints. Consequently, articular cartilage function and homeostasis largely rely on complex interactions between its main extracellular components: interstitial fluid, aggrecan and a Type II collagen network [5, 8]. For example, the rate of tissue strain under sustained load largely depends on the interstitial fluid movement through the cartilage tissue and across the cartilage surfaces, influencing the mechanical and chemical microenvironments continually being sensed by chondrocytes, while the fluid contributes to synovial joint lubrication [5, 14]. When cartilage is subjected to compressive loading, it consolidates. The load is initially carried by the fluid phase, which is slowly squeezed out of the extracellular matrix, helping to sustain very low frictional force between two opposing cartilage surfaces. As cartilage interstitial fluid exudes through the tissue surface, load is gradually transferred to the solid matrix, resulting in a gradual increase in friction at contacting surfaces.
3 Cartilage Damage Mechanics
The ability of cartilage to maintain its physiological function in this hostile mechanical environment depends on the tissue’s ability to continually synthesize extracellular matrix components, while avoiding excessive strain, an attribute normally conferred by its composite structure. Aggrecans are negatively charged molecules that have counter ions in a diffuse double-layer to maintain overall electroneutrality. Overlapping double-layers repel and so normally expand and imbibe water. However, this expansion is resisted by the collagen network [15]. The aggrecan molecules within the collagen network normally provide the equilibrium compressive stiffness for cartilage tissue [16], and ensure a very small hydraulic permeability which delays consolidation of the tissue to its equilibrium state. Consequently, when loaded, a long consolidation time follows (e.g. up to three or more hours).
As shown schematically in Fig. 6.1, a damaged collagen network is not able to effectively retain a high enough concentration of aggrecan molecules within the collagen network, which leads to cartilage softening [17]. Reduced aggrecan content also leads to larger hydraulic conductivity, more rapid consolidation and larger strains. This means the aggregate, collagen tissue network and chondrocytes are more likely to be damaged by excessive strain (following even normal load), leading to further loss of aggrecan [18]. This positive feedback cycle is just one important pathway that can lead to disease such as osteoarthritis. One can imagine many more and so osteoarthritis is not just one disease [8, 19]. Its management is likely to also differ depending on the etiology.
4 Role of Computational Modelling to Capture Complex Interactions
A key attraction of computational modeling is that it can be employed to reveal the spatial and temporal distribution of tissue microenvironments experienced by chondrocytes embedded within articular cartilage. This involves interpolating sparse experimental data sets, often measured at tissue boundaries, to define local conditions experienced by chondrocytes throughout the cartilage tissue. This immediately opens up the possibility of beginning to define previously inaccessible variables that are likely to be driving local ECM damage and chondrocyte repair processes within articular cartilage. This new capability, together with experimentally calibrated computational damage and repair functions, then naturally leads to predictions about the integrity of cartilage under various short and long-term scenarios.
Through this process, computational modeling can provide a pathway from laboratory data to quantitative predictions about future tissue states under various scenarios. This should be of great interest to clinicians, as they are in the business of advising patients as to the optimal path to follow in response to their problem. The process of building and calibrating computational models of cartilage tissue also offers up the possibility of a new pathway to more effective use of the new data being generated by ‘precision medicine’ for individual patients.
There are many chemical molecules and mechanical cues that regulate articular cartilage homeostasis. Therefore, to realistically define cartilage microenvironments requires consideration of interactions between many specific and rather detailed computational modules (involving multi-physics and multiphasic modelling). The theory of porous media has been widely employed to simulate the mechanical behaviour of biological soft tissues, such as articular cartilage [20,21,22,23,24,25] and fracture callus [26,27,28]. Here the extracellular matrix and interstitial fluid interaction contributes to the time-dependent observed tissue stiffness and deformation behaviour. By combining the porous media theory with transport models and chemical reactions, we can also simulate three-dimensional diffusion and advection of different molecules in cartilage, and use this information to predict different cellular activities [14, 29,30,31,32,33,34,35,36]. For example, insulin-like growth factors mediate cartilage cellular activities such as cell proliferation, differentiation, apoptosis and synthesis of extracellular matrix [32, 37, 38]. We have built a spatial model for IGF in cartilage tissue that includes many simultaneous chemical reactions, as well as transport parameters [36]. Each of these parameters depends on the actual chemical structure of IGF and its binding proteins, as these determine the chemical rate constants that define their interactions. These rate constants depend on the amino acid sequence in each molecule, which in turn depends on the genetic code in that individual. If the genetic code is known, as revealed by precision medicine, it should be possible to predict the effect of that person’s genetic code on the chemical rate constants, enabling the creation of customized computational models for each individual’s IGF system for their cartilage. By this means, we can bridge the information gap between genetic data and what this data actually means in the context of a tissue.
This same principle can be applied to all the other chemical molecules found in cartilage tissue. For example, the inflammatory cytokine IL-1a is known to modulate biochemical degradation of cartilage tissue following a traumatic joint injury, so we built a detailed model of IL-1beta in cartilage, and calibrated the model using detailed experimental data generated exclusively in the Grodzinsky lab [37]. The model simulated the experimental observation of biochemical degradation of bovine articular cartilage explants. The developed model can help improve our understanding of in vivo events after a joint injury and potentially be employed for assessing the influence of different therapeutic molecules on osteoarthritis management [39, 40].
Since the biochemical signaling pathways are influenced by the mechanical microenvironment of cartilage, we built a mechanical model of cartilage. We have developed and published a state-of-the-art biphasic model of cartilage mechanics that is validated against ex-vivo mechanical experiments on human osteochondral plugs subject to cyclic loading [22]. The model takes into account tensile loading being carried by the collagen network, and compressive load carried by water and aggrecan. The model has a non-linear compressive stiffness and non-linear hydraulic permeability based on the aggrecan concentration, which changes as the cartilage tissue deforms. As such this model represents a new constitutive model of articular cartilage, which helps provide a sound foundation for new models describing cartilage damage and repair modelling (Fig. 6.2).
Our cartilage mechanics model can accurately reproduce experimental data of time-course of deformation in both the loading and recovery phase of the experiment. (Figure adapted from Zhang et al. [22] with permission)
5 Using Models to Investigate Pathways to Cartilage Failure
Synovial joint lubrication is one of the key roles of articular cartilage. Synovial joints can experience very small frictional force, with initial friction coefficient ranging from 0.005 to 0.02, while bearing extremely large mechanical stress [41, 42]. However, experimental studies have shown that the cartilage friction coefficient can rise with time (~minutes) under loading [43, 44]. Our computational modelling in conjunction with experimental observations have shown that there is a strong correlation between cartilage friction coefficient and the degree of cartilage consolidation. This suggests that after prolonged period of loading, in particular stationary activities (e.g. standing), consolidation has occurred and friction coefficient rises (Fig. 6.3). The cartilage surface can experience relatively large friction coefficient (e.g. 0.2–0.3, with subsequent additional cartilage damage likely as motion recommences).
There is a strong correlation between degree of consolidation of articular cartilage and friction coefficient in synovial joint. (This figure has been reproduced from Miramini et al. [45] with permission)
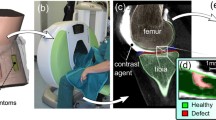
It is known that large frictional force at the joints can result in elevated cartilage surface wear and damage and cartilage delamination. A well calibrated and patient-specific computational modelling can help us simulate the likely impact of physical activities on synovial joint health and thereby design patient-specific physical therapy activities for management of osteoarthritis We have incorporated different joint states such as meniscectomy and cartilage surface defects, and simulated cartilage time-dependent lubrication. As shown in Fig. 6.4, the response of damaged cartilage, to the same loading conditions, was a faster rate of consolidation and quicker increase in surface friction coefficient. The expectation then is these compromised joints will experience a higher average friction coefficient, than a healthy cartilage, and so a higher surface wear rate. Knowing this, from medical history (e.g. observation of defects in MRI) it is possible to devise activities that minimize the likelihood of these adverse situations occurring, thereby increasing the likelihood cartilage will maintain its functional integrity.
A faster consolidation is predicted for cartilage with meniscectomy and the one with a full thickness defect. (This figure has been adapted from Miramini et al. [45] with permission)
Although we have shown above that defects and meniscectomies can increase consolidation and extend the time a cartilage surface experiences high friction, we still do not know how critical this is in a particular individual. The load the joint experiences depends on factors such as body weight, joint size and shape, limb geometry and lifestyle. Some of these biomechanical aspects can be incorporated for an individual through a combination of imaging and gait analysis to predict joint loads. In addition, the functional mechanical properties of the cartilage tissue are also expected to vary in a population due to genetic and environmental histories. These factors can be also incorporated in patient -specific simulation.
Computational modelling can also assist clinicians in assessment of cartilage health. For example, we can assess cartilage tissue functional properties by combined fluoroscopic and MRI imaging of the knee in a standing still posture and measuring the degree of joint closure over time [46]. The calculated degree of consolidation of knee joint together with computational modelling enable evaluation of knee joint ability to sustain interstitial fluid pressure and so experience a normal low surface friction coefficient [45].
6 Probabilistic Modelling and Osteoarthritis Risk Assessment
As alluded to above, there are numerous uncertainties and variability associated with the parameters affecting cartilage behaviour. For example, cartilage loading condition depends on many factors including physical activity, body weight and joint anatomy. In addition, the physical properties of cartilage also remain uncertain and depend on factors such as age, joint health and genetic factors. Therefore, it is of critical importance to consider the uncertainty and variability of different factors when simulating cartilage behaviors. Probabilistic analysis has been traditionally developed and employed for reliability assessment of engineering structure such as bridges and nuclear power stations. Compared with a deterministic approach that adopts a discrete value for a specific model parameter, a probabilistic modelling approach takes into account the distribution of environmental factors and model parameters in the deterministic calculation and therefore generates a distribution of tissue trajectories (including pathways to disease) and therefore outcomes. In the context of engineering, we can define the ‘probability of failure’ as the likelihood of exceeding some pre-determined state critical to the functional performance of the engineered structure. For example, it might be the probability of a load exceeding the structure’s (e.g. a bridge’s) strength, or the probability of a load exceeding a certain level of deformation in the structure, or the probability of environmental factors causing a certain level of material damage (e.g. component fatigue damage, irradiation damage, or corrosion damage). Reliability can be defined as one minus the probability of failure. In the context of loading a structure, the probability of failure can be defined as the overlap between the probability density function of a ‘generalized loading’ applied on the structure and probability density function of the structure ‘generalized resistance’, as shown in Fig. 6.5.
The probability of failure of a structure can be estimated by finding the overlapping area under the probability density functions of generalized load and generalized resistance. (Figure adapted with permission from Miramini and Yang [47])
Recently, we have used this approach to predict the likelihood of knee osteoarthritis [9]. This was done on the basis of a simple model of chondrocyte ECM synthesis in response to loading and the possibility for chondrocyte apoptosis under that load. Failure was defined by the ability to resist a test load (i.e. not exceed a maximum strain threshold). The model predicted that low activity leads to low ECM synthesis and so a gradual softening of the tissue. High activity increases ECM synthesis but also exposure to excessive loads. The probabilistic predictions had the median time to onset of failure occurred earlier in the low activity model, and with a relatively narrow uncertainty in onset time. The high activity level had a delayed median onset, but had much wider distribution of failure onset, relative to the low activity predictions [9].
In addition, we have recently developed a multi-scale probabilistic computational model (Fig. 6.6) to simulate the cartilage lubrication behaviour by incorporating the uncertainties associated with the key variables governing cartilage contact gap mechanics [48,49,50]. The model takes into account the internal relation between different variables and their correlated influence on cartilage lubrication. The simulation results show that an increase of polymer brush border thickness at the cartilage surface improves the hydrodynamic lubrication of cartilage, while the increasing surficial GAG content of the cartilage and increasing asperity stiffness could negatively affect hydrodynamic lubrication. Finally, we note that this probabilistic approach has also been adopted to estimate the probability of delayed bone fracture healing [47, 51].
Probabilistic computational model of cartilage lubrication. (Figure adapted with permission from Liao et al. [48])
7 Conclusion
To conclude, we are reaching a stage where it is now possible to connect all the pieces together into a whole picture of articular cartilage homeostasis and to identify pathways to disease. Computational modeling seems to be the natural platform upon which to integrate, into their proper context, the many interacting processes involved. Here we presented various mechanistic sub-models describing aspects of articular cartilage health. However we have also advocated for the merging of these mechanistic sub-models with the statistical-based models or approaches from (structural) reliability engineering. This then can provide a ‘bridge’ between the molecular and cell biology, biomechanics and epidemiology of osteoarthritis to give a rational basis for patient specific treatments. Although all the computational approaches are present to make this approach possible, the barriers to its adoption depends, not the least, on the adoption by clinicians.
References
Kisiday J et al (2002) Self-assembling peptide hydrogel fosters chondrocyte extracellular matrix production and cell division: implications for cartilage tissue repair. Proc Natl Acad Sci 99(15):9996–10001
Buschmann MD, Gluzband YA, Grodzinsky AJ, Hunziker EB (1995) Mechanical compression modulates matrix biosynthesis in chondrocyte/agarose culture. J Cell Sci 108(4):1497–1508
Vunjak-Novakovic G et al (1999) Bioreactor cultivation conditions modulate the composition and mechanical properties of tissue-engineered cartilage. J Orthop Res 17(1):130–138
Buckwalter JA, Mankin HJ, Grodzinsky AJ (2005) Articular cartilage and osteoarthritis, vol 54. Instructional Course Lectures-American Academy of Orthopaedic Surgeons, p 465
Grodzinsky AJ, Levenston ME, Jin M, Frank EH (2000) Cartilage tissue remodeling in response to mechanical forces. Annu Rev Biomed Eng 2(1):691–713
Buschmann MD, Gluzband YA, Grodzinsky AJ, Kimura JH, Hunziker EB (1992) Chondrocytes in agarose culture synthesize a mechanically functional extracellular matrix. J Orthop Res 10(6):745–758
Gray ML, Pizzanelli AM, Grodzinsky AJ, Lee RC (1988) Mechanical and physicochemical determinants of the chondrocyte biosynthetic response. J Orthop Res 6(6):777–792
Smith DW, Gardiner BS, Zhang L, Grodzinsky AJ (2019) Articular cartilage dynamics. Springer, Singapore
Gardiner BS et al (2016) Predicting knee osteoarthritis. Ann Biomed Eng 44(1):222–233
Fregly BJ et al (2012) Grand challenge competition to predict in vivo knee loads. J Orthop Res 30(4):503
Melchers RE (1999) Structural reliability analysis and prediction, 2nd edn. Wiley, England
Tobias P, Trindade D (2012) Applied reliability, 3rd edn. Taylor & Francis, Boca Raton
Taylor WR, Heller MO, Bergmann G, Duda GN (2004) Tibio-femoral loading during human gait and stair climbing. J Orthop Res 22(3):625–632
Zhang L, Gardiner BS, Smith DW, Pivonka P, Grodzinsky A (2008) A fully coupled poroelastic reactive-transport model of cartilage. Mol Cell Biomech 5(2):133
Smith DW, Gardiner BS, Davidson J, Grodzinsky AJ (2016) Computational model for the analysis of cartilage and cartilage tissue constructs. J Tissue Eng Regen Med 19(10):1160–1170
Basser PJ, Schneiderman R, R. A. Bank, Wachtel E, Maroudas A (1998) Mechanical properties of the collagen network in human articular cartilage as measured by osmotic stress technique. Arch Biochem Biophys 351(2):207–219
Poole A et al (1993) Osteoarthritis in the human knee: a dynamic process of cartilage matrix degradation, synthesis and reorganization. Agents Actions Suppl 39:3–13
Loening AM et al (2000) Injurious mechanical compression of bovine articular cartilage induces chondrocyte apoptosis. Arch Biochem Biophys 381(2):205–212
Dell’Isola A, Steultjens M (2018) Classification of patients with knee osteoarthritis in clinical phenotypes: Data from the osteoarthritis initiative. PloS One 13(1):e0191045
Liao J, Smith DW, Miramini S, Gardiner BS, Zhang L (2020) A coupled contact model of cartilage lubrication in the mixed-mode regime under static compression. Tribol Int 145:106185
Liao J, Smith DW, Miramini S, Thibbotuwawa N, Gardiner BS, Zhang L (2019) The investigation of fluid flow in cartilage contact gap. J Mech Behav Biomed Mater 95:153–164
Zhang L, Miramini S, Gardiner BS, Smith DW, Grodzinsky AJ (2015) Time evolution of deformation in a human cartilage under cyclic loading. Ann Biomed Eng 43(5):1166–1177
Ateshian G, Lai W, Zhu W, Mow V (1994) An asymptotic solution for the contact of two biphasic cartilage layers. J Biomech 27(11):1347–1360
Ateshian GA (2009) The role of interstitial fluid pressurization in articular cartilage lubrication. J Biomech 42(9):1163–1176
Soltz MA, Ateshian GA (2000) A conewise linear elasticity mixture model for the analysis of tension-compression nonlinearity in articular cartilage. J Biomech Eng 122(6):576–586
Ganadhiepan G et al (2019) The Effects of Dynamic Loading on Bone Fracture Healing Under Ilizarov Circular Fixators. J Biomech Eng 141(5):051005
Ghimire S, Miramini S, Richardson M, Mendis P, Zhang L (2018) Role of dynamic loading on early stage of bone fracture healing. Ann Biomed Eng 46(11):1768–1784
Ganadhiepan G, Miramini S, Patel M, Mendis P, Zhang L (2021) Optimal time-dependent levels of weight-bearing for bone fracture healing under Ilizarov circular fixators. J Mech Behav Biomed Mater 121:104611
Zhang L (2011) Solute transport in cyclic deformed heterogeneous articular cartilage. Int J Appl Mech 3(03):507–524
Zhang L, Gardiner BS, Smith DW, Pivonka P, Grodzinsky A (2007) The effect of cyclic deformation and solute binding on solute transport in cartilage. Arch Biochem Biophys 457(1):47–56
Zhang L, Gardiner BS, Smith DW, Pivonka P, Grodzinsky AJ (2008) IGF uptake with competitive binding in articular cartilage. J Biol Syst 16(02):175–195
Zhang L, Gardiner BS, Smith DW, Pivonka P, Grodzinsky AJ (2009) Integrated model of IGF-I mediated biosynthesis in a deformed articular cartilage. J Eng Mech 135(5):439–449
Zhang L, Gardiner BS, Smith DW, Pivonka P, Grodzinsky AJ (2010) On the role of diffusible binding partners in modulating the transport and concentration of proteins in tissues. J Theor Biol 263(1):20–29
Zhang L, Gardiner BS, Smith DW, Pivonka P, Grodzinsky AJ (2010) The transport of insulin-like growth factor through cartilage. In: Vafai K (ed) Porous media: applications in biological systems and biotechnology. Taylor & Francis Group, pp 399–453
Zhang L, Gardiner BS, Smith DW, Pivonka P, Grodzinsky AJ (2009) Integrated model of IGF-I mediated biosynthesis in deforming articular cartilage. J Eng Mech 135(3):439–449
Zhang L, Smith DW, Gardiner BS, Grodzinsky AJ (2013) Modeling the insulin-like growth factor system in articular cartilage. PLoS One 8(6):e66870
Li Y et al (2015) Effects of insulin-like growth factor-1 and dexamethasone on cytokine-challenged cartilage: relevance to post-traumatic osteoarthritis. Osteoarthr Cartil 23(2):266–274
Bonassar LJ, Grodzinsky AJ, Srinivasan A, Davila SG, Trippel SB (2000) Mechanical and physicochemical regulation of the action of insulin-like growth factor-I on articular cartilage. Arch Biochem Biophys 379(1):57–63
Kar S, Smith DW, Gardiner BS, Li Y, Wang Y, Grodzinsky AJ (2016) Modeling IL-1 induced degradation of articular cartilage. Arch Biochem Biophys 594:37–53
Kar S, Smith DW, Gardiner BS, Grodzinsky AJ (2016) Systems based study of the therapeutic potential of small charged molecules for the inhibition of IL-1 mediated cartilage degradation. PLoS One 11(12):e0168047
Merkher Y, Sivan S, Etsion I, Maroudas A, Halperin G, Yosef A (2006) A rational human joint friction test using a human cartilage-on-cartilage arrangement. Tribol Lett 22(1):29–36. [Online]
Longmore RB, Gardner DL (1975) Development with age of human articular cartilage surface structure. A survey by interference microscopy of the lateral femoral condyle. Ann Rheum Dis 34(1):26–2. [Online]
Forster H, Fisher J (1999) The influence of continuous sliding and subsequent surface wear on the friction of articular cartilage. Proc Inst Mech Eng H J Eng Med 213(4):329–345
Forster H, Fisher J (1996) The influence of loading time and lubricant on the friction of articular cartilage. Proc Inst Mech Eng H 210(2):109–119. [Online]
Miramini S, Smith DW, Zhang L, Gardiner BS (2017) The spatio-temporal mechanical environment of healthy and injured human cartilage during sustained activity and its role in cartilage damage. J Mech Behav Biomed Mater 74:1–10
Hosseini A et al (2010) In-vivo time-dependent articular cartilage contact behavior of the tibiofemoral joint. Osteoarthr Cartil 18(7):909–916
Miramini S, Yang Y (2019) A probabilistic-based approach for computational simulation of bone fracture healing. Comput Methods Programs Biomed 180:105011
Liao J, Smith DW, Miramini S, Gardiner BS, Zhang L (2021) A probabilistic failure risk approach to the problem of articular cartilage lubrication. Comput Methods Prog Biomed 203:106053
Liao J, Miramini S, Liu X, Zhang L (2020) Computational study on synovial fluid flow behaviour in cartilage contact gap under osteoarthritic condition. Comput Biol Med 123:103915
Liao J, Smith DW, Miramini S, Gardiner BS, Zhang L (2021) Investigation of role of cartilage surface polymer brush border in lubrication of biological joints. Friction 10:1–18
Ganadhiepan G, Miramini S, Mendis P, Patel M, Zhang L (2021) A probabilistic approach for modelling bone fracture healing under Ilizarov circular fixator. Int J Numer Method Biomed Eng 37:e3466
Acknowledgements
The authors would like to thank Alan J. Grodzinsky for his enthusiasm, openness and endless support and encouragement to us over many, many years. We would also like to acknowledge the support of Australian Research Council (ARC DP180100915).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Miramini, S., Smith, D.W., Gardiner, B.S., Zhang, L. (2023). Computational Modelling for Managing Pathways to Cartilage Failure. In: Connizzo, B.K., Han, L., Sah, R.L. (eds) Electromechanobiology of Cartilage and Osteoarthritis. Advances in Experimental Medicine and Biology, vol 1402. Springer, Cham. https://doi.org/10.1007/978-3-031-25588-5_6
Download citation
DOI: https://doi.org/10.1007/978-3-031-25588-5_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-25587-8
Online ISBN: 978-3-031-25588-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)