Abstract
There is a growing need for upstream suicide prevention in schools as well as guidance for program implementation that can maximize effectiveness and sustainability. This chapter highlights the benefits of using an implementation science framework to guide partnerships between schools, community partners, and healthcare organizations to enhance youth suicide prevention efforts. Examples illustrating this approach using the PAX Good Behavior Game and the Signs of Suicide Prevention Program (SOS) are described. Finally, policy implications and future directions are discussed.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
Suicide is the second leading cause of death among school-aged youth aged 10–19, and the sharpest increase in number of suicides occurs between early adolescence and young adulthood. Moreover, the majority of those who have ever considered or attempted suicide first did so during their youth (Nock et al., 2013). Ayer and colleagues (Chap. 4, this volume) emphasize that schools provide a context for meaningful suicide prevention activity. Effective school-based suicide prevention programs modify school culture, enhance connectedness, and improve student help-seeking attitudes while reducing mental health stigma. Suicide prevention programs in schools can reduce self-reported suicidal behavior among students and improve school staff confidence and competence in identifying and supporting students at risk for suicide (Aseltine et al., 2007; Wasserman et al., 2015). However, if programming is time-limited or fails to attend to the local needs of the community, benefits do not extend beyond a year or two (Garraza et al., 2019). Faced with limited resources, schools often use a piecemeal approach to prevention, reducing the effectiveness and level of sustainability necessary to maintain reductions in student suicidal behaviors. Schools and communities need to know not only what programs work but how to implement those programs for them to take root and fit into an existing array of supports.
This chapter highlights the role of implementation science and quality improvement strategies to improve school engagement, staff buy-in, and program sustainability. We discuss the role of hospital-school-community partnerships in enhancing the delivery of upstream suicide prevention efforts using the PAX Good Behavior Game (elementary) and the SOS Signs of Suicide Prevention Program (secondary) as examples. We highlight gaps in research regarding the effectiveness of suicide prevention programs as well as ideal dissemination strategies. Recommendations are provided to support how schools and communities can maximize implementation and sustainability.
Implementation Science Framework
It is important to frame our discussion with a few basic assumptions drawn from the implementation science literature. First, suicide prevention efforts should have clearly operationalized outcomes, and programs need to be tested rigorously to gauge effectiveness of implementation in the real world. Suicide prevention knowledge and attitude improvements are important in assessing a program’s relative value, but a change in student and staff behaviors should also be prioritized by evaluation (e.g., increased help-seeking behaviors and linkage rates or reduced suicide attempts, hospital admissions, and suicide deaths). Second, prevention program outcomes tend to be positively linked with implementation fidelity (Durlak & Dupre, 2008). Implementation fidelity, or the degree to which a program is implemented as planned and originally evaluated, requires that programs have well-articulated core elements that can be replicated by schools. However, it is also necessary to balance program fidelity with flexibility as perfect implementation fidelity is unrealistic in school settings. Taking an overly rigid or prescriptive approach may inadvertently reduce program adoption and ownership by schools. Furthermore, states differ in requirements and support for mental health programming, which may present both opportunities and barriers. Prevention programming should match local needs to maximize school engagement and effectiveness. Lastly, sustainability should be part of planning from the very beginning. Shared decision-making with partners from the school community is critical to buy-in. Empowering local leadership is needed to drive a lasting culture shift around mental health in schools.
Challenges and Opportunities in Schools
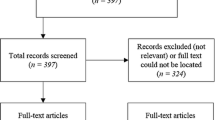
Currently, there are few universal youth suicide prevention programs that have been rigorously evaluated using randomized control trials (RCTs) with strong statistical controls. Furthermore, many outcome evaluations fail to use valid and reliable outcome measures, engage in external peer review processes, or replicate findings (see Miller et al., 2009). Often programs promote certain “active ingredients” thought to be necessary to improve individual or school-level outcomes, but data are unsuited to confirm or refute potential mechanisms of change. Despite these limitations, there are processes known to enhance implementation of suicide prevention efforts which include the following: (1) assessing school needs and readiness for program implementation, (2) developing a strong infrastructure (e.g., hospital-school-community partnerships), (3) building capacity in the school while providing technical assistance, and (4) maintaining fidelity while focusing on program sustainability.
School Readiness for Suicide Prevention
Although schools represent a setting well situated to identify and support youth at risk for suicide, there are gaps in building capacity and delivering program content with fidelity. A key first step in the implementation process is to determine the readiness of a school community for programming. Implementation partners should evaluate school staff and administrator attitudes toward youth suicide and perceptions of prevention. Mental health education and suicide prevention programs are typically consistent with a school’s values, yet buy-in from leadership is still essential for engagement and sustained success. Leadership investment tends to drive a school’s willingness to dedicate meaningful resources, including staff professional development and classroom time, messaging and family engagement, school-based mental health capacity, and collaboration with local mental health providers. Schools differ considerably with respect to resources, demographic makeup, student needs, and integration of mental healthcare. Certain districts have dedicated staff to drive comprehensive prevention and social emotional learning (SEL) efforts; in other districts, there are not a systematic approach and limited staff to support such efforts. Ideally, suicide prevention is part of a larger K–12 prevention framework with targeted interventions for students with elevated risk or mental health needs.
Assessing School Suicide Prevention Needs
Assessing school suicide prevention needs should involve a review of school and community partners, organizational capacity to deliver programming, and an exploration of barriers to adoption and sustainability. Those who plan to support suicide prevention efforts should have a clear understanding of a school community’s past experiences with student suicide, attempts, and/or loss experiences by the school community. An inventory of local mental health partnerships and crisis supports with clear pathways for student support is also a prerequisite for any programming with depression and suicide screening. Awareness of cultural factors that may influence how emotional distress is expressed and to whom should be explored (see Chu et al., Chap. 11, this volume), recognizing that program adaptations and additional community engagement may be needed. Attention to historically marginalized groups and potential barriers to access of local resources are critical for planning and universal implementation (see Cwik et al., Chap. 16, this volume; Rubin et al., Chap. 13, this volume; Sheftall & Boyd, Chap. 12, this volume). Many schools have a desire to engage in suicide prevention, but implementation will often falter if there is not a strong level of guidance and collaboration around the issues noted above. External partners such as hospitals or other mental health agencies can support implementation by playing a role in convening meetings, listening to concerns, problem-solving, offsetting funding, and maintaining the momentum of school efforts.
Ensuring Sustainability
The adoption and implementation phase of a suicide prevention program is critical, but for lasting impact to be achieved, a focus on maintenance and sustainability is required. The same factors that drive success in the adoption phase may differ from those that predict success with continued delivery (Durlak & Dupre, 2008). It is common for there to be a decline in program effectiveness unless there is ongoing attention to fidelity, training, and organizational change. Problems can arise as drift from fidelity occurs and buy-in and energy around an initiative can wane. Champion turnover (i.e., the loss of a key school partner) can lead to a decline in enthusiasm, administrative capacity, and delivery skill. Diffusion of program ownership can also occur. Sustainable prevention and the institutional memory of a program should not exist in one person, or it is at high risk for failure should a role change occur. Making sure there are multiple individuals with “skin in the game” and elements of the program embedded within the school culture are key to ongoing efforts.
Several strategies exist to combat these barriers. Regular, transparent communication and two-way feedback is needed at all stages of implementation. Implementation partners should provide tools and create accessible resources for staff and students, given that school staff face many competing demands. Providing direct reinforcement, such as appreciation for their commitment, data illustrating the effectiveness of their efforts (e.g., number of youths who were identified and linked with care), and training and resources delivered at a frequency that keeps efforts top of mind without being overwhelming is ideal. Programs should seek out staff and student input regularly and incorporate changes in an iterative fashion. Family engagement should be prioritized to enhance community commitment. Program champions can be nurtured through collaborative planning meetings, continuous education, and communities of practice to learn from other schools (Flaspohler et al., 2012). Virtual trainings and consultation can enhance connection and reduce barriers for geographically isolated schools and overcome barriers posed by the recent pandemic (see Michael & Ramtekkar, Chap. 17, this volume).
Implementation in Action: Examples from Nationwide Children’s Hospital
As part of an effort to expand behavioral health services in the community, Nationwide Children’s Hospital (NCH) has focused on the dissemination and implementation of two universal suicide prevention programs to increase awareness, enhance early identification, and reduce youth suicide rates in the community. Throughout central and southeastern Ohio, elementary schools are offered the PAX Good Behavior Game (PAX GBG), and middle and high schools are offered an enhanced Signs of Suicide Prevention Program (SOS). These programs are offered without cost, taking a “fidelity with flexibility” approach. Both programs were selected on the basis of replicated outcome data reflecting consistent reductions in youth suicidal behaviors. PAX GBG is a universal prevention model that is implemented in schools by classroom teachers and aims to improve student self-regulation skills by promoting a nurturing school environment and prosocial student behaviors. PAX GBG targets early risk factors and fosters resiliency in elementary-aged children. Longitudinal examination shows that elementary students in PAX GBG classrooms are less likely to experience behavioral disorders, substance use, and suicidal ideation in adolescence and young adulthood (Wilcox et al., 2008).
SOS is a universal suicide prevention program delivered in middle schools and high schools that combines three critical best-practice features: (1) gatekeeper training for staff, (2) student education and guidance for seeking support, and (3) universal screening. These elements increase awareness about suicide, reduce stigma, inform students of crisis resources, and teach action steps to respond to someone displaying warning signs of suicide. SOS helps identify vulnerable students using several approaches (e.g., self-referral, standardized screening, and referral by a concerned peer/adult). In multiple RCTs, SOS has led to approximately 40–64% reductions in student self-reported suicide attempts, greater knowledge of depression and suicide, and more adaptive attitudes toward these issues (Aseltine & DeMartino, 2004; Aseltine et al., 2007; Schilling et al., 2016). These studies also find that staff display increased competence and confidence when managing at-risk students which empowers school staff to sustain this work.
Implementation of PAX GBG and Sustainability Considerations
NCH has invested in the dissemination of the PAX GBG since 2013 viewing it as a critical upstream prevention program aimed at reducing risk factors and promoting resilience. Initially, NCH primarily provided implementation and consultation support to local schools in an urban context but has since expanded efforts to include numerous rural counties. In partnership with local community agencies, including mental health boards and behavioral health agencies, the hospital supports a multi-county regional PAX GBG initiative. Three overarching research-based themes guide the hospital’s approach to sustainable PAX GBG expansion:
-
1.
Community Partnerships: The hospital sought to maximize community partnerships by including key leadership representatives from all agencies that have roles in the initiative to facilitate buy-in and shared ownership. Ongoing stakeholder meetings were held to review progress and to facilitate bidirectional feedback and continuous quality improvement efforts. Community partners took active roles in building connections with local schools and collaborators to increase local commitment to the initiative over time. Local coaches/champions (called “PAX partners”) were recruited and trained to support implementation efforts in each region. Finally, a braided funding model combining local, state, and hospital funding was leveraged to expand dissemination and available consultants within the communities served.
-
2.
Consulting: NCH took on a consulting role to support local PAX partners. These individuals were recruited and embedded in schools as a means to increase local and regional knowledge and the capacity to implement the program in the long term. Emphasis was placed on developing the expertise of local coaches through learning collaboratives, technical assistance, opportunities for PAXIS trainings, and individualized consultation.
-
3.
Sustainability: Sustainability is discussed at the onset of partnerships with the school and local stakeholders. Sustainability plans are developed in alignment with Positive Behavioral Interventions and Supports (PBIS) and other school initiatives. A 2-year cycle of support is provided with the goal of gradually increasing local capacity to implement PAX GBG independently with the help of local coaches and school-based champions by the end of the second year.
Signs of Suicide: Scaling Up Universal Suicide Prevention with a Focus on Sustainability
The Center for Suicide Prevention and Research (CSPR) at NCH was created in 2015 to address the growing need for youth suicide prevention in Ohio with a focus on implementation of evidence-based programming and long-term viability in schools. Most schools engaged by the CSPR had never implemented a formal suicide prevention program, and other schools had embarked on time-limited efforts that ended as grants expired or as motivated partners left the table. Such outcomes demanded a different way of thinking about engagement, training, and resource utilization for suicide prevention to become a priority. Traditional approaches to program adoption have involved a partnership between a mental health organization and a school where an outside organization delivers the suicide prevention program often in collaboration with school-based mental health providers or counselors. This can result in the incomplete administration of a program or reduced levels of staff competence and effectiveness. Moreover, internal capacity to address youth suicide risk often diminishes when partnering organizations leave the building. NCH takes a different approach to training and implementation. Hospitals with a prevention focus can serve as implementation partners with an emphasis on training and practical support throughout the most challenging pieces of implementation with an eye toward independent delivery over the course of approximately 2–3 years depending on capacity and resources.
CSPR staff engage schools in an effort to build suicide prevention infrastructure in a way that addresses the unique needs of a school community. Implementation staff are licensed professional counselors and social workers with specialized training in suicide prevention, risk assessment, and safety planning. CSPR staff guide schools through two planning meetings to gauge readiness, walk through program elements, and identify school staff to support SOS implementation. Four trainings occur before SOS classroom implementation including (1) a 90-minute staff gatekeeper training to teach awareness, competence in identifying and responding to at-risk students, and confidence in using these skills, (2) a 60-minute parent/community suicide prevention gatekeeper training, (3) a 90-minute classroom presenter training to support teacher implementation of SOS curriculum and strategies for discussing suicide with youth, and (4) a 90-minute triage training to support counselors and support staff to administer and respond to positive depression/suicide screens and determine need for further risk assessment and safety planning. Following these trainings, students engage in one to two class periods of SOS program content which involves learning about depression and the risk factors and warning signs of suicide, viewing videos and discussing effective strategies to support friends displaying warning signs, and education around how to access help for yourself or a friend. This curriculum is followed by a brief depression/suicide screening. Students are also given response cards each day to request counselor support for themselves or a friend. Student screening responses are reviewed and categorized by school staff so that students with elevated suicide risk receive same-day risk assessments by onsite clinicians who obtain consent from parents/guardians and remain in communication throughout the process. Subsequently, recommendations for local services and an appropriate level of care are provided to parents. After the program is delivered, the implementation team engages in a school debriefing session held to identify opportunities for improving SOS processes. Outcomes are shared with the school and adjustments are discussed to be implemented the following year.
Sustainability is a critical goal emphasized from the first meeting. In order to build response capacity, CSPR staff provide district- or county-wide trainings in suicide risk assessment and collaborative safety planning which increase the number of community providers who are able to support school screening efforts. Local mental health partners are engaged both as referral options and as prevention partners. Initially, CSPR staff support risk assessment and safety planning on site, but providers and local mental health boards are engaged with the aim of connecting them to the schools as prevention partners to maximize sustainability. Typically, CSPR staff support is reduced by about 50% in year two, and by year three most schools can provide enhanced SOS and screening with brief consultation and planning support. The CSPR has initiated virtual communities of practice to share lessons learned and best practices in school-based suicide prevention. An evaluation of the factors that promote adoption and sustainability is a vital next step.
Policy Recommendations
-
1.
School districts should invest in K–12 evidenced-based SEL programs that promote resiliency and reduce risk factors for suicide. Universal, suicide-specific programs should be integrated into such initiatives to maximize impact.
-
2.
Diverse partners (such as schools, parents, youth, and mental health organizations) should be engaged to increase ownership, community buy-in, and momentum for suicide prevention efforts which is critical for successful program implementation and for driving lasting change in the school culture around mental health and suicide.
-
3.
The implementation of school-based suicide prevention programs should incorporate a plan for sustainability throughout the prevention program cycle – from initial planning to implementation and evaluation. Tailoring the program implementation plan with school needs in mind, including training, coaching, and consultation, in collaboration with behavioral health partners is ideal.
-
4.
Consider intentionally cultivating school-based champions to lead suicide prevention efforts, sustain them overtime, and embed programs into school culture. This effort should include robust plans for gatekeeper training, continuous education, and local communities of practice.
-
5.
There should be investment by state and federal agencies in the development and evaluation of youth suicide prevention programs with an emphasis on fidelity with flexibility to meet the unique needs and available resources of schools with attention to prevention systems that can support sustained implementation.
Conclusion
Schools provide an important and meaningful context in which suicide prevention can occur. Schools leaders need to know not only which prevention programs work but also how to implement and sustain these programs with fidelity and flexibility to meet the needs of the community. Benefits from suicide prevention programs are fleeting when limited to a single training. Therefore, the implementation of school-based suicide prevention programs should incorporate a plan for sustainability throughout the prevention program cycle. Connecting community partners, local behavioral health organizations, and school-based champions is critical for creating lasting change. School and community cultures focused on sustainable suicide prevention can maintain gains, even after initial funding ends.
References
Aseltine, R. H., & DeMartino, R. (2004). An outcome evaluation of the SOS suicide prevention program. American Journal of Public Health, 94, 446–451. https://doi.org/10.2105/ajph.94.3.446
Aseltine, R. H., Jr., James, A., Schilling, E. A., & Glanovsky, J. (2007). Evaluating the SOS suicide prevention program: A replication and extension. BMC Public Health, 7, 161. https://doi.org/10.1186/1471-2458-7-161
Durlak, J. A., & DuPre, E. P. (2008). Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affecting implementation. American Journal of Community Psychology, 41, 327–350. https://doi.org/10.1007/s10464-008-9165-0
Flaspohler, P. D., Meehan, C., Maras, M. A., & Keller, K. E. (2012). Ready, willing, and able: Developing a support system to promote implementation of school-based prevention programs. American Journal of Community Psychology, 50, 428–444. https://doi.org/10.1007/s10464-012-9520-z
Godoy Garraza, L., Kuiper, N., Goldston, D., McKean, R., & Walrath, C. (2019). Long-term impact of the Garrett Lee Smith Youth Suicide Prevention Program on youth suicide mortality, 2006–2015. Journal of Child Psychology and Psychiatry, 60, 1142–1147. https://doi.org/10.1111/jcpp.13058
Miller, D. N., Eckert, T. L., & Mazza, J. J. (2009). Suicide prevention programs in the schools: A review and public health perspective. School Psychology Review, 38, 168–188.
Nock, M. K., Green, J. G., Hwang, I., McLaughlin, K. A., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2013). Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry, 70(3), 300–310. https://doi.org/10.1001/2013.jamapsychiatry.55
Schilling, E. A., Aseltine, R. H., Jr., & James, A. (2016). The SOS suicide prevention program: Further evidence of efficacy and effectiveness. Prevention Science, 17, 157–166. https://doi.org/10.1007/s11121-015-0594-3
Wasserman, D., Hoven, C., Wasserman, C., Wall, M., Eisenberg, R., et al. (2015). School-based suicide prevention programmes: The SEYLE cluster-randomised, controlled trial. Lancet, 385, 1536–1544. https://doi.org/10.1016/S0140-6736(14)61213-7
Wilcox, H. C., Kellam, S., Brown, C. H., Poduska, J., Ialongo, N., Wang, W., & Anthony, J. (2008). The impact of two universal randomized first- and second-grade classroom interventions on young adult suicide ideation and attempts. Drug & Alcohol Dependence, 95(Suppl 1), S60–S73.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Ackerman, J.P., Khoury, O., Boddapati, S. (2022). Implementation and Dissemination Strategies for School-Based Suicide Prevention Programs. In: Ackerman, J.P., Horowitz, L.M. (eds) Youth Suicide Prevention and Intervention. SpringerBriefs in Psychology(). Springer, Cham. https://doi.org/10.1007/978-3-031-06127-1_5
Download citation
DOI: https://doi.org/10.1007/978-3-031-06127-1_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-06126-4
Online ISBN: 978-3-031-06127-1
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)