Abstract
In most countries, including the Netherlands, decision-making about the COVID-19 policy measures was initially based on medical information, and only later did it also include insights from social sciences. However, ethical implications of COVID-19 policy measures have not frequently been explicitly considered. As a result, critical ethical issues have been overlooked, and values, concerns, and emotions have not been considered appropriately. In this chapter, I will argue that emotions can help to make important moral dilemmas around decision-making about COVID-19 explicit and to make ethically justified decisions. I will do so by zooming in specifically on how the Netherlands has handled the pandemic so far. My discussion aims to contribute to morally better and more socially acceptable decision-making about the challenges that COVID-19 poses, as well as to hopefully learn lessons for possible future pandemics.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
1 Introduction
A Chinese colleague said in early March 2020: “My Chinese friends and I are very concerned. We have seen what happened in China. This is not just any virus. We don’t understand that Western countries do not take stricter measures.” In the beginning of the COVID-19 pandemic, many people in Western countries, including politicians, took pride in publicly stating that they were not worried about the Sars-Cov-2 virus. For example, Dutch prime minister Mark Rutte insisted to shake hands with a journalist when asked about safety measures concerning social distancing. In various respects, the Netherlands were late in introducing measures that were already urgently recommend by the WHO (NOS, 2021d). Likewise, some virologists assured the public that COVID-19 was nothing more than just another flu virus from which they could not get sick because only people with vulnerable health conditions were susceptible. Potential worries were explained away. For example, in February 2020, in pieces for major news outlets, psychologists Paul Slovic and Daniel Kahneman as well as legal scholar Cass Sunstein claimed that supposedly exaggerated reactions to the COVID-19 virus could be elucidated by an opposition between reason and emotions. They argued that people’s perception of risk is driven by ‘irrational’ emotions based on which people close themselves off from scientific facts (Fisher, 2020; Sunstein, 2020). Slovic and Sunstein stated that worries about COVID-19 could be readily explained via this framework. A few weeks later, almost the whole world went into lockdown, but it was already too late to stop this supposedly harmless virus, the pandemic was a fact, and the rest is history.
If these experts and politicians were wrong in their initial assessment of the virus, could they also be wrong about their dismissal of emotional responses that did highlight concerns about the virus at an early stage? And could we learn important lessons from this, leading to more appreciation of emotions and underlying ethical values and concerns? This is the idea I will pursue in this chapter.
2 COVID-19 and Emotions
In his initial speeches about COVID-19 policy, Dutch Prime Minister Mark Rutte repeatedly emphasized the importance of listening exclusively to medical-scientific experts, particularly the virologists and modellers of the National Institute for Environmental Studies (RIVM) and the Outbreak Management Team (OMT). He explicitly said that we should not listen to historians and lawyers, for example, and that we should not “philosophize”. Closing the schools in mid-March 2020 wouldn’t have been scientifically necessary, but here people have “voted with their feet” (NOS, 2020). Interestingly, a few weeks later, Rutte mentioned that he had been pondering on “dilemmas”. However, he still explicitly stated that he would only listen to medical and virological advice, thereby dismissing possible expertise on addressing dilemmas, such as from philosophers and social scientists.
Notably, many people were (and still are) worried because of the impact that policies may have on public health, the economy, and the way of life people are used to. Some are concerned whether it is responsible to send their children to school or to go outside without a mask. Others are angry because they perceive the measures as too strict and because their income is at stake. Until vaccines were available in early 2021, many older people in care homes languished in loneliness during various lockdowns because their loved ones were not allowed to visit. The question is how policy makers and politicians should deal with such emotions and worries, and how philosophical research may shed light on this. In this chapter, I will argue that emotions such as empathy and compassion, as well as resentment and concern, can help to make critical moral dilemmas explicit and thereby contribute to taking moral considerations into account when policy decisions are made about virus-restriction measures.
Obviously, it is crucial to uncover the relevant scientific facts to make important decisions on dealing with a pandemic. But I will argue in this chapter that addressing the COVID-19 crisis and making decisions about trade-offs between different risks is not just a matter of gathering scientific information and listening to scientists, as crucial as that is. Scientific information is necessary to make assessments and policy decisions in such a crisis situation, but not sufficient. We also have to take into account societal and ethical considerations, which requires explicit ethical reflection and attending to emotions. This argument is grounded in my philosophical approach, according to which emotions can play an important role in ethical reflection (e.g. Roeser, 2011, 2018).
My ideas go against the dominant scientific and political approaches to risk and emotion. As mentioned above, scholars such as Paul Slovic (2010), Cass Sunstein (2005) and Nobel Prize winner Daniel Kahneman (2011) think that all kinds of misunderstandings about risks and statistics can be explained by a contradiction between reason and emotion, so-called ‘Dual Process Theory’ (DPT). According to DPT, we process information via two distinct systems, “system 1” versus “system 2”. System 1 is said to be based on emotion and intuition, and while fast, it is unreliable. System 2 is based on rationality and analytical thinking. System 2 is slower but much more reliable than system 1. According to Kahneman, Slovic, Sunstein, and other psychologists and decision theorists, all kinds of misunderstandings about risks and statistics can supposedly be explained by this: people respond emotionally in their risk perceptions (system 1) and therefore close themselves off to scientific facts (which require system 2 processes).
However, many emotion researchers from psychology and philosophy reject the reason-emotion dichotomy that underlies Dual Process Theory. Instead, they have developed so-called cognitive theories of emotions. The renowned Dutch psychologist Nico Frijda (Frijda, 1986) considered emotions crucial for our appraisals and actions. Philosophers Robert Solomon (1993), Martha Nussbaum (2001) and Bob Roberts (2003) have argued for the importance of emotions for our moral thinking. The neuropsychologist Antonio Damasio (1994) has shown that people who seize to have emotions due to specific brain damage can no longer make practical and moral decisions. These ideas give us a very different and much richer understanding of emotions: emotions are not by definition at odds with rationality as dualistic views of emotion and rationality, such as DPT, entail. Rather, emotions can be an important source of moral reflection and deliberation (Roeser, 2011; Furtak, 2018). Emotions can point to what morally matters. Of course, emotions can also be misguided, but that holds for all our sources of insight. Instead of dismissing emotions, we should see them as an important source of ethical reflection in the context of risks. Emotions can draw attention to important ethical considerations that are frequently overlooked in quantitative, STEM-based approaches to assessing risks. Emotions such as sympathy, compassion, care, and feelings of responsibility can highlight ethical concerns such as justice, fairness, and autonomy. In my previous work, I have argued that these ideas can shed a different light on the role of emotions in decision making about risks, primarily in the context of technological risks (Roeser, 2018). In the remainder of this chapter, I will apply these insights to decision making about COVID-19.
3 COVID-19, Risks, Uncertainty, Complexity, and Ethics
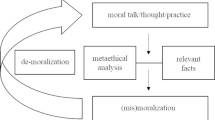
The dominant approaches to decision making about risk view emotions as a source of irrationality. A standard approach to decision making about risks is, therefore, to rely solely on scientific expertise. This is what I would call the “technocratic approach”; quantitative information is guiding, public concerns are dismissed as irrelevant. A common alternative strategy is what I call the “populist approach”; here, the public’s will is seen as leading. Even if the public’s will is attributed to supposedly irrational emotions, it is still followed, either for seemingly democratic or pragmatic (instrumental) reasons to avoid public opposition (cf. e.g. Loewenstein et al., 2001, De Hollander & Hanemaaijer, 2003). However, both approaches fall short because they do not take emotions and underlying values seriously. In neither approach is there a genuine dialogue and deliberation about the values that are at stake (Roeser, 2018). Technocratic risk approaches rely solely on descriptive information and consequentialist methods such as risk-cost-benefit analysis. But such approaches contain implicit and often problematic value judgments. Only net impacts at a high level of aggregation are considered, and often only a limited type of impact, such as the number of deaths. For example, issues such as justice, fairness and autonomy are usually overlooked in such approaches, as are long-term consequences for health and (psychological) well-being (cf. Roeser, 2006; Asveld & Roeser, 2009). Let us begin by zooming in on the ethical intricacies of decision making under risk and uncertainty. After this, in the following section, I will argue that policy measures to combat COVID-19 are intrinsically value-laden. I will then proceed to explore how emotions can contribute to highlighting these ethical issues.
As mentioned above, at various crucial moments, the Dutch government explicitly stated that they would follow the technocratic approach by directly acting on the advice of the STEM-based RIVM and OMT. It can be argued that it is not the task of such STEM-based policy organizations to include ethical considerations in their recommendations. STEM-based approaches are limited to discerning the facts relating to the transition of COVID-19. However, this means that there is an important, unaccounted for ‘is-ought gap’Footnote 1 between descriptive STEM data and policy decisions, which also have important normative dimensions. One could solve this by having the following separate steps: first, gather the descriptive information, and then have an intermediate step of ethics evaluation before policymakers make decisions based on both steps. However, things are even more complicated: descriptive research also involves normative assumptions, e.g. concerning how to measure, assess and compare data, specifically in the context of risk and uncertainty (Roeser et al., 2012). To account for these issues, even STEM-based councils should include social science experts (to account for the impact and role of society) as well as ethicists to point out implicit ethical and other normative assumptions, highlight ethical dilemmas, and provide for explication of ethical considerations to make these transparent and object of critical deliberation by policymakers and societal stakeholders. This is the case with various governmental advisory boards in the Netherlands, e.g. at the COGEM (committee on genetic modification), as well as the Dutch Health Council, which also provides advice concerning e.g. COVID vaccinations. Ethicists have also been involved in the development of COVID-19 track-and-trace apps. Despite this, ethicists have not yet been involved in decision making on the policy measures, even though these measures include many pressing ethical considerations. This means that these ethical considerations have either been ignored, not made explicit, or dealt with haphazardly without consulting ethics experts’ relevant expertise. This is not to say that ethicists should have the final word on such vital issues. Still, they could play an important role in explicating ethical considerations and highlighting potentially ethically problematic decisions. I will illustrate this in what follows by discussing various aspects of Dutch COVID-19 policies.
There are methodological issues of risk, uncertainty, and complexity that give rise to ethical issues. The measures policy makers implement directly impact the development of the pandemic. Furthermore, numerous actors are involved, and the virus may develop in unforeseen ways, with scientific knowledge lagging behind. This can lead to complex interaction effects, high uncertainty, and a lack of predictability. As pointed out by the critical ‘Red Team’, COVID-19 should be seen as a case of complexity, requiring different decision-making approaches than conventional, more predictive types of risk. The Red Team was an interdisciplinary team of Dutch scientists (from STEM as well as the social sciences) that criticized the approach of the Dutch government to deal with the pandemic. In 2020, the Red Team strongly influenced Dutch public opinion via social media, as well as being consulted at certain stages of the pandemic by the government. However, they were silent for most of 2021. They recently announced that they had decided to stop working altogether, as their advice was largely ignored and was fundamentally at odds with the strategy of the Dutch government. The Red Team advised to keep infection rates low via early lockdown measures and tracking and tracing. In direct contrast, the Dutch government has from the beginning followed a strategy that primarily steers at preventing the health care sector from getting overburdened, in the meantime being reluctant to employ safety measures.
In recent reports, it has been argued that the initial Dutch, UK, and Swedish approaches to strive for so-called heard immunity were irresponsible, infeasible from the start, and eventually led to thousands of unnecessary deaths. Interestingly, the Dutch government later denied having had such a strategy. Instead, they claimed that they only wanted to achieve herd immunity as a side effect, not as a goal in itself. However, publicly available information such as press communications from the early days of the pandemic as well as internal documentation clearly shows that this was the initial strategy in the Netherlands (cf. NOS, 2021a, b, c). Such wavering communications obviously do not contribute to public trust, which is already a delicate issue given the controversies about different COVID-measures and the various other scandals that the Dutch government and political institutions are currently involved in.Footnote 2
Ethical decision-making about risks presents us with different challenges than ethical decision-making about options where the outcomes are easily predictable or even fixed, as argued by the Swedish risk ethicist Sven Ove Hansson (2009). Hansson has argued that there is a significant ethical difference between so-called “type-1” errors and “type-2” errors, i.e. false positives versus false negatives. In scientific research, we aim to prevent false positives, that is, false claims that something is the case. But in the context of, for example, policy making about health risks, we want to avoid false negatives, that is, false claims that people are safe while they are at risk. This is based on an ethical consideration, namely that it is prudent to be cautious when dealing with health effects for human beings, in other words that we would rather be safe than sorry. In the context of a pandemic, this can support following the precautionary principle: we don’t know how the contagion curve will play out, so it is better to intervene early and be extremely cautious, rather than reach a point where it’s too late to prevent disastrous consequences.
For example, the Dutch RIVM had to adjust previous information: initially, it said that Sars-Cov-19 would not be a dangerous virus, not much more than the normal flu. Furthermore, the RIVM initially stated that Sars-Cov-19 could only be spread by people who have symptoms, and therefore not by children as they hardly get sick from COVID-19; they furthermore maintained that aerosols do not play an important role in the spreading of this virus, and that face masks are unnecessary. We now know that all of these claims are wrong. Interestingly, the RIVM and OMT maintained these claims for many months, even in the light of countervailing evidence from other countries, as well as the WHO. Presumably, the OMT and RIVM held on to very high scientific standards concerning sufficient evidence about these matters: as long as it is not entirely clear that these hypotheses are true, they are rejected in order to avoid false positives. As was discussed above, while these are important standards in the context of scientific research, they may not be suitable in the context of public health measures where prevention can also be an important concern, and these standards may not be responsive enough in an urgent crisis. In the words of World Health Organization health emergencies programme executive director Dr. Mike Ryan from 14 March 2020 [sic]:
Perfection is the enemy of the good when it comes to emergency management. Speed trumps perfection, and the problem in society we have at the moment is everyone is afraid of making a mistake – everyone is afraid of the consequence of error. But the greatest error is not to move. The greatest error is to be paralyzed by the fear of failure (WHO, 2020).
A precautionary approach could have involved a ‘what if’ exercise at an earlier stage: let’s assume the worst and start planning how to deal with this situation. Communicating the difficulties of dealing with uncertain information and complex developments can also help, much more than downplaying these difficulties and claiming certainty. Downplaying uncertainty can easily backfire when things turn out differently (cf. Van Asselt & Vos, 2006), as this will lead to distrust. Striving for certainty cannot always be a priority in situations that are intrinsically uncertain and highly complex, while stakes are high and urgent decision making is needed. As I will discuss in Sect. 11.5, emotions such as compassion and care can highlight important ethical considerations, such as precaution. But first in the following section I will zoom in in more detail on the value-ladenness of COVID-19 policy measures.
4 The Value-Ladenness of COVID-19 Policy Measures
The previous discussion highlights that decision-making about possible COVID-19 precautions and their intended positive and negative effects requires ethical reflection. I will now zoom in in more detail on various policy options, by highlighting that they involve important values that need to be deliberated on. In Sect. 11.5 I will then argue that emotions can play an important role in such a deliberation.
In schematic terms, the following COVID-19 strategies can be distinguished. Each comes with underlying assumptions about values and ethical implications:
-
Laissez faire: herd immunity
Business as usual for everyone, but substantial health risks, especially for vulnerable people.
-
(Partial) lockdown:
Everyone affected in terms of secondary health effects and limitation of civil liberties, partial containment of the virus, uncertain evidence about how the virus spreads.
-
Containment: intensive testing and selective quarantine:
Containment of virus, low number of deaths and shorter lockdown, but sophisticated testing, monitoring, and health infrastructure needed; civil liberties restrained.
In the early stages of the pandemic, different countries chose various strategies. They also switched or mixed aspects of these strategies, depending on developments of the pandemic as well as on other societal factors. This is because the development of the pandemic does not just rely on virological issues; it also depends on socio-political and behavioural issues. This means that it requires insight of impacts of behaviour and strategies, as well as reflection on the significant ethical implications of these strategies, by explicating underlying values.
It is crucial to explicitly face the question of how to evaluate different scenarios on how to respond to the COVID-19 crisis. This involves considering available alternatives and their respective advantages and disadvantages, each of which requires ethical reflection. Which values are at stake? How can we assess, compare, and weigh them? Values such as the inconvenience and drastic consequences of social distancing must be weighed against values such as protecting public health and containing a pandemic promptly. This relates to the ethical question as to how to balance direct versus indirect health effects. An example of direct health effects is the need to protect people who are vulnerable to infections. An example of indirect health effects is the need to mitigate the consequences of lockdowns for those who are disproportionally vulnerable to them (e.g. children, young people, people working in the hospitality and cultural sectors).
In any case, those most vulnerable in society will be disproportionally most exposed to the risks of a pandemic. People without health insurance, a steady income, and proper housing are more exposed, for example. These people have fewer means available to ameliorate the impacts of exposure to the virus or lockdown measures than wealthy people and citizens of affluent countries with well-functioning and accessible public health services. The social disruption of a lockdown, for example, is much more profound in a society that does not have a robust social safety net. In a society with such facilities, people whose jobs are at risk due to social distancing policies have better protection, and society’s implications will be less disastrous. Finally, the existing political and socio-economic infrastructure in a society is based on ethical considerations. These contextual features need to be considered when ethically evaluating scenarios on how to deal with this and future pandemics.
Furthermore, is increasing herd immunity ethically acceptable if it means that some people will end up in intensive care units when they would not have gotten sick under stricter measures? Given the (specifically in the early stages of the pandemic) uncertain knowledge surrounding the possible immunity against the SARS-Cov-2 virus, can it be ethically defended to make such an assumption? How to deal with ‘triage’, that is, how to compare the need for ICU treatment of different patients? In the Netherlands, Covid-19 patients with urgent health care needs are prioritized above other patients who are waiting for non-emergency surgery, and COVID-19 patients stay significantly longer in ICU units than other patients. This means that increasing hospitalization of COVID-19 patients has significant health effects for people with other, less urgent but also eventually life-threatening conditions.
Fundamental and difficult, if not impossible to answer, ethical questions such as ‘what is the value of a human life?’ are at stake here. Do we opt for a consequentialist approach to assign a monetary value to human lives, while also allowing human lives to be traded off against each other and other monetized considerations? Or are human lives of intrinsic value, meaning that they cannot be put into a simple equation? The latter seems to be a rhetorical question. From an emotional point of view, we experience the life of a loved one, for example, as infinitely valuable. Deontological approaches in ethics seem to fit better with this insight because they say that we should not use people merely as a means. On the other hand, it is evident that government policies need to balance deontological and consequentialist considerations.
Furthermore, there are ethical questions related to civil liberties, freedom of choice and privacy. Several countries have adopted measures requiring COVID-19 passes, showing that citizens are ‘safe’ if they have been: (1) fully vaccinated, (2) recovered from COVID-19, or (3) recently tested negative. The privacy of citizens is preserved to a significant degree by not needing to show which of the three criteria they meet. Others see this as a disproportionally restrictive measure, which is unsuited for a liberal society. However, respecting people’s freedom of choice here comes at the price that vulnerable people – e.g. those who have immune deficiencies and therefore have no or limited choice – are less protected. Even though freedom of choice is of vital importance in a liberal society, we always have to make concessions and trade-offs between individual liberties and societal concerns, i.e. the liberty, safety, and health of other people. Safety measures may provide a reasonable trade-off, such as wearing masks and COVID passes.
A crucial issue is that between distributive and procedural justice. While from a distributive justice perspective, it seems fair to have such preventive measures, from a procedural point of view it is essential to have fair means of decision-making that are also experienced as such. Politicians could convey more explicitly that in their decisions, they also take into count ethical and societal concerns and engage with the views of societal stakeholders before making – often complicated – decisions that require trading off or balancing important values. Doing this may have the effect of showing the public the complex value trade-offs that are required in a public health crisis. Such transparency can help the public to see that the decision making was complicated but fair. Making the difficult moral dilemmas and trade-offs explicit as well as reminding people of the responsibilities towards others that come with individual liberties, and appealing to solidarity, can make an important contribution in public deliberation and support for measures. However, these important moral arguments have only rarely been made explicitly by politicians in the Netherlands and other countries.
5 The Importance of Emotions
In the previous sections, I have discussed the ethical intricacies of risk assessments and the value-ladenness of COVID-policy measures. The technocratic approach that politicians have primarily used does not suffice to address these issues, but neither would a populist approach be a solution. As mentioned above, populist approaches merely follow the dominant view in society at a particular moment, rather than explicitly addressing the concerns and values at stake. This avoids the problematic ethical deliberations that are sorely needed. Emotions such as compassion, feelings of responsibility, and care can help highlight these ethical aspects. More generally, emotions such as sympathy, empathy, and indignation can play an important role in alerting us to ethically relevant aspects of risks. These and other emotions are at stake within the public at large. Addressing these emotions in explicit ethical deliberation would mean that ethical concerns of the public could be seriously addressed, rather than waved off as in the technocratic approach, or superficially followed without further reflection as in the populist approach, leading to wavering and inconsistent policies.
When thinking about COVID-19 measures, the emotions of diverse stakeholders could therefore play an essential role in highlighting ethical issues and doing justice to important values. The emotions in society can be an essential source of moral insights; indeed, some of the ethical considerations I have mentioned have also been raised by concerned citizens. But, of course, emotions can also be misleading, like all our sources of insight. Emotions can unnecessarily inflate risks, letting them appear overly frightening. At the same time, emotions can make us overlook latent dangers. Intense emotions can magnify our own suffering and thereby ignore the suffering of others (Steinert & Roeser, 2020). This means that emotions must be critically assessed based on scientific information and ethical reflection. But emotions themselves can also play an important role in the latter. Elsewhere, I call this ‘emotional deliberation’ (Roeser & Pesch, 2016, Roeser, 2018). Furthermore, people’s emotions and ethical evaluations can diverge. But rather than eschewing deliberation about these emotions and values, we should engage with them. Such diverging emotions and values can highlight different horns of the complex dilemmas we face. For example, should we require vaccination, e.g. for people working in the care professions or teaching settings or even for all occupations where people interact with each other? Or should we respect people’s free choice? But what if that comes at a high price for other members of society, such as people with immune conditions, or those whose medical treatment is getting postponed because of overfull hospitals, or because, say, of secondary health effects due to lockdowns? These are intricate ethical dilemmas, and different stakeholders in society have different views on the best ways to address these. There are, by definition, no easy solutions to moral dilemmas. Instead, they require deliberation, exchange of viewpoints, arguments and experiences to hopefully come to solutions that are acceptable to a broad range of stakeholders. For example, emotions such as a sense of responsibility and concern for others can contribute to putting one’s suffering in perspective and being open to policy options that can contribute to the well-being of others. Furthermore, compassion can help understand the suffering of an individual victim, which can disappear in a cold, consequentialist calculation. Opening up deliberation to such concerns can also overcome seemingly unavoidable trade-offs and open new perspectives, by learning from each other and encouraging creative solutions. This can help devise innovative strategies that do justice to public health, economic resilience, and an ecologically sustainable society at the same time.
One might worry that including ethical deliberation and emotional concerns would delay decision making when quick responses are needed. However, there can be explicit ethical deliberation under time pressure, as well as more extensive ethical deliberation, involving stakeholders etc., when preparing strategies in advance. Emotions can actually contribute to a sense of urgency. I will discuss these issues in more detail in the following section.
6 COVID-19 Risks, Imagination and Feeling a Sense of Urgency
Emotions, such as a sense of responsibility and empathy, can encourage us to imagine the implications of alternative action options. Works of art and documentaries can facilitate this and contribute to a sense of urgency that currently seems to be lacking in policy approaches to the COVID-19 pandemic, such as in the Netherlands.
It is striking that aside from the warnings of virologists, artists have also warned of the real possibilities of a severe pandemic. There are many examples of this, but John Suits’ 2016 film, Pandemic, maps this out in depth. Despite these warnings from the arts and sciences, policy makers around the globe seem to be continuously improvising about how to respond to the current pandemic. One would imagine that every government should have a range of scenarios available with concrete and adaptive plans for a situation like this. Furthermore, on the level of international politics, strategies for dealing with such a situation should have been prepared in advance, e.g. in the context of the WHO. But presumably, other issues were perceived as more urgent, and as we have seen, the Dutch authorities have frequently put recommendations from the WHO concerning COVID-19 aside.
This happened at various stages of the pandemic, not only in the beginning but for example also in the early autumn 2020, when infection rates in the Netherlands started to increase, presumably due to international travel during summer vacations, schools reopening, and seasonal effects. While some other countries were already taking more precautionary measures, the Netherlands waited until the numbers were so high that harsh lockdown measures were eventually unavoidable, in the meantime implying hospitalizations, severe illness and death as well as overburdening the health sector, which had been trimmed down over the last decades in the light of efficiency considerations. Dutch ICU patients had to be admitted to German hospitals at several stages due to Germany’s significantly larger ICU capacity. A lack of preparedness also surrounded the early stages of the Dutch vaccination strategy. In autumn 2020, the world was getting unexpected good news: much earlier than hoped for, several vaccines proved to be effective and could be available on a large scale within a few months. Dutch newsreaders could learn on a daily basis how the UK, Israel, Germany, and other countries were preparing their vaccination strategies. They didn’t hear much about the Dutch strategies until late December 2020. It was then announced that the vaccination would start in early January 2021, weeks later than the countries mentioned above. The Dutch health minister, Hugo de Jonge, justified this by saying that the Dutch needed more time because they would do things ‘thoroughly’, implying a less thorough approach by the other countries. Yet, the first weeks of vaccinating were dominated by news about chaotic and inefficient bureaucracy, and multiple changes in strategy, while other countries were making quick progress. Eventually, the Netherlands caught up and now has one of the highest vaccination rates in the world. But a lot of time seems to have been wasted in the early weeks and months. More timely preparations could have alleviated COVID-19 numbers and accompanying direct and indirect health burdens, not to mention the sense of despair that many people felt during that time.
At the time of writing this article (autumn 2021) we see a similar situation in the Netherlands as 1 year before. Despite high vaccination rates, infection rates are rapidly rising, presumably due to the much more infectious Delta-variant in combination with seasonal effects and the loosening of measures when infections rates still were low. While there is a lot of societal concern about this, politicians are slowly and only hesitantly responding, again primarily relying on STEM-based advice by the modellers of the RIVM and the medical and virological experts of the OMT, without consulting social scientists and ethicists. This is despite the fact that there is a growing public tension, for example, an opposition between those who are vaccinated and those who are not, and different views in societies on whether more safety measures are needed or not. This is an issue for which the expertise of social scientists and ethicists could be of crucial importance. Yet, these experts are not systematically consulted by the government or policymakers, except consultation of ethicists for specific medical policy advice concerning vaccination or triage in hospitals and concerning some issues, behavioural scientists at the RIVM and OMT. But, as argued above, all aspects of COVID-policies have significant ethical and societal dimensions, thereby requiring systematically involving the expertise of ethicists and social scientists concerning the overall policy measures.
Emotionally charged human capacities, such as imagination, can play an important role in experiencing urgency, as well as in moral deliberation and in developing and thinking about future scenarios. As mentioned above, the work of artists, filmmakers, and writers can play an essential role in such future scenario thinking. Artworks can appeal to the imagination, make abstract problems more concrete and facilitate ethical deliberation on the implications of such future scenarios (Roeser, 2018). Artworks such as (science fiction) novels and films in which the consequences of a pandemic are described can appeal to the imagination, make abstract problems tangible and thereby facilitate ethical deliberation about the implications of such future scenarios. If policy makers can heed the warnings of artists (such as Pandemic, for example), then the arts may have potential to help catalyse future pandemic-prevention strategies, taking into account the implications for public health, as well as for the economy and well-being of different population groups.
7 Conclusion
The current COVID-19 crisis highlights that decision-making about risks always requires scientific knowledge to be accompanied by societal and ethical considerations. My approach to emotions in the context of risk offers an alternative to the technocratic or populist approaches used to combat COVID-19. Emotions are a rich and valuable resource that is wrongly rejected in decision-making about risk and uncertainty. The current approach should be enriched, focusing on citizens’ concerns, involving ethical reflection on different choices and policy options. Emotions such as compassion, feelings of responsibility, and concern can help us reflect on the ethical implications of the difficult decisions we face. In the current situation and coming years, we will need all the sources of insight we have at our disposal to meet the enormous challenges of the COVID-19 crisis as well as possible future pandemics. So indeed, we need to consider the insights of virologists and medical experts. Still, we also need expertise from ethicists, social scientists, and the arts and humanities to take social and ethical considerations into account. In order to take on the severe challenges of this situation, we need to draw on our rich human capacities: scientific knowledge, insights from social sciences, arts and humanities, and emotional capacities. Rather than dismissing emotions, we should embrace them as a vital resource. Emotions such as compassion and feelings of responsibility and care can help us to reflect on the ethical implications of the hard choices we face. They can play an essential role in motivating actions of solidarity and courage that can hopefully contribute to solutions to the ongoing as well as future pandemics.
Notes
- 1.
- 2.
The Dutch government fell in January 2021 due to the so-called ‘toeslagenaffaire’, i.e. a more than 15 year long systematic tax scandal based on racist and other biases, with widespread consequences for numerous people, and continuously growing evidence of the failure of the rule of law. Since then, various other scandals have emerged that would presumably have led to the falling of the government, if it hadn’t stepped down already. Despite elections in March 2021, as of December 2021, the date of finalizing the writing of this chapter, there is still no new government, and the most likely new government is a continuation of the previous coalition.
References
Asveld, L., & Roeser, S. (Eds.). (2009). The ethics of technological risk. Earthscan.
Damasio, A. R. (1994). Descartes’ error: Emotion, reason and the human brain. G.P. Putnam.
De Hollander, A. E. M., & Hanemaaijer, A. H. (2003). Nuchter omgaan met risico’s: Milieu—En natuurplanbureau (MNP)—RIVM. RIVM.
Fisher, M. (2020). Coronavirus ‘hits all the hot buttons’ for how we misjudge risk. https://www.nytimes.com/2020/02/13/world/asia/coronavirus-risk-interpreter.html, visited: 3 November 2021.
Frijda, N. (1986). The emotions. Cambridge University Press.
Furtak, R. A. (2018). Knowing emotions: Truthfulness and recognition in affective experience. Oxford University Press.
Hansson, S. O. (2009). An agenda for the ethics of risk. In L. Asveld & S. Roeser (Eds.), The ethics of technological risks (pp. 11–23). Earthscan.
Hume, D. (1975) [1739-40]. L. A. Selby-Bigge (Ed.), A treatise of human nature, 2nd ed. revised by P.H. Nidditch, Clarendon press, Oxford.
Kahneman, D. (2011). Thinking fast and slow. Farrar, Straus and Giroux.
Loewenstein, G. F., Weber, E. U., Hsee, C. K., & Welch, N. (2001). Risk as feelings. Psychological Bulletin, 127(2), 267–286. https://psycnet.apa.org/doi/10.1037/0033-2909.127.2.267
Moore, G.E. (1988) [1903]. Principia Ethica. Promotheus Books.
NOS. (2020). https://nos.nl/artikel/2328889-rond-19-00-uur-wordt-duidelijk-hoe-gaan-we-verder-na-6-april; visited: 3 November 2021.
NOS. (2021a). https://nos.nl/nieuwsuur/collectie/13881/artikel/2403299-reconstructie-nederland-koos-te-laat-voor-bestrijden-corona; visited: 3 November 2021.
NOS. (2021b). https://nos.nl/nieuwsuur/collectie/13881/artikel/2403300-verantwoording-reconstructie-corona-aanpak-nieuwsuur; visited: 3 November 2021.
NOS. (2021c). https://nos.nl/nieuwsuur/collectie/13881/artikel/2403432-gommers-en-kuipers-kritisch-sturen-op-besmettingen-had-reguliere-zorg-minder-belast; visited: 3 November 2021.
NOS. (2021d). https://www.youtube.com/watch?v=Zp0MDXy7F2k; visited: 10 December 2021.
Nussbaum, M. C. (2001). Upheavals of thought: The intelligence of emotions. Cambridge University Press.
Prichard, H. A. (1912). Does moral philosophy rest on a mistake? Mind, 21(81), 21–37. https://doi.org/10.1093/mind/XXI.81.21
Roberts, R. C. (2003). Emotions: An essay in aid of moral psychology. Cambridge University Press.
Roeser, S. (2006). The role of emotions in judging the moral acceptability of risks. Safety Science, 44(8), 689–700. https://doi.org/10.1016/j.ssci.2006.02.001
Roeser, S. (2011). Moral emotions and intuitions. Palgrave Macmillan.
Roeser, S. (2018). Risk, technology, and moral emotions. Routledge.
Roeser, S., Hillerbrand, R., Peterson, M., & Sandin, P. (Eds.). (2012). Handbook of risk theory: Epistemology, decision theory, ethics, and social implications of risk. Springer. https://doi.org/10.1007/s11948-012-9362-y
Roeser, S., & Pesch, U. (2016). ‘An emotional deliberation approach to risk’. Science, Technology & Human Values, 41, 274-297.
Slovic, P. (2010). The feeling of risk: New perspectives on risk perception. Earthscan.
Solomon, R. C. (1993). The passions: Emotions and the meaning of life. Hackett Publishing Company.
Steinert, S., & Roeser, S. (2020). Emotions, values and technology: Illuminating the blind spots. Journal of Responsible Innovation, 7(3), 298–319. https://doi.org/10.1080/23299460.2020.1738024
Sunstein, C. R. (2005). Laws of fear. Cambridge University Press.
Sunstein, C.R. (2020). The cognitive bias that makes us panic about coronavirus. Bloomberg. https://www.bloombergquint.com/gadfly/coronavirus-panic-caused-by-probability-neglect ; visited 10 December 2021.
Van Asselt, M., & Vos, E. (2006). The precautionary principle and the uncertainty paradox. Journal of Risk Research, 9, 313–336. https://doi.org/10.1080/13669870500175063
WHO. (2020). https://www.youtube.com/watch?v=e-XPL91r0uk&t=4s; visited 26 November 2021.
Acknowledgements
I would like to thank Matthew Dennis and the other editors for their very helpful comments on an earlier version of this chapter. The chapter incorporates updated and significantly expanded passages from a Dutch article: Sabine Roeser (2020), ‘Corona, risico’s en morele emoties’, Tijdschrift voor Bioethiek 27:3 pp. 7–9 (reprinted at the blog ‘bijnaderinzien’). Available at: https://nvbioethiek.files.wordpress.com/2020/07/podium-20-3-naar-een-morele-agenda-na-de-coronacrisis.pdf
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Roeser, S. (2022). Understanding Risks and Moral Emotions in the Context of COVID-19 Policy Making: The Case of the Netherlands. In: Dennis, M.J., Ishmaev, G., Umbrello, S., van den Hoven, J. (eds) Values for a Post-Pandemic Future. Philosophy of Engineering and Technology, vol 40. Springer, Cham. https://doi.org/10.1007/978-3-031-08424-9_11
Download citation
DOI: https://doi.org/10.1007/978-3-031-08424-9_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08423-2
Online ISBN: 978-3-031-08424-9
eBook Packages: Religion and PhilosophyPhilosophy and Religion (R0)