Abstract
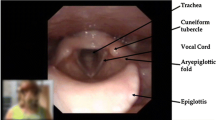
Functional disorders of the larynx can present in a diverse manner with symptoms such as dysphonia, dyspnea, and dysphagia. Muscle tension dysphonia (MTD) may cause disrupted phonation due to overactive laryngeal musculature. MTD is diagnosed by a thorough clinical history and laryngoscopic visualization of the vocal cords and supra-glottic region. Vocal hygiene and voice therapy are the foundations of MTD treatment with concomitant medical therapy when indicated. Paradoxical vocal cord dysfunction (PVCD) can cause shortness of breath due to inappropriate vocal cord adduction during respiration. Laryngoscopic evaluation is the gold standard in the diagnosis of PVCD and remains an important investigation to differentiate PVCD from other respiratory conditions. Patient reassurance during an acute event of PVCD is most often indicated, whereas speech therapy is the principal treatment for the prevention of further episodes. Globus pharyngeus may present as the sensation of a lump in the throat, although the etiology of this functional disorder remains unclear. The diagnosis of globus pharyngeus requires the exclusion of alternative diagnoses such as gastroesophageal reflux disease and major esophageal motor disorders. Globus pharyngeus is a benign disorder that can be treated with careful reassurance, a trial of gastric acid suppression, or neuromodulator medications. Altogether, functional disorders of the larynx require careful attention from clinicians. When such disorders are appropriately diagnosed and treated, the quality of life of patients can greatly improve.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Sasaki CT, Issacson G. Functional anatomy of the larynx. Otolaryngol Clin N Am. 1988;21(4):595.
Beslie GM, Morrison MD. Anatomic correlation for muscle tension dysphonia. J Otolaryngol. 1983;12(5):319–21.
Van Houtte E, Van Lierde K, Claeys S. Pathophysiology and treatment of muscle tension dysphonia: a review of the current knowledge. J Voice. 2011;25(2):202–7.
Gardner GM, Benninger MS. Other neuromuscular causes of dysphonia and trauma. In: Otolaryngoloy: a color handbook. Boca Raton, FL: CRC Press; 2016. p. 189–200.
Morrison MD, Rammage LA, Beslie GM, Pullan CB, Nichol H. Muscular tension dysphonia. J Otolaryngol. 1983;12(5):302–6.
Morrison MD, Rammage LA. Muscle misuse voice disorders: description and classification. Acta Otolaryngol. 1993;113(3):428–34.
Van Houtte E, Van Lierde K, D’Haeseleer E, Claeys S. The prevalence of laryngeal pathology in a treatment-seeking population with dysphonia. Laryngoscope. 2010;120(2):306–12.
Roy N. Functional dysphonia. Curr Opin Otolaryngol Head Neck Surg. 2003;11:144–8.
Bridger MW, Epstein R. Functional voice disorders: a review of 109 patients. J Laryngol Otol. 1983;97(12):1145.
Sama A, Carding PN, Price S, Kelly P, Wilson JA. The clinical features of functional dysphonia. Laryngoscope. 2001;111(3):458–63.
Hočevar-Boltežar I, Janko M, Žargi M. Role of surface EMG in diagnostics and treatment of muscle tension dysphonia. Acta Otolaryngol. 1998;118(5):739–43.
Redenbaugh MA, Reich AR. Surface EMG and related measures in normal and vocally hyperfunctional speakers. J Speech Hear Disord. 1989;54(1):68.
Koufman JA, Blalock PD. Functional voice disorders. Otollaryngol Clin North Am. 1991;1(24):1059–73.
Koufman JA, Blalock PD. Classification and approach to patients with functional voice disorders. Ann Otol Rhinol Laryngol. 1982;91:372–7.
Roy N, Bless DM, Heisey D. Personality and voice disorders: a superfactor trait analysis. J Speech Lang Hear Res. 2000;43:749–68.
Roy N, McGrory JJ, Tasko SM, Bless DM, Heisey D, Ford CN. Psychological correlates of functional dysphonia: an investigation using the Minnesota multiphasic personality inventory. J Voice. 1997;11(4):443–51.
Van Mersbergen M, Patrick C, Glaze L. Functional dysphonia during mental imagery: testing the trait theory of voice disorders. J Speech Lang Hear Res. 2008;51(6):1405–23.
Angsuwarangsee T, Morrison MD. Extrinsic laryngeal muscular tension in patients with voice disorders. J Voice. 2002;16(3):333–43.
Altman KW, Atkinson C, Lazarus C. Current and emerging concepts in muscle tension dysphonia: a 30-month review. J Voice. 2005;19(2):261–7.
McGarey PO, Barone NA, Freeman M, Daniero JJ. Comorbid dysphagia and dyspnea in muscle tension dysphonia: a global laryngeal musculoskeletal problem. OTO Open. 2018;2(3):2473974X1879567.
Koufman JA, Amin MR, Panetti M. Prevalence of reflux in 113 consecutive patients with laryngeal and voice disorders. Otolaryngol Head Neck Surg. 2000;123(4):385–8.
Abitbol J, Abitbol P, Abitbol B. Sex hormones and the female voice. J Voice. 1999;13(3):424–46.
D’Haeseleer E, Depypere H, Claeys S, Van Borsel J, Van Lierde K. The menopause and the female larynx, clinical aspects and therapeutic options: a literature review. Maturitas. 2009;64(1):27–32.
Bielamowicz S. Aging voice or vocal fold paresis. Arch Otolaryngol Neck Surg. 2004;130(9):1114.
Morrison MD, Nichol H, Rammage LA. Diagnostic criteria in functional dysphonia. Laryngoscope. 1986;96(1):1.
Ruotsalainen J, Sellman J, Lehto L, Verbeek J. Systematic review of the treatment of functional dysphonia and prevention of voice disorders. Otolaryngol Head Neck Surg. 2008;138(5):557–65.
Smith ME, Houtz DR. Muscle tension dysphonia and puberphonia. Multidisciplinary management of pediatric voice and swallowing disorders. Cham: Springer; 2020. p. 239–44.
Mackenzie K, Millar A, Wilson JA, Sellars C, Deary IJ. Is voice therapy an effective treatment for dysphonia? A randomised controlled trial. BMJ. 2001;323(7314):658.
Carding PN, Horsley IA, Docherty GJ. A study of the effectiveness of voice therapy in the treatment of 45 patients with nonorganic dysphonia. J Voice. 1999;13(1):72–104.
Ruotsalainen JH, Sellman J, Lehto L, Jauhiainen M, Verbeek JH. Interventions for treating functional dysphonia in adults. Cochrane Database Syst Rev. 2007;(3):CD006373.
Roy N, Leeper HA. Effects of the manual laryngeal musculoskeletal tension reduction technique as a treatment for functional voice disorders: perceptual and acoustic measures. J Voice. 1993;7(3):242–9.
Roy N, Ford CN, Bless DM. Muscle tension dysphonia and spasmodic dysphonia: the role of manual laryngeal tension reduction in diagnosis and management. Ann Otol Rhinol Laryngol. 1996;105(11):851–6.
Roy N, Bless DM, Heisey D, Ford CN. Manual circumlaryngeal therapy for functional dysphonia: an evaluation of short- and long-term treatment outcomes. J Voice. 1997;11(3):321–31.
Ali MES. Laryngopharyngeal reflux: diagnosis and treatment of a controversial disease. Curr Opin Allergy Clin Immunol. 2008;8(1):28–33.
Ibrahim WH, Gheriani HA, Almohamed AA, Raza T. Paradoxical vocal cord motion disorder: past, present and future. Postgrad Med J. 2007;83(977):164–72.
Halvorsen T, Walsted ES, Bucca C, Bush A, Cantarella G, Friedrich G, et al. Inducible laryngeal obstruction: an official joint European Respiratory Society and European Laryngological Society statement. Eur Respir J. 2017;50(3):1602221.
Morris MJ, Christopher KL. Diagnostic criteria for the classification of vocal cord dysfunction. Chest. 2010;138(5):1213–23.
Lee J, Denton E, Hoy R, Tay TR, Bondarenko J, Hore-Lacy F, et al. Paradoxical vocal fold motion in difficult asthma is associated with dysfunctional breathing and preserved lung function. J Allergy Clin Immunol Pract. 2020;8(7):2256–62.
Koufman JA, Block C. Differential diagnosis of paradoxical vocal fold movement. Am J Speech Lang Pathol. 2008;17(4):327.
Marcinow AM, Thompson J, Chiang T, Forrest LA, Desilva BW. Paradoxical vocal fold motion disorder in the elite athlete: experience at a large division i university. Laryngoscope. 2014;124(6):1425–30.
Forrest LA, Husein T, Husein O. Paradoxical vocal cord motion: classification and treatment. Laryngoscope. 2012;122(4):844–53.
Seear M, Wensley D, West N. How accurate is the diagnosis of exercise induced asthma among Vancouver schoolchildren? Arch Dis Child. 2005;90(9):898–902.
Pasternak K, Thibeault SL. Factors affecting initiation of voice therapy for paradoxical vocal fold motion disorder. J Voice. 2020;34(4):559–66.
Bucca C. Are asthma-like symptoms due to bronchial or extrathoracic airway dysfunction? Lancet. 1995;345(8978):791–5.
Ayres JG, Gabbott PLA. Vocal cord dysfunction and laryngeal hyperresponsiveness: a function of altered autonomic balance? Br Med J. 2002;57(4):284.
Newman KB, Mason UG, Schmaling KB. Clinical features of vocal cord dysfunction. Am J Respir Crit Care Med. 1995;152(4):1382.
Christopher KL, Eckert RC, Blager FB, Raney RA, Souhrada JF. Vocal-cord dysfunction presenting as asthma. N Engl J Med. 1983;308(26):1566.
Brugman SM, Simons SM. Vocal cord dysfunction: don’t mistake it for asthma. Phys Sportsmed. 1998;26(5):63–85.
Morris MJ, Deal LE, Bean DR, Grbach VX, Morgan JA. Vocal cord dysfunction in patients with exertional dyspnea. Chest. 1999;116(6):1676–82.
Guss J, Mirza N. Methacholine challenge testing in the diagnosis of paradoxical vocal fold motion. Laryngoscope. 2006;116(9):1558–61.
Pitchenik AE. Functional laryngeal obstruction relieved by panting. Chest. 1991;100(5):1465–7.
Patel RR, Venediktov R, Schooling T, Wang B. Evidence-based systematic review: effects of speech-language pathology treatment for individuals with paradoxical vocal fold motion. Am J Speech Lang Hear Res. 2015;24(2):1–14.
Weir M. Vocal cord dysfunction mimics asthma and may respond to heliox. Clin Pediatr (Phila). 2002;41(1):37–41.
Morris MJ, Allan PF, Perkins PJ. Vocal cord dysfunction: etiologies and treatment. Clin Pulm Med. 2006;13(2):73–86.
Woisard V, Liu X, Bes MCA, Simonetta-Moreau M. Botulinum toxin injection in laryngeal dyspnea. Eur Arch Otorhinolaryngol. 2017;274(2):909–17.
deSilva B, Crenshaw D, Matrka L, Forrest LA. Vocal fold botulinum toxin injection for refractory paradoxical vocal fold motion disorder. Laryngoscope. 2019;129(4):808–11.
Christopher KL, Morris MJ. Vocal cord dysfunction, paradoxic vocal fold motion, or laryngomalacia? Our understanding requires an interdisciplinary approach. Otolaryngol Clin N Am. 2010;43(1):43–66.
Rameau A, Foltz RS, Wagner K, Zur KB. Multidisciplinary approach to vocal cord dysfunction diagnosis and treatment in one session: a single institutional outcome study. Int J Pediatr Otorhinolaryngol. 2012;76(1):31–5.
Heiser JM, Kahn ML, Schmidt TA. Functional airway obstruction presenting as stridor: a case report and literature review. J Emerg Med. 1990;8(3):285–9.
Aziz Q, Fass R, Gyawali CP, Miwa H, Pandolfino JE, Zerbib F. Esophageal disorders. Gastroenterology. 2016;150(6):1368–79.
Zerbib F, Rommel N, Pandolfino J, Gyawali CP. ESNM/ANMS review. Diagnosis and management of globus sensation: a clinical challenge. Neurogastroenterol Motil. 2020;32(9):1–8.
Ortiz AS, Lawton A, Rives E, Gutierrez G, Dion GR. Correlating videofluoroscopic swallow study findings with subjective globus location. Laryngoscope. 2019;129(2):335–8.
Lee BE, Kim GH. Globus pharyngeus: a review of its etiology, diagnosis and treatment. World J Gastroenterol. 2012;18(20):2462–71.
Tang B, Da CH, Xie HL, Chen DY, Jiang SM, Jia L. Epidemiology of globus symptoms and associated psychological factors in China. J Dig Dis. 2016;17(5):319–24.
Moloy PJ, Charter R. The Globus Symptom. Arch Otolaryngol. 1982;108(11):740.
Josefsson A, Palsson O, Simrén M, Sperber AD, Törnblom H, Whitehead W. Oesophageal symptoms are common and associated with other functional gastrointestinal disorders (FGIDs) in an English-speaking Western population. United Eur Gastroenterol J. 2018;6(10):1461–9.
Timon C, O’Dwyer T, Cagney D, Walsh M. Globus pharyngeus: long-term follow-up and prognostic factors. Ann Otol Rhinol Laryngol. 1991;100:351–4.
Järvenpää P, Arkkila P, Aaltonen LM. Globus pharyngeus: a review of etiology, diagnostics, and treatment. Eur Arch Otorhinolaryngol. 2018;275(8):1945–53.
Vakil NB, Kahrilas PJ, Dodds WJ, Vanagunas A. Absence of an upper esophageal sphincter response to acid reflux. Am J Gastroenterol. 1989;84(6):606–10.
Thompson WG, Heaton KW. Heartburn and globus in apparently healthy people. Can Med Assoc J. 1982;126(1):46–8.
Selleslagh M, Van Oudenhove L, Pauwels A, Tack J, Rommel N. The complexity of globus: a multidisciplinary perspective. Nat Rev Gastroenterol Hepatol. 2014;11(4):220–33.
Van Daele DJ. Esophageal manometry, pH testing, endoscopy, and videofluoroscopy in patients with globus sensation. Laryngoscope. 2020;130(9):2120–5.
Norder Grusell E, Mjörnheim AC, Finizia C, Ruth M, Bergquist H. The diagnostic value of GerdQ in subjects with atypical symptoms of gastro-esophageal reflux disease. Scand J Gastroenterol. 2018;53(10–11):1165–70.
Hill J, Stuart RC, Fung HK, Ng EKW, Cheung FM, Chung SCS, et al. Gastroesophageal reflux, motility disorders, and psychological profiles in the etiology of globus pharyngis. Laryngoscope. 1997;107(10):1373–7.
Tokashiki R, Yamaguchi H, Nakamura K, Suzuki M. Globus sensation caused by gastro epophageal reflux disease. Auris Nasus Larynx. 2002;29(4):347–51.
Cook IJ, Dent J, Collins SM. Upper esophageal sphincter tone and reactivity to stress in patients with a history of globus sensation. Dig Dis Sci. 1989;34(5):672–6.
Deary IJ, Smart A, Wilson JA. Depression and “hassles” in globus pharyngis. Br J Psychiatry. 1992;161(JULY):115–7.
Wilson JA, Deary IJ, Maran AGD. Is globus hystericus? Br J Psychiatry. 1988;153(Sep.):335–9.
Khan M, Saha M, Mamun M, Salam K, Chowdhury M, Hasque M, et al. Upper GIT endoscopic evaluation and psychological state assessment of patients with globus sensation. Mymensingh Med J. 2019;28(2):405–9.
Tang B, Wang X, Chen C, Deng X, Ouyang X, Jia L, et al. The differences in epidemiological and psychological features of globus symptoms between urban and rural Guangzhou, China: a cross-sectional study. Medicine. 2018;97(43):16–8.
Chen CL, Szczesniak MM, Cook IJ. Evidence for oesophageal visceral hypersensitivity and aberrant symptom referral in patients with globus. Neurogastroenterol Motil. 2009;21(11):1142–8.
Wilson JA, Harris MB, Deary IJ. Globus pharyngis: development assessment scale. J Psychosom Res. 1995;39(2):203–13.
The Rome Foundation. Rome IV Diagnostic Criteria. Rome IV Book.
Sanyaolu LN, Jemah A, Stew B, Ingrams DR. The role of transnasal oesophagoscopy in the management of globus pharyngeus and non-progressive dysphagia. Ann R Coll Surg Engl. 2016;98(1):49–52.
Gawron AJ, Rothe J, Fought AJ, Fareeduddin A, Toto E, Boris L, et al. Many patients continue using proton pump inhibitors after negative results from tests for reflux disease. Clin Gastroenterol Hepatol. 2012;10(6):620–5.
Yadlapati R, Ciolino JD, Craft J, Roman S, Pandolfino JE. Trajectory assessment is useful when day-to-day esophageal acid exposure varies in prolonged wireless pH monitoring. Dis Esophagus. 2019;32(3):1–7.
Dworkin JP, Dowdall JR, Kubik M, Thottam PJ, Folbe A. The role of the modified barium swallow study and esophagram in patients with globus sensation. Dysphagia. 2015;30(5):506–10.
Järvenpää P, Ilmarinen T, Geneid A, Pietarinen P, Kinnari TJ, Rihkanen H, et al. Work-up of globus: assessing the benefits of neck ultrasound and videofluorography. Eur Arch Otorhinolaryngol. 2017;274(2):931–7.
Li J, Zhang J, Guo P, Tian S, Li K. Dynamic swallowing study for globus patients. World J Otorhinolaryngol Head Neck Surg. 2016;2(4):198–202.
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJPM, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160–74.
Cybulska EVAM. Globus Hystericus—a somatic symptom of depression ? The role of electroconvulsive therapy and antidepressants. Psychosom Med. 1997;69(10):67–9.
Brown SR, Schwartz JM, Summergrad P, Jenike MA. Globus hystericus syndrome responsive to antidepressants. Am J Psychiatry. 1986;143(7):917–8.
Khalil HS, Bridger MW, Hilton-Pierce VJ. The use of speech therapy in the treatment of globus pharyngeus patients. A randomised controlled trial. Rev Laryngol Otol Rhinol (Bord). 2002;124(4):187–90.
Kristo I, Rieder E, Paireder M, Schwameis K, Jomrich G, Dolak W, et al. Radiofrequency ablation in patients with large cervical heterotopic gastric mucosa and globus sensation: closing the treatment gap. Dig Endosc. 2018;30(2):212–8.
Klare P, Meining A, Von Delius S, Wolf P, Konukiewitz B, Schmid RM, et al. Argon plasma coagulation of gastric inlet patches for the treatment of globus sensation: it is an effective therapy in the long term. Digestion. 2013;88(3):165–71.
Weijenborg PW, de Schepper HS, Smout AJPM, Bredenoord AJ. Effects of antidepressants in patients with functional esophageal disorders or gastroesophageal reflux disease: a systematic review. Clin Gastroenterol Hepatol. 2015;13(2):251–259.e1.
Zhou W-C, Jia L, Chen D-Y, Liu Y, Liu J, Jiang S-M, et al. The effects of paroxetine and amitriptyline on the upper esophageal sphincter (UES) pressure and its natural history in globus pharyngeus. Dig Liver Dis. 2017;49(7):757–63.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
McNeely, B.D., Hu, A. (2023). Functional Disorders of the Larynx: Muscle Tension Dysphonia, Paradoxical Vocal Cord Dysfunction, and Globus Pharyngeus. In: Blakley, B.W., Blakley, J.E. (eds) Functional Illness of the Head and Neck. Springer, Cham. https://doi.org/10.1007/978-3-031-12998-8_18
Download citation
DOI: https://doi.org/10.1007/978-3-031-12998-8_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-12997-1
Online ISBN: 978-3-031-12998-8
eBook Packages: MedicineMedicine (R0)