Abstract
This chapter presents critical components of the interaction between the professional and the person, needed to effectively support behaviour change. Most of these components are relational competencies assisted by communication skills. Relational competencies include person-centredness and shared decision-making, contributing to the person’s empowerment, a concept strongly linked with health literacy. Communication skills comprise the basic interchange and optimised linguistic features. Further, coping strategies to deal with negative emotions and psychosocial implications of chronic disease are summarised.
This chapter also proposes an integrated approach (ABCD) for first and follow-up encounters in behaviour change interventions. The ABCD approach comprises four stages: setting the stage (A), establishing an information base (B), obtaining a commitment (C) and negotiating an intervention plan (D).
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Patient empowerment
- Person-centredness
- Shared decision-making
- Health literacy
- Communication skills
- Verbal language
- Personalised education
- Coping skills
- ABCD approach
This chapter contributes to achieving the following learning outcomes:
-
BC6.1 Generate with the person opportunities for behaviour change.
-
BC6.2 Assess the extent to which the person wishes and can become co-manager of his/her chronic disease.
-
BC6.3 Demonstrate how to promote coping skills and self-efficacy to manage chronic disease’s physical, emotional and social impacts in everyday life.
-
BC6.4 Assist the person to become co-manager of his/her chronic disease in partnership with health professionals.
-
BC7.1 Apply strategies to support the cooperative working relationship between the person and a healthcare provider.
-
BC7.2 Demonstrate active listening of the person’s concerns and difficulties in the self-management of chronic disease.
-
BC14.1 Share information and adequate educational materials according to individual factors (e.g. knowledge gaps, health literacy level and preferences).
5.1 Overview of Key Concepts
Supporting successful behaviour change interventions requires relational and communication skills. It is well accepted that communication adopted by professionals can foster engagement in behaviour change or, if suboptimal, bears a detrimental effect.
Concepts such as patient-centred communication and shared decision-making are pivotal in behaviour change interventions; these two concepts remind health and other professionals that they must embrace the idea that change happens within each person, not through professionals’ willingness.
In this chapter, we will address the essential features of a relationship between the professional and the person when supporting the change or the maintenance of a self-management behaviour.
5.1.1 Patient Empowerment
A current conceptualisation of patient empowerment posits that it occurs when patients make autonomous, informed decisions about their health, supported by a professional, to increase their capacity to think critically and make independent and informed decisions (Anderson & Funnell, 2010).
One definition of patient empowerment considers that patients are empowered when they have the knowledge, skills, attitudes and self-awareness necessary to influence their and others’ behaviours to improve the quality of their lives (Funnell et al., 1991).
Another definition defines patient empowerment in the healthcare context as promoting autonomous self-regulation to maximise the individual’s potential for health and wellness (Lau, 2002). As one can realise, patient empowerment begins with information and education and includes seeking out information about one’s condition and actively participating in treatment decisions.
How does it start? Patient empowerment begins when professionals acknowledge that patients with chronic diseases are in control of their daily care. Professionals must recognise that the most significant impact on a person’s health and well-being results from their own management decisions and daily actions.
The professionals involved in patient empowerment make clear to patients that being in control of their daily self-management decisions comes with responsibility for those decisions and the resulting consequences. Responsibility, in turn, means that patients cannot surrender their control over chronic disease self-management, no matter how much they wish.
While professionals cannot control and therefore cannot be responsible for the self-care decisions, they are accountable for ensuring that their patients make informed self-management decisions. Here, “informed” means an adequate understanding of self-management and an awareness of the aspects of their personal lives that influence self-management decisions.
A conceptual framework proposed by the EMPATHiE project considers patient empowerment on three different levels: macro, meso and micro, as depicted in Fig. 5.1. All associated variables work as moderators of patient empowerment (Kayser et al., 2019).
-
Macro-level, i.e. the vision circulated by the authorities. This level comprises the definition of the joint plans at the organisational level, e.g. shorter hospital stays.
-
Meso-level, i.e. the medicine level and the perspective of patients living with multimorbidity on professionals and informal caregivers’ role. It comprises patient-centred care and autonomy support.
-
Micro-level, i.e. patients’ perspective stemming from their personal health experiences. This level comprises patient participation through shared decision-making to foster involvement.
The EMPATHiE conceptual framework. (Adapted from Kayser et al., (2019) and European Patients’ Forum (2017))
In this chapter, the focus will be on the meso- and micro-level patient empowerment. Empowering patients encompasses concepts such as patient-centredness, shared decision-making, motivational interviewing, counselling and signposting to support services. According to Holmström & Röing (2010), patient-centeredness as a process is of great value in patient empowerment. Patient empowerment can be achieved by patient-centeredness, but patients can also empower themselves. Nevertheless, one should not forget that patient empowerment is influenced by attributes of professionals, such as individual features, training, personal values and professional goals.
At the patient level, the ability to engage in empowerment activities is influenced by context, personal characteristics, values, social support and disease circumstances (e.g. duration, severity). Professionals also need to pay attention to patient’s health literacy and self-management skills.
How can a patient’s empowerment be assessed? The empowered patient has to feel like they have the ability and are given the confidence to manage their condition. Patients can indicate this state through their:
-
Capacities, beliefs or resources including self-efficacy, sense of meaning and coherence about their condition, health literacy, perceived control and feelings. Health and other professionals should respect all these.
-
Activities or behaviours (things patients do), such as participating in shared decision-making and self-management of their condition. When the patient can choose meaningful and realistic goals and takes steps to achieve those goals, such as participating in collective activities (e.g. patient support or advocacy groups), the professional is dealing with an empowered patient. Active search for information about their health condition (e.g. on the Internet) is also a sign of empowerment, even if misinformation is present, which is a distinct issue.
5.1.2 Person-Centredness
This section deals with another well-known concept in healthcare provision, known as patient-centredness.
The terms person-centred, people-centred and patient-centred will be used interchangeably. Looking at the Mead & Bower (2002) definition of patient-centred care, it is the understanding of the patient as a unique human being or entering that person’s world to see illness through their perspective.
Person-centredness supports the care of the whole person (negative and positive aspects), for the person (assisting the fulfilment of life projects), by the person (competent and high ethical conduct) and with the person (respectful collaboration).However, the concept can be seen as further complex. According to a systematic review from Scholl et al. (2014), patient-centredness encompasses 15 dimensions, organised in principles, enablers and activities (see Fig. 5.2):
-
Principles: essential characteristics of professionals, professional-patient relationship, patient as a unique person, the biopsychosocial perspective.
-
Enablers: integration of medical and non-medical care, teamwork and team building, access to care, coordination and continuity of care.
-
Activities: patient information, patient involvement in care, involvement of family and friends, patient empowerment, physical support, emotional support.
A model of person-centeredness. (Scholl et al., 2014)
One can realise from all previous dimensions that some are more dependable on the healthcare professional, e.g. professional-patient communication and relationship and patient involvement in care and empowerment, than others, e.g. access to care and medical and non-medical care integration.
Although robust evidence about the positive effects of person-centredness in health endpoints is still lacking, review studies have provided objective and positive accounts, such as the reduction of inappropriate prescription and use of benzodiazepines and related drugs (Mokhar et al., 2018), as well as improvements in the clinical outcomes of persons with type 2 diabetes in primary healthcare (Vuohijoki et al., 2020).
5.1.3 Shared Decision-Making
When making health-related decisions, some people prefer those decisions to be taken and controlled by healthcare professionals. Other persons are willing to participate in decision-making and enjoy a degree of autonomy when managing their conditions.
Assessing the level of direct responsibility in decision-making, and reflecting on a person’s empowerment, is an area of research and education named shared decision-making (SDM).
Shared decision-making in healthcare is especially relevant for the success of health behaviour change interventions. It requires applying strategies to create an environment conducive to open and effective communication, from active listening to building a trustful relationship.
Reasons for incorporating the person’s views and preferences in healthcare decisions are twofold. The first reason is an ethical imperative. This imperative emerges from the known ethical principles of autonomy, beneficence, non-maleficence and justice (Beauchamp & Childress, 2019). Attempting to involve persons in decision-making is expected to respect their independence, do good, prevent harm and be equitable. Ensuring these principles in practice and involving persons in decision-making can be challenging; for example, cultural or cognitive barriers make it harder for them to understand the information.
Another reason, from a practical nature, is that evidence shows that persons’ preferences for healthcare options differ. The typical examples are the preferences for cancer treatment (e.g. Hamelinck et al., 2014; Stalmeier et al., 2007); it has been shown that professionals are inaccurate in predicting persons’ preferences.
At least in principle, decisions in healthcare (including those respecting to behaviour change interventions) can be categorised as “effective” or “preference-sensitive”.
Effective decisions are those where there is agreement on the best management strategy. Preference-sensitive decisions are those for which there is little evidence on the best course of action or for which, despite the available evidence, weighing the benefits and harms of options may greatly vary from one person to the other.
In treatment decisions, SDM has been recommended when a decision is preference-sensitive. When it comes to behaviour change, while there is robust evidence for the effectiveness of behaviour change techniques (BCTs) in promoting sustained health behaviour changes, the majority of the existing research tests BCTs in groupings (i.e. bundles of BCTs that are hypothesised to be effective), which means that when selecting individual BCTs in practice, professionals sometimes need to make preference-sensitive decisions. There is, nonetheless, a growing body of research using optimisation designs to test individual BCTs and compare their efectiveness. SDM is, therefore, a means to ensure that people’s views are incorporated in the process, leading, hopefully, to decisions that fit their beliefs and preferences. The general effects of SDM mainly relate to outcomes on the cognitive level (e.g. showing command of the treatment options available and their implications) and affective level (e.g. showing acceptance or denial of a treatment option), especially when persons perceive to have been involved in decisions (Agbadjé et al., 2020).
The literature offers examples of SDM shared decision in behaviour change in chronic disease, such as approaches to initiate behaviour change in persons with cardiovascular disease (Cupples et al., 2018).
Some authors devoted attention to the intervention functions and behaviour change techniques (BCTs) needed to implement SDM in clinical practice, i.e. BCTs to achieve SDM, a different focus from employing BCTs as part of an intervention plan to achieve self-management behaviours. Intervention functions are “a broad category of means by which an intervention can change behaviour” (Michie et al., 2011). For instance, the intervention function “education”, alone or in combination with other intervention functions (e.g. education + persuasion, education + training + modelling + enablement), was associated with effective SDM implementation. Examples of BCTs associated with effective SDM implementation were instruction on how to perform the behaviour, demonstration of the behaviour, feedback on behaviour, pharmacological support, material reward and biofeedback (Agbadjé et al., 2020).
One of the most cited approaches for achieving SDM is the work from Elwyn et al., (2012), updated by the same authors in 2017 (Elwyn & Durand, 2017). SDM depends on activities that help confer agency, which refers to the capacity of individuals to act independently and make their own free choices.
SDM aims to confer agency by two activities:
-
1.
Providing high-quality information
Based on knowledge acquired previously and during the intervention, the person can assess what is important concerning the outcomes associated with different options, processes and paths that lead to these outcomes.
-
2.
Supporting deliberation
Support the person to deliberate about their options by exploring their reactions to the information provided. When offered a role in decisions, persons can be surprised, unsettled by the possibilities and uncertain about what might be best.
For instance, in the field of behaviour change in health promotion, interventions to increase levels of SDM take two forms (Gültzow et al., 2021):
-
Training healthcare professionals (and/or persons) in BCTs.
-
Decision aids to be used before, during or following consultations or more generic question prompt lists. Decision aids can potentially be beneficial in supporting people to change preventive health behaviours, especially regarding smoking.
5.1.4 Health Literacy and Education
The linkage between behaviour change and health literacy is well recognised. Self-management behaviours may be promoted when enhancing a person’s health knowledge through education, even if the relationship between education and behaviour change is not linear (Walters et al., 2020).
One note should be added regarding the difference between information and education. While information is predominantly one-way communication, from the professional to the person, education aims to confirm the person has acquired the knowledge and makes excellent and independent use of it.
Health literacy can be defined as the achievement of a level of knowledge, personal skills and confidence to take action to improve individual and community health by changing one’s lifestyle and living conditions. A useful resource for this and other definitions is the World Health Organization (WHO) Health Promotion Glossary, commissioned in 1986 and updated in 2021 (Nutbeam & Muscat, 2021).
Thus, health literacy means more than reading pamphlets and making appointments (i.e. functional literacy). It involves improving persons’ access to health information and the role of professionals in developing their capacity to use it effectively (i.e. interactive and critical literacy).
Professionals in brief or long interventions can contribute to improving a person’s health literacy through generic education and by using BCTs that increase knowledge, understanding or impart skills (training).
Several approaches can be used to provide tailored education about a condition its treatment or self-management behaviours; a simple approach is the “Elicit-Provide-Elicit” technique, described below. The person should do most of the talking; this allows an understanding of the person’s current knowledge and potential knowledge gaps and misconceptions. Personal views must be heard and listened to, even if the professional thinks they are incorrect (Bull & Dale, 2021).
First, the professional finds out what a person already knows about a condition, treatment or self-management behaviour, plus what she or he would like to know (“Elicit”), by posing questions such as “What do you know about X?”. Then, the professional asks for permission and provides information that is helpful for the person (“Provide”), in a non-judgemental way, e.g. “Others have benefited from”, “What we know about X is”. Next, the professional checks the person’s understanding, interpretation or response to what has been said (“Elicit”) e.g. - “What do you think about this information I gave you?” “What questions do you have?”.
A critical success factor in providing education or training is how the professional communicates. Fear tactics have no place in person-centred behaviour change communication. It is also important to remember that some people need time to adjust to new information, master new skills or make short- or long-term behaviour changes.
Simple rules to maximise effective education are:
-
Using preferably tangible support, either printed or digital, depending on the person’s preference, and factors such as literacy, numeracy and culture (e.g. brochures, podcasts, YouTube videos, videos, PowerPoint presentations, posters or charts or models).
-
Combining text with graphics and pictures, instead of long written instructions only.
-
Asking open-ended questions to assess the person’s understanding of printed or online materials.
-
Speaking at a moderate pace, especially when providing instructions.
-
Respecting the person’s limits, offering only the amount of information that an individual can handle at one time.
-
Using plain language, avoiding complicated medical terminology or jargon to minimise the risk of misunderstanding.
Box 5.1 Examples of Simpler Wording
-
“Swallow” instead of “take” the medicine.
-
“Harmful” instead of “adverse” effect.
-
“Fats” instead of “lipids” reduction in daily food.
-
“Belly” instead of “abdomen” perimeter as an indicator of cardiovascular risk.
-
“Lasting a short time, but often causing a serious problem” instead of “acute” conditions.
The type of educational resources that a person responds to varies from person to person. Using a mixed media approach often works best. Professionals must review these resources before sharing them with persons living with chronic diseases. When developing their own materials, professionals should seek some form of validation, e.g. by pretesting the materials in a controlled sample and evaluating knowledge and/or skills acquisition.
Table 5.1 presents educational materials to support behaviour change interventions from reliable sources. Other online resources include webpages such as the WHO, national centres for disease control (e.g. health directorates) and other national health organisations (e.g. medicines agencies).
There is a constantly growing number of digital resources, such as websites and mobile applications. Many have commercial purposes, variable information quality and trustworthiness. One tool to aid the choice of digital health apps is ORCHA (https://orchahealth.com/services/digital-health-libraries/). HON (https://www.hon.ch/en/) certifies quality health information on websites.
5.2 Providing Person-Centred Behaviour Change Support
Effective communication strategies are paramount for collaborative planning, understanding the person’s situation and successfully supporting behaviour change, either in single, opportunistic or repeated and more extended interactions.
As explained in Chap. 4, brief interventions are delivered in a short interaction between the provider and the person, often carried out when the opportunity arises, typically taking no more than a few minutes. Although shorter, a brief intervention can be delivered in several sessions. Brief interventions are often the only practical way of supporting behaviour change.
Long-term interventions are delivered in extended interactions (e.g. around 30 minutes) between the professional and the person, following a structured plan and multiple sessions over time.
Either brief or long, behaviour change interventions tend to be nested in existing encounters. Both interventions involve plans developed in cooperation with the person. One well-accepted approach to co-generating collaborative plans is using person-centred communication and mechanisms to involve the person in decisions; these two topics will be explored in the next sections.
5.2.1 Basic Communication Skills
Effective behaviour change interventions require two basic communication skills: good questioning and adequate listening.
Questions can be divided into four main types, detailed below.
-
1.
Open-ended questions, which are questions that cannot be answered with a simple yes, no or another preconceived response. Often, they start with “What”, “How” or “How come”. They facilitate communication by encouraging the person to describe or explain the health or behaviour issue in their own words. Examples of these questions include “Please, tell me more about your smoking behaviour” and “What are the triggers that make you crave for a cigarette?”.
Open-ended questions are frequently used early in the interaction process, to expand the dialogue and encourage the person to tell his or her story.
An interaction with a predominance of open-ended questions will be lengthier, and there is a possibility of handling less relevant information.
-
2.
Focused or closed-ended questions, which are questions that direct the person to a specific answer. These questions can frequently be answered by yes, no or through a simple, definitive reply, as exemplified by “Do you always smoke after meals?”
Focused questions are frequently used to fine-tune the understanding of a problem and clarify details that the person may not have addressed in response to an open-ended question.
If the preceding questions have been open, closed questions may result in a more detailed answer than just plain and straightforward facts, as shown in Box 5.2.
Box 5.2 Example of Detailed Information Collected with a Focused Closed Question Proceeded by Open Questions
-
Professional: “Do you always smoke after meals?”
-
Person: “Yes, it gives more ‘me’ time”.
An interaction with mostly closed-ended questions will limit the person’s participation and increase the risk of collecting a different story from what the person truly experiences.
-
3.
Circular questions are a more sophisticated information-gathering technique that asks the person to provide information from a different or someone else’s perspective (e.g. “How might this problem change in the near future?”). These questions are often very effective for gaining an understanding of the subtle nuances of a problem.
-
4.
Leading or directive questions suggest a correct answer, as evident in the case of “You know that smoking is bad for your health, right?”. These questions introduce undue bias in a person’s accounts and should be avoided.
Listening skills are crucial to demonstrate that the person has been heard and understood. Listening involves responses to the content, feelings or both. There are four general types of responses to the content presented next.
-
1.
Nodding means providing non-verbal feedback by using paralanguage and head movements to encourage the person to talk, as illustrated in Box 5.3.
Box 5.3 Example of Nodding
-
Person: I have had issues with quitting smoking… for several years. I have tried… the last time was…
-
Professional (looks into the person, nods his head): hum-hum… (i.e., I am listening).
-
2.
Parroting consists of repeating the last few words that the person said, and it is the most straightforward responding skill. This response demonstrates that the professional is listening and frequently encourages the person to continue and/or elaborate, as exemplified in Box 5.4.
Box 5.4 Example of Parroting
-
Person: This last month, I felt that I had to make another attempt to quit smoking…
-
Professional: Quit smoking…
-
3.
Paraphrasing is slightly more sophisticated than parroting. It offers key points for a small amount of content and helps check the accuracy of what the professional has heard (Box 5.5). This response reveals higher attention levels. It provides the possibility to correct any misconceptions and demonstrates attention.
Box 5.5 Example of Paraphrasing
-
Person: Well, I started smoking 15 years ago. I tried several times to quit smoking and even managed to be two months without smoking. I have heard about consultations out there, but I want none of that. It is about my will...to stop smoking.
-
Professional: So, I understand you want to quit smoking. What makes you crave a cigarette?
-
4.
Summaries are another form of responding to content. They are usually lengthier and deal with a more significant amount of information than paraphrasing or parroting (Box 5.6). Summaries are used throughout an interaction to make sure the narrative is heard wholly and correctly. Its main objective is to explore the content of the dialogue or bring it to a conclusion.
Box 5.6 Example of a Summary
-
Person: I get up from my desk to take a break, and I suddenly feel that I really want to light up. I feel a strong urge to smoke in all my breaks at work. It really helps me to unwind.
-
Professional: You are telling me that smoking when you have a break at work helps you relax, so that is a trigger for smoking in your case...
Paraphrasing and summaries are examples of active listening. The listener highlights the main ideas expressed by the person, with summarising allowing for further content development in the next communication cycle, by reviewing in more detail a previous one.
Active listening skills also comprise reflective responses, in which the listener identifies feelings and emotions. Responses to feelings can take different forms and are particularly useful for demonstrating proper understanding and empathy.
There are three types of reflective responses:
-
1.
Sympathetic responses communicate how the professional feels about what has been said or happened, centred on the professional’s own framework (Box 5.7). It does not consistently demonstrate an emotional synchronisation with the person’s feelings.
Box 5.7 Example of a Sympathetic Response
-
Person: Well, I started smoking 15 years ago. I tried several times to quit smoking and even managed to go two months without smoking. I know consultations are a good option, but I would like to try on my own. It is about my willpower... to stop smoking.
-
Professional: Professionals can offer help to quit smoking.
-
2.
Empathetic responses demonstrate that the professional understands and accepts the feelings that the person has experienced, centred on the person’s agenda (Box 5.8). To be effective, it must be perceived as genuine and sincere. This emotional resonance is essential to build acceptance of behaviour change support.
Box 5.8 Example of an Empathetic Response
-
Person: Well, I started smoking 15 years ago. I tried several times to quit smoking and even managed to go two months without smoking. I have heard about consultations out there, but I want none of that. It is about my will...to stop smoking.
-
Professional: It is hard to quit smoking after several years, and trying certainly requires motivation. Would you like to talk about smoking cessation?
-
3.
Denial responses contradict what the person expresses and undermine the interview process (Box 5.9). Like leading questions, denial responses should be avoided.
Box 5.9 Example of a Denial Response
-
Person: Well, I started smoking 15 years ago. I tried several times to quit smoking and even managed to go two months without smoking. I have heard about consultations out there, but I want none of that. It is about my willpower...to stop smoking.
-
Professional: You should really seek professional support to get a better chance to quit smoking.
The following two dialogues illustrate the previous concepts based on the communication design proposed by Rollnick et al. (2005):
Dialogue 1
Professional : Your test result shows that glucose levels in your blood are raised today. This means that you really need to watch your diet. Have you thought about adjusting this?
Person : Well, it is not that easy. I have tried, but you know what it’s like. I mean, it’s not that easy with my job, driving around in a rush, and you know, you just have to grab some food at lunch and keep going.
Professional : Could you bring your own lunch with you…?
Person : I could do that, but it’s so busy in the morning, just getting us all out of the house, and then I stop in a cafe anyway at lunch, so I would then have to avoid the easy option of just getting a roll and feeling full and ready for action.
Professional : Well, you are treating this as your top priority, right?
In Dialogue 1, the professional uses an informing mode drawing on a rigid interaction routine, making assumptions about the diet, uses a predominance of closed questions and resorts to leading or directive questions. This may elicit resistance to change and guilt and is unlikely to generate opportunities for changing behaviour.
Dialogue 2
Professional : Your test result shows that glucose levels in your blood are raised today. I wonder what sense you make of this?
Person : I don’t know. It’s hard to live 24/7 with diabetes, I’m so busy, and it’s another thing to worry, the blood sugar levels.
Professional : I completely understand. Everyday life can’t stop because you have diabetes [empathic response].
Person : Yes, exactly, but I know I need to be careful.
Professional : In what way?
Person : I need to watch my diet and get more exercise. I know that, but it’s not that easy.
Professional : What might be manageable for you right now?
Person : It’s got to be exercise, but please don’t expect great things from me.
Professional : Well, a change in diet or exercise may be of help. How might you succeed with exercising more?
Dialogue 2 corresponds to a guiding communication style or a patient-centred dialogue. Asking open questions elicits the person’s perspective on self-management behaviours. Listening is used to convey an understanding of the person’s experience and to encourage further exploration. Informing is combined with asking, to encourage choice and promote autonomy. This option is more likely to generate opportunities for changing behaviour.
Other crucial interpersonal communication skills involve using positive non-verbal and body language (e.g. visual contact, framing shoulders with the other, leaning the torso slightly forward), optimising verbal language (as described in the next section) and managing the exchange to provide opportunities for the person to speak.
5.2.2 Optimising Verbal Language
Person-centred care has implications for the language used by professionals when communicating with persons with chronic diseases. For example, the biomedical lexicon can hinder comprehension for some persons. As explained in the section on “health literacy”, using plain language minimises the risk of misunderstanding. Beyond this aspect, recommendations on the use of language to communicate with persons with diabetes and obesity have been issued (Banasiak et al., 2020; Cooper et al., 2018; Dickinson et al., 2017; Speight et al., 2012; Speight et al., 2021), to encourage terms promoting positive interactions and, subsequently, positive outcomes.
Table 5.2 provides examples of preferred terms for behaviour change support interactions in chronic disease based on this work. In their scoping review, Lloyd et al. (2018) elegantly articulated arguments in favour and against the use of “person-first language” (“person with diabetes”) instead of a disease-first language (“diabetic”). While some persons may find it acceptable to refer to themselves as “diabetics”, others find it offensive or harmful; professionals have the responsibility to use language that respects everyone’s preferences. As Speight et al. (2021) pointed out, people are rarely offended by being referred to as a “person”.
5.2.3 Coping Skills to Manage Chronic Disease
When dealing with a chronic disease, it is common to experience negative emotions related to the disease onset, progress and treatments, as well as psychosocial implications, e.g. social isolation and difficulties in engaging in daily activities. This is illustrated by the concept of diabetes distress, introduced in 1995 to designate “the negative emotional or affective experience resulting from the challenge of living with the demands of diabetes” (Skinner et al., 2020). There is compelling evidence that diabetes distress is common, affecting roughly one in three persons living with type 2 diabetes, and is a barrier to emotional well-being, self-care and diabetes management. Consequently, monitoring diabetes distress is advocated by many clinical guidelines (Skinner et al., 2020).
It is also common for persons with chronic disease to experience various lapses when trying to maintain self-management behaviours, such as physical activity, a healthy diet or following prescribed treatment. To deal with these stressful situations, people can implement various coping strategies.
The American Psychological Association defines coping as “the use of cognitive and behavioural strategies to manage the demands of a situation when these are appraised as taxing or exceeding one’s resources or to reduce the negative emotions and conflict caused by stress” (from https://dictionary.apa.org/coping).
The individual can adopt various coping strategies to self-manage chronic disease resulting from the cognitive and emotional representations associated with the stressors. These coping strategies can be positive (i.e. adaptive), e.g. taking time to exercise in the middle of a hectic day, or negative (i.e. maladaptive, avoidant), e.g. not asking for support when decisions on medication-taking are not being met, binge drinking or overeating.
One of the main distinctions of coping strategies is between problem-focused coping and emotion-focused coping (Lazarus & Folkman, 1984). As the name suggests, problem-focused coping aims to remove or reduce the cause of stress by the person through, e.g. problem-solving techniques (such as coping or barrier planning, a common behaviour change technique previously described), better time management or support from others. Emotion-focused coping includes those strategies used to regulate the person’s negative emotions, such as fear, anxiety, sadness or frustration; examples are distraction, mindfulness and relaxation. Please note that distraction is a coping strategy that fits various categorisations of coping strategies. Figure 5.3 presents more examples of problem-focused and emotion-focused coping strategies.
Another common distinction is between approach and avoidance coping. Approach coping is any behaviour, cognitive or emotional activity that directly deals with the stressor or threat, such as problem-solving using if-then plans (“If I feel too tired, I will do a shorter exercise session and with a less intensive pace”). Avoidance coping refers to any behaviour, cognitive or emotional activity taken to avoid the threat. It can be maladaptive, such as denial of diagnosis or progress of a disease or withdrawal from a beneficial treatment; in other instances, it can be helpful, for example, distraction (doing something else to avoid thinking about the problem in a given situation can help in reducing high levels of distress).
When managing chronic disease, individuals should be flexible and use different types of coping skills according to the characteristics of the situation, such as the level of control the individual has over the situation or if it leads to powerful emotional reactions.
Professionals can support persons in understanding the type of coping skills they tend to use for different stressful situations and deal with negative emotions, if these are adaptive and maladaptive, and facilitate the acquisition and enactment of coping skills described in Fig. 5.3. Each person may need to experiment with various coping strategies to discover which ones work best as ongoing events and life circumstances change, and come up with his or her own toolkit of strategies.
When exploring and training individuals in coping skills, professionals must use the communication skills addressed in this chapter, namely, non-judgemental and empathic communication.
5.2.4 Structuring the Interaction: The ABCD Approach
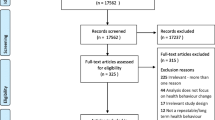
Smith et al. (2000) have proposed evidence-based guidelines for patient-centred communication. Their approach has been adapted in this book for providing behaviour change support. In the interest of simplicity, our adaptation has been coined ABCD, as it encompasses four sequential stages, detailed in Fig. 5.4, which in turn contain several steps.
These sequential stages apply to each behaviour change interaction, either in brief or long-term interventions, although not all steps subsumed in the different stages are necessarily applicable. Brief interventions are usually opportunistic and shorter, and therefore within each stage, some steps may be omitted, as explained in the following sections.
Long-term interventions involve follow-up, which may also be part of brief interventions. Interactions after the first encounter resort to the same sequential stages, as depicted by the circular nature of this approach (Fig. 5.4).
The ABCD approach is meant to aid professionals in flexibly structuring their behaviour change interactions, considering both the context and the person, and is not intended to be used prescriptively. Table 5.3 outlines the purpose of each stage.
5.2.4.1 First Encounter
-
A.
Setting the stage
Setting the stage is probably the most challenging component of effective behaviour change interventions. Fisher et al. (2017) highlighted that professionals should be prepared for a different interactive mindset and to make an effort to slow the conversation pace. Additionally, professionals need to re-orient themselves to motivational needs and obstacles, i.e. moving from an information delivery focus to listening and reflecting on conversation. It is not about extra time but addressing the nuances of the person’s engagement by supporting and encouraging their motivation to change (Fisher et al., 2017).
Setting the stage in the present model comprises seven steps, detailed in Table 5.4. It may be unfeasible to implement these seven steps in brief interventions due to their shorter and opportunistic nature, and therefore, two steps (welcoming the person and agreeing on the agenda) are suggested as a priority.
When welcoming the person, the professional should ask how the person wishes to be addressed, by first or last name, sometimes including titles. It is generally a good practice to use the surname to start with, although this may vary between countries and cultures.
Steps 2 to 6 intend to develop rapport, commonly defined as the level of connection between persons communicating bidirectionally (Box 5.10). Furthermore, a relationship based on mutual trust is expected when rapport is established. Developing rapport with the person is essential since it builds meaningful conversations and promotes the willingness to embrace different points of view.
Box 5.10 Example of a Dialogue Initiation and Rapport Building
-
Professional: Good morning. You must be Paul.
-
Person: That’s right.
-
Professional: Come on in, and make yourself comfortable, Paul. Is it all right to call you Paul?
-
Person: I would prefer Mr. Jonhson.
-
Professional: Sure. Let me close the door, Mr. Johnson, so we can have a quiet talk. My name is Jeff, and I provide counselling on health-related behaviours. Your wife mentioned that you were thinking of quitting smoking.
-
Person: Well, my wife suggested this appointment…
-
Professional: I’m glad you had the time to visit us today, Mr. Johnson. Your wife expressed concern about your increasing breathing difficulties.
-
Person: She cares about me a lot.
-
Professional: That’s nice to know. During your time with us today, I would like you to feel at ease. If, for any reason, you want to end the conversation, that’s perfectly fine. We can resume it on another occasion if you prefer.
-
Person: I understand.
-
Professional: So, our conversation will be about ways to help you give up smoking. In general, this does not take more than 20 minutes. Would that be OK for you?
-
Person: Perfectly fine. Thank you for your time.
The last point, agreeing on the agenda, in this case comprising health behaviour change, should happen when both the professional and the person are bonded in the conversation, even for other reasons. In brief interventions, it may be feasible to use a warm welcome or quick social talk to facilitate this bond. In essence, agreeing on the agenda means deciding whether the person is receptive to discussing behaviour change. Directive conversation to persuade the person to change behaviour based on the professional’s agenda, disregarding the person’s priorities, preferences, beliefs and resources, is not congruent with a person-centred approach.
Four techniques described in the literature to initiate a health behaviour change talk (Albury et al., 2020) are helpful to agree on the agenda and decide whether the interaction can proceed to the next stage (B. Establish an information base). The first three techniques described below should be preferred.
-
Person-initiated discussion is a technique where the person initiates the talk by asking directly for advice or raising a concern (Box 5.11). The professional should capitalise on this situation, as it facilitates receptiveness.
Box 5.11 Example of Person-Initiated Discussion
-
Person: You know, smoking is a health issue for me. I have started to have shortness of breath when I exercise.
-
Professional: OK. Have you considered quitting smoking?
-
Direct questioning by professionals (e.g. do you smoke?) may lead to acknowledging the risk behaviour and eliciting helpful information, such as disclosing attempts to change behaviours or providing explanations for not doing so. Professionals can resort to the information elicited to inform the subsequent discussion.
-
Non-personalised initiation is another technique that is less likely to generate resistance. As described in Box 5.12, this approach consists of establishing a generic statement on the behavioural problem, securing agreement on this statement from the person and then moving to a more personalised discussion.
Box 5.12 Example of Non-personalised Initiation
-
Professional: Smoking is a public as well as an individual health concern. Implications of smoking are well established, such as damage to the lungs and the heart.
-
Person: You know, smoking is a health issue for me. I have started to have shortness of breath when I exercise.
-
Professional: OK. Have you considered quitting smoking?
-
As illustrated in Box 5.13, linking health behaviours to a medically relevant concern is expected to facilitate the interaction by emphasising its salience for the person. However, this technique has varying effectiveness; it has been shown to elicit resistance even when the link between the health concern and health behaviour had relevance to the person. Resistance has been defined as a response that halts the conversation progressivity, ranging from no response, a minimal response, or not displaying alignment with behaviour change (Albury et al., 2020).
Box 5.13 Example of Linking Health Behaviour to a Medically Relevant Concern
-
Person: You know, I cannot get pregnant right now. So, I have to take my contraceptive pills.
-
Professional: Do you still smoke?
-
Person: Yeah.
-
Professional: Following regular hormonal contraception is generally accepted as an effective and safe option. At the same time, smoking and taking birth control pills brings additional health risks.
Caution should be exercised when associating a person’s disease with health behaviours, as several other determinants play a role in the health state. These determinants include healthcare, genetic vulnerability, socio-economic characteristics and environmental and physical influences, mainly beyond the person’s control (Naughton, 2018). Linking a person’s disease with individual health behaviours implies being blamed for the disease, which can lead to resistance to change and should therefore be avoided.
Initiating a change in topic is recommended to manage resistance during behaviour change talks (Albury et al., 2020); it can be equally helpful to deal with displays of resistance when “Setting the stage”, as exemplified in Box 5.14.
Box 5.14 Example of Change in the Topic When Setting the Stage
-
Professional: Do you still smoke?
-
Person: Yeah.
-
Professional: There are some strategies that really help with quitting…
-
Person: [5 sec silence]
-
Professional: Well... so... how’re you getting along with your pedometer? Seems okay?
-
Person: No problem… I’m enjoying tracking of my progress
-
Professional: Tracking your progress... good.
After confirming the receptiveness to discuss behaviour change, the professional can suggest continuing the conversation to collect more information, which should be timewise, i.e. based on the professional and the person’s availability, as illustrated in Box 5.15.
Box 5.15 Example of a Dialogue on Time Limits When Setting the Stage
-
Professional: So, I see that you have been thinking about quitting smoking. Should we discuss this?
-
Person: Well, I only have about 5 minutes, actually…
-
Professional: That’s fine, I am also pressured today. What about starting to discuss, and you can return on another day?
-
Person: Sounds good!
-
B.
Establish an information base
Establishing the information base comprises two steps, detailed in Table 5.5. Although the depth of information collected may vary, these two steps apply to long-term and brief interventions. For instance, discussing factors that influence a behaviour is required in a brief intervention to inform the plan, but it will be less comprehensive than in a long-term intervention due to time constraints.
Put simply, identifying self-management needs answers the question “what target behaviour(s) need to be changed?” and leads to prioritisation if more than one risk behaviour emerges. As explained in Sect. 3.2, assessing the person’s behaviour relies, often, on an interview. The communication should begin with open-ended questions, using non-focusing open-ended skills: silence, neutral utterances and non-verbal encouragement. These can be followed by focusing on open-ended inquiry, if needed, to get the person talking (e.g. parroting and summarising). Further, closed-ended questions can be used for clarification and additional information can be obtained from sources such as non-verbal cues, physical characteristics, autonomic changes and the environment.
Box 5.16 Example of Dialogue to Establish an Information Base
-
Professional: I see that you have asthma. What other issues would you like to discuss, in addition to smoking?
-
Person: Well… I don’t use my inhalers exactly as prescribed, but I’m doing fine, so I don’t regard that as an issue.
-
Professional: Hum, hum.
-
Person: Really, smoking is a health issue for me. I started to have shortness of breath when I exercise.
-
Professional: Right. Do you regard quitting smoking as a priority?
-
Person: Not sure if it is a priority, I’m not doing much.
-
Professional: I’m sure you did what you could. How many cigarettes do you smoke per day?
One note on non-verbal information. While body presentation and language are well recognised and possible to interpret correctly based on the social and cultural background, autonomic changes such as cold sweating and abdominal discomfort are not easily detected.
The second step, eliciting behaviour determinants, should follow the same communicational approach when an interview is used: starting with open-ended questions on what stops the person from adopting the target behaviour and what facilitates its adoption. It may be helpful to focus questions on barriers and facilitators in adopting a target behaviour (e.g. quitting smoking, being physically active) instead of exploring factors influencing the person’s current behaviour (e.g. what makes the person smoke, what makes the person sedentary). For assessing behaviour determinants using measures refer to Sect. 4.1.2.
The focus on the person’s relevant factors improves rapport and trust. Closed questioning is also used to confirm the information elicited. Eliciting behaviour determinants in long and brief interventions through interviews is exemplified below; in the former, there is time for more exploration through listening skills, such as parroting and summaries. To save time, paraphrasing may be preferable in brief interventions instead of parroting, which encourages the person to continue talking.
Box 5.17 Example of Eliciting Behaviour Determinants in a Brief Intervention
-
Professional: Can you think of issues that prevent you from stopping smoking?
-
Person: Well… stress, really.
-
Professional: So, I understand that stress gets in the way of your will to stop smoking.
Box 5.18 Example of Eliciting Behaviour Determinants in a Long-term Intervention
-
Professional: Can you think of issues that prevent you from stopping smoking?
-
Person: Well… stress, really.
-
Professional: Stress….
-
Person: I deal with a lot of pressure at work, and it’s a way of unwinding. And it piles up, I get home, the kids and all that, you want to be in your best for them, so after dinner it also helps me to unwind.
-
Professional: Right. Are there other factors that get in the way of your will to stop smoking?
-
Person: Now that you mention that… I never had support. I have heard about consultations out there, but I don’t know how to access them.
-
Professional: Correct me if I’m wrong… the main reasons for not stopping smoking are stress and not knowing how to access smoking cessation consultations.
Assessing the person’s readiness to change involves ascertaining the degree of motivation which influences the behaviour, as illustrated by the COM-B model. Establishing motivation is important in the first and follow-up interactions, mainly if behaviour change is not being unattained.
The motivation ruler is a 1–10 scaling exercise to help the person think about the target behaviour and articulate reasons for changing. As the person verbalises these reasons, they may become more natural. To maintain a cooperative relationship with the person, questions such as “Why is it not higher?” or “Why x?” should be avoided. This exchange may be regarded as confrontational and raise resistance. It is vital to promote an empathic climate through positive communication. In the end, the professional should help the person summarise the reasons underlying the performance of a behaviour. An examples is presented in Box 5.19 regarding smoking cessation, focusing on communication aspects. Footnote 1
Box 5.19 Example of a Dialogue Using the Motivation Ruler
-
Professional: On a scale of 1–10, how important for you is stopping smoking in the next three months?
-
Person: 5.
-
Professional: OK. What was important to you when you decided on that score?
-
Person: You know, smoking is a health issue for me. I started to have shortness of breath when I exercise.
-
Professional: I see. Have you considered other issues regarding smoking?
-
C.
Obtain a commitment
Obtaining a commitment comprises two steps, detailed in Table 5.6. Implementing these two steps in brief interventions may not be feasible due to their shorter and opportunistic nature. Step 1 – discussing expectations – is not vital to define the intervention plan but may be helpful to smooth implementation. Box 5.20 illustrates a dialogue to reaffirm commitment in a brief intervention.
Ascertaining the expectations for success entails understanding the person’s views on the process (e.g. what it is about and how to achieve it), as exemplified in Box 5.21, and providing a different perspective if expectations appear unrealistic. Before reaffirming commitment, the professional may need to address emotion(s) empathically. Filling the person’s information gaps may also be required to reaffirm commitment to decisions and actions in behaviour change. In long interventions, the professional has room to provide more detailed explanations on the process of behaviour change, if pertinent.
Box 5.20 Example of Obtain a Commitment in a Brief Intervention
-
Professional: Now that you told me about what prevents you from quitting smoking… we can discuss your options and adapt them to your needs and preferences. How does this sound?
-
Person: That’s very much appreciated.
Box 5.21 Example of Obtain a Commitment in a Long-term Intervention
-
Professional: Let’s discuss your expectations about quitting smoking. What do you think is ahead of you?
-
Person: Well, I tried several times to quit smoking and even managed to go two months without any cigarettes. Then I went back again. I don’t think it’s easy...
-
Professional: As you said, many people find it challenging. We are here to offer support throughout the process! We can discuss your options and adapt them to your needs and preferences. How does this sound?
-
Person: That’s very much appreciated.
-
D.
Negotiate an intervention plan
The steps subsumed in the “Negotiating an intervention plan” stage are detailed in Table 5.7. Due to their opportunistic nature, it may be unfeasible to implement follow-up in brief interventions.
The professional should keep in mind the communication skills and strategies already described (e.g. questioning, active listening, change in topic to manage resistance). Linking health behaviours to a salient concern may be helpful at at this stage to address resistance. Asking for feedback is a relevant way to check the person’s rapport and pay attention to non-verbal communication signs.
Negotiating a specific plan can draw on shared decision-making models’ strategies, such as the three-talk model (Elwyn & Durand 2017), which includes “team talk”, “option talk” and “decision talk”.
“Team talk” refers to making sure the person knows that reasonable options are available, to provide support when making the person aware of choices and to elicit the person’s goals to guide decision-making processes.
“Option talk” refers to providing more detailed information about options and comparing alternatives using risk communication principles. While this has been established for comparing alternatives in drug therapy, it is less settled on what concerns different possible strategies to change behaviour.
“Decision talk” refers to arriving at decisions that reflect the informed preferences of persons, guided by the experience and expertise of health professionals.
Box 5.22 offers an example of applying the three-talk model to behaviour change in medication-taking; this example illustrates honesty about what is known and explores the person’s understanding, reactions and opinions about the information.
Box 5.22 Example of a Three-Talk Dialogue in Medication-Taking
-
Person: As I said, it’s not that I don’t want to take my blood pressure pill; it’s just that I have too much going on some days….
-
Professional: So, let’s work as a team to make a decision that suits you best. One option that appears suitable is setting up an alarm when you choose to take your blood pressure pill, for example, using your mobile phone. You said you take the pill in the morning?
-
Person: Yeah, that’s right.
-
Professional: OK. Other options are having your pillbox on the table where you have breakfast to see them or bringing a blister pack around with you in your purse/wallet. Are there any children in your house?
-
Person (laughs): Not really. They got off to university.
-
Professional: Oh, that’s lovely. Having medicines within reach of children would not be a good idea. So, what do you think of these three options?
-
Person: They sound good, but whether they work for me is a different story. I already have my pillbox on the kitchen counter.
-
Professional: So, you’re telling me that you forget to take your blood pressure pill in the morning, but having the medicine at sight doesn’t work. We don’t really know whether what works best in terms of comparing these options. It depends on each person’s preference and resources.
-
Person: Right….
-
Professional: If you are the type of person who uses a mobile phone, you might want to set up an alarm.
-
Person: Well… I tend to stop alarms and then still forget.
-
Professional: If the alarm doesn’t work for you currently, then maybe add a post-it to the fridge door?
-
Person: I think I could give it a try; after a couple of days, I might not notice the post-it anymore….
-
Professional: OK, let’s go with your choice, then! When would you like to start sticking the post-it on the fridge’s door?
-
Person: I’ll give it a try this week.
-
Professional: Great! You will tell me whether it works in our next encounter.
Active listening is a central component of deliberation, i.e. the process where the person becomes aware of the choice, considers the pros and cons of the options and assesses their practical and emotional implications.
Deliberation begins as soon as awareness about options develops. The process is iterative, as options have been described and understood. Deliberation encompasses the need to work collaboratively with professionals and may involve the person’s broader networks.
The person may need time and support to reflect on preferences and practicalities. Therefore, several encounters with the professional may be required, not necessarily face to face, and may include decision aids and discussions with others.
In addition to the three-talk model, which applies to any preference-sensitive decision in healthcare, the literature offers specific recommendations to guide communication during health behaviour change interventions (Albury et al., 2020). Collaborative talk, exemplified in Box 5.22, is associated with uptake displays. It requires inviting and accommodating the person’s perspective and presenting decisions as their choice. This strategy may facilitate engagement when a display of resistance emerges, and the professional chooses to continue the conversation. As already explained, initiating a change in the topic is a technique that also helps managing displays of resistance at this stage, as evidenced in Box 5.23.
Box 5.23 Example of a Change in the Topic When Negotiating an Intervention Plan
-
Person: As I said, it’s not that I don’t want to take my blood pressure pill; it’s just that I have too much going on some days….
-
Professional: Bringing a blister pack around with you in your purse may help.
-
Person: Everybody keeps telling me that but it doesn’t work for me.
-
Professional: OK. So, let’s work as a team to make a decision that suits you best. One option that appears suitable is setting up an alarm when you choose to take your blood pressure pill, for example, using your mobile phone. You said you take the pill in the morning?
-
Person: Yeah, that’s right.
Deciding collaboratively on the intervention includes agreeing on BCTs, to be implemented during encounters or techniques that the person can self-enact. Finalise this step includes confirming the person’s understanding and reaffirming the plan Box 5.23.
The encounter closure should include setting dates/times for a follow-up visit, usually in the case of long interventions. Brief interventions do not necessarily encompass follow-up due to their opportunistic nature. Avoiding repetition of agreed actions contributes to expediting closing.
5.2.4.2 Follow-Up Encounters
Interactions after the first encounter resort to the same ABCD stages; Table 5.8 details the purpose of each stage in follow-up encounters.
It is essential to monitor the intervention plan in these encounters, i.e. gather information to assess progress and adjust the plan accordingly.
The encounter should start by setting the stage. In follow-up encounters, agreeing on the agenda means deciding whether the person is receptive to discuss the intervention plan. Displays of resistance can be managed by initiating a change in the topic or offering the opportunity of a subsequent encounter.
In stage B, the professional should gather information regarding the agreed plan, using the communication strategies already discussed (e.g. open to close questioning, active listening). Discussing the intervention plan’s implementation involves ascertaining how it is working regarding the application of behaviour change techniques and the outcomes achieved. If the plan is not working, either because the person is struggling with self-enactable BCTs or expected outcomes are not achieved, it is helpful to review BCTs application and behaviour determinants, as uncovered or additional barriers may emerge. An empathic and legitimising conversation, as described in Box 5.24, focusing on achievements, current or future, is more empowering than emphasising failures.
Box 5.24 Example of an Empathetic Dialogue When Establishing an Information Base (Follow-up Encounter)
-
Person: Well, I was unable to cut down the number of daily cigarettes. The last two weeks were very stressful for me.
-
Professional: Good that you are still motivated to quit smoking. I completely understandable that it is hard to reduce the number of cigarettes under stress. Would you like to talk more about this?
If the plan is working, the professional should positively reinforce the person’s efforts when reviewing their actions to change behaviour. If only small successes were achieved, the talk should also focus on reviewing BCTs application and behaviour determinants without blaming the person.
Box 5.25 Example of a Non-blaming Dialogue When Establishing an Information Base (Follow-up Encounter)
-
Person: Well, I’m smoking just once a day when I’m feeling very stressed.
-
Professional: Excellent! Many congrats on achieving this outcome. Should we discuss strategies to reduce stress or alternative ways of avoiding that one cigarette?
Maintenance should be discussed when a target behaviour is achieved, self-management needs identified again and the process restarted for another target behaviour, if pertinent. Guidance to address multi-behaviour change interventions is still in a nascent phase.
Stage C, “Obtain a commitment”, involves discussing the person’s expectations and reaffirming the intention of engaging in behaviour change.
In Stage D the plan should be reaffirmed or reviewed collaboratively through the three-talk model or techniques such as inviting and accommodating the person’s perspective and presenting decisions as the person’s choice, already described. Reviewing the plan should consider information gathered in stage B and his or her engagement in behaviour change.
Key Points
-
At a meso- and micro-level patient empowerment encompasses approaches such as patient-centredness and shared-decision making, which contribute to increase the capacity of persons living with chronic disease to think critically and make independent and informed decisions.
-
Key aspects of person-centredness care are considering individual preferences, needs and values, being respectful of and responsive to those preferences, needs and values, and thus fully engaging the person in the intervention.
-
Shared decision-making is a collaborative process in which a (healthcare) professional works together with a person to make health-related decisions based on evidence and individual choices.
-
Education aims to increase knowledge and ensure that the person makes excellent and independent use of that knowledge. The “Elicit-Provide-Elicit” technique promotes personalised education.
-
Health literacy involves not only comprehending health information, but also the ability to access it and use it effectively.
-
To effectively support behaviour change professionals need relational and communication skills, including the use of open-ended questions, active listening and empathetic responding. Talking to persons with chronic disease should preferably make use of language that is non-judgmental, blame-free and that empowers.
-
Professionals can assist persons with chronic disease to develop Coping skills (e.g. problem-focused coping and emotion-focused coping) to deal with negative emotions and psychosocial implications associated with their conditions.
-
The ABCD approach is a framework to structure behaviour change interactions, it facilitates engagement through person-centred communication and shared-decision making.
Notes
- 1.
Additional details can be found in textbooks, such as the following reference: Miller, W.R., & Rollnick, S., (2012). Motivational Interviewing: Helping People Change (Applications of Motivational Interviewing). London: Guildford Press.
References
Agbadjé, T. T., Elidor, H., Perin, M. S., Adekpedjou, R., & Légaré, F. (2020). Towards a taxonomy of behavior change techniques for promoting shared decision making. Implement. Sci., 15(1), 67. https://doi.org/10.1186/s13012-020-01015-w
Albury, C., Strain, W. D., Le Brocq, S., Logue, J., Lloyd, C., & Tahrani, A. (2020). The importance of language in engagement between healthcare professionals and people living with obesity: a joint consensus statement. Lancet Diabetes Endocrinol., 8(5), 447–455. https://doi.org/10.1016/S2213-8587(20)30102-9
Anderson, R. M., & Funnell, M. M. (2010). Patient empowerment: myths and misconceptions. Patient Educ. Couns., 79(3), 277–282. https://doi.org/10.1016/j.pec.2009.07.025
Banasiak, K., Cleary, D., Bajurny, V., Barbieri, P., Nagpal, S., Sorensen, M., et al. (2020). Language matters–a diabetes Canada consensus statement. Can. J. Diabetes, 44(5), 370–373. https://doi.org/10.1016/j.jcjd.2020.05.008
Beauchamp, T., & Childress, J. (2019). Principles of biomedical ethics: marking its fortieth anniversary. Am. J. Bioeth., 19(11), 9–12. https://doi.org/10.1080/15265161.2019.1665402
Bull, E. R., & Dale, H. (2021). Improving community health and social care practitioners’ confidence, perceived competence and intention to use behaviour change techniques in health behaviour change conversations. Health Soc Care Community, 29(1), 270–283. https://doi.org/10.1111/hsc.13090
Cooper, A., Kanumilli, N., Hill, J., Holt, R. I. G., Howarth, D., Lloyd, C. E., Kar, P., Nagi, D., Naik, S., Nash, J., Nelson, H., Owen, K., Swindell, B., Walker, R., Whicher, C., & Wilmot, E. (2018). Language matters. Addressing the use of language in the care of people with diabetes: position statement of the English Advisory Group. Diabet. Med., 35(12), 1630–1634. https://doi.org/10.1111/dme.13705
Cupples, M. E., Cole, J. A., Hart, N. D., Heron, N., McKinley, M. C., & Tully, M. A. (2018). Shared decision-making (SHARE-D) for healthy behaviour change: a feasibility study in general practice. BJGP Open, 2(2). https://doi.org/10.3399/bjgpopen18X101517
Dickinson, J. K., Guzman, S. J., Maryniuk, M. D., O’Brian, C. A., Kadohiro, J. K., Jackson, R. A., et al. (2017). The use of language in diabetes care and education. Diabetes Care, 40(12), 1790–1799. https://doi.org/10.2337/dci17-0041
Elwyn, G., & Durand, M. A. (2017). Mastering shared decision making: the when, why and how. EBSCO Health. (https://health.ebsco.com)
Elwyn, G., Frosch, D., Thomson, R., Joseph-Williams, N., Lloyd, A., Kinnersley, P., et al. (2012). Shared decision making: A model for clinical practice. J. Gen. Intern. Med., 27(10), 1361–1367. https://doi.org/10.1007/s11606-012-2077-6
Fisher, L., Polonsky, W. H., Hessler, D., & Potter, M. B. (2017). A practical framework for encouraging and supporting positive behaviour change in diabetes. Diabet. Med., 34(12), 1658–1666. https://doi.org/10.1111/dme.13414
Funnell, M. M., Anderson, R. M., Arnold, M. S., Barr, P. A., Donnelly, M., Johnson, P. D., et al. (1991). Empowerment: an idea whose time has come in diabetes education. Diabetes Edu, 17(1), 37–41. https://doi.org/10.1177/014572179101700108
Gültzow, T., Zijlstra, D. N., Bolman, C., de Vries, H., Dirksen, C. D., Muris, J. W. M., Smit, E. S., & Hoving, C. (2021). Decision aids to facilitate decision making around behavior change in the field of health promotion: a scoping review. Patient Educ. Couns., 104(6), 1266–1285. https://doi.org/10.1016/j.pec.2021.01.015
Hamelinck, V. C., Bastiaannet, E., Pieterse, A. H., Jannink, I., van de Velde, C. J. H., Liefers, G. J., & Stiggelbout, A. M. (2014). Patients’ preferences for surgical and adjuvant systemic treatment in early breast cancer: a systematic review. Cancer Treat. Rev., 40(8), 1005–1018. https://doi.org/10.1016/j.ctrv.2014.06.007
Holmström, I., & Röing, M. (2010). The relation between patient-centeredness and patient empowerment: a discussion on concepts. Patient Educ. Couns., 79(2), 167–172. https://doi.org/10.1016/j.pec.2009.08.008
Kayser, L., Karnoe, A., Duminski, E., Somekh, D., & Vera-Muñoz, C. (2019). A new understanding of health related empowerment in the context of an active and healthy ageing. BMC Health Serv. Res., 19(1), 1–13. https://doi.org/10.1186/s12913-019-4082-5
Lau, D. H. (2002). Patient empowerment--a patient-centred approach to improve care. Hong Kong Med. J., 5, 372–374. (PMID: 12376717).
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal and coping. Springer.
Mead, N., & Bower, P. (2002). Patient-centred consultations and outcomes in primary care: a review of the literature. Patient Educ. Couns., 48(1), 51–61. https://doi.org/10.1016/S0738-3991(02)00099-X
Michie, S., van Stralen, M. M., & West, R. (2011). The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement. Sci., 6(1), 42. https://doi.org/10.1186/1748-5908-6-42
Mokhar, A., Topp, J., Härter, M., Schulz, H., Kuhn, S., Verthein, U., & Dirmaier, J. (2018). Patient-centered care interventions to reduce the inappropriate prescription and use of benzodiazepines and z-drugs: A systematic review. PeerJ. 6:e5535. https://doi.org/10.7717/peerj.5535
Rollnick, S., Butler, C. C., McCambridge, J., Kinnersley, P., Elwyn, G., & Resnicow, K. (2005). Consultations about changing behaviour. BMJ, 331(7522), 961–963. https://doi.org/10.1136/bmj.331.7522.961
Scholl, I., Zill, J. M., Härter, M., & Dirmaier, J. (2014). An integrative model of patient-centeredness-A systematic review and concept analysis. PLoS One, 9(9). https://doi.org/10.1371/journal.pone.0107828
Skinner, T. C., Joensen, L., & Parkin, T. (2020). Twenty-five years of diabetes distress research. Diabet. Med., 37(3), 393–400. https://doi.org/10.1111/dme.14157
Smith, R. C., Marshall-Dorsey, A. A., Osborn, G. G., Shebroe, V., Lyles, J. S., Stoffelmayr, B. E., et al. (2000). Evidence-based guidelines for teaching patient-centered interviewing. Patient Educ. Couns., 39(1), 27–36. https://doi.org/10.1016/S0738-3991(99)00088-9
Speight, J., Conn, J., Dunning, T., & Skinner, T. C. (2012). Diabetes Australia position statement. A new language for diabetes: improving communications with and about people with diabetes. Diabetes Res. Clin. Pract., 97(3), 425–431. https://doi.org/10.1016/j.diabres.2012.03.015
Speight, J., Skinner, T., Dunning, T., Black, T., Kilov, G., Lee, C., Scibilia, R., & Johnson, G. (2021). Our language matters: improving communication with and about people with diabetes. A position statement by Diabetes Australia. Diabetes Res. Clin. Pract., 173, 108,655. https://doi.org/10.1016/j.diabres.2021.108655
Stalmeier, P. F. M., van Tol-Geerdink, J. J., van Lin, E. N. J. T., Schimmel, E., Huizenga, H., van Daal, W. A. J., & Leer, J. W. (2007). Doctors’ and patients’ preferences for participation and treatment in curative prostate cancer radiotherapy. J. Clin. Oncol., 25(21), 3096–3100. https://doi.org/10.1200/JCO.2006.07.4955
Vuohijoki, A., Mikkola, I., Jokelainen, J., Keinänen-Kiukaanniemi, S., Winell, K., Frittitta, L., Timonen, M., & Hagnäs, M. (2020). Implementation of personalized care plan for patients with Type 2 diabetes is associated with improvements in clinical outcomes: An observational real-world study. Journal of Primary Care & Community Health, 11, 1–7.
Walters, R., Leslie, S. J., Polson, R., Cusack, T., & Gorely, T. (2020). Establishing the efficacy of interventions to improve health literacy and health behaviours: a systematic review. BMC Public Health, 20(1), 1040. https://doi.org/10.1186/s12889-020-08991-0
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Cavaco, A.M., Quitério, C.F., Félix, I.B., Guerreiro, M.P. (2023). Communication and Person-Centred Behaviour Change. In: Guerreiro, M.P., Brito Félix, I., Moreira Marques, M. (eds) A Practical Guide on Behaviour Change Support for Self-Managing Chronic Disease. Springer, Cham. https://doi.org/10.1007/978-3-031-20010-6_5
Download citation
DOI: https://doi.org/10.1007/978-3-031-20010-6_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-20009-0
Online ISBN: 978-3-031-20010-6
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)