Abstract
Dementia presents unique challenges for the measurement of health-related quality of life (HRQL). The subjective nature of the HRQL construct, the cognitive demands of questionnaires, and the necessity of sometimes relying on a proxy report taken together mean that traditional questionnaires scored using classical psychometrics may not provide robust measurement. Advanced psychometric methods, such as those based on Rasch measurement theory, can provide possible solutions to these challenges. Rasch based methods have been used with the DEMQOL/DEMQOL-Proxy disease specific HRQL instrument to measure HRQL in people with dementia, to provide robust scales, to equate self- and proxy-reported instruments, and to create a cross walk from a proxy-reported measurement to the equivalent self-reported measurement. These methods also provide a qualitative understanding of statistical change. Advanced psychometric methods such as those based on Rasch measurement theory therefore provide a potentially powerful way to address the challenges of measuring HRQL for people with dementia. However, the use of these methods is not a quick fix. They require careful development of a conceptual framework describing the construct (HRQL) and a commitment to keeping the person with dementia’s perspective central at all stages of the process.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
3.1 The Challenge of Measuring HRQL in Dementia
3.1.1 The Nature of Dementia
The term dementia refers to a collection of diseases (including Alzheimer’s disease, dementia with Lewy bodies, vascular and frontotemporal dementia) causing short term memory loss, difficulties with thinking (concentration, planning and organizing), language (following a conversation), orientation (losing track of what day it is, who people are) and visuospatial awareness (judging distance or seeing in three dimensions). People with dementia may also experience changes in mood, becoming more frustrated, irritable or withdrawn, anxious or easily upset or unusually sad. Dementia is progressive and degenerative and although some pharmacological treatments can delay the progress, there is currently no cure.
Globally, dementia affected an estimated 50 million people in 2017 [2] with prevalence expected to increase to 75 million by 2030. In the UK, estimated prevalence in 2020 was 907,900, rising to 1,590,100 by 2040 [62]. Dementia had a worldwide cost in 2014 of £26.3 billion [32] and in the UK alone, costs of social care for people with dementia are expected to triple by 2040 [62]. Its impact is wide ranging with effects on almost all aspects of life for both the patient [9] and their family [17].
The ability to measure health-related quality of life in dementia (HRQL) as an outcome of treatment and interventions, or to monitor the effect of disease progression, is therefore important. There have been several attempts to make recommendations about outcome measures including HRQL for use in dementia research, [59], clinical trials [57] and in routine monitoring [14, 15] with the intention that standardization of choice of instrument will improve interpretation and help to create a more meaningful body of evidence. Yet to be clinically meaningful for use in clinical trials, applied research, clinical audit and clinical practice, instruments that purport to measure HRQL of people with dementia need to be fit for purpose and provide robust and rigorous measurements [22]. To date, few disease-specific HRQL instruments for dementia have achieved this.
3.1.2 Requirements for Rigorous Measurement of HRQL
The robust measurement of a construct such as HRQL in any condition requires a number of requirements to be met. First there must be a clear definition and conceptual framework to fully describe the construct, thus laying the foundations for validity [18]. Every component of the construct should be represented by questions (or items) on the questionnaire, phrased in a standard way that is clear, non-ambiguous and easy to follow. The conceptual framework should ideally include a hierarchical continuum of the components (items) of the construct along the scale (or “ruler”) [22]. When this a priori hierarchy of items exists, it is possible to provide descriptions of HRQL for any score along the scale, and thus measurement provides not only a number along the scale but also a clear understanding of what that number means [52]. This also enables change in HRQL to be evaluated in a way that is more meaningful.
The questionnaire should be completed by the person best able to report accurately on the experience that is being asked about (usually the patient themselves). Prioritizing a self-report in this way helps to minimize bias and further error. The questions (or items) that make up the questionnaire should be able to be combined into a scale that has robust psychometric measurement properties (reliability and validity). Typically this has been through the use of methods based on Classical Test Theory [29] and standard guidelines have been established [18, 24, 37]. These requirements create a paradox as good measurement requires that the perspective of the person with dementia themselves is kept central as far as possible, yet the nature of the condition can challenge each of these criteria. The remainder of this chapter addresses whether and to what extent each of these requirements has been addressed in attempts to measure HRQL in dementia.
3.1.3 Four Challenges to Robust Measurement of HRQL in Dementia
3.1.3.1 HRQL Is Subjective
Although there is no universal definition of HRQL, there is general agreement that it is the subjective impact of a person’s health condition on their life. That is, it relies on the individual’s perception and understanding of their experience of their health condition, rather than an objective report of an observable event [12]. There is obvious tension therefore with the abilities of people with dementia to articulate and express these types of concepts, particularly as insight is known to deteriorate with increasing severity of dementia. Nevertheless, international guidelines on quality of life in dementia [59] have retained this subjectivity in their definition of HRQL in dementia, remarking on “… . the integration of self-perceptions, a satisfactory cognitive functioning, personal activities, psychological well-being, and social interactions.”
HRQL is therefore distinct in nature from constructs of “function” (how well can a person do something) or “symptoms” (what observable indications does a person experience). For the same severity of a condition two people may report very different levels of HRQL, because they appraise their symptoms, function and health experience in a different way. This may be the result of factors such as coping mechanisms [3], available support [19], or personality [7].
Historically, frameworks that describe HRQL have typically included elements of physical, mental and social well-being [31, 60], so in addition to the subjective experience of physical aspects of health, HRQL also includes some complex components concerned with the individual’s understanding and experience of non-observable elements of health such as mental and social wellbeing. Qualitative work to explore the meaning of HRQL in dementia can be compromised because people with dementia may have difficulties with speech production and/or comprehension. In addition, the detrimental impact of dementia on reflective thinking and ultimately the loss of insight can make it difficult to ask people with dementia directly about their individual subjective experience of HRQL. Understanding what HRQL means for people with dementia and developing clear conceptual frameworks requires attentive and collaborative working with people with dementia and those who know them well to ensure that the perspective of people with dementia remains central.
3.1.3.2 Questionnaires Are Cognitively Demanding
Typical methods to minimize bias in questionnaires may not be helpful for people with dementia. Difficulties with memory, concentration and confabulation as a result of dementia can create limitations in reporting information in a consistent and meaningful manner and can mean that reporting with reference to a short time frame (such as the last week) can be unreliable. The familiar question and answer format can create challenges for people with dementia as their ability to combine cognitive functions (e.g., retention, comprehension, articulation and communication) may be reduced. Even the common strategy of using both positively and negatively worded questions to minimize reporting bias is also potentially confusing to people with dementia [46]. Likewise, although pictorial responses are preferred for people with some cognitive impairments (e.g., aphasia), they can be more demanding than a simple verbal scale for people with dementia [46]. Robust use of questionnaires with people with dementia therefore necessitates careful solutions that are grounded in consideration of the experience and ability of people with dementia.
3.1.3.3 Proxy-Report Is Sometimes Necessary
The cognitive difficulties associated with dementia mean that it can be difficult to obtain a reliable self-report of HRQL from the person with dementia themselves. Although careful questionnaire development and attention to the abilities of people with dementia mean that people with mild/moderate dementia can often successfully complete questionnaires [11, 23, 44, 45, 55], this is not possible in more severe dementia. Measurement of HRQL in dementia across the range of severity has therefore relied on a proxy (usually a family carer) to report on behalf of the patient. It is well known that agreement between patients and proxies is not always high [23, 28, 47, 51, 54], particularly for subjective, non-observable constructs such as HRQL and proxies tend to report HRQL as worse than the person with dementia themselves reports [47].
Further, in dementia there is also qualitative evidence to suggest that proxies report differences in type of components affecting HRQL as well as in extent of HRQL [44, 45]. For example, while both carers and people with dementia report an impact on the social aspects of HRQL, people with dementia describe this as a positive experience involving a social network of friends and family and the valued role they see for themselves within this community. In contrast carers tend to emphasize the negative impact of dementia on social relationships, describing unwanted or predatory social contacts and the challenges of communication in social situations. People with dementia also often compare themselves with their peers, whereas carers compare the person with dementia to how they used to be [44, 45].
3.1.3.4 Self- and Proxy-Reports Are Scaled on Different Metrics
It is not clear how to compare or interpret the different HRQL scores reported by people with dementia and those who care for them. When reported on instruments developed by Classical psychometric methods, these scores are on different scales (“rulers”) and similar numbers do not necessarily have similar meanings. With relatively mild cognitive impairment people with dementia are (with appropriately designed instruments and supports) likely to be able to respond for themselves and there is little need for a proxy. As cognitive impairment progresses, people with dementia are still likely to be able to self-report but it might be necessary to also have a proxy report as carers are likely to notice different aspects of HRQL. The two perspectives are therefore complementary, though not substitutable (because they are on different scales).
As cognitive function declines further, the person with dementia is no longer able to self-report, but a family carer would be able to make a proxy report. The challenge here is in how to keep the person with dementia’s perspective central even though their self-report is no longer reliable. With yet further cognitive decline, it is likely that the person with dementia is no longer living at home, and a family carer proxy-report is not appropriate because they do not see them frequently enough. Hence, the reliance on behaviorally observed instruments in later stages of dementia (Fig. 3.1). A potential solution to the proxy problem is described later.
3.2 Responses to the Challenge
Several reviews [10, 36, 44, 45, 57] have identified responses to these challenges in the form of disease-specific questionnaire-based instruments developed to measure subjective HRQL for people with dementia. Other approaches have relied solely on behavioral observation (e.g., QUALID, [58]), but as these do not assess the subjective element of HRQL we do not consider these further here. Instruments designed to measure HRQL via a written questionnaire include: Progressive Deterioration Scale (PDS) [13]; DQOL [11]; Quality of Life-AD (QOL-AD) [23]; Alzheimer’s Disease Related Quality of Life (ADRQL) [8, 33]; Community Dementia Quality of Life Profile (CDQLP) [38,39,41]; The Pleasant Events Schedule – AD [1]; Quality of Life in dementia Scale (QOL-D) [53]; Cornell Brown Scale for QOL in Dementia [35]; BASQID [55]; DEMQOL/DEMQOL-Proxy [47]. A further questionnaire-based instrument has also been developed that uses individualized domains, where content is specific to each respondent (Quality of Life Assessment Schedule: QOLAS) [42], but as this cannot be used to compare individuals, is not considered further here.
3.2.1 Proxy Reported Instruments
Of these instruments, six (PDS, ADRQL, CDQLP, Pleasant Events Schedule, QOL-D, Cornell Brown Scale for QoL in Dementia) have relied solely on a proxy-report (often from a family carer). While this by-passes the reporting difficulties associated with cognitive decline in dementia and makes obtaining reliable responses potentially easier, it does not address the challenge of the known differences between self- and proxy-reports of HRQL (as described above). Even when asked to report from the perspective that they think the person with dementia themselves would give, carers often find it hard to separate their own feelings from those that they think the person with dementia has [44, 45]. These reporting problems suggest that even if a proxy–reported instrument demonstrates robust psychometric properties, it is unlikely to be an accurate reflection of the experience of the person with dementia themselves.
3.2.2 Self-Reported Instruments
Two instruments (DQOL and BASQID) have developed successful methods to elicit self –reports on questionnaires from people with dementia. Both instruments made adaptations to the method of administration to minimize the bias associated with responses from people with a cognitive impairment. Both DQOL and BASQID are interviewer administered (i.e., questions are read out verbatim by an interviewer), though responses are self-reported (i.e., the interviewer records verbatim the response given by the respondent), using large fonts and cards with the response scales printed on them, which respondents can use to point to their answer. Both instruments are reported to be reliable and valid with people with mild/moderate dementia (MMSE> = 12) [11, 55] but are not appropriate for people with severe dementia. It is therefore difficult to use instruments that rely solely on a self-report for assessments of the change in HRQL over time, as the progressive and deteriorating nature of dementia is likely to mean that there will come a point where self-report is no longer possible.
3.2.3 Instruments with Both Self- and Proxy-Reported Forms
Two instruments (QOL-AD and DEMQOL/DEMQOL-Proxy) have been developed with both self-report and proxy-reported forms. In QOLAD the same questions (13 items) are asked of both person with dementia (interviewer administered, but self-reported) and their carer (self-administered). DEMQOL (28 items) and DEMQOL-proxy (31 items) include slightly different questions but have a common core of 15 items. Originally both were developed to be interviewer-administered [44, 45], though DEMQOL-Proxy has since been found to also be appropriate for use in self-administered format [20]. It is recommended that DEMQOL and DEMQOL-Proxy should always be administered together as they address different aspects of HRQL and are therefore complementary, but not substitutable.
A key advantage of having both self- and proxy-reported versions is that in circumstances where it is necessary to take repeated assessments of HRQL (either because the outcomes of an intervention are evaluated at different time points or because the impact of disease progression on HRQL is being monitored over time) there is an appropriate reporting method for all stages of severity (i.e., self-reported for mild/moderate dementia and proxy-reported for severe dementia). However, the limitations of the psychometric methods used to develop both QOLAD and DEMQOL/DEMQOL-Proxy mean that for both instruments the self- and proxy-reports exist on different rulers (that is, the scores are sample dependent) and there is no method for determining whether people with dementia and their careers are reporting on the same construct of HRQL or whether their understanding is slightly different nor for how to combine or equate scores from the two different rulers.
3.2.4 Psychometric Approaches
All of the available HRQL instruments for people with dementia were originally developed using psychometric methods based on Classical Test Theory (CTT) [30] and although widely used at the time, instruments developed using CTT have a number of weaknesses (see [22] for an overview). Firstly, they generate scales that at best are ordinal rather than equidistant interval scales. This means the scales are inappropriate for use in many statistical analyses (because they assume interval scales) and that evaluating change over time may not be very accurate, due to the different interpretation that can be given to the semantic labels of response scales at different time points.
Thus, the response option label “sometimes” may be interpreted and used in one way by a sample at baseline but given a slightly different meaning by the sample at follow up. As there is no way to know whether this is the case for a given evaluation of change it is a hidden problem within the data which is rarely investigated within the CTT paradigm. The scores generated with CTT methods can only be used for group comparisons and not for comparisons of individual patients. This is because the measures of statistical uncertainty (e.g. the standard error) are only computed at the group level. These scores are therefore of limited use in applied clinical settings for monitoring or evaluating individual patients and even in research contexts where group comparisons might be used, there is much less confidence around the scores at the extremes of the distribution compared with those in the middle, yet there is no way of addressing this. How well an instrument performs psychometrically is dependent on the particular sample it is tested in, making it difficult to know how robust the instrument is in other samples. This makes it difficult to compare studies and challenges the understanding of how scores change over time, since these will also be from different samples. Advanced psychometric methods, such as those based on Rasch measurement theory (RMT), provide a way of overcoming these challenges.
3.3 Benefits of Using Methods Based on Rasch Measurement Theory (RMT) for HRQL in Dementia
The Rasch paradigm [5, 34] is advantageous over other approaches to measurement because the model is chosen on a priori grounds, rather than on the basis of whether or not the data fit the model. The model meets the criterion of invariance (i.e., that measurement should be independent of the person constructing the test and that a particular measurement should be independent of the particular items and of other people taking the test). Data that fit the model therefore also meet the criterion of invariance. If the data do not fit the model in initial efforts at calibrating a new instrument, the Rasch paradigm advocates investigating the anomalies in the data to determine why the misfit has occurred and to identify improvements that can be made in the instrument by revising items or the sampling protocol. Given a calibrated instrument with a conceptually validated construct interpretation that is shown to be stable across samples, inconsistent data patterns are no longer a threat to validity, but are instead actionable information on special strengths and weaknesses that clinicians, families, advocates, and patients can use.
In addition, in the Rasch context, combinations of items and people can be placed on the same continuum (or “ruler”), depending on the particular model that is developed. Assuming a well-developed conceptual framework and data that fit the model, this characteristic provides powerful solutions to the challenges dementia poses for measurement.
3.3.1 Diagnostic Information About the Instrument
In practical terms for HRQL in dementia, the Rasch paradigm provides a helpful set of diagnostic tools by which anomalies in the instrument can be identified (e.g. items that are not working in the way that was intended). Rather than removing these items (as might be advocated in CTT or item response theory) the Rasch paradigm provides opportunity to further investigate these items qualitatively and to determine how they can be improved. In this way, the conceptual framework of the construct being measured (i.e., HRQL in dementia) is retained and items are optimized in an iterative process to represent each aspect of the construct. This ultimately aids understanding and interpretation of scores and application to individual patients. The interval scale produced as a result of measurement developed using RMT provides greater accuracy in scores for individuals at the extremes of the distribution and provides an individual standard error, meaning that instruments that fit the model are potentially robust enough to be used at the individual level, for example in clinical decision making.
Ability to identify anomalies and to investigate why these items have not been understood in the way that was intended is particularly valuable to resolve the reporting and cognitive difficulties associated with dementia. Given a robust conceptual framework, developed in partnership with people with dementia and their carers, it is possible to retain each of the components originally deemed to be important. Items are not removed because they have not worked well in the questionnaire format (as would typically happen in CTT item reduction), rather items that misfit can be investigated to improve wording or to further hone the underlying concept. The perspective of the person with dementia themselves is therefore retained in the questionnaire and the items are expressed in a way that can be best understood by them.
3.3.2 Equating HRQL Scores
The Rasch approach provides the opportunity for a unique solution to the self- versus proxy-reporting problem. Placing both self- and proxy-responses on the same ruler (i.e., in the same model) means that it is possible to equate proxy-reports with the equivalent self-report for the same question. In this way, when it is no longer possible to obtain a self-report from a person with dementia, we can use the proxy-reports to estimate (from the Rasch model) within a stated uncertainty range what the person with dementia would have said if they were able to respond. The person with dementia’s perspective is therefore not only central at the conceptual framework stage but also throughout the measurement process.
3.3.3 Quantifying and Understanding Impact on HRQL
Locating both respondents and items on the same interval continuum (or “ruler”) aids interpretation of scores in a way that is not possible in traditional approaches. In addition to a quantitative estimate of change in relation to an intervention or disease progression, the Rasch approach enables a qualitative description of what each particular point on the scale means. It is therefore possible to provide qualitative description (based on the content of the items) of what a particular change means in terms of the impact on a patient’s life. This is important and valuable for the practical application of such instruments in clinical decisions.
3.4 The Example of DEMQOL and DEMQOL-Proxy
Few instruments developed to measure HRQL for people with dementia have used the Rasch approach. This may reflect the spate of activity in this field in the early 2000s at a time when CTT methods were prevalent and advanced psychometric methods were only just becoming known in health-related research. Subsequently, a few studies have applied invariance scaling models to HRQL instruments in dementia in adaptations to other languages [56], evaluating instruments for new settings such as residential care [4], behaviorally based instruments [16, 38] and as part of a raft of item reduction methods to develop preference measures [25, 26]. However, DEMQOL/DEMQOL-Proxy is the only HRQL instrument in dementia to have systematically utilized the strengths of the Rasch paradigm to address the unique methodological challenges presented by measurement of HRQL in people with dementia.
3.4.1 Robust Scales for Use at the Individual Level
Analyses based on RMT [21] to establish whether and to what extent the data from DEMQOL and DEMQOL-Proxy fit the Rasch model found that Rasch measurements (based on 23 of the DEMQOL items and 26 of the DEMQOL-Proxy items) could be determined and, like all Rasch measurements, have interval properties and individual standard errors. Although future work is necessary to address the items that did not fit the model well, this approach enables greater confidence in the precision of an individual measurement and ensures they are robust enough for use with individual patients.
This is illustrated in Fig. 3.2. On the top half, the figure shows the raw scores (from the original CTT based scoring algorithm, [47]) for 3 cases referred to Memory Assessment Services for dementia (low, medium and high HRQL) and the associated error around them. Note that the error is very wide around each score and overlaps substantially between each of the three cases. Therefore, it is difficult to say whether these patients are substantially different in their HRQL. On the bottom half of the figure, the Rasch measurements for the same three cases are presented and it is clear that the error around each individual case is now much smaller, suggesting that the differences are substantive rather than part of the noise of the data.
This provides sufficient confidence in the data to potentially make it useful for clinical decision making with individual patients. For example, based on these Rasch measurements it would be possible to give patients illustration of the types of HRQL scenario that other people at the same stage have experienced and how the trajectory has developed.
3.4.2 A Solution to the Proxy Problem
RMT has also provided a practical solution to the methodological issue of proxy-reporting in dementia [49]. The developers of DEMQOL-DEMQOL-Proxy used a Rasch equating analysis to determine whether DEMQOL and DEMQOL-Proxy could be placed on the same metric (or “ruler”) and if they could, to establish a cross walk from DEMQOL Proxy to an estimate of the equivalent DEMQOL score. From the 28 items in DEMQOL and 31 in DEMQOL-Proxy, there were a pool of 44 items (of which 15 were common to both instruments). Previous analysis [21] had established that the 7 positive emotion items were not part of the same continuum and were removed from the pool, leaving 37 items (12 of which were common to both instruments).
Equating analysis was conducted on these 37 items, anchored by the DEMQOL (self-reported) items when the items were common. This model was evaluated for well-established criteria [6, 43, 61] including the extent to which there was item fit to the Rasch model; ordering of thresholds; differences in scores for different groups (assuming the same amount of the construct being measured) (DIF); dependence of items on each other; unidimensionality and whether the items were measuring a similar range of the construct as existed in the people being measured (targeting). Results indicated that items from both DEMQOL and DEMQOL-proxy could be placed on the same metric (or “ruler”) and therefore people with dementia (reporting on DEMQOL) and family carers (reporting on DEMQOL-Proxy) were sharing a common understanding of the construct of HRQL.
As RMT places both items and people on the same scale it was then possible to estimate for any DEMQOL-Proxy score the equivalent values for DEMQOL. Cross-walk tables (see [49] mean that for every DEMQOL-Proxy score it is now possible to look up the equivalent DEMQOL score. Thus, even when a person with dementia can no longer self-report we can obtain an estimate of what their score would have been, by cross referencing the equivalent score on the cross-walk table. This avoids simply relying on a proxy-report with known imprecision and biases. This is an important development in the measurement of subjective constructs such as HRQL in dementia. For the first time it is possible to keep the person with dementia’s view central throughout the process of measurement and at all stages of the disease progression.
3.4.3 Clear Qualitative Understanding of Statistical Change
The use of RMT methods has for the first time enabled a clear interpretation of the scores provided by instruments such as DEMQOL/DEMQOL-Proxy. To illustrate, imagine the case of Mr. Jones who goes to the Memory Assessment Service [48]. When he gets there, the nurse measures his height (which was 1.83 m), his weight (which was 82 kg) and he is told that there is a waiting time of 15 min. He is also asked to fill in a questionnaire and after a while the nurse tells him that his quality-of-life measurement is 67. To interpret and understand all of this information, Mr. Jones is implicitly using the standard definitions of length, mass and time and he can use that information to compare with other examples he knows about in his life experience.
For example, he understands that his height is appropriate for an adult man and that he is taller than his wife, but not as tall as the bus on which he travelled to the clinic. He understands that his weight is about average for someone of his height and that he is heavier than his young granddaughter but not as heavy as the elephant he saw in the zoo last year. He also understands that the waiting time means he will have to wait longer than it takes to make a cup of tea, but not as long as an episode of his favorite TV show. However, as there is no standard definition of quality of life, he is not sure what a measurement of 67 means for HRQL. The properties of the Rasch model, in placing both people and items on the same continuum, mean that we can help Mr. Jones to understand his measurement of 67 [48, 50].
As the measurements for DEMQOL range from 0 to 100 (where higher scores represent better HRQL), 67 is actually fairly high. The items located at that point on the DEMQOL scale indicate that this person is likely to report “a little” of a number of negative emotions and “a little” worry about not being able to do things she/he used to be able to and “a little” worry about short term memory. Someone else with a slightly lower measurement (say 56), would additionally be likely to have “a little” worry about a range of cognitive difficulties as well as beginning to feel “a little” distressed and being “quite a bit” worried about short term memory.
In addition to these negative emotions and worry about cognitive function, a third patient who reports a fairly low measurement (say 38) would also report “a lot” of worry about the social impact of having dementia (e.g. “a lot” of worry about how they got on with people close to them, people not listening, not being able to make themselves understood). Thus we can see that on the DEMQOL scale the HRQL impact of dementia is likely to be first noticed in terms of negative emotion, as HRQL worsens impact is seen in terms of worry about cognitive function and later when impact is greatest, also worry about social impact of dementia.
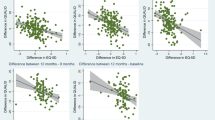
Smith et al. [50] report that statistically (using distribution-based methods, [27]) the minimal important difference (MID) for DEMQOL is about 6 scale points. For Mr. Jones, a 6 point improvement (from 67 to 73) indicates that he would now be “not at all” worried or anxious, “not at all” frustrated, “not at all” fed up, “not at all” worried about things he/she wanted to do but couldn’t and “not at all” worried about forgetting things that happened recently. Thus a MID change of 6 points is about 1 response option (see Fig. 3.3).
Other authors [30] have reported that people with dementia who start on anti-dementia drugs in the UK, report on average a 6-point improvement in HRQL and a similar impact was reported by people receiving psychosocial interventions (6.6 points). By providing a guide as to the most likely areas of impact, this “map” of where items are located based on RMT methodology provides a language with which patients and clinicians can potentially discuss the impact of intervention and/or disease progression on a person’s quality of life.
3.5 Conclusions
The progressive and deteriorating nature of dementia presents fundamental challenges for the robust measurement of subjective constructs such as HRQL. The cognitive demand of completing self-reported questionnaires, the necessity of relying on a proxy-reported questionnaire and reliance on psychometric methods based on Classical Test Theory have resulted in instruments that have only limited precision and are not appropriate for use with individual patients. The use of psychometric methods based on RMT with instruments such as DEMQOL/DEMQOL-Proxy has largely resolved these problems. However, the use of these methods is not a quick fix. They require careful development of a conceptual framework describing the construct (HRQL) and a commitment to keeping the person with dementia’s perspective central at all stages of the process. It involves working with people with dementia as partners, listening to what they tell us about what works and what is important in questionnaires. Combined with the statistical techniques embodied in RMT this provides a powerful way of improving measurement of HRQL for people with dementia.
References
S.M. Albert, C. del Castillo-Castanada, M. Sano, D.M. Jabobs, K. Marder, K. Bell, et al., Quality of life in patients with Alzheimer’s disease as reported by patient proxies. J. Am. Geriatr. Soc. 44, 1342–1347 (1996)
Alzheimer’s Disease International webpage (2020), https://www.alz.co.uk/research/statistics. Accessed 24 Aug 2020
R.J. Adams, D. Wilson, B.J. Smith, R.E. Ruffin, Impact of coping and socioeconomic factors on quality of life in adults with asthma. Respirology 9(1), 87–95 (2004)
E. Adler, B. Resnick, Reliability and validity of the Dementia Quality of Life measure in nursing home residents. West. J. Nurs. Res. 32(5), 686–704 (2010)
D. Andrich, A rating formulation for ordered response categories. Psychometrika 43, 561–573 (1978)
D. Andrich, Rasch Models for Measurement (Sage, Newbury Park, 1988)
M. Axelsson, E. Brink, J. Lötvall, A personality and gender perspective on adherence and health-related quality of life in people with asthma and/or allergic rhinitis. J. Am. Assoc. Nurse Pract. 26(1), 32–39 (2014)
B.S. Black, P.V. Rabins, J.D. Kasper, Alzheimer Disease Related Quality of Life (ADRQL) User’s Manual (Baltimore, DEMeasure, 1999)
S. Biggs, A. Carr, H.I. Irja, Dementia as a source of social disadvantage and exclusion. Australas. J. Ageing 38(Suppl 2), 26–33 (2019)
A. Bowling, G. Rowe, S. Adam, P. Sands, K. Samsi, M.L. Crane, J. Manthorpe, Quality of life in dementia: a systematically conducted narrative review of dementia-specific measurement scales. Aging Ment. Health 19(1), 13–31 (2015)
M. Brod, A.L. Stewart, L. Sands, P. Walton, Conceptualization and measurement of quality of life in dementia: The Dementia Quality of Life Instrument (DQoL). The Gerontologist 39(1), 25–35 (1999)
M. Bullinger, R. Anderson, D. Cella, N. Aaronson, Developing and evaluating cross-cultural instruments from minimum requirements to optimal models. Qual. Life Res. 2, 451–459 (1993)
R. DeJong, O.W. Osterlund, G.W. Roy, Measurement of quality of life changes in patients with Alzheimer’s disease. Clin. Ther. 11(4), 545–555 (1989)
Department of Health, The Adult Social Care Outcomes Framework 2015/16 (Department of Health, London, 2014), p. 37
Department of Health, Prime Minister’s Challenge on Dementia 2020. Implementation Plan (Department of Health, London, 2016), p. 13
T.P. Ettema, R.M. Dröes, J. de Lange, G.J. Mellenbergh, M.W. Ribbe, QUALIDEM: development and evaluation of a dementia specific quality of life instrument. Scalability, reliability and internal structure. Int. J. Geriatr. Psychiatry 22(6), 549–556 (2007)
A. Feast, M. Orrell, G. Charlesworth, N. Melunsky, F. Poland, E. Moniz-Cook, Behavioural and psychological symptoms in dementia and the challenges for family carers: Systematic review. Br. J. Psychiatry 208(5), 429–434 (2016)
Food US, Administration D, Guidance for industry on patient-reported outcome measures: use in medicinal product development to support labeling claims. Fed. Regist. 74, 1–43.16 (2009)
R. Gallagher, A. Sullivan, R. Burke, S. Hales, P. Sharpe, G. Tofler, Quality of life, social support and cognitive impairment in heart failure patients without diagnosed dementia. Int. J. Nurs. Pract. 22(2), 179–188 (2016)
A.A.J. Hendriks, S.C. Smith, T. Chrysanthaki, S.J. Cano, N. Black, DEMQOL and DEMQOL-Proxy: a Rasch analysis. Health Qual. Life Outcomes 15(1), 164 (2017a)
A.A.J. Hendriks, S.C. Smith, T. Chrysanthaki, N. Black, Reliability and validity of a self-administration version of DEMQOL-Proxy. Int. J. Geriatr. Psychiatry 32(7), 734–741 (2017b)
J. Hobart, S. Cano, Improving the evaluation of therapeutic interventions in multiple sclerosis: The role of new psychometric methods. Health Technol. Assess. 13(12), iii–168 (2009)
R.G. Logsdon, L.E. Gibbons, S.M. McCurry, L. Teri, Quality of life in Alzheimer’s disease: patient and caregiver reports. J. Ment. Health Aging 5(1), 21–32.4 (1999)
Medical Outcomes Trust, Assessing health status and quality of life instruments: Attributes and review criteria. Qual. Life Res. 11, 193–205 (2002)
B. Mulhern, D. Rowen, J. Brazier, S. Smith, R. Romeo, R. Tait, C. Watchurst, K.-C. Chua, T. Loftus Young, D. Lamping, M. Knapp, R. Howard, S. Banerjee, Development of DEMQOL-U and DEMQOL-PROXY-U: generation of preference-based indices from DEMQOL and DEMQOL-PROXY for use in economic evaluation. Health Technol. Assess. 17(5), 1–140 (2013)
K.H. Nguyen, B. Mulhern, S. Kularatna, B.J. Joshua, M.M. Wendy, C.T. Tracy, Developing a dementia-specific health state classification system for a new preference-based instrument AD-5D. Health Qual. Life Outcomes 15(1), 21 (2017)
G.R. Norman, J.A. Sloan, K.W. Wyrwich, Interpretation of changes in health-related quality of life. The remarkable universality of half a standard deviation. Med. Care 41(5), 582–592 (2003)
J.L. Novella, F. Boyer, C. Jochum, N. Jovenin, I. Morrone, D. Jolly, S. Bakchin, F. Blanchar, Health status in patients with Alzheimer’s disease: an investigation of inter-rater agreement. Qual. Life Res. 15(5), 811–819 (2006)
J.C. Nunnally, I.H. Bernstein, Psychometric Theory (McGraw Hill, New York, 1994), p. 15
M.H. Park, S.C. Smith, C.W. Ritchie, A.A.J. Hendriks, N. Black, Memory assessment services and health-related quality of life: 1-year follow-up. Int. J. Geriatr. Psychiatry 33(9), 1220–1228 (2018)
D.L. Patrick, P. Erickson, in Quality of Life in Health Care Evaluation and Resource Allocation, ed. Health Status and Health Policy. Concepts of Health-Related Quality of Life (Oxford University Press, Oxford, 1993, pp 76–112
M. Prince, M. Knapp, M. Guerchet, P. McCrone, M. Prina, A. Comas-Herrera, R. Wittenberg, B. Adelaja, B. Hu, D. King, A. Rehill, D. Salimkumar, Dementia UK Report (Alzheimer’s Society, London, 2014)
P.V. Rabins, J.D. Kasper, L. Kleinman, B.S. Black, D.L. Patrick, Concepts and methods in the development of the ADRQL: an instrument for assessing health-related quality of life in persons with Alzheimer’s disease. J. Ment. Health Aging 5(1), 33–48 (1999)
G. Rasch, Probabilistic Models for Some Intelligence and Attainment Tests (Danish Institute for Educational Research, Copenhagen, 1960). (Expanded edition with foreword and afterword by BD Wright. University of Chicago Press, Chicago, 1980)
R.E. Ready, B.R. Ott, J. Grace, I. Fernandez, The Cornell-Brown scale for quality of life in dementia. Alzheimer Dis. Assoc. Disord. 16, 109–115 (2002)
R.E. Ready, B.R. Ott, Quality of Life measures for dementia. Health Qual. Life Outcomes. 1(11) (2003)
B.B. Reeve, K.W. Wyrwich, A.W. Wu, G. Velikova, C.B. Terwee, C.F. Snyder, C. Schwartz, D.A. Revicki, C.M. Moinpour, L.D. McLeod, J.C. Lyons, W.R. Lenderking, P.S. Hinds, R.D. Hays, J. Greenhalgh, R. Gershon, D. Feeny, P.M. Fayers, D. Cella, M. Brundage, S. Ahmed, N.K. Aaronson, Z. Butt, ISOQOL recommends minimum standards for patient-reported outcome measures used in patient-centered outcomes and comparative effectiveness research. Qual. Life Res. 22(8), 1889–1905 (2013)
B. Resnick, E. Galik, A. Kolanowski, K. Van Haitsma, M. Boltz, J. Ellis, L. Behrens, N.M. Flanagan, Reliability and validity testing of the Quality of Life in Late-Stage Dementia Scale. Am. J. Alzheimers Dis. Other Dement. 33(5), 277–283 (2018)
S. Salek, N. Ramgoolam, S.A. Edwards, D.K. Luscombe, A.J. Bayer, in Quality of Life Assessment in Alzheimer’s Disease: Reliability of a Dementia-Specific Measure (CDQLP). European Symposium on Clinical Pharmacy (26th) (Tours, Loire Valley, 1997)
S. Salek, E. Schwartzberg, A.J. Bayer, in Evaluating Health-Related Quality of Life in Patients with Dementia: Development of a Proxy Self-Administered Questionnaire. E.S.C.P. 25th European Symposium on Clinical Pharmacy (Lisbon, 1996)
S. Salek, M.D. Walker, A.J. Bayer, The Community Dementia Quality of Life Profile (CDQLP): A factor analysis. Qual. Life Res. 8(7), 660 (1999)
C.E. Selai, M.R. Trimble, M.N. Rossor, R.J. Harvey, Assessing quality of life in dementia: preliminary psychometric testing of the Quality of Life Assessment Schedule. Neuropsychol. Rehabil. 11, 219–243 (2000)
E.V. Smith Jr., R.M. Smith, Introduction to Rasch Measurement (JAM Press, Maple Grove, 2004), p. 23
S. Smith, D. Lamping, S. Banerjee, et al., Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology. Health Technol. Assess. 9(10) (2005a)
S.C. Smith, J. Murray, S. Banerjee, B. Foley, J.C. Cook, D.L. Lamping, et al., What constitutes health-related quality of life in dementia? Development of a conceptual framework for people with dementia and their carers. Int. J. Geriatr. Psychiatry 20, 889–895 (2005b)
S.C. Smith, D.L. Lamping, B. Foley, J. Murray, S.S. Banerjee, in Obtaining Self-Reports about HRQL from Cognitively Impaired Respondents. Presented at ISOQOL Conference (Amsterdam, 2001)
S.C. Smith, D.L. Lamping, S. Banerjee, R.H. Harwood, B. Foley, P. Smith, J.C. Cook, J. Murray, M. Prince, E. Levin, A. Mann, M. Knapp, Development of a new measure of health-related quality of life for people with dementia: DEMQOL. Psychol. Med. 37, 737–746 (2007)
S.C. Smith, A.A.J. Hendriks, N. Black, in Understanding DEMQOL Scores: Minimal Important Differences. Presented at UK PROMs Conference (Oxford, 2017)
S.C. Smith, A.A.J. Hendriks, S.J. Cano, N. Black, Proxy reporting of health-related quality of life for people with dementia: a psychometric solution. Health Qual. Life Outcomes 18 (1) (2020)
S.C. Smith, A.A.J. Hendriks, S.J. Cano, N. Black, Minimally Important Difference on DEMQOL and DEMQOL-Proxy. Patient Reported Outcomes (Submitted)
K.C. Sneeuw, M.A.G. Sprangers, N.K. Aaronson, The role of health care providers and significant others in evaluating the quality of life of patients with chronic disease. J. Clin. Epidemiol. 55, 1130–1143 (2002)
A.J. Stenner, M. Smith, D. Burdick, Toward a theory of construct definition. J. Educ. Meas. 20, 4 (1983)
S. Terada, H. Ishizu, Y. Fujusawa, D. Fujita, O. Yokota, H. Nakashima, et al., Development and evaluation of a health-related quality of life questionnaire for the elderly with dementia in Japan. Int. J. Geriatr. Psychiatry 17, 851–858 (2002)
G. Torisson, M.L. Stavenow, E. Londos, Reliability, validity and clinical correlates of the Quality of Life in Alzheimer’s disease (QoL-AD) scale in medical inpatients. Health Qual. Life Outcomes 14, 90 (2016)
R. Trigg, S.M. Skevington, R.W. Jones, How can we best assess the quality of life of people with dementia? The Bath assessment of subjective quality of life in dementia (BASQID). The Gerontologist 47, 789–797 (2007)
L.P. Wan, R.L. He, Y.M. Ai, H.M. Zhang, M. Xing, L. Yang, Y.L. Song, H.M. Yu, Item function analysis on the Quality of Life-Alzheimer’s Disease(QOL-AD) Chinese version, based on the Item Response Theory (IRT). Zhonghua Liu Xing Bing Xue Za Zhi 34(7), 728–731 (2013)
L. Webster, D. Groskreutz, A. Grinbergs-Saull, R. Howard, J.T. O’Brien, G. Mountain, et al., Core outcome measures for interventions to prevent or slow the progress of dementia for people living with mild to moderate dementia: Systematic review and consensus recommendations. PLoS One 12(6), e0179521 (2017)
M.F. Weiner, K. Martin-Cook, D.A. Svetlik, K. Saine, B. Foster, C. Fontaine, The quality of life in late- stage dementia (QUALID) scale. J. Am. Med. Dir. Assoc. 1(3), 114–116 (2000)
P.J. Whitehouse, Harmonization of Dementia Drug Guidelines (United States and Europe): a report of the International Working Group for the Harmonization for Dementia Drug Guidelines. Alzheimer Dis. Assoc. Disord. 14(Suppl 1), S119–S122 (2000)
Study protocol for the World Health Organization project to develop a Quality of Life assessment instrument (WHOQOL). Qual Life Res. 2(2), 153–9 (1993)
M. Wilson, Constructing Measures (Lawrence Erlbaum, Mahwah, 2005)
R. Wittenberg, B. Hu, L. Barraza-Araiza, A. Rehill, Projections of Older People Living with Dementia and Costs of Dementia Care in the United Kingdom, 2019–2040 (Care Policy and Evaluation Centre, London School of Economics and Political Science, London, 2019)
Acknowledgments
I am grateful to Dr. Jolijn Hendriks for her methodical and thorough work on the Rasch scoring of the DEMQOL/DEMQOL-Proxy instruments and Dr. Stefan Cano for his patient advice and encouragement.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Smith, S.C. (2023). Measuring Health-Related Quality of Life in Dementia. In: Fisher, Jr., W.P., Cano, S.J. (eds) Person-Centered Outcome Metrology. Springer Series in Measurement Science and Technology. Springer, Cham. https://doi.org/10.1007/978-3-031-07465-3_3
Download citation
DOI: https://doi.org/10.1007/978-3-031-07465-3_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-07464-6
Online ISBN: 978-3-031-07465-3
eBook Packages: Physics and AstronomyPhysics and Astronomy (R0)