Abstract
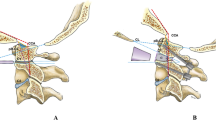
Basilar invagination (BI) and chronic atlanto-axial dislocation (AAD) are the most common congenital anomalies of the CVJ, can occur combined and become symptomatic when produce a ventral cervicomedullary compression. The standard transoral approach (TOA) allows a satisfactory surgical exposure and decompression in more then 80% of patients with BI and AAD. In cases of limited mandibular excursion (i.e. interdental space ≤30 mm) and/or severe basilar invagination (odontoid tip projecting ≥20 mm above the Chamberlain’s line) with a resultant neural compression at the level of the nasopharynx, the endonasal endoscopic approach is an effective alternative option. In patients with tonsillar prolapse and basilar invagination, transoral decompression allows the ascent of cerebellar tonsils into the posterior fossa and the resolution of associated syringomyelia due to the restoration to normal of CSF flow at the CVJ level. The occurrence of acute or delayed spinal instability (occipito-atlantal, atlanto-axial, or occipito-atlanto-axial instability) after transoral decompression is invariably high and requires posterior fixation and fusion. In our experience, the single anesthesia transoral decompression and subsequent posterior fusion eliminate the risk of postoperative instability and allow to mobilize the patients as soon as possible. After an adequate learning curve and following the basic tenets of skull base surgery, the approach related-morbidity in standard TOA is less than 10%.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Chamberlain WE. Basilar impression (platybasia). A bizzarre developmental anomaly of the occipital bone and upper cervical spine with striking and misleading neurologic manifestations. Yale J Biol Med. 1939;11:487–96.
Hadley MN, Spetzler RF, Sonntag VKH. The transoral approach to the superior cervical spine. A review of 53 cases of extradural cervicomedulary compression. J Neurosurg. 1989;71:16–23.
Menezes AH, VanGilder JC, Graf CJ, McDonnell DE. Craniocervical abnormalities. A comprehensive surgical approach. J Neurosurg. 1980;53:444–55.
Perrini P, Benedetto N, Guidi E, Di Lorenzo N. Transoral approach and its superior extensions to the craniovertebral junction malformations: surgical strategies and results. Neurosurgery. 2009;64(5 Suppl 2):331–42.
Kanavel AB. Bullet located between the atlas and the base of the skull: technique of removal through the mouth. Surg Clin Chicago. 1917;1:361–6.
Di Lorenzo N, Fortuna A, Guidetti B. Craniovertebral junction malformations. Clinicoradiological findings, long-term results and surgical indications in 63 cases.J. Neurosurgery. 1982;57:603–8.
Di Lorenzo N. Transoral approach to extradural lesions of the lower clivus and upper cervical spine: an experience of 19 cases. Neurosurgery. 1989;24:37–42.
Di Lorenzo N. Craniocervical junction malformation treated by transoral approach. A survey of 25 cases with emphasis on postoperative instability and outcome. Acta Neurochir. 1992;118:112–6.
Perrini P, Benedetto N, Di Lorenzo N. Transoral approach to extradural non-neoplastic lesions of the craniovertebral junction. Acta Neurochir. 2014;156:1231–6.
Perrini P, Benedetto N, Cacciola F, Gallina P, Di Lorenzo N. Refinement of the transoral approach to the craniovertebral junction malformations. Acta Neurochir Suppl. 2019;125:235–40.
Crockard HA, Johnston F. Development of transoral approaches to lesions of the skull base and craniocervical junction. Neurosurg Q. 1993;3(2):61–82.
Dlouhy BJ, Dahdaleh NS, Menezes AH. Evolution of transoral approaches, endoscopic endonasal approaches, and reduction strategies for treatment of craniovertebral junction pathology: a treatment algorithm. Neurosurg Focus. 2015;38(4):E8.
Menezes AH, VanGilder JC. Transoral-transpharyngeal approach to the anterior craniocervical junction. Ten-year experience with 72 patients. J Neurosurg. 1988;69:895–903.
Menezes AH, Traynelis VC, Gantz BJ. Surgical approaches to the craniovertebral junction. Clin Neurosurg. 1994;41:187–203.
Menezes AH. Surgical approaches: postoperative care and complications “transoral-transpalatopharyngeal approach to the craniocervicxal junction”. Childs Nerv Syst. 2008;24:1187–93.
Menezes AH, Fenoy KA. Remnants of occipital vertebrae: proatlas segmentation abnormalities. Neurosurgery. 2009;64:945–54.
Visocchi M. Transnasal and transoral approach to the clivus and the craniovertebral junction. J Neurosurg Sci. 2019;63(5):498–500.
Sasaki CT, Lowlicht RA, Tokashiki R. Horizontal maxillotomy for exposure of the central skull base: the Yale experience. J Neuro-Oncol. 2001;55:173–7.
James D, Crockard HA. Surgical access to the base of skull and upper cervical spine by extended maxillotomy. Neurosurgery. 1991;29:411–6.
de Almeida JR, Zanation AM, Snyderman CH, Carrau RL, Prevedello DM, Gardner PA, Kassam AB. Defining the nasopalatine line: the limit for endonasal surgery of the spine. Laryngoscope. 2009;119(2):239–44.
El-Sayed IH, Wu JC, Dhillon N, Ames CP, Mummaneni P. The importance of platybasia and the palatine line in patient selection for endonasal surgery of the craniocervical junction: a radiographic study of 12 patients. World Neurosurg. 2011;76(183):188.
Husain M, Rastogi M, Ojha BK, Chandra A, Jha DK. Endoscopic transoral surgery for craniovertebral junction anomalies. Technical note. J Neurosurg Spine. 2006;5:367–73.
Lindley T, Greenlee JD, Teo C. Minimally invasive surgery (endonasal) for anterior fossa and sellar tumors. Neurosurg Clin N Am. 2010;21:607–20.
Fenoy AJ, Menezes AH, Fenoy KA. Craniovertebral junction fusions in patients with hindbrain herniation and syringohydromyelia. J Neurosurg Spine. 2008;9:1–9.
Goel A, Bhatjiwale M, Desai K. Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg. 1998;88:962–8.
Goel A, Desai K. Surgery for syringomyelia: an analysis based on 163 surgical cases. Acta Neurochir. 2000;142:293–302.
Menezes AH. Craniovertebral junction abnormalities with hindbrain herniation and syringomyelia: regression of syringomyelia after removal of ventral craniovertebral junction compression. J Neurosurg. 2012;116(2):301–9.
Dickman CA, Locantro J, Fessler RG. The influence of odontoid resection on stability of the craniovertebral junction. J Neurosurg. 1992;77:525–30.
Naderi S, Crawford NR, Melton MS, Sonntag VK, Dickman CA. Biomechanical analysis of cranial settling after transoral odontoidectomy. Neurosurg Focus. 1999;6(6):Article 7.
Tuite GF, Veres R, Crockard HA, Sell D. Pediatric transoral surgery: indications, complications and long-term outcome. J Neurosurg. 1996;84(4):573–83.
Balasingam V, Anderson GJ, Gross ND, Cheng CM, Noguchi A, Dogan A, McMenomey SO, Delashaw JB Jr, Andersen PE. Anatomical analysis of transoral surgical approaches to the clivus. J Neurosurg. 2006;105:301–8.
Choi D, Crockard HA. Evolution of transoral surgery: three decades of change in patients, pathologies, and indications. Neurosurgery. 2013;73:296–304.
Naderi S, Pamir MN. Further cranial settling of the upper cervical spine following odontoidectomy. Report of two cases. J Neurosurg. 2001;95(2 Suppl):246–9.
Jones DC, Hayter JP, Vaughan ED, Findlay GF. Oropharyngeal morbidity following transoral approaches to the upper cervical spine. Int J Oral Maxillofac Surg. 1998;27:295–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Perrini, P., Benedetto, N., Di Lorenzo, N. (2022). Basilar Invagination and Atlanto-Axial Dislocation. In: Menchetti, P.P.M. (eds) Cervical Spine. Springer, Cham. https://doi.org/10.1007/978-3-030-94829-0_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-94829-0_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94828-3
Online ISBN: 978-3-030-94829-0
eBook Packages: MedicineMedicine (R0)