Abstract
The number of patients with cancer is increasing, resulting in complex disease patterns and multifaceted patient needs. Both the municipal health service and specialist health services face growing challenges. Oncology nursing students must be trained to see situations comprehensively, act when a patient’s situation worsens, and communicate effectively with the patient and the patient’s relatives. Much of this training will take place during the students’ practice studies, but these periods are short, and there are many aspects of nursing for students to focus on. Simulation offers one option for promoting learning in nursing education. Simulation is an effective supplement to traditional lectures in oncology nursing programs, giving students the opportunity to rehearse their skills and learn where they need more practice.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Cancer cases are expected to increase in the next few years. Caring for patients with cancer is becoming more common in acute and critical care settings. In 2020, 35,515 new cases of cancer were registered in Norway [1]. A number of factors may underlie this trend, such as population growth, an increase in the proportion of the elderly, better diagnostics and screening, and an actual increase in the risk of certain types of cancer. Complex disease patterns and complex needs are increasing, resulting in greater challenges for both municipal and specialist health services. Patients who were previously treated in the hospital can now receive advanced treatment and nursing at home. According to the Coordination Reform [2], patients with cancer require a comprehensive health service. Due to the increase in patients with cancer and guidelines from government agencies, health and care services face new challenges. There will be an increased need for professional competence, skills development, and collaboration, and patients will ideally experience a holistic service and a coordinated patient process. Collaboration is important for the patient to receive the optimal care and treatment and for the patient’s relatives to receive adequate support [3].
According to the national cancer strategy “Living with cancer” 2018–2022 [3], Norway will be a pioneer for positive patient outcomes by pursuing the national objectives of more user-oriented cancer care and enhanced cancer prevention. More people will survive and live longer with cancer, and cancer patients and their families will enjoy the best possible quality of life.
2 Objective for Education
There are increasing demands for quality in the municipal and specialist health services, and therefore educational institutions must prepare qualified oncology nurses.
Oncology nurses must be prepared to care for cancer patients of all ages and in all phases of the disease. This means that their education must lead to competence: the oncology nurse must be able to meet cancer patients and their relatives at different stages of navigating the municipal health services and specialist health service and in all phases of their illness. Oncology nursing education consists of theory taught at an educational institution and practice studies in the municipal health service and specialist health service [4]. Oncology nursing focuses not only on pain management but also on safety management, the side effects of chemotherapy, and emergency situations [5]. The oncology nursing student needs training to see situations comprehensively, take action when the patient’s situation worsens, and communicate effectively with the patient and their relatives. The bachelor’s education program in nursing does not have the opportunity to provide in-depth training on nursing for cancer patients. Therefore, additional education is needed to ensure optimal professional competency in oncology nursing. Much of this training will take place during the students’ practice studies, but these periods are short, and there are many aspects of nursing for students to focus on. It can be challenging to combine basic and partly advanced theoretical knowledge with practical knowledge. There is thus a need for educational institutions to develop pedagogical methods that help students combine theory and practice through concrete exercises relevant to patient situations.
3 Simulation in Oncology Nursing
The implications of waning nursing competency and the requirement to deliver safe care have led to the investigation of simulation education modalities. Simulations can assist nurses with knowledge acquisition and the maintenance of oncologic competencies [6]. Self-learning, return demonstration, and skills fairs do not provide the same learning efficacy and competency assessment as simulating via a human patient simulation [7]. Simulation scenarios provide students the opportunity to develop their confidence as they learn to control their fear and panic when faced with clinical emergencies [8].
Since 1950, simulation as a pedagogical method has been used with good results in nursing education [9]. Simulation has proven to be an effective clinical adjunct to hands-on patient care [10]. Simulation can contribute to the conscious use of didactics, which can increase students’ learning [11]. Through simulation, students become more confident in their own profession, retain more information, and achieve a better learning outcome [12, 13]. Learning involves both relevance and realism. It is therefore important that teaching is anchored in practice so that the students experience learning situations that are as relevant as possible [14]. Simulation has proven useful in connection with skills training, decision-making, situation understanding, patient safety, communication training, skills development, teamwork, and management [15,16,17,18]. Through simulation, students can practice situations that require mastery in a safe environment. Through simulations’ attempts to imitate reality, students have the opportunity to recognize themselves in the situation, allowing them to reflect on their own skills and critically analyze their own and others’ actions in a scenario [10]. Participating in simulations can reduce students’ anxiety about current practice situations and provide a good opportunity to use theoretical knowledge and acquire new knowledge [19].
Benner [20] describes how nurses undergo a process of development in their clinical knowledge, progressing from novice to expert. Benner [20] divides this development into five competence levels: novice, advanced beginner, competent, knowledgeable, and expert. Reflection is a prerequisite for students to achieve expert level. The pedagogical basis for simulation is learning through action, which comes from Dewey’s [21] “learning by doing.” It presupposes a learning process characterized by reflection on theoretical and practical knowledge processing [22]. Schön [23, 24] distinguishes between two types of professional reflection: “reflection in action,” where the professional uses a combination of knowledge, experience, and intuition in parallel with action, and “reflection on action,” where the professional reflects on the process and the consequences after the event. These processes pertain to the connection between how the professional thinks and acts. Reflection allows professionals to create new proposals for solutions or gain an understanding of the challenges they face so that the next time they encounter a similar situation, “reflection in action” is triggered. The professional will then be better able to produce the new knowledge or behavior they have planned to use [23, 24].
Simulation requires a combination of learning methods. Students must acquire theoretical knowledge, which is fact-based, through research, theories, models, laws, and rules that form the basis for understanding how and why they should respond in various forms. Furthermore, they must acquire practical knowledge, which means having the necessary skills required to perform nursing. This concrete knowledge is developed through experience and practice. It is also important that students possess ethical knowledge, which means integrating the nursing subject’s values so that ethics are reflected in the nurse’s actions and attitudes. The nurse’s values, attitudes, and views help influence decisions about what should be done or not done. During a simulation, nurses can enter the role they want to have in practice with the patient and can perform a job as realistically as possible. Simulation can prepare the student for developing problem-solving and critical thinking, seeing connections in practice, collaborating in groups, and reflecting on skills.
Simulation aims to prepare students for various situations they will encounter in practice and prevent students from encountering real patient situations without adequate preparation. In addition to action-competent nurses, society demands a greater degree of patient safety. High-fidelity simulation may provide a suitable method for refining important skills. In high-fidelity simulations, students can identify patient needs and perform relevant nursing measures while simultaneously mastering patient treatment and communication with patients, relatives, and other health professionals. Furthermore, students develop the ability to process and relate to new information that they receive during the scenario. In this way, students have the opportunity to practice realistic situations that may arise in practice without exposing actual patients to risk [6, 25].
4 Examples of Scenarios
Simulation scenarios must reflect the learning outcomes and have a clear aim. Simulations should build qualifications and competence around the concepts students should be able to understand or the tasks students must be able to perform.
Administering chemotherapy can be practiced through simulation. Chemotherapy is one of the methods increasingly used to treat cancer. The administration of chemotherapy is a complex task that involves many safety issues due to the narrow safety margin of the cytotoxic medications used in the therapeutic regimen [26]. Chemotherapy medications are classified as high-alert medications due to the potential harm if an error occurs [7].
Communication is another fundamental competency of oncology nurses. It enables them to assess, teach, counsel, question, intervene, and validate the myriad problems that affect patients’ health and care for relatives [27,28,29,30].
Here are some examples of scenarios that are used in further education and master’s program in oncology nursing.
4.1 Patient with an Allergic Reaction to Chemotherapy
Scenario | Linda (40 years old) has breast cancer. Today she will have her first treatment with chemotherapy at the outpatient clinic. She suffers from nausea |
Status start-up: | |
– Blood pressure 120/80 | |
– Pulse 80 | |
– Saturation 98% | |
– Respiratory rate 12 | |
– Temperature 37 °C | |
– Skin color normal | |
– Glasgow coma scale (GCS) awake | |
– Height 165 cm | |
– Weight 70 kg | |
– Pollen allergy | |
Linda works as a nurse. She likes to go hiking and enjoys being out in nature. Linda has a boyfriend, but he is traveling for work | |
Linda does not want to talk; she is nervous and just wants to finish the treatment | |
After Linda receives chemotherapy, her status will change, and she will get worse. She will have an allergic reaction to the chemotherapy. New values during the scenario | |
Learning outcomes | – Observe according to ABCDE methodology and implement relevant measures |
– Recognize symptoms of anaphylactic shock | |
– Communicate systematically with doctor or other personnel based on ISBAR (Identify, Situation, Background, Assessment, and Recommendation) | |
Patient | Manikin (SimMan 3G) and actor/role player |
4.2 Palliative Care to a Patient with Prostate Cancer
Scenario | Magnus (72 years old) was admitted to the hospital 2 days ago, as he has severe pain in his back, hips, and shoulders. Magnus has prostate cancer, and the cancer has spread to the skeleton. Palliative chemotherapy has been started to limit the disease and keep it “in check” if possible |
Status: | |
– Blood pressure 120/60 | |
– Pulse 92 | |
– Saturation 96% | |
– Respiratory rate 14 | |
– Temperature 37.3 °C | |
– Severe pain in the back, hips, and shoulders | |
– Nausea, poor appetite | |
– Dehydrated | |
– Height 182 cm | |
– Weight 61 kg | |
– Blood tests: available during simulation | |
– Medication: available during simulation | |
Magnus is a retired teacher who worked in secondary schools. His wife, Marie, is also retired and worked as an accountant. The couple has three adult children who all have their own families and children. In total, Magnus and Marie have seven grandchildren from 3 to 12 years old. The unity in the family seems good | |
Magnus clearly has great pain as well as nausea, discomfort, and lethargy. The pain is becoming more and more troublesome. He is tired and exhausted. His wife is desperate about the situation | |
Learning outcomes | – Observe according to ABCDE methodology and implement relevant measures |
– Be able to use Edmonton Symptom Assessment System (ESAS) as a tool in mapping the patient’s situation | |
– Inform/talk about planned treatment with patient and relatives | |
Patient | Manikin (SimMan 3G) and actor/role player |
Relatives | Actor/role player |
4.3 A Consultation with a Patient with Colon Cancer and his Next of Kin
Scenario | Daniel (48 years old) has colon cancer which spread to the liver. He is receiving chemotherapy. There is a plan to assess the effectiveness of the cure after cure number 4; today, he will receive cure number 2 |
Daniel works as a bank adviser. He has a wife, Brit, and two children, Tobias (16 years old) and Trine (18 years old). His wife works in a kindergarten. The children have many friends, and both are busy with schoolwork and playing football | |
Daniel is clearly concerned about things being done right. He can be a little restless and asks many questions about whether he is getting the right treatment. He does not settle for the fact that the spread to the liver is inoperable. He is not happy with receiving only chemotherapy | |
He has searched the Internet and looked at various treatments abroad. He and his wife have talked about wanting to try other treatments, but this will be expensive, and they may have to take out a loan to make it happen. He has also found natural medicine that he wants to try. | |
Learning outcomes | – Observe according to ABCDE methodology and implement relevant measures |
– Be able to meet the patient’s need for psychosocial support and care at all stages of the cancer | |
– Have insight into how one’s own values govern actions in encounters with cancer patients and their relatives and be able to reflect on ethical issues and dilemmas | |
Patient | Actor/role player |
Relatives | Actor/role player |
5 Preparation and Implementation of Simulation
The first time the students participate in a simulation, they receive a theoretical review of the simulation as a pedagogical method and tour the simulation center. It is important for instructors to be clear about what is expected of the individual students, and great emphasis is placed on the duty of confidentiality. Prior to the simulation, information from the current literature is posted on a digital learning platform to be reviewed along with a description of the scenario. This ensures that the students gain an understanding of simulation as a pedagogical method and insight into the various practice exercises. Central to the simulation experience is the students’ attainment of mastery. By letting the students know in advance which topics will be the subject of the simulation, they have the opportunity to review the syllabus and think about the situation. Having the opportunity to prepare can increase the feeling of mastery during the simulation. Mastery experiences unlock the mind for learning, while experiences of lacking control can block learning.
Before the simulation, students receive a briefing about the situation they will encounter. They then have some time to prepare mentally, reflect, and get acquainted with the “workplace” environment before the action begins. It is important that students are assigned roles that match their practice; an oncology nursing student does not get the role of a doctor, for instance. Students should be aware of the responsibilities of their role for the simulation to be successful. Therefore, students should not have a role they do not have competence in, and the participants should not play roles different from their actual practice. This would not provide an effective learning situation.
Some students feel uncomfortable during simulations. They have no control over the situation, and insecurity characterizes the activity [6]. When an educational program carries out simulations, it is usually two students who participate. When two students work together, it provides safety for the students, as they are not alone in the situation. It is important to focus on the students’ learning and ensure that the students experience mastery in the situation. Students who do not participate in the simulation have the role of observers and are given the task of observing their respective learning outcomes. The actual scenario takes 10–40 min, depending on how the scenario develops.
Debriefing is an important aspect of simulation as a pedagogical method. One of the facilitators’ tasks is to build a bridge between simulation and practice in the debriefing, as it is through the reflections that the students learn [11]. During the debriefing, the students’ critical reflections on their own behavior are highlighted. If the debriefing is to be able to promote student reflection, it is important that the facilitator structures the debriefing so that the reflection is meaningful [11].
Debriefing methods used in simulation in nurse education can vary widely, and there are many different debriefing methods. According to Steinwachs [31], debriefing takes place in three phases. The first is the description phase, in which the students describe what happened without interpretations so that everyone can identify the action. Next comes the analysis phase, in which the predefined learning outcomes govern the professional reflection that takes place. The students who were active in the scenario describe two or three things that they did well and justify their assertions. Then they have the opportunity to reflect on what they could do differently if they encountered a similar situation in practice. Finally, the observers are given the opportunity to explain what they thought was done well and what could have been done differently based on the learning outcomes. During the final phase, the application phase, each student reflects on how they will utilize this experience to improve their knowledge and skills. The utilization of high-fidelity simulations in nursing has been shown to increase learner knowledge, self-confidence, satisfaction, and self-efficacy in managing critical oncologic infusion emergencies [26].
6 Experiences and Feedback from the Students
In the bachelor’s education in nursing program, there is rarely much focus on teaching oncological content. This represents a missed opportunity for students who intend to study oncology nursing, as they have little knowledge of the field before they start their studies. There are many areas where the oncology nurse must have expertise. The competent oncology nurse can effectively manage the complex cancer patient, their disease process, modalities of cancer treatment, multidisciplinary care teams, and the patient’s psychosocial and symptom management [4].
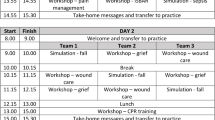
According to the education program, simulation and skills training create commitment and active students while at the same time allowing them to face a variety of situations and practice competence [32]. Some students who participated in simulations became more active, and this may be because they felt secure in what they were supposed to do. Some students felt some pressure at first, dreading to expose themselves academically and personally to fellow students. On the feedback after the simulation, it emerged that these students were very engaged by the simulation situation and that they eventually forgot those who were observers. In one example, the situation with the patient and relatives became the focus [32]. Experience so far suggests that the educational program sees the importance of offering an arrangement to students that provides the opportunity to acquire competence by practicing real situations [32]. The debriefing increases the learning effect, and reflection creates space for discussion, questions, sharing experiences, improving actions, and processing experiences. Feedback from the students after the simulation was unanimous that it was very useful. The students want more time for simulations [32]. During the further education and master’s program in oncology nursing, several days of simulation, skills training, and other exercises will be implemented.
7 More Focus on Oncology Nursing for Children and Collaboration
In Norway, the incidence of cancer in children and young people has been stable for the past 40 years. There are approximately 140 new cases annually in the age group 0–15 years [3]. Globally, more than 300,000 children are diagnosed with cancer each year [33], and according to the National Cancer Institute [34], the incidence of childhood cancer has improved over the past 40 years. Oncology nursing students have little knowledge of nursing for children from their previous education, and this is something the education program wants to strengthen in the coming years in further education and master’s program in oncology nursing. Treatment for cancer in children includes chemotherapy, radiation therapy, and/or surgery [35]. Nurses lack training and confidence in caring for pediatric oncology patients [36], and simulation is well suited for helping nurses acquire knowledge and training in caring for children.
A large increase in the number of patients living with cancer and who have undergone cancer treatment is also expected in the future. Some of these patients will continue to require significant health and care services. This increase will place great demands on capacity and competence in the specialist health service and in the municipal health and care service. There are increasing demands for collaboration between hospitals and between the specialist health service and the municipal health service. Patients’ complex needs must be managed in a coordinated and competent way while ensuring as much home time as possible for the patients [3]. Further education and master’s program in oncology nursing must have a greater focus on collaboration, and health services must be coordinated so that the patient and their family experience security and continuity. Simulation can be a well-suited method for such training, provided that roles and expectations for each participant are clear.
8 Conclusion
Simulation as a pedagogical method in further education and master’s program in oncology nursing is an effective learning activity to achieve desired learning outcomes. The challenges nurses will face through their work are significant. By having the opportunity to practice in different situations, they will gain a feeling of safety, greater room for flexibility, and better-quality education. Oncology nurses work in hospitals, home health care, home nursing, and other institutions. They are often faced with situations that must be handled independently, and it is therefore important that they have the knowledge and skills to solve problems and complete tasks. This is important for both quality assurance and patient safety. Simulation as a pedagogical method is suitable and effective, as it stimulates engagement and curiosity among students in the field of practice and with colleagues. Simulation helps oncology nursing students train from simple to more advanced procedures, and it ensures that patient safety is given priority by training within a safe framework that does not expose the patient to risk.
References
Cancer Registry of Norway. Cancer in Norway 2020—cancer incidence, mortality, survival and prevalence in Norway. Oslo: Cancer Registry of Norway; 2021.
Report No. 47 (2008-2009) to the Storting. The coordination reform. Proper treatment—at the right place and right time. Oslo: Norwegian Ministry of Health and Care Services; 2009.
Ministry of Health and Care Services. Leve med kreft. Nasjonal kreftstrategi (2018-2022) (Living with cancer. National cancer strategy (2018-2022)). Oslo: Ministry of Health and Care Services; 2018.
Ministry of Education and Research. Rammeplan for videreutdanning i kreftsykepleie (Curriculum for further education in oncology nursing). Oslo: Ministry of Education and Research; 2005.
Campbell P, Torrens C, Kelly D, Charalambous A, Domenech-Climent N, Nohavova I, Östlund U, Patiraki E, Salisbury D, Sharp L, Wiseman T, Oldenmenger W, Wells M. Recognizing European cancer nursing: protocol for a systematic review and meta-analysis of the evidence of effectiveness and value of cancer nursing. J Adv Nurs. 2017;73:3144–53. https://doi.org/10.1111/jan.13392.
Simmers PC. Simulation as a learning tool in the oncology setting. J Adv Pract Oncol. 2014;5:217–33. https://doi.org/10.6004/jadpro.2014.5.3.7.
Crannell C. Chemotherapy administration: using simulation case-based scenarios to assess chemotherapy competency. Oncol Nurs Forum. 2012;39:19–22. https://doi.org/10.1188/12.onf.19-22.
Perry P. Concept analysis: confidence/self-confidence. Nurs Forum. 2011;46:218–30. https://doi.org/10.1111/j.1744-6198.2011.00230.x.
Morrison AM, Catanzaro AM. High-fidelity simulation and emergency preparedness. Public Health Nurs. 2010;27:164–73. https://doi.org/10.1111/j.1525-1446.2010.00838.x.
Jeffries PR. Simulation in nursing education. From conceptualization to evaluation. New York: National League for Nursing; 2012.
Husebø SE, Dieckmann P, Rystedt H, Søreide E, Friberg F. The relationship between facilitators’ questions and the level of reflection in postsimulation debriefing. Simul Healthc. 2013;8:135–42. https://doi.org/10.1097/sih.0b013e31827cbb5c.
Mikkelsen J, Reime MH, Harris AK. Nursing student’s learning of managing cross-infections-scenario-based simulation training versus study groups. Nurse Educ Today. 2008;28:664–71. https://doi.org/10.1016/j.nedt.2007.11.003.
Reime MH, Harris AK, Aksnes J, Mikkelsen J. The most successful method in teaching nursing students infection control—E-learning or lecture? Nurse Educ Today. 2008;28:798–806. https://doi.org/10.1016/j.nedt.2008.03.005.
Benner P, Sutphen M, Leonard V, Day L. Educating nurses: a call for radical transformation. San Francisco: Jossey-Bass; 2010.
Aase K. Pasientsikkerhet – teori og praksis i helsevesenet (Patient safety—theory and practice in the health care system). Oslo: Universitetsforlaget; 2010.
Alessi SM, Trollip SR. Multimedia for learning. Methods and development. 3rd ed. Massachusetts: Allyn and Bacon; 2001.
Brinchmann-Hansen Å, Wisborg T, Brattebø G. Simulering – en god metode i legers videre- og etterutdanning (Simulation—a good method in doctors’ further and continuing education). Tidsskr Nor Laegeforen. 2004;124:2113–5.
Marshall DA, Manus DA. A team training program using human factors to enhance patient safety. AORN J. 2007;86:994–1011. https://doi.org/10.1016/j.aorn.2007.11.026.
Phillips J, Grant JS, Milligan GW, Moss J. Using a multicultural family simulation in public health nursing education. Clin Simul Nurs. 2012;8:187–91. https://doi.org/10.1016/j.ecns.2011.08.007.
Benner P. From novice to expert: excellence and power in clinical nursing practice. Menlo Park, CA: Addison-Wesley; 1984.
Dewey J. How we think. A restatement of relation of reflective thinking to the educative process. Boston: Health & Co; 1933.
Molnes SI, Hunstad I. Kan simulering forberede studentene til praksis? (Can simulation prepare students for practice?). Psykisk helse og rus. 2014;1:26–9.
Schön DA. The reflective practitioner: how professionals think in action. New York: Basic Books; 1983.
Schön DA. Educating the reflective practitioner. San Francisco: Jossey-Bass Publishers; 1987.
Arafeh JMR, Snyder Hansen S, Nichols A. Debriefing in simulated-based learning: facilitating a reflective discussion. J Perinat Neonatal Nurs. 2010;24:302–9. https://doi.org/10.1097/jpn.0b013e3181f6b5ec.
Sharour LA. Implementing simulation in oncology emergencies education: a quasi-experimental design. Technol Health Care. 2019;24:223–32. https://doi.org/10.3233/THC-181543.
Erickson J. Bedside nurse involvement in end-of-life decision making: a brief review of the literature. Dimens Crit Care Nurs. 2013;32:65–8. https://doi.org/10.1097/DCC.0b013e318280833b.
Fox M. Improving communication with patients and families in the intensive care unit: palliative care strategies for the intensive care unit nurse. J Hospice Palliat Nurs. 2014;16:93–8. https://doi.org/10.1097/NJH.0000000000000026.
Strang S, Henoch I, Danielson E, Browall M, Melin-Johansson C. Communication about existential issues with patients close to death—nurses’ reflections on content, process and meaning. Psychooncology. 2013;23:562–8. https://doi.org/10.1002/pon.3456.
Thorne S, Oliffe JL, Stajduhar KI, Oglov V, Kim-Sing C, Hislop TG. Poor communication in cancer care: patient perspectives on what it is and what to do about it. Cancer Nurs. 2013;36:445–53. https://doi.org/10.1097/NCC.0b013e31827eeda4.
Steinwachs B. How to facilitate a debriefing. Simul Gaming. 1992;23:186–95. https://doi.org/10.1177/1046878192232006.
Molnes SI, Brenne IHR. Simulering gir bedre ferdigheter (Simulation provides better skills). Kreftsykepleie. 2013;2:10–4.
American Childhood Cancer Organization. United States childhood cancer statistics. 2020. https://www.acco.org/us-childhood-cancer-statistics/.
National Cancer Institute. Age-adjusted surveillance epidemiology, and end results program cancer incidence rates, 1975-2015, ages 0-19. 2020. https://seer.cancer.gov/csr/1975_2015/browse_csr.php?sectionSEL¼28&pageSEL¼sect_28_table.02#table2.
Alcoser PW, Rodgers C. Treatment strategies in childhood cancer. J Pediatr Nurs. 2003;18:103–12. https://doi.org/10.1053/jpdn.2003.10.
Helt J, Gilmer MJ, Connors L. Clinical simulation training in nurses caring for pediatric oncology patients. Clin Simul Nurs. 2020;47:73–81. https://doi.org/10.1016/j.ecns.2020.06.001.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Molnes, S.I. (2023). Facilitating Learning Activities in Further Education and Master’s Program in Oncology Nursing. In: Akselbo, I., Aune, I. (eds) How Can we Use Simulation to Improve Competencies in Nursing?. Springer, Cham. https://doi.org/10.1007/978-3-031-10399-5_3
Download citation
DOI: https://doi.org/10.1007/978-3-031-10399-5_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-10398-8
Online ISBN: 978-3-031-10399-5
eBook Packages: MedicineMedicine (R0)