Abstract
The knee is a pivot-condylar joint, through which important loads pass in weight-bearing position, and is also an essential joint involved in gait.
In children, radiographic measurements may be challenging, given some ossification centers may only be partially visible.
From a biomechanical perspective, growth causes a significant change in angular measurements. Therefore, the angle measurements presented in this chapter must be interpreted in an age-dependent manner. It should be noted that the measurement can be significantly affected by the degree of flexion or when performed in a standing position.
Knee disorders in children may have an effect on gait and weight-bearing and therefore have an impact on the biomechanics of other joints and in the general health.
An understanding of the biomechanics and different relations between the components of the joint is necessary to correctly diagnose pathology of the knee in children.
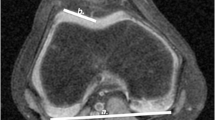
Radiography and ultrasound remain the initial imaging modalities of choice, with an increase in the use of MRI from early ages, although the prolonged imaging time and need for sedation in younger children may limit its use in daily practice. Because of the exposure to ionizing radiation, the use of computed tomography is limited to selected cases. In this chapter, we describe the normal radiological measurements of the tibiofemoral joint, the soft tissues of the tibiofemoral joint, and the patellofemoral joint.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Koifman A, Lefebvre J. Appearance of secondary ossification points and age determination of bone. Arch Fr Pediatr. 1956;13:1101–5.
Vergara-Amador E, Davalos Herrera D, Moreno LÁ. Radiographic features of the development of the anterior tibial tuberosity. Radiologia. 2016;58:294–300. https://doi.org/10.1016/j.rx.2016.01.005.
D’Amore T, Tanaka MJ, Cosgarea AJ. When and how far to move the tibial tuberosity in patients with patellar instability. Sports Med Arthrosc Rev. 2017;25:78–84. https://doi.org/10.1097/JSA.0000000000000146.
Laor T, Jaramillo D. MR imaging insights into skeletal maturation: what is normal? Radiology. 2009;250:28–38. https://doi.org/10.1148/radiol.2501071322.
Salenius P, Vankka E. The development of the tibiofemoral angle in children. J Bone Joint Surg Am. 1975;57:259–61.
Levine AM, Drennan JC. Physiological bowing and tibia vara. The metaphyseal-diaphyseal angle in the measurement of bowleg deformities. J Bone Joint Surg Am. 1982;64:1158–63.
Kristiansen LP, Gunderson RB, Steen H, Reikerås O. The normal development of tibial torsion. Skelet Radiol. 2001;30:519–22. https://doi.org/10.1007/s002560100388.
Botchu R, Obaid H, Rennie W. Correlation between trochlear dysplasia and the notch index. J Orthop Surg (Hong Kong). 2013;21:290–3. https://doi.org/10.1177/230949901302100305.
Lima FM, Debieux P, Aihara AY, et al. The development of the intercondylar notch in the pediatric population. Knee. 2020;27:747–54. https://doi.org/10.1016/j.knee.2020.04.020.
Reid JC, Yonke B, Tompkins M. The angle of inclination of the native ACL in the coronal and sagittal planes. Knee Surg Sports Traumatol Arthrosc. 2017;25:1101–5. https://doi.org/10.1007/s00167-017-4419-8.
Murao H, Morishita S, Nakajima M, Abe M. Magnetic resonance imaging of anterior cruciate ligament (ACL) tears: diagnostic value of ACL-tibial plateau angle. J Orthop Sci. 1998;3:10–7. https://doi.org/10.1007/s007760050016.
Perkins CA, Willimon SC. Pediatric anterior cruciate ligament reconstruction. Orthop Clin N Am. 2020;51:55–63. https://doi.org/10.1016/j.ocl.2019.08.009.
Wörtler K. MRT des Kniegelenks. Radiologe. 2007;47:1131–46. https://doi.org/10.1007/s00117-007-1581-x.
Fox MG. MR imaging of the meniscus: review, current trends, and clinical implications. Radiol Clin N Am. 2007;45:1033–53. https://doi.org/10.1016/j.rcl.2007.08.009.
Nietosvaara Y. The femoral sulcus in children. An ultrasonographic study. J Bone Joint Surg Br. 1994;76:807–9.
Richmond CG, Shea KG, Burlile JF, et al. Patellar-trochlear morphology in pediatric patients from 2 to 11 years of age: a descriptive analysis based on computed tomography scanning. J Pediatr Orthop. 2020;40:e96–e102. https://doi.org/10.1097/BPO.0000000000001405.
Trivellas M, Kelley B, West N, et al. Trochlear morphology development: study of normal pediatric knee MRIs. J Pediatr Orthop. 2021;41:77–82. https://doi.org/10.1097/BPO.0000000000001697.
Düppe K, Gustavsson N, Edmonds EW. Developmental morphology in childhood patellar instability: age-dependent differences on magnetic resonance imaging. J Pediatr Orthop. 2016;36:870–6. https://doi.org/10.1097/BPO.0000000000000556.
Brattstroem H. Shape of the intercondylar groove normally and in recurrent dislocation of patella. A clinical and x-ray-anatomical investigation. Acta Orthop Scand Suppl. 1964;68(SUPPL 68):1–148.
Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg, Sports Traumatol Arthrosc. 1994;2:19–26. https://doi.org/10.1007/BF01552649.
Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114–21. https://doi.org/10.1177/0363546503260788.
Mizobuchi RR, Galbiatti JA, Quirici Neto F, et al. Ultrasonographic study of the femoropatellar joint and its attachments in normal infants from birth to 24 months of age: part I. J Pediatr Orthop B. 2007;16:262–5. https://doi.org/10.1097/BPB.0b013e32809256d0.
Nietosvaara AY, Aalto KA. Ultrasonographic evaluation of patellar tracking in children. Clin Orthop Relat Res. 1993;(297):62–4.
Nietosvaara Y, Aalto K. The cartilaginous femoral sulcus in children with patellar dislocation: an ultrasonographic study. J Pediatr Orthop. 1997;17:50–3.
Carrillon Y, Abidi H, Dejour D, et al. Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology. 2000;216:582–5. https://doi.org/10.1148/radiology.216.2.r00au07582.
Koëter S, Bongers EMHF, de Rooij J, van Kampen A. Minimal rotation aberrations cause radiographic misdiagnosis of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2006;14:713–7. https://doi.org/10.1007/s00167-005-0031-4.
Malghem J, Maldague B. Depth insufficiency of the proximal trochlear groove on lateral radiographs of the knee: relation to patellar dislocation. Radiology. 1989;170:507–10. https://doi.org/10.1148/radiology.170.2.2911676.
Ali SA, Helmer R, Terk MR. Analysis of the patellofemoral region on MRI: Association of Abnormal Trochlear Morphology with Severe Cartilage Defects. Am J Roentgenol. 2010;194:721–7. https://doi.org/10.2214/AJR.09.3008.
van Huyssteen AL, Hendrix MRG, Barnett AJ, et al. Cartilage-bone mismatch in the dysplastic trochlea. An MRI study. J Bone Joint Surg Br. 2006;88:688–91. https://doi.org/10.1302/0301-620X.88B5.16866.
Pfirrmann CW, Zanetti M, Romero J, Hodler J. Femoral trochlear dysplasia: MR findings. Radiology. 2000;216:858–64. https://doi.org/10.1148/radiology.216.3.r00se38858.
Dickens AJ, Morrell NT, Doering A, et al. Tibial tubercle-trochlear groove distance: defining normal in a pediatric population. J Bone Joint Surg Am. 2014;96:318–24. https://doi.org/10.2106/JBJS.M.00688.
Schoettle PB, Zanetti M, Seifert B, et al. The tibial tuberosity–trochlear groove distance; a comparative study between CT and MRI scanning. Knee. 2006;13:26–31. https://doi.org/10.1016/j.knee.2005.06.003.
Koshino T, Sugimoto K. New measurement of patellar height in the knees of children using the epiphyseal line midpoint. J Pediatr Orthop. 1989;9:216–8.
Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–4. https://doi.org/10.1148/101.1.101.
Miller TT, Staron RB, Feldman F. Patellar height on sagittal MR imaging of the knee. AJR Am J Roentgenol. 1996;167:339–41. https://doi.org/10.2214/ajr.167.2.8686598.
Caton J, Deschamps G, Chambat P, et al. Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot. 1982;68:317–25.
Thévenin-Lemoine C, Ferrand M, Courvoisier A, et al. Is the caton-deschamps index a valuable ratio to investigate patellar height in children? J Bone Joint Surg Am. 2011;93:e35. https://doi.org/10.2106/JBJS.J.00759.
Grelsamer RP, Meadows S. The modified insall-salvati ratio for assessment of patellar height. Clin Orthop Relat Res. 1992:170–6.
Blackburne JS, Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59:241–2. https://doi.org/10.1302/0301-620X.59B2.873986.
Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–6.
Grelsamer RP, Newton PM, Staron RB. The medial-lateral position of the patella on routine magnetic resonance imaging: when is normal not normal? Arthroscopy. 1998;14:23–8. https://doi.org/10.1016/s0749-8063(98)70116-1.
Meyers AB, Laor T, Sharafinski M, Zbojniewicz AM. Imaging assessment of patellar instability and its treatment in children and adolescents. Pediatr Radiol. 2016;46:618–36. https://doi.org/10.1007/s00247-015-3520-8.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Aparisi Gómez, M.P., Simoni, P., Bazzocchi, A. (2023). Knee. In: Simoni, P., Aparisi Gómez, M.P. (eds) Essential Measurements in Pediatric Musculoskeletal Imaging. Springer, Cham. https://doi.org/10.1007/978-3-031-17735-4_9
Download citation
DOI: https://doi.org/10.1007/978-3-031-17735-4_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-17734-7
Online ISBN: 978-3-031-17735-4
eBook Packages: MedicineMedicine (R0)