Abstract
Precision medicine has emerged as an optimal health-care delivery platform, which emphasizes integration of individual patient characteristics into patient care. For lung cancer, precision approaches have focused mostly on targeted therapies directed at tyrosine kinases and immunotherapy. It is proposed that refinements should focus on improved risk stratification of patients at heightened risk of lung malignancy, namely patients with chronic obstructive pulmonary disease (COPD). African ancestry is associated with worsened clinical outcomes in COPD and lung cancer, which is relevant for Latinx populations given that varying degrees of African ancestry exist among several Latinx subgroups. The work reviewed here focuses on ORF1p, a protein encoded by Long Interspersed Element-1 (LINE-1) and associated with genetic instability. Because high expression of ORF1p is associated with poor prognosis in patients with non-small-cell lung cancer (NSCLC), it is hypothesized that circulating ORF1p can be monitored as a proxy of genetic instability in patients with COPD and lung cancer. Circulating ORF1p levels correlate with FEV1 deficits and airflow limitation (the hallmark of COPD) in former smokers, and tissue expression of ORF1p is increased in TP53 mutant NSCLC compared to wildtype. Understanding the role of ORF1p in COPD and lung cancer and its utility as a biomarker of genetic instability may lead to advances in lung cancer care and development of novel targeted therapies.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
Unmet Needs in Lung Cancer Diagnosis and Treatment
Lung cancer remains the leading cause of cancer-related mortality worldwide [1], with deaths likely to remain elevated, in part, due to continued use of tobacco products among young adults [2], increasing recreational use of inhaled toxic substances [3], and worsening levels of environmental pollution in some parts of the world [4]. Every year, 1.8 million people are diagnosed with lung cancer, with 5-year survival rates ranging from 4% to 17%, depending on stage and regional differences [5]. Lung cancer deaths account for more lives lost every year than colon, breast, prostate, and pancreatic cancers combined [1, 6]. Non-small-cell lung cancer (NSCLC) accounts for ~85% of all lung cancer cases, with the majority of cases linked to tobacco smoke [7]. NSCLC disproportionately affects African Americans (AAs) compared to Caucasian Americans (CAs), even after adjusting for tobacco use [8]. Despite the introduction of low-dose computerized tomography screening, lung cancers in all racial and ethnic groups are often diagnosed late when curative surgical interventions are no longer an option [9]. Several targeted therapies are now available including: epidermal growth factor receptor inhibitors (such as the tyrosine kinase inhibitors erlotinib and gefitinib and the monoclonal antibody cetuximab); vascular endothelial growth factor inhibitors (such as bevacizumab); EML4-ALK inhibitors (such as crizotinib, with benefits mostly in relatively young, never, or light smokers with adenocarcinoma); and programmed cell death protein 1 (PD-1)/programmed cell death ligand 1 (PD-L1) checkpoint inhibitors (pembrolizumab, with antitumor activity against immune-positive cancers) [10]. Targeted therapies are considerably more effective against specific NSCLC variants, thus leaving a large number of patients with limited options for treatment. These knowledge gaps emphasize the need for more precise stratification of racial and ethnic groups; development of noninvasive, early biomarkers of lung cancer; and additional research to uncover molecular pathways of malignant conversion that can be targeted for therapeutic intervention.
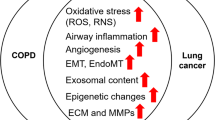
COPD is a highly prevalent chronic disease, characterized by persistent airflow limitation, debilitating morbidity, and staggering mortality [11]. The public health burden of COPD has increased substantially throughout the world, with chronic respiratory diseases now ranked as the third leading cause of death worldwide [12]. There is only limited understanding of the genetic factors that predispose to disease and, other than smoking cessation, no therapies to specifically modify trajectory of disease. A focus on COPD within the context of lung cancer is critical given that 50–80% of lung cancer patients have COPD compared with a 15–20% prevalence of COPD in the general smoking population [13, 14], and growing evidence that smokers with COPD are at significantly increased risk of lung cancer development [15,16,17,18,19,20,21]. In fact, in some patients, COPD may be an intermediate phenotype between smoking and lung cancer, although the exact mechanisms driving this relationship remain uncertain.
Racial and Ethnic Differences in COPD and Lung Cancer
COPD and lung cancer are related diseases associated with substantial morbidity and mortality [22]. Both of these conditions present more severely in individuals with African ancestry compared to CAs [23, 24], although the root causes of these differences have not been studied in detail. A recent study of genomic samples from Colombia, Mexico, Peru, and Puerto Rico identified several ancestry-enriched single nucleotide polymorphisms (SNPs) in genes coding for cytokine receptors, T cell receptor signaling, and antigen presentation [25]. The study also described SNPs with excess African or European ancestry that were linked to ancestry-specific expression patterns of genes involved in both the innate and adaptive immune systems, indicating their possible effects on health- and disease-related phenotypes in Latin(x) populations. In this regard, differential gene expression has been found in the lung tumors of AAs compared to CAs, along with significant differences in M1 and M2 macrophage infiltration into the tumor [26]. Other studies point to racial differences in genes involved in inflammation and oxidative stress in both lung cancer and COPD [27]. Such differences may eventually help explain the lower 5-year survival rate for lung cancer in AAs (16%) relative to CAs (19%). Survival is lower in AAs at every stage of diagnosis, which has been attributed to differences in timely, high-quality medical care [28, 29]. However, racial disparities may persist even after accounting for socioeconomic factors and access to care [30,31,32]. Interestingly, AAs develop COPD with less cumulative smoking and at younger ages [33,34,35], suggesting greater susceptibility to tobacco smoke carcinogens. The racial differences in lung cancer outcomes found in AAs are relevant to Latin(x) populations because this ethnic group is characterized by pervasive admixture among European settlers, Native Americans, and Africans. The large degree of admixture among Latin(x) suggests that their relative susceptibility is highly variable, and that subgroups with large African ancestry may share the enhanced susceptibility of AAs. The same argument may be raised for many AAs, where considerable genetic admixture exists across the United States. Interestingly, despite lower socioeconomic status, Latin(x) have been found to be at lower risk of COPD and lung cancer compared to AAs or CAs, even after accounting for differences in smoking status and intensity [36,37,38]. While the debate continues to determine whether such differences are accounted for by social, behavioral, environmental, and economic factors, growing evidence supports that “protection” of Latin(x) may be partly accounted for by Native American ancestry [39, 40]. In sharp contrast, the proportion of African ancestry has been associated with increased risk [41], suggesting that ancestral heterogeneity generates a broad spectrum of susceptibility among Latin(x) depending on the balance of protection and susceptibility afforded by the Native American and African ancestry components. This scenario is consistent with the inverse relation of African ancestry to lung function among AAs [42, 43].
ORF1p in COPD and Lung Cancer
The search for circulating biomarkers has become a research priority in the study of complex diseases. Blood is readily accessible and provides a relatively noninvasive means to detect illness-related alterations and track disease trajectory over time, allowing for amplification of the signal of interest for association with other clinical measures. One of our focuses over the past 10 years has been the study of LINE-1 retroelements and their role in the regulation of lung epithelial cell phenotypes and genetic instability. We have also been interested in examining the utility of measurements of LINE-1-encoded proteins in tissue and the general circulation as biomarkers of lung cancer. Human LINE-1 is ~6 kb and consists of an internal promoter, two open reading frames encoding two proteins (ORF1p and ORF2p), and a poly (A) tail [44] (Fig. 8.1). LINE-1 propagates its own DNA and other DNAs through a copy-and-paste mechanism that uses an RNA intermediate, a process known as retrotransposition. This process can lead to full-length or truncated insertions of LINE-1 sequences or other sequences throughout the genome [45]. Approximately 100 full-length, retrotransposition-competent copies of LINE-1 remain in the human genome [46]. In healthy somatic cells, LINE-1 is epigenetically silenced through DNA methylation, histone covalent modifications, and nucleosome positioning (Fig. 8.2). Hypomethylation of selected CpG sites by DNA damage, activation of the aryl hydrocarbon receptor by lung carcinogens present in tobacco smoke, or various other forms of toxic injury mediate transcriptional activation of LINE-1 and result in cellular buildup of ORF1p. This protein in turn modulates oncogenic signaling and participates in retrotransposition [47, 48]. To date, we have extensively characterized the molecular effectors responsible for epigenetic silencing of LINE-1 [49], and more recently have begun to exploit this knowledge to develop prevention strategies and targeted therapeutics against lung cancer.
Schematic representation of LINE-1. Full length LINE-1 is approximately 6 kb in length and consists of 5′ and 3′ untranslated regions (UTRs) and two proteins, ORF1 (orange) and ORF2 (blue). ORF1 is a nucleic acid binding protein consisting of an alpha helix in between the N- and C-terminal domains (NTD and CTD), with an RNA recognition motif (RRM) near the CTD. Coiled-coil interactions facilitate the formation of higher order multimers and polymers of ORF1p. ORF2p is approximately 150 kDa and contains both endonuclease (EN) and reverse transcriptase (RT) domains
The genome of NSCLCs is strongly affected by LINE-1 insertions [50, 51]. Several studies by our group and others have shown that ORF1p accumulates in lung cancer cells [52, 53]. This buildup is consistent with increased LINE-1 hypomethylation in lung cancer [54, 55]. Because COPD may be viewed as a preneoplastic state, at least in a subset of NSCLC patients, we hypothesized that measurements of circulating ORF1p may inform the clinical evaluation of patients with COPD. To test this hypothesis, the association of ORF1p with lung function and airflow limitation (the hallmark of COPD) was examined in a population-based cohort of adults [56]. Stratification by smoking status showed consistent associations of ORF1p with FEV1, FVC, and airflow limitation in former smokers, after adjustment for the above covariates and active asthma. The observed increases in ORF1p after smoking cessation suggest that sustained alterations in genetic control of LINE-1 coupled with genetic instability occur in at least a subgroup of former smokers. Indeed, previous reports have shown that airway and systemic inflammation may persist in a proportion of smokers after smoking cessation, posing increased risk of inception and progression of COPD years after quitting [57]. Given that the cohort examined was mostly CAs, and that our sample size was only 427 subjects, additional studies are required to evaluate the generalizability of our findings and their relevance to different racial and ethnic groups. These limitations notwithstanding our findings suggest that ORF1p is associated with lower lung function and increased airflow limitation in former smokers. A preliminary study comparing self-identified Latin(x) and African Americans has suggested that ostensibly healthy AAs have higher levels of circulating ORF1p than Latin(x), and that females exhibit higher protein levels than males (Ramos et al., unpublished). These data are consistent with our working hypothesis and raise important questions about the impact of genetic admixture and sex on ORF1p levels in the general circulation.
ORF1p is a basic protein with conserved C- and N-terminal coiled-coil domains responsible for multimerization [58]. Coiled-coil proteins are involved in tethering of transport vesicles and regulation of cargo binding [59], functions consistent with the accumulation of ORF1p in circulating human exosomes [60]. ORF1p functions as a single-stranded RNA and DNA-binding protein with chaperone activity and is known to participate in retrotransposition [61,62,63]. As such, measurements of ORF1p reflect the LINE-1 status and serve as a tool for development of sensitive biomarkers of genetic instability in lung cancer. ORF1p interacts with a number of cellular proteins [64], including nucleolin (NCL). NCL is an RNA-binding protein with multiple roles in ribosome biogenesis, transcription, RNA turnover, translation, DNA repair, and apoptosis [65,66,67]. This protein accumulates in the cytoplasm and the cell surface in several cancer types, including lung cancer [68, 69]. We have recently shown that NCL regulates ORF1p expression and that this interaction can be targeted by NCL antagonists [70]. We also showed that pharmacological inhibition of NCL arrests NSCLC growth in a nude mouse xenograft model of lung cancer. These findings open the door to novel therapies for lung cancer treatment focused on inhibition of LINE-1 activity in cancer cells.
Concluding Remarks
Given the molecular heterogeneity that characterizes lung cancer, precision approaches that risk stratify individuals and populations, coupled with targeted therapies, are needed. Population stratification is particularly relevant for precise identification of individuals at risk of lung malignancy. While the increased susceptibility to lung cancer in individuals of African ancestry has been recognized for years, little is known about the genetic, environmental, and lifestyle determinants of this increased susceptibility. For Latin(x) groups, this gap in knowledge is significant given their large degree of genetic admixture, which may either afford protection or increased susceptibility depending on the relative degree of genetic admixture. Such differences in susceptibility also become relevant for future development of targeted therapies. Currently available therapies only benefit a small subset of NSCLC patients, mostly those who are either relatively young or never/light smokers. Thus, novel strategies are needed to increase the numbers of lung cancer patients who may benefit from precision therapies. Precision approaches will help to better define the root causes of lung cancer heterogeneity in different populations and address some of the shortcomings of low-dose computerized tomography screening. Together, the evidence reviewed here can be contextualized to develop novel risk stratification strategies and targeted therapies for lung cancer that take into account genetic admixture and health disparities among Latin(x) populations.
References
Dela Cruz CS, Tanoue LT, Matthay RA. Lung cancer: epidemiology, etiology and prevention. Clin Chest Med. 2011;32(4):605–44. https://doi.org/10.1016/j.ccm.2011.09.001.
Centers for Disease Control and Prevention. Tobacco use by youth is rising. https://www.cdc.gov/vitalsigns/youth-tobacco-use/index.html. Accessed 2 Sept 2020.
Centers for Disease Control and Prevention. Outbreak of lung injury associated with the use of e-cigarette, or vaping, products. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html. Accessed 1 Sept 2020.
Song Q, Christiani DC, Wang X, Ren J. The global contribution of outdoor air pollution to the incidence, prevalence, mortality and hospital admission for chronic obstructive pulmonary disease: a systematic review and meta-analysis. Int J Environ Res Public Health. 2014;11(11):11822–32. https://doi.org/10.3390/ijerph111111822.
Travis WD. Pathology of lung cancer. Clin Chest Med. 2011;32(4):669–92. https://doi.org/10.1016/j.ccm.2011.08.005.
Alberg AJ, Brock MV, Ford JG, Samet JM, Spivack SD. Epidemiology of lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e1S–e29S. https://doi.org/10.1378/chest.12-2345.
Molina JR, Yang P, Cassivi SD, Schild SE, Adjei AA. Non–small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc. 2009;83(5):584–94. https://doi.org/10.4065/83.5.584.
Ryan BM. Lung cancer health disparities. Carcinogenesis. 2018;39(6):741–51. https://doi.org/10.1093/carcin/bgy047.
Schabath MB, Cress WD, Munoz-Antonia T. Racial and ethnic differences in the epidemiology of lung cancer and the lung cancer genome. Cancer Control. 2016;23(4):338–46. https://doi.org/10.1177/107327481602300405.
Halliday PR, Blakely CM, Bivona TG. Emerging targeted therapies for the treatment of non-small cell lung cancer. Curr Oncol Rep. 2019;21(3):21. https://doi.org/10.1007/s11912-019-0770-x.
Segal LN, Martinez FJ. Chronic obstructive pulmonary disease subpopulations and phenotyping. J Allergy Clin Immunol. 2018;141:1961–71. https://doi.org/10.1016/j.jaci.2018.02.035.
GBD Chronic Respiratory Disease Collaborators. Prevalence and attributable health burden of chronic respiratory diseases, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir Med. 2020;8:585–96. Available from: https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30105-3/fulltext. Accessed 4 Sept 2020.
El-zein, RA, Young RP, Hopkins RJ, Etzel CJ. Genetic predisposition to chronic obstructive pulmonary disease and/or lung cancer: important considerations when evaluating risk. Cancer Prev Res. 2012;5(4):522–7. Available from: https://doi.org/10.1158/1940-6207.CAPR-12-0042.
Young RP, Hopkins RJ. How the genetics of lung cancer overlap with COPD. Respirology. 2011;16(7):1047–55. https://doi.org/10.1111/j.1440-1843.2011.02019.x.
Husebo GR, Nielsen R, Hardie J, Bakke PS, Lerner L, D’Alessandro-Gabazz C, Gyuris J, Gabazza E, Aukrust P, Eagan T. Risk factors for lung cancer in COPD – results from the Bergen COPD cohort study. Respir Med. 2019;152:81–8. https://doi.org/10.1016/j.rmed.2019.04.019.
Mannino DM, Aguayo SM, Petty TL, Redd SC. Low lung function and incident lung cancer in the United States: data from the first National Health and Nutrition Examination Survey follow-up. Arch Intern Med. 2003;163:1475–80.
Gagnat AA, Gulsvik A, Bakke P, Gjerdevik M. Comparison of two lung cancer screening scores among patients with chronic obstructive pulmonary disease: a community study. Clin Respir J. 2019;13(2):114–9. https://doi.org/10.1111/crj.12988.
Tockman MS, Anthonisen NR, Wright EC, Donithan MG. Airways obstruction and the risk for lung cancer. Ann Inter Med. 1987;106:512–8.
Lowry KP, Gazelle GS, Gilmore ME, Johanson C, Munshi V, Choi SE, et al. Personalizing annual lung cancer screening for patients with chronic obstructive pulmonary disease: a decision analysis. Cancer. 2015;121:1556–62. https://doi.org/10.1002/cncr.29225.
Wang J, Spitz MR, Amos CI, Wu X, Wetter DW, Cinciripini PM, et al. Method for evaluating multiple mediators: mediating effects of smoking and COPD on the association between the CHRNA5-A3 variant and lung cancer risk. PLoS One. 2012;7(10):e47705.
Yang IA, Relan V, Wright CM, Davidson MR, Sriram KB, Savarimuthu SM, et al. Common pathogenic mechanisms and pathways in the development of COPD and lung cancer. Expert Opin Ther Targets. 2011;15(4):439–56. https://doi.org/10.1517/14728222.2011.555400.
Young RP, Hopkins RJ, Gamble GD, Etzel C, El-Zein R, Crapo JD. Genetic evidence linking lung cancer and COPD: a new perspective. Appl Clin Genet. 2011;4:99–111. https://doi.org/10.2147/TACG.S20083.
Mina N, Soubani AO, Cote ML, Suwan T, Wenzlaff AS, Jhajhria S, et al. The relationship between COPD and lung cancer in African American patients. Clin Lung Cancer. 2012;13(2):149–56. https://doi.org/10.1016/j.cllc.2011.09.006.
Dransfield MT, Davis JJ, Gerald LB, Bailey WC, et al. Racial and gender differences in susceptibility to tobacco smoke among patients with chronic obstructive pulmonary disease. Respir Med. 2006;100(6):1110–6.
Bryc K, Durand EY, Macpherson JM, Reich D, Mountain JL. The genetic ancestry of African Americans, Latinos and European Americans across the United States. Am J Hum Genet. 2015;96(1):37–53. https://doi.org/10.1016/j.ajhg.2014.11.010.
Jacklute J, Zermaitis M, Pranys D, Sitkauskiene B, Miliauskas S, Vaitkiene S, et al. Distribution of M1 and M2 macrophages in tumor islets and stroma in relation to prognosis of non-small cell lung cancer. BMC Immunol. 2018;19:3. https://doi.org/10.1186/s12865-018-0241-4.
Barnes PJ. Molecular genetics of chronic obstructive pulmonary disease. Thorax. 1999;54:245–52. https://doi.org/10.1136/thx.54.3.245.
Bach PB, Schrag D, Brawley OW, Galaznik A, Yakren S, Begg CB. Survival of blacks and whites after a cancer diagnosis. JAMA. 2002;287(16):2106–13. https://doi.org/10.1001/jama.287.16.2106.
Schwartz AG, Prysak GM, Bock CH, Cote ML. The molecular epidemiology of lung cancer. Carcinogenesis. 2006;28(3):507–18. https://doi.org/10.1093/carcin/bgl253.
William DR, Priest N, Anderson N. Understanding associations between race, socioeconomic status and health: patterns and prospects. Health Psychol. 2016;35(4):407–11. https://doi.org/10.1037/hea0000242.
Centers for Disease Control and Prevention (CDC). Racial/ethnic disparities and geographic differences in lung cancer incidence – 38 States and the District of Columbia, 1998–2006. Morb Mortal Wkly Rep. 2010;59(44):1434–8.
American Cancer Society. Cancer facts & figures for African Americans 2019–2021. Atlanta: American Cancer Society; 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-african-americans/cancer-facts-and-figures-for-african-americans-2019-2021.pdf. Accessed 1 Sept 2020.
Chatila WM, Wynkoop WA, Vance G, Criner CJ. Smoking patterns in African Americans and whites with advanced COPD. Chest. 2004;125(1):15–21. https://doi.org/10.1378/chest.125.1.15.
Putcha N, Han MK, Martinez CH, Foreman MG, Anzueto AR, Casaburi R, et al. Comorbidities of COPD have a major impact on clinical outcomes, particularly in African Americans. Chronic Obstr Pulm Dis. 2014;1(1):105–14. https://doi.org/10.15326/jcopdf.1.1.2014.0112.
Roberts ME, Colby SM, Lu B, Ferketich AK. Understanding tobacco use onset among African Americans. Nicotine Tob Res. 2016;18(S1):S49–56.
Diaz AA, Celli B, Celedon JC. Chronic obstructive pulmonary disease in Hispanics. A 9-year update. Am J Resp Crit Care Med. 2018;197:15–21. https://doi.org/10.1164/rccm.201708-1615PP.
Bruse S, Sood A, Petersen H, Liu Y, Leng S, Celedon JC, et al. New Mexican Hispanic smokers have lower odds of chronic obstructive pulmonary disease and less decline in lung function than non-Hispanic whites. Am J Respir Crit Care Med. 2011;184(11):1254–60. https://www.atsjournals.org/doi/full/10.1164/rccm.201103-0568OC. Accessed 3 Sept 2020.
Young RP, Hopkins RJ. A review of the Hispanic paradox: time to spill the beans? Eur Respir Rev. 2014;23(134):439–49. https://doi.org/10.1183/09059180.00000814.
Leng S, Liu Y, Thomas CL, Gauderman WJ, Picchi MA, Bruse SE, et al. Native American ancestry affects the risk for gene methylation in the lungs of Hispanic smokers from New Mexico. Am J Respir Crit Care Med. 2013;188(9):1110–6. https://www.atsjournals.org/doi/full/10.1164/rccm.201305-0925OC. Accessed 1 Sept 2020.
Stern MC, Fejerman L, Das R, Setiawan VW, Cruz-Correa MR, Perez-Stable EJ, et al. Variability in cancer risk and outcomes within US Latinos by national origin and genetic ancestry. Curr Epidemiol Rep. 2016;3:181–90. https://link.springer.com/article/10.1007/s40471-016-0083-7. Accessed 1 Sept 2020.
Haiman CA, Stram DO, Wilens LR, Pike MC, Kolonel LN, Henderson BE, et al. Ethnic and racial differences in the smoking-related risk of lung cancer. N Engl J Med. 2006;354:333–42. https://www.nejm.org/doi/full/10.1056/NEJMoa033250.
Kumar R, Seibold MA, Aldrich MC, Williams LK, Reiner AP, Colangelo L, et al. Genetic ancestry in lung-function predictions. N Engl J Med. 2010;363(4):321–30. https://doi.org/10.1056/NEJMoa0907897.
Aldrich MC, Kumar R, Colangelo LA, Williams LK, Sen S, Kritchevsky SB, et al. Genetic ancestry-smoking interactions and lung function in African Americans: a cohort study. PLoS One. 2012;7(6):e39541. https://doi.org/10.1371/journal.pone.0039541.
Khalid M, Bojang P, Hassanin AAI, Bowers EC, Ramos IN, Ramos KS. LINE-1: implications in the etiology of cancer, clinical applications and pharmacological targets. Mut Res Rev. 2018;778:51–60. https://doi.org/10.1016/j.mrrev.2018.09.003.
Bojang P, Roberts R, Anderton M, Ramos KS. De novo LINE-1 retrotransposition in HepG2 cells preferentially targets gene poor regions of chromosome 13. Genomics. 2014;104(2):96–104. https://doi.org/10.1016/j.ygeno.2014.07.001.
Beck CR, Collier P, Macfarlane C, Malig M, Kidd JM, Eichler EE, et al. LINE-1 retrotransposition activity in human genomes. Cell. 2010;141:1159–70. https://doi.org/10.1016/j.cell.2010.05.021.
Reyes-Reyes EN, Ramos I, Tavera-Garcia MA, Ramos KS. The aryl hydrocarbon receptor agonist benzo(a)pyrene reactivates LINE-1 in HepG2 cells through canonical TGF-β1 signaling: implications in hepatocellular carcinogenesis. Am J Cancer Res. 2016:1066–77. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4889720/. Accessed 1 Sept 2020.
Reyes-Reyes EM, Aispuro I, Tavera-Garcia MA, Field M, Moore S, Ramos IN, et al. LINE-1 couples EMT programming with acquisition of oncogenic phenotypes in human bronchial epithelial cells. Oncotarget. 2017:103828–42. https://doi.org/10.18632/oncotarget.21953.
Bojang P, Ramos KS. Epigenetic reactivation of LINE-1 disrupts NuRD co-repressor functions and induces oncogenic transformation of human bronchial epithelial cells. Mol Oncol. 2018;12:1342–57. https://febs.onlinelibrary.wiley.com/doi/full/10.1002/1878-0261.12329. Accessed 1 Sept 2020.
Iskow RC, McCabe MT, Mills RE, Torene S, Pittard WS, Neuwald AF, et al. Natural mutagenesis of human genomes by endogenous retrotransposons. Cell. 2010;141:1253–61. https://doi.org/10.1016/j.cell.2010.05.020.
Rodic N, Sharma R, Sharma R, Zampella J, Dai L, Taylor MS, et al. Long interspersed element-1 protein expression is a hallmark of many human cancers. Am J Pathol. 2014;184:1280–6. https://doi.org/10.1016/j.ajpath.2014.01.007.
Asch HL, Eliacin E, Fanning TG, Connolly JL, Bratthauer G, Asch BB. Comparative expression of the line-1 p40 protein in human breast carcinomas and normal breast tissues. Oncol Res. 1996;8:239–47. https://doi.org/10.1373/clinchem.2016.257444.
Su Y, Davies S, Davis M, Lu H, Giller R, Krailo M, et al. Expression of LINE-1 p40 protein in pediatric malignant germ cell tumors and its association with clinicopathological parameters: a report from the Children’s Oncology Group. Cancer Lett. 2007;247:204–12. https://doi.org/10.1016/j.canlet.2006.04.010.
Ikeda K, Shiraishi K, Eguchi A, Shibata H, Yoshimoto K, Mori T, et al. Long interspersed nucleotide element 1 hypomethylation is associated with poor prognosis of lung adenocarcinoma. Ann Thorac Surg. 2013;96:1790–4. https://doi.org/10.1016/j.athoracsur.2013.06.035.
Saito K, Kawakami K, Matsumoto I, Oda M, Watanabe G, Minamoto T. Long interspersed nuclear element 1 hypomethylation is a marker of poor prognosis in stage IA non-small cell lung cancer. Clin Cancer Res. 2010;16:2418–26. https://doi.org/10.1158/1078-0432.CCR-09-2819.
Guerra S, Vasquez MM, Bojang P, Ramos IN, Sherrill DL, Martinez FD, et al. Serum levels of LINE1-ORF1p and airflow limitation. Eur Respir J Open. 2019;5:00247-2018. https://openres.ersjournals.com/content/5/4/00247-2018. Accessed 1 Sept 2020.
Hogg JC. Why does airway inflammation persist after the smoking stops. Thorax. 2006;61:96–7. https://doi.org/10.1136/thx.2005.049502.
Martin SJ. The ORF1 protein encoded by LINE-1: structure and function during L1 retrotransposition. J Biomed Biotechnol. 2006;2006:45621. https://doi.org/10.1155/JBB/2006/45621.
Truebestein L, Leonard TA. Coiled-coils: the long and short of it. BioEssays. 2016;38:903–16. https://doi.org/10.1002/bies.201600062.
Bowers EC, Cavalcante AM, McKay BS, Ramos KS. The LINE-1 ORF1 protein content of extracellular vesicles mirrors cellular expression profiles in Non-Small Cell Lung Cancer cell lines. Submitted for publication, 2020.
Martin SL, Bushman FD. Nucleic acid chaperone activity of the ORF1 protein from the mouse LINE-1 retrotransposon. Mol Cell Biol. 2001;2:467–75. https://doi.org/10.1128/MCB.21.2.467-475.2001.
Naufer MN, Furano AV, Williams MC. Protein-nucleic acid interactions of LINE-1 ORF1p. Semin Cell Dev Biol. 2019;86:140–9. https://doi.org/10.1016/j.semcdb.2018.03.019.
Naufer NM, Callahan KE, Cook PR, Perez-Gonzalez CE, Williams MC, Furano AV. L1 retrotransposition requires rapid ORF1p oligomerization, a novel coiled coil-dependent property conserved despite extensive remodeling. Nucleic Acids Res. 2016;44:281–93. https://doi.org/10.1093/nar/gkv1342.
Goodier JL, Cheung LE, Kazazian HH. Mapping the LINE1 ORF1 protein interactome reveals associated inhibitors of human retrotransposition. Nucleic Acids Res. 2013;41(15):7401–19. https://doi.org/10.1093/nar/gkt512.
Abdelmohsen K, Goroscope M. RNA-binding protein nucleolin in disease. RNA Biol. 2012;9(6):799–808. https://doi.org/10.4161/rna.19718.
Piazzi M, Bavelloni A, Gallo A, Faenza I, Blalock WL. Signal transduction in ribosome biogenesis: a recipe to avoid disaster. Int J Mol Sci. 2019;20(11):2718. https://doi.org/10.3390/ijms20112718.
Jia W, Yao Z, Zhao J, Guan Q, Gao L. New perspectives of physiological and pathological functions of nucleolin (NCL). Life Sci. 2017;186:1–10. https://doi.org/10.1016/j.lfs.2017.07.025.
Huang F, Wu Y, Tan H, Guo T, Zhang K, Li D, et al. Phosphorylation of nucleolin is indispensable to its involvement in the proliferation and migration of non-small cell lung cancer cells. Oncol Rep. 2019;41:590–8. https://doi.org/10.3892/or.2018.6787.
Xu J-Y, Lu S, Xu X-Y, Hu S-L, Li B, Li W-X, et al. Prognostic significance of nuclear or cytoplasmic nucleolin expression in human non-small cell lung cancer and its relationship with DNA-PKcs. Tumor Biol. 2016;37(8):10349–56. https://doi.org/10.1007/s13277-016-4920-6.
Ramos KS, Moore S, Rogue I, Courty J, Reyes-Reyes EM. The nucleolin antagonist N6L inhibits LINE1 retrotransposon expression in non-small cell lung cancer cells. J Cancer. 2019;11:733–40. https://doi.org/10.7150/jca.37776.
Acknowledgments
The creative contributions of Dr. Emma Bowers in the design of figures and the editorial assistance of Ms. Kim Nguyen are gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Ramos, K.S., Guerra, S., El-Zein, R. (2023). Precision Medicine Approaches for Stratification and Development of Novel Therapies of Latin(x) Patients at Risk of Lung Malignancy. In: Ramirez, A.G., Trapido, E.J. (eds) Advancing the Science of Cancer in Latinos. Springer, Cham. https://doi.org/10.1007/978-3-031-14436-3_8
Download citation
DOI: https://doi.org/10.1007/978-3-031-14436-3_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-14435-6
Online ISBN: 978-3-031-14436-3
eBook Packages: MedicineMedicine (R0)