Abstract
This chapter illustrates dietary strategies in the treatment of fecal incontinence. Although some foods must be excluded, the proportion of macronutrients should remain unchanged. One important strategy in dietary schemes to improve the symptoms of fecal incontinence is to drastically reduce several simple carbohydrates, in particular those known as FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols). The recommended percentage of calories from carbohydrates in patients with fecal incontinence should be around 55% and the percentage of energy from lipids around 30%. Moderate coffee consumption should be allowed, although each patient’s individual response should be monitored. Spices, as well as spicy and smoked foods, should be avoided or at least limited for their irritating action on the mucous membranes of the digestive system and stimulating effect on secretions and motility. The importance of the preferential use of healthy foods (fruit and vegetables, fish, extra virgin olive oil) is also discussed.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 General Principles of Diet
A diet is correct and balanced when, on a daily basis, a series of suggestions and rules relating to the quantity, quality, and variety of foods eaten are followed [1]. The daily energy intake must be adequate for calorie consumption, and all the nutrients that allow you to derive health benefits must be present in a diet. There is no food that can be said to be truly complete (if we exclude breast milk for babies up to 8–12 months). The simplest and safest way to be able to assimilate, in the right quantities, all the nutrients necessary for the proper functioning of our body is to vary the foods eaten and combine them in the most appropriate way. The body contains almost all the nutritional elements that we find in food, the nutrients, that are divided into macronutrients (carbohydrates, lipids, and proteins) and micronutrients (vitamins and minerals). Macronutrients give energy, while micronutrients do not give energy, but they are necessary for biological functions [2, 3]. Alcohol is a particular macronutrient that gives energy, but it is not necessary for a healthy diet.
Water, despite being an indispensable element for many functions (and the composition itself!) of the human body, is not considered a nutrient.
To follow a balanced diet, it is advisable to take the correct quantities of macro- and micronutrients and that the daily calorie intake is divided into specific proportions. This means that 15% of the daily calories should come from protein, 25–30% from lipids, and 55–60% from carbohydrates.
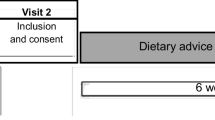
2 Dietary Therapeutic Strategies
The general principles of dietary strategies for the treatment of fecal incontinence [4] are the same as those for people without fecal incontinence. Some foods must be excluded from the diet of patients suffering from fecal incontinence (Table 8.1), but the proportion of macronutrients remains unchanged. A drastic reduction of many simple carbohydrates is an important strategy in dietary schemes to improve the symptoms of patients with fecal incontinence [5, 6].
2.1 Low FODMAP Diet
The carbohydrates that need to be drastically reduced are those known as FODMAPs, i.e., “fermentable oligosaccharides, disaccharides, monosaccharides, and polyols”. These are short-chain carbohydrates that are poorly absorbed by the small intestine and induce excessive fluid and gas accumulation, resulting in bloating, abdominal distention, and pain. FODMAPs are found in many foods, including those containing fructose, lactose, galacto-oligosaccharides, fructans, and polyols (such as mannitol, sorbitol, maltitol, and xylitol). The rapid fermentation of these carbohydrates causes important osmotic effects. FODMAPs are poorly absorbed for several reasons: (1) the absence of luminal enzymes capable of hydrolyzing the glycosidic bonds contained in carbohydrates, (2) low activity of brush border enzymes (e.g., lactase), or (3) the presence of low-capacity epithelial transporters, such as glucose transporter 5 and fructose (GLUT-5) and glucose transporter 2 (GLUT-2).
Fructose, which is an important FODMAP, is absorbed across villous epithelium through low-capacity, carrier-mediated diffusion involving GLUT-5. The absorption of free fructose is increased in the presence of glucose via GLUT-2. When fructose is present in excess of glucose, the fructose malabsorption is enhanced. Furthermore, several substances, such as polyols, are too large for simple diffusion. On the other hand, oligosaccharides are rapidly fermented, compared to polysaccharides. Fermentation produces hydrogen, carbon dioxide, and methane. Finally, osmotically active small molecules draw more water into the small intestine.
Thus, a diet low in FODMAPs is an important tool in the therapeutic strategy for fecal incontinence.
2.2 Percentage of Macronutrients
Meal composition influences the gastrocolic reflex. This is a physiological reflex that controls the motility of the lower gastrointestinal tract following a meal. The gastrocolic reflex is induced by the gastric stretch due to food ingestion and its activation results in the urge to defecate. Foods that stimulate this reflex too much should be drastically reduced in the diet of patients with fecal incontinence [7].
Carbohydrate meals induce a colonic motor response, but the effects are short lived when compared with fat meals. The prolonged, segmental, and retrograde phasic activity induced by a fat meal may delay colon transit. Thus, meal composition influences colonic motor response [8, 9].
It has been shown that meals containing fat delay gastric and small bowel transit. Experimental evidence showed that the infusion of fat into the duodenum induces a duodenal brake. These events are probably due to the stimulation of specialized mucosal cells (such as I cells of the duodenojejunum that secrete cholecystokinin) or due to the release of peptide YY, both of which can delay gastric emptying. In contrast, the shorter duration and more rapid onset of the colonic motor response after a carbohydrate meal may be due to the faster transit of this meal through the stomach and small bowel.
Considering that the recommended percentage of calories from carbohydrates ranges from 55% to 60%, the advisable percentage of energy from carbohydrates in patients with fecal incontinence should be closer to 55% than 60%; similarly, since the recommended percentage of calories from lipids ranges from 25% to 30%, the advisable percentage of energy from lipids should be closer to 30% than 25%.
2.3 Coffee
Although there is some experimental evidence showing that coffee stimulates the contraction of the gallbladder and the motor response of the colon, it is not conclusively proven that coffee induces a major increase in colonic motor activity [10]. Therefore, moderate coffee consumption should be allowed in patients with fecal incontinence, although the response should be monitored in a personalized manner.
2.4 Spices, Spicy and Smoked Foods
Spices, as well as spicy and smoked foods, should also be avoided or at least limited for their irritating action on the mucous membranes of the digestive system, as well as for their stimulating effect on secretions and motility.
2.5 Supplementation with Vitamins and Minerals
Micronutrient supplements should always be considered for patients with fecal incontinence. Vitamins and/or mineral salts should be used to supplement any deficiencies caused by dietary restrictions regarding the quality and quantity of food.
3 Importance of Healthy Foods
The importance of the preferential use of healthy foods should not be overlooked. In particular, the following foods should always be present: fruit and vegetables (obviously only those allowed in fecal incontinence), fish, and extra virgin olive oil (Table 8.2).
3.1 Fruit and Vegetables
Fruit and vegetables can be divided into five colors (the so-called colors of well-being):
-
(a)
Blue/Purple (e.g.: berries, eggplant, grape)
Important substances: anthocyanin, carotenoids, vitamin C, potassium, and magnesium.
-
(b)
Green (e.g.: kiwi, lettuce, peppers, zucchini)
Important substances: chlorophyll, carotenoids, magnesium, vitamin C, folic acid and lutein
-
(c)
Red (e.g.: peppers, tomatoes, strawberries)
Important substances: lycopene, anthocyanins.
-
(d)
White (e.g.: celery, grape)
Important substances: polyphenols, flavonoids, potassium, vitamin C.
-
(e)
Yellow-Orange (e.g.: carrots, clementines, mandarins, oranges, peppers)
Important substances: flavonoids, carotenoids, vitamin C.
The phytochemicals contained in these foods have remarkable antitumoral and antiaging effects.
3.2 Fish
Fish is a food with excellent nutritional properties and numerous beneficial effects for human health [11]. It contains a good amount of proteins, about 15–20% by weight, which are proteins with a high biological value and easily digestible (especially compared to meat proteins). Fish also contains omega-3 polyunsaturated fatty acids (PUFA), vitamins (especially vitamins D, B, and A), and mineral salts such as potassium, phosphorus, iodine, calcium, and iron [12].
Omega 3 PUFA contain two or more double bonds and are derived from the essential fatty acid alpha-linoleic acid. They are found in fish and fish oils and their health benefits are numerous as they serve various functions in our body. They are components of phospholipids in cell membranes, are involved in the metabolism of cholesterol, and are precursors of biologically active compounds such as prostaglandins, interleukins, and thromboxanes. All these functions indicate that they have pivotal roles in the immune response, blood clotting, and inflammation.
Thanks to these characteristics, fish is considered a “friend of health”. In particular, oily fish and fish with a high content of omega 3 PUFA, such as anchovies, sardines, mackerel, tuna, salmon, and cod, should be consumed more frequently. The consumption of fish is associated with numerous benefits that affect many aspects of health.
Specifically, evidence suggests that fish consumption is associated with a lower risk of cardiovascular disease, depression, and mortality. Furthermore, an inverse association exists between fish intake and risk of metabolic syndrome. Fish consumption is also associated with antiaging effects, cell protection, and improvement of cell functions and cognitive functions. Additionally, the anti-inflammatory properties of omega-3 PUFA may also have a beneficial effect on remission of aforementioned pathologies. Therefore, fish can be considered a healthy animal-based dietary source of protein.
3.3 Extra Virgin Olive Oil
Extra virgin olive oil (EVOO) is the product of the mechanical extraction process of olives deriving from Olea europaea L., commonly known as the olive tree. EVOO is a fundamental ingredient of the Mediterranean diet and is responsible for a great many health benefits associated with this diet [13]. The features of this food, which is also called “the golden food”, are in part due to the production process since it is obtained using exclusively mechanical procedures, and it has a free acidity that cannot be greater than 0.8%. Furthermore, to be defined as EVOO, it must not show sensory defects and it must have a fruity taste.
EVOO is characterized by a high concentration of bioactive components, such as phenolic compounds, but also vitamins A, D, and E, as well as β-carotene, and it exerts countless health benefits, mainly due to its antioxidant activity. It is also rich in oleic acid which possesses beneficial health effects [14]. Its antioxidant activity is linked to its ability to protect DNA, proteins, and lipids from damage caused by exposure to reactive oxygen species (ROS), which in turn are increased in patients with inflammation. Studies show a significant improvement in protein carbonylation, lipid peroxidation, and mental health status, and beneficial effects on several cardiovascular risk markers after a dietary intervention with EVOO. The biological activities related to the beneficial effects of consuming EVOO have been mainly attributed to the unsaturated fatty acid (UFA) composition and phytochemical compounds in these foods (polyphenols). Both UFA and polyphenols exert anti-inflammatory and antioxidant effects [15].
Furthermore, EVOO could improve health through positive effects on gut microbiota.
Therefore, evidence suggests that EVOO is a natural antioxidant that can be used in primary prevention and is recommended in preference to the use of antioxidant supplements.
References
Temple NJ, Guercio V, Tavani A. The Mediterranean diet and cardiovascular disease: gaps in the evidence and research challenges. Cardiol Rev. 2019;27(3):127–30.
Głąbska D, Guzek D, Groele B, Gutkowska K. Fruit and vegetable intake and mental health in adults: a systematic review. Nutrients. 2020;12(1):115. https://doi.org/10.3390/nu12010115.
Głąbska D, Guzek D, Groele B, Gutkowska K. Fruit and vegetables intake in adolescents and mental health: a systematic review. Rocz Panstw Zakl Hig. 2020;71(1):15–25.
Nakano K, Takahashi T, Tsunoda A, Shimizu Y. Effects of dietary guidance without dietary fiber supplements on the symptoms, quality of life, and dietary intake in patients with fecal incontinence. J Anus Rectum Colon. 2020;4(3):128–36.
Menees SB, Chandhrasekhar D, Liew EL, Chey WD. A low FODMAP diet may reduce symptoms in patients with fecal incontinence. Clin Transl Gastroenterol. 2019;10(7):e00060. https://doi.org/10.14309/ctg.0000000000000060.
Zahedi MJ, Behrouz V, Azimi M. Low fermentable oligo-di-mono-saccharides and polyols diet versus general dietary advice in patients with diarrhea-predominant irritable bowel syndrome: a randomized controlled trial. J Gastroenterol Hepatol. 2018;33(6):1192–9.
Colavita K, Andy UU. Role of diet in fecal incontinence: a systematic review of the literature. Int Urogynecol J. 2016;27(5):1805–10.
Andy UU, Ejike N, Khanijow KD, et al. Diet modifications in older women with fecal incontinence: a qualitative study. Pelvic Med Reconstr Surg. 2020;26(4):239–43.
Bliss DZ, Savik K, Jung HJ, et al. Dietary fiber supplementation for fecal incontinence: a randomized clinical trial. Res Nurs Health. 2014;37(5):367–78.
Iriondo-DeHond A, Uranga JA, del Castillo MD, Abalo R. Effects of coffee and its components on the gastrointestinal tract and the brain–gut axis. Nutrients. 2021;13(1):88. https://doi.org/10.3390/nu13010088.
Karimi G, Heidari Z, Firouzi S, Haghighatdoost F. A systematic review and meta-analysis of the association between fish consumption and risk of metabolic syndrome. Nutr Metab Cardiovasc Dis. 2020;30(5):717–29.
Jayedi A, Shab-Bidar S. Fish consumption and the risk of chronic disease: an umbrella review of meta-analyses of prospective cohort studies. Adv Nutr. 2020;11(5):1123–33.
Campos VP, Portal VL, Markoski MM, et al. Effects of a healthy diet enriched or not with pecan nuts or extra-virgin olive oil on the lipid profile of patients with stable coronary artery disease: a randomised clinical trial. J Hum Nutr Diet. 2020;33(3):439–50.
Jimenez-Lopez C, Carpena M, Lourenço-Lopes C, et al. Bioactive compounds and quality of extra virgin olive oil. Foods. 2020;9(8):1014. https://doi.org/10.3390/foods9081014.
Mazza E, Fava A, Ferro Y, et al. Effect of the replacement of dietary vegetable oils with a low dose of extravirgin olive oil in the Mediterranean diet on cognitive functions in the elderly. J Transl Med. 2018;16(1):10. https://doi.org/10.1186/s12967-018-1386-x.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (http://creativecommons.org/licenses/by-nc-nd/4.0/), which permits any noncommercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if you modified the licensed material. You do not have permission under this license to share adapted material derived from this chapter or parts of it.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Monda, M. (2023). Diet in Fecal Incontinence. In: Docimo, L., Brusciano, L. (eds) Anal Incontinence. Updates in Surgery. Springer, Cham. https://doi.org/10.1007/978-3-031-08392-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-031-08392-1_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08391-4
Online ISBN: 978-3-031-08392-1
eBook Packages: MedicineMedicine (R0)