Abstract
Sleep is critical for a healthy, engaged and satisfying life. A large proportion of our lives is spent asleep, and a large proportion of our housing, resources, expenditure, and attention are dedicated to it. Good sleep strongly predicts better outcomes across a very broad range of life-long health, social, and industrial indices. Poor sleep has very significant and costly impacts upon physical and mental health (including metabolic health, depression, and anxiety), learning and education outcomes, and work-related outcomes (including stress, absenteeism, safety and performance). The social importance of good sleep can be seen in robust associations between sleep and loneliness, isolation, perceived social support, family and interpersonal relationships, and broader community participation and engagement. The availability and power of new sleep tracking devices mean that access and opportunity for satisfactory, satisfying, and sufficient sleep could be greatly increased. In this Chapter, we discuss the importance of sleep for quality of life and the limitations of existing monitoring technologies. We then introduce new tracking technologies and consider their benefits as well as potential pitfalls.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
The Importance of Sleep
Sleep is, broadly, a recuperative and restorative process. As behavior, it is characterized by reduced activity, withdrawal, quiescence, and reduced responsiveness. Put simply, humans typically tend to move to a designated sleep space (such as a bed), lie down, close their eyes and lie still. Sleep is also a very complex neurophysiological process, of which only some features can be readily observed or measured [1], with associated complex changes in physiology, including reduced respiration and heart rate, changes in heart-rate variability, cyclical changes in muscle tone, amongst others.
Humans are regarded as diurnal (day active) animals, and as adults they tend to achieve their major sleep episode during the night-time hours. This timing of sleep is largely governed by circadian processes, and particularly by the evening expression of the hormone melatonin, together with a ‘homeostatic’ increase in the likelihood of sleep, the longer a person is awake. These two processes ideally function to promote regular, consistent, and sufficient sleep. However, the achievement of good sleep also depends on opportunity and environment. In the contemporary context, sleep is often disrupted by choice or by externalities. These can include preferences around work, study, or leisure hours (including engagement in social media, gaming and other device use), education demands, the presence of illness and pain, stress and worry, environmental factors including noise and extremes of temperature, natural and other disasters, and the suppression of melatonin expression by artificial light.
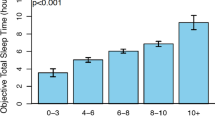
While there is robust debate around the idea of an ‘epidemic of sleeplessness’ [2], many people are not getting sufficient sleep. Current evidence-based recommendations for sleep duration [3] suggest that 7 or more hours of sleep is required by most adults, and that more than 9 hours might be needed by young adults. In contrast, the US Centres for Disease Control report that 30–40% of people habitually achieve fewer than 7 hours of sleep [4], defined as short sleep duration, with almost 70% of high school students sleeping fewer than 8 hours [5]. Although normal sleep duration can vary between individuals, sleep restricted to less than 6 hours per night has been associated with significant impairments in cognitive performance, vigilance, and affect [6].
The effects of sleep loss can be seen very acutely. For example, sleep restricted by just a few hours can be observed in objective performance the next day [7, 8]. However, sleep loss can also accumulate over nights, so that an hour less sleep each night over a week may be equivalent in effect to a full night of sleep deprivation. The impact of chronic partial sleep restriction may not be observed immediately, but may be seen many years later through increased health and mental health problems [9]. This possibility has been raised by data showing strong links between involvement in shift work and later long-term health consequences. This means that sleep needs to be understood across timescales ranging from a single night to decades, and the nature, level, and intensity of measurement needs to reflect those timescales.
The two most common sleep disorders are insomnia and Obstructive Sleep Apnoea (OSA). It is possible that as many as a billion adults globally have Obstructive Sleep Apnoea, with a prevalence approaching 50% in some countries [10, 11]. The prevalence of insomnia may range from 6–10% by strict clinical definitions, to over 30% for poor or unsatisfactory sleep [12]. The direct (medical and industrial) and indirect (social) costs associated with these sleep disorders, and with other forms of poor or disrupted sleep, are very high, e.g. over $680 Billion across just 5 OECD nations [13]. The understanding, identification, and treatment of sleep disorders have seen very rapid growth over the past decade. While current treatment approaches to these disorders are regarded as both effective and cost effective [14, 15], this growth still represents a very high additional cost. Due to the high global burden of OSA and insomnia, health-care systems will face major cost and logistic challenges, and must adopt more effective and efficient diagnostic and management strategies so that the negative health impacts can be minimized. There is a specific and growing need for broader public health, individual health, early intervention, and prevention approaches to sleep health.
Sleep is clearly not a unitary state. Instead, it has distinct dimensions including duration, quality, timing and regularity, each of which can have corresponding objective and subjective meaning. Further, sleep matters for daytime function so that constructs such as daytime alertness, clarity, speed, energy and satisfaction are also very important. This multidimensionality means that approaches to the measurement of sleep by devices must also be multidimensional, or be understood to be constrained to one or more dimensions, in order to understand sleep meaningfully. Another implication is that a measure optimized for measurement along one dimension may not function well to measure another. Rather than asking ‘how well does this device measure sleep’, we might ask ‘what is it about sleep that this device measures’. Sleep science is a relatively new field, and the parallel rise in personal miniaturized sensing technology suggests a great opportunity for increased measurement, and increased range and mode of measurement, to inform new understanding of this complex state.
Individuals are increasingly interested in their own sleep, mirroring increasing public interest and understanding of the role of sleep in overall health and wellbeing alongside nutrition and exercise. Quality of Life Technologies (QoLT) provide immediate feedback through smart devices that people can use in their daily life to assess and enhance their health and well-being [16]. Most sleep tracking devices appear to have achieved the fundamental aims of QoLT, for instance, in that they claim to enable individuals to quantify their sleep through apps or wearable devices. However, important questions remain. Are these devices addressing a need that cannot be met by existing methods? Can they provide an objective and reliable assessment of sleep? Are there potential pitfalls in the use of such devices? Our Chapter aims to cover all these questions.
Why Are Existing Methods Not Adequate?
Sleep disorders are defined by recognized clinical criteria such as the International Classification of Sleep Disorders, ICSD-3 [17], the International Classification of Diseases, ICD-11 [18], and the Diagnostic and Statistical Manual of Mental Disorders, DSM-V [19]. Meeting these criteria generally requires an overnight sleep study using polysomnography (PSG) to confirm the clinical diagnosis of a specialist sleep physician (e.g. for suspected OSA), or may require careful clinical diagnosis by a psychologist without reference to PSG (in the case of insomnia).
Polysomnography (PSG) is regarded as the gold standard for diagnosis of specific sleep disorders (shown in Fig. 7.1). PSG objectively quantifies sleep-related indices from a combination of electroencephalogram (EEG, brain states), electrocardiogram (ECG, cardiac states), electromyogram (EMG, muscle tension), electro-oculogram (EOG, eye movements in sleep) and indices related to sleep disorders such as nasal airway pressure and flow, respiratory effort, infra-red video, sound recording, and blood oxygen saturation. Individuals typically spend one or more nights in a hospital or clinic sleep laboratory, where they are monitored throughout the night, although there is increasing uptake of home-based and limited channel studies [20].
While PSG remains the gold standard for assessment of specific sleep disorders and is an evolved medical technology, it has certain features that limit its use. One or two nights of assessment does not allow for longer-term tracking of change, and does not assess the habitual sleep of individuals in their natural sleep environments and schedules. PSG requires extensive resources including equipment, staff, and software. In addition, it is not always easy for someone to undertake a sleep study when needed as waiting times for access can be considerable [21]. The interpretation of sleep data is another challenge. Variability in the use of established rule sets for visual scoring of the PSG results in unreliability in key PSG outcome indices (such as the Apnea-Hypopnea Index, AHI) both within individual scorers and across laboratories [22], even when a single rule set is adopted [23]. For this reason, automated analysis of studies using Machine Learning have been proposed as a way to reduce scoring variability and error. While these analytical models increase the consistency of scoring, and perform well against expert visual scoring, no single model has achieved widespread acceptance. The promise of neural network models and more recent Artificial Intelligence models has been recognized [24, 25] as a way to increase efficiency and accuracy in sleep medicine, but also to provide a deeper understanding of sleep and circadian biology.
A second key method used to understand sleep is through elicitation of self-reported experience. This approach is required to capture the qualitative or subjective dimensions of sleep [26]. In some cases, this experience cannot be measured objectively (e.g. satisfaction with sleep), or is necessary to understand predictors or consequences of poor sleep (such as increased alcohol use, or poor work performance). This can be done through structured ‘sleep diaries’ or time use surveys [27], or through clinical and non-clinical rating scales and other measures. These measures can be used to complement objective measurements from PSG, or may stand-alone for use in other settings such as epidemiological surveys.
Subjective assessment using instruments such as the Pittsburgh Sleep Quality Index [28] is seen as relatively inexpensive and quick, and for those reasons is often used as an initial screen for sleep diagnosis [29]. However, the use of paper-and-pencil measures in particular can lead to high transcription and scoring costs, significant user effort, and simple measurement error. There is typically a requirement for careful development of subjective measures along sound psychometric principles, and a need for high quality normative studies (e.g. stratified by age, gender, socioeconomics or other factors) to inform meaningful interpretation. This work has been done in a number of recent initiatives, e.g. Yu et al. [30], but these measures are not in widespread use in sleep medicine.
A final common method for sleep and circadian rhythm measurement is actigraphy. This is typically in the form of a wrist-worn ‘movement watch’ based on accelerometry or other movement capture methods and which can be used to measure sleep over extended periods in a naturalistic environment including the person’s home, work, or other settings. Generation of these devices have been widely used in the past two decades for sleep assessment [31].
The American Academy of Sleep Medicine (AASM) provides a guideline to establish clinical practice recommendations for using actigraphy in sleep medicine. The purpose of using actigraphy is not to replace the gold standard of sleep measurement but rather to assist in deriving helpful metrics for sleep disorder assessment and treatment [32]. Actigraphy devices are typically continuously worn for 24-hours a day for several days to months. Sleep parameters are extracted from the movement data via specific sleep detection algorithms [33], and other derivatives such as circadian rhythm parameters and estimates of activity level can also be generated. By using actigraphy, clinicians are able to obtain unique information about sleep in a person’s natural or habitual sleep environment. This can be particularly important when sleep schedules are dictated by work demands (e.g. shift work), circadian phase shifts (e.g. international travel) or other circumstances where variation over time is predicted. Although actigraphy has been well studied and has been validated against PSG in specific populations, there are essential limitations to the concordance between the two approaches. The devices used in research and clinical practice tend to prioritize reliability, standardization, long battery life, and capacity for re-use over other considerations that might be more important for consumer-grade devices.
Methods and Tools for Objective and Quantitative Assessment of Daily Sleep
Consumers now have access to a number of technologies to objectively and quantitatively assess their daily sleep in their home environment. Below we review mobile applications, wearable devices (smartwatches, rings, headbands), as well as co-called ‘nearables’ that are near the individual, embedded in the sleep environment (e.g. in mattresses). Broadly speaking, mobile applications are more widely available to many consumers. Wearables and nearables, on the other hand, are more expensive; yet potentially provide a holistic view of our health and well-being along metrics such as daily activities, heart rate, and sleep. Wearables typically also contain a wider variety of sensor technology such as Electrocardiogram (ECG), Electroencephalogram (EEG) and Photoplethysmogram (PPG), which can lead to more accurate data.
Mobile applications are readily available at the consumer’s fingertips. Consumers can manually record their sleep via sleep diaries or use mobile-embedded sensors to track their sleep automatically. Sleep logs and diaries allow consumers to record their bedtime, number of awakenings, activities before going to sleep and after awakening. There are two main approaches to keep track of sleep diaries: paper and electronic sleep diaries. Tonetti et al. [34] suggested that both methods achieved similar results, whereas electronic sleep diaries provide more benefits over paper diaries in terms of reducing time for data entry and automatically recording the time when the diary is logged. Choe et al. [35] emphasized that electronic sleep diaries are more beneficial to individuals when the diary application is quick to use, engaging, and encourages self-reflection.
Automatic sleep tracking apps require minimal or no data entry. They are easy to use and inexpensive for self-tracking. However, their accuracy is often neglected, and their sleep results are often over claimed. Most sleep apps are not clinically validated against laboratory PSG, the gold standard of sleep tracking, because PSG is labor intensive, expensive and difficult to access. Sleep Cycle, a popular sleep-tracking app, monitors a sleep-wake stage through motion or sound sensors, and provides a summary of sleep quality. Fino et al. [36] showed that the Sleep Cycle app failed to show adequate reliability when compared against PSG for sleep-wake detection. Despite the lack of reliability, Sleep Cycle app has continuously been used widely due to word of mouth (e.g. Editors’ Choice on the Apple App Store in October, 2020), and its potential benefits. Robbins et al. [37] report the use of Sleep Cycle to understand sleep duration and quality for four-year trends in general population. The results reveal helpful information. However, there is still some concern about its reliability and validity of sleep outcomes. Similar to Sleep Cycle, Sleep Time app shows poor correlation with PSG in terms of sleep parameters (e.g., sleep duration and number of awakenings) and sleep-wake stages [38]. Overall, further studies are needed to assess applications’ utility and examine how much trust that we could potentially improve so that we are more confident using it.
Popular smartwatches like the Apple Watch, Samsung Gear and Fitbit become part of our daily living and are potentially helpful to remind us to do more exercise or to sleep more. Current studies [39, 40] investigate the accuracy of using the Apple Watch to determine sleep-wake stages and their results yielded reliable performance compared with a clinical-grade device and PSG. Roomkham’s study suggested that using an Apple Watch to monitor sleep-wake stages could be an add-on to traditional actigraphy as well as a way to study the broader population. Both studies have transparent methods to evaluate the reliability of smartwatches, which increases the confidence in using such devices or adopting their techniques for tracking sleep in medicine, research, and self-tracking. There is clear potential for smartwatches to monitor not only sleep itself but also sleep quality [41].
Smart rings are becoming less intrusive and more attractive for consumers. Smart rings usually contain similar sensors to smartwatches, such as motion, heart rate, pulse rate, and body temperature. A recent investigation of healthy adolescents shows promising sleep outcomes beyond the sleep-wake stage into the whole sleep cycle [42]. However, the ŌURA ring used in this study employs a proprietary sleep algorithm to derive sleep stages, and most studies can only validate the overall sleep outcomes against PSG.
A variety of headbands exist that track sleep through EEG sensors around the head. At the time of writing, the Dreem headband is a popular choice amongst consumers and researchers. The Dreem headband is able to measure brain activity (EEG), breathing, and movement. The results of heart rate, breathing frequency and respiratory rate variability are reliable which resulted in providing precision sleep stages and sleep parameters [43].
Nearables [44] are another type of consumer-grade device. They are placed near the sleep environment, e.g. under the mattress or on the bedside table. An example of nearables is the Beddit Sleep tracker, which measures heart rate through ballistocardiography (BCG) derived from pressure sensors under the mattress. Tuominen et al. [45] reported that the accuracy of the sleep tracking is low and that consumers should be careful interpreting these results. Similar with other types of consumer-grade devices, total sleep time was overestimated, and wake after sleep onset underestimated. These results were also based on healthy participants only, and the reliability of such devices for users with obstructive sleep apnea, insomnia, and other types of sleep disorders is unclear. Another example is the DoppleSleep [46], a contactless sleep system that is placed next to the bed and uses radar signals to gather movement, heart rate, and breathing data. It performed well for sleep-wake classification (~90% recall), and to a lesser extent on sleep staging (~80% recall for REM vs. Non-REM). The S+ system by ResMed is another nearable, which relies on ultra-low power radiofrequency waves to monitor the user’s movements and breathing. Schade et al. [47] evaluated it against PSG and actigraphy and reported showed good sleep detection accuracy (~93%) and lower wake detection accuracy (69–73%), as for most devices. It is worth noting that wake detection was better than actigraphy (at 48%), thanks to a higher accuracy in detecting wake before sleep onset.
Overall, it is important that convenience does not come at the expense of the accuracy and usefulness of the information that can be derived from consumer-grade devices [49]. Recent work from Depner et al. [48] identified important metrics for sleep using wearable devices, and circadian metrics that may influence sleep (such as a level of exercise, which can be captured passively through the wearable devices). Tables 7.1 and 7.2 capture important metrics that are essential for validation against the gold standard.
Another crucial consideration is that when the sleep algorithm is provided by the device manufacturer, it is often a proprietary black box. One consequence is that data consistency is at the mercy of a software update over which the users often have no control. This can be a problem, especially for long-term tracking. The device may also suddenly disappear from the market. Users, in particular in a research context, should favor devices that provide access to the raw data and allow the deployment of open algorithms, and tracking methods that have been validated for a broad range of users (age, healthy vs. sleep disorders, etc.).
Benefits, Limitations, and Potential Pitfalls
There are many benefits for consumers from having relatively easy access to sleep data from apps, wearables and nearables. A major benefit is a better awareness of sleep. People often purchase devices for other purposes, e.g. to track steps, and sleep data comes as a bonus [50, 51]. Once people have access to sleep data, they are curious about what the data may tell them about themselves, and whether they can see any trends. Based on such data, sleep may become more of a priority because they become more conscious of how much sleep they actually get, as well as how much sleep they ought to get for a healthy night of sleep. Having an awareness of sleep and tracking sleep often goes hand in hand with goal setting, e.g. aiming for at least 7 hours of sleep. Many apps provide virtual rewards for getting enough sleep that can increase motivation [52]. However, the main challenge here is that (unlike with the number of steps walked) people cannot voluntarily control how much time they spend in a particular sleep stage. Another benefit is the ability to explore links between sleep and other quality of life data, e.g. to identify if you sleep more on days when you exercise [50]. Exploring such links in the data is particularly useful for people with sleep disorders and other chronic conditions, who seek to identify reasons for their sleep problems and other health conditions [53]. Going one step further, some people benefit from experimenting based on sleep and other quality of life data. For example, members of the Quantified Self community—a worldwide community of self-tracking enthusiasts—report self-experiments with sleep. These include experiments to improve sleep, e.g. by changing their sleep patterns, environmental aspects like reducing the noise and light in their bedroom, or sleep health strategies such as reducing their caffeine consumption. Conversely, sleep data also allows for experiments on the impact of sleep on other lifestyle factors, e.g. if they feel more alert at work and in everyday life [54].
Studies of consumers tracking their own sleep highlight also several challenges and pitfalls. In collecting and organizing data, consumers face the challenge of working with potentially inaccurate data, e.g. because accelerometer data alone cannot reliably determine insights into sleep stages (without EEG data), and accelerometer may also inadvertently respond to the movements of partners in the same bed [55]. Consumer devices that contain EEG sensors potentially provide more accurate data, but the downside is that they are often uncomfortable to wear and impede sleep, and as a result are not worn for longer periods of time [56]. Consumers also report that they lack information on triggers (e.g. why they went to bed late) and contextual information (e.g. their stress and wellbeing) that may help to explain sleep data [54]. Even when consumers track such information through other means, they may not have the skills and tools to confidently relate data from different devices and sources to establish relationships, cause and effect [50].
The interpretation of sleep data also poses several challenges to consumers. People often report a lack of time to revisit and interpret data [57]. Sleep data can be overwhelming or even stressful when the desired outcomes do not materialize [58]. Particular information about sleep stages can be difficult to interpret, because we do not consciously experience sleep stages, nor is the relationship between objective sleep stages and subjective sleep quality clear to consumers [53]. A related challenge is that sleep data and what might objectively constitute quality sleep (e.g. more than 8 hours of sleep), may not relate to how consumers experience sleep or how refreshed they feel when they wake up [56]. There appears to be a disconnect between the various scientific metrics for quantifying sleep (e.g. sleep efficiency and sleep stages) and the way people experience and understand their sleep, which is more aligned with sleep duration and how satisfied or alert they feel as a result [59]. Unfortunately, this disconnect is not helped by the fact that most consumer devices are black boxes that conceal how data is collected and processed, which is partly a result of the complexity of sensor hardware and algorithms used [56], but partly also a deliberate choice of companies to protect their intellectual property [60].
A final challenge for sleep-trackers is that seeing a problem in the data is not the same as finding an opportunity to change it [61]. If our fitness-tracking device tells us that we have not achieved our 10,000 steps goal, then we can at least in principle remedy this by going for an extended walk. On the other hand, if the same device tells us that we only get 5 hours of sleep or not enough deep sleep, then the opportunity to change this is less clear [50, 62]. We can change the sleep environment (e.g. block out light with curtains) and we can also improve our sleep hygiene (e.g. reduce the consumption of caffeinated products) to increase the chances of getting more sleep, but we cannot voluntarily control sleep itself [53]. Furthermore, in making adjustments to our environment and sleep hygiene we often face external constraints, e.g. we may not be able to adjust the start time for school or work to better suit our own sleep needs, nor do we have control over autonomous conditions like our mood, stress, and hormone cycle [50].
To help mitigate these challenges, sleep-tracking at home is often conducted in collaboration with others. Family members, and especially bed partners, can play a vital role in supporting sleep tracking. Parents and older siblings often need to set up technology, interpret data, encourage healthy sleep hygiene, manage medical appointments, etc. [63]. Health professionals continue to play a crucial role to interpret the data, ask questions to reflect on sleep, and to provide advice on what actions to take [64].
Coming back to our original question, we have shown that personal sleep tracking technologies can improve quality of life by increasing awareness of sleep, and by offering opportunities to explore connections with other quality of life data and potential sleep problems. However, we have also shown that collecting data, making sense of it to take action can be difficult and perhaps even overwhelming, because it requires expertise on sleep and tracking technology. We hope that this chapter will provide a useful introduction to these issues to get the most out of quantifiable sleep data. However, we also add a note of caution: quantification is important, but sleep cannot yet be reduced to a collection of measures. As we have discussed above, there is a mismatch between scientific sleep metrics and our subjective experience of sleep. Quantifying sleep also invites people to search for signs of sleep problems, instead of promoting good sleep health [59]. No matter how elaborate, measures will always only provide a partial picture of sleep. A complete picture requires complementary information from subjective assessments, a broad perspective (overall health, but also inputs and interactions with other Quality of Life indicators), and an understanding of the varying needs and concerns of different individuals over a life course.
References
Dement WC. The stanford sleep book. 2006.
Marshall NS, Lallukka T. Sleep pirates-are we really living through a sleep deprivation epidemic and what’s stealing our sleep? Eur J Pub Health. 2018;28(3):394–5.
Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, Kushida C, Malhotra RK, Martin JL, Patel SR, Quan SF, Tasali E. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of sleep medicine and Sleep Research Society. Sleep. 2015;38(6):843–4.
Shockey TM, Wheaton AG. Short sleep duration by occupation group–29 states, 2013–2014. Morb Mortal Wkly Rep. 2017;66:207–13.
Wheaton AG, Jones SE, Cooper AC, Croft JB. Short sleep duration among middle school and high school students–United States, 2015. Morb Mortal Wkly Rep. 2018;67:85–90.
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, Hazen N, Herman J, Katz ES, Kheirandish-Gozal L, Neubauer DN. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–3.
Belenky G, Wesensten NJ, Thorne DR, Thomas ML, Sing HC, Redmond DP, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12(1):1–12.
Rossa KR, Smith SS, Allan AC, Sullivan KA. The effects of sleep restriction on executive inhibitory control and affect in young adults. J Adolesc Health. 2014;55(2):287–92.
Kecklund G, Axelsson J. Health consequences of shift work and insufficient sleep. BMJ. 2016;355:i5210.
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MS, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL, Peppard PE. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7(8):687–98.
Lyons MM, Bhatt NY, Pack AI, Magalang UJ. Global burden of sleep-disordered breathing and its implications. Respirology. 2020;25:690–702.
Morin CM, Jarrin DC. Epidemiology of insomnia: prevalence, course, risk factors, and public health burden. Sleep Med Clin. 2013;8(3):281–97.
Hafner M, Stepanek M, Taylor J, Troxel WM, Van Stolk C. Why sleep matters–the economic costs of insufficient sleep: a cross-country comparative analysis. Rand health quarterly. 2017;6(4)
Reynolds SA, Ebben MR. The cost of insomnia and the benefit of increased access to evidence-based treatment: cognitive behavioral therapy for insomnia. Sleep Med Clin. 2017;12(1):39–46.
Streatfeild J, Hillman D, Adams R, Mitchell S, Pezzullo L. Cost-effectiveness of continuous positive airway pressure therapy for obstructive sleep apnea: health care system and societal perspectives. Sleep. 2019;42(12):zsz181.
Wac K. Quality of life technologies. In: Gellman M, editor. Encyclopedia of behavioral medicine. New York, NY: Springer; 2020. https://doi.org/10.1007/978-1-4614-6439-6_102013-1.
American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014.
World Health Organization International classification of diseases for mortality and morbidity statistics (11th revision). 2018. Retrieved from https://icd.who.int/browse11/l-m/en
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013.
Corral J, Sánchez-Quiroga MÁ, Carmona-Bernal C, Sánchez-Armengol Á, de la Torre AS, Durán-Cantolla J, Egea CJ, Salord N, Monasterio C, Terán J, Alonso-Alvarez ML. Conventional polysomnography is not necessary for the management of most patients with suspected obstructive sleep apnea. Noninferiority, randomized controlled trial. Am J Respir Crit Care Med. 2017;196(9):1181–90.
Rotenberg BW, George CF, Sullivan KM, Wong E. Wait times for sleep apnea care in Ontario: a multidisciplinary assessment. Can Respir J. 2010;17
Collop NA. Scoring variability between polysomnography technologists in different sleep laboratories. Sleep Med. 2002;3(1):43–7.
Ruehland WR, O'Donoghue FJ, Pierce RJ, Thornton AT, Singh P, Copland JM, Stevens B, Rochford PD. The 2007 AASM recommendations for EEG electrode placement in polysomnography: impact on sleep and cortical arousal scoring. Sleep. 2011;34(1):73–81.
Goldstein CA, Berry RB, Kent DT, Kristo DA, Seixas AA, Redline S, Westover MB. Artificial intelligence in sleep medicine: background and implications for clinicians. J Clin Sleep Med. 2020;16(4):609–18.
Stephansen JB, Olesen AN, Olsen M, Ambati A, Leary EB, Moore HE, et al. Neural network analysis of sleep stages enables efficient diagnosis of narcolepsy. Nat Commun. 2018;9(1):1–15.
Shahid A, Wilkinson K, Marcu S, Shapiro CM, editors. STOP, THAT and one hundred other sleep scales. Springer Science & Business Media; 2012.
Carney CE, Buysse DJ, Ancoli-Israel S, Edinger JD, Krystal AD, Lichstein KL, Morin CM. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. 2012;35(2):287–302.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Ibáñez V, Silva J, Cauli O. A survey on sleep assessment methods. PeerJ. 2018;6:e4849.
Yu L, Buysse DJ, Germain A, Moul DE, Stover A, Dodds NE, Johnston KL, Pilkonis PA. Development of short forms from the PROMIS™ sleep disturbance and sleep-related impairment item banks. Behav Sleep Med. 2012;10(1):6–24.
Ancoli-Israel S, Cole R, Alessi C, et al. The role of actigraphy in the study of sleep and circadian rhythms. American Academy of sleep medicine review paper. Sleep. 2003;26(3):342–92.
Smith MT, McCrae CS, Cheung J, Martin JL, Harrod CG, Heald JL, Carden KA. Use of actigraphy for the evaluation of sleep disorders and circadian rhythm sleep-wake disorders: an American Academy of sleep medicine clinical practice guideline. J Clin Sleep Med. 2018;14(7):1231–7.
Martin JL, Hakim AD. Wrist actigraphy. Chest. 2011;139(6):1514–27.
Tonetti L, Mingozzi R, Natale V. Comparison between paper and electronic sleep diary. Biol Rhythm Res. 2016;47(5):743–53.
Choe EK, Consolvo S, Watson NF, Kientz JA. Opportunities for computing technologies to support healthy sleep behaviors. In: Proceedings of the SIGCHI conference on human factors in computing systems; 2011. p. 3053–62.
Fino E, Plazzi G, Filardi M, Marzocchi M, Pizza F, Vandi S, Mazzetti M. (not so) smart sleep tracking through the phone: findings from a polysomnography study testing the reliability of four sleep applications. J Sleep Res. 2020;29(1):e12935.
Robbins R, Affouf M, Seixas A, Beaugris L, Avirappattu G, Girardian J-L. Four-year trends in sleep duration and quality: a longitudinal study using data from a commercially available sleep tracker. J Med Internet Res. 2020;22(2):e14735.
Bhat S, Ferraris A, Gupta D, Mozafarian M, DeBari VA, Gushway-Henry N, Gowda SP, Polos PG, Rubinstein M, Seidu H, Chokroverty S. Is there a clinical role for smartphone sleep apps? Comparison of sleep cycle detection by a smartphone application to polysomnography. J Clin Sleep Med. 2015;11(7):709–15.
Roomkham S, Hittle M, Cheung J, Lovell D, Mignot E, Perrin D. Sleep monitoring with the apple watch: comparison to a clinically validated actigraph. F1000Research. 2019;8(754):754.
Walch O, Huang Y, Forger D, Goldstein C. Sleep stage prediction with raw acceleration and photoplethysmography heart rate data derived from a consumer wearable device. Sleep. 2019;42(12):zsz180.
Alfeo AL, Barsocchi P, Cimino MG, La Rosa D, Palumbo F, Vaglini G. Sleep behavior assessment via smartwatch and stigmergic receptive fields. Pers Ubiquit Comput. 2018;22(2):227–43.
de Zambotti M, Rosas L, Colrain IM, Baker FC. The sleep of the ring: comparison of the ŌURA sleep tracker against polysomnography. Behav Sleep Med. 2019;17(2):124–36.
Arnal PJ, Thorey V, Ballard ME, Hernandez AB, Guillot A, Jourde H, et al. The Dreem headband as an alternative to polysomnography for EEG signal acquisition and sleep staging. Sleep. 2019;43(11):662734.
Bianchi MT. Sleep devices: wearables and nearables, informational and interventional, consumer and clinical. Metabolism. 2018;84:99–108.
Tuominen J, Peltola K, Saaresranta T, Valli K. Sleep parameter assessment accuracy of a consumer home sleep monitoring ballistocardiograph beddit sleep tracker: a validation study. J Clin Sleep Med. 2019;15(3):483–7.
Rahman T, Adams AT, Ravichandran RV, Zhang M, Patel SN, Kientz JA, Choudhury T. Dopplesleep: a contactless unobtrusive sleep sensing system using short-range doppler radar. In: Proceedings of the 2015 ACM international joint conference on pervasive and ubiquitous computing; 2015. p. 39–50.
Schade MM, Bauer CE, Murray BR, Gahan L, Doheny EP, Kilroy H, et al. Sleep validity of a non-contact bedside movement and respiration-sensing device. J Clin Sleep Med. 2019;15(7):1051–61.
Depner CM, Cheng PC, Devine JK, Khosla S, de Zambotti M, Robillard R, et al. Wearable technologies for developing sleep and circadian biomarkers: a summary of workshop discussions. Sleep. 2020;43(2):zsz254.
Hunasikatti M. Non-contact sensors: need for optimum information is more important than convenience. J Clin Sleep Med. 2019;15(11):1707.
Liang Z, Ploderer B, Liu W, Nagata Y, Bailey J, Kulik L, Li Y. SleepExplorer: a visualization tool to make sense of correlations between personal sleep data and contextual factors. Pers Ubiquit Comput. 2016;20(6):985–1000.
Whooley, M., Ploderer, B., & Gray, K. On the integration of self-tracking data amongst quantified self. Proceedings of British HCI 2014. 2014. Retrieved from http://tinyurl.com/m3lj2c7
Rooksby J, Rost M, Morrison A, Chalmers M. Personal tracking as lived informatics. In: Proceedings of the SIGCHI conference on human factors in computing systems; 2014. p. 1163–72.
Ravichandran R, Sien SW, Patel SN, Kientz JA, Pina LR. Making sense of sleep sensors: how sleep sensing technologies support and undermine sleep health. In: Proceedings of the 2017 CHI conference on human factors in computing systems; 2017. p. 6864–75.
Choe EK, Lee NB, Lee B, Pratt W, Kientz JA. Understanding quantified-selfers’ practices in collecting and exploring personal data. In: Proceedings of the SIGCHI conference on human factors in computing systems; 2014. p. 1143–52.
Roomkham S, Lovell D, Cheung J, Perrin D. Promises and challenges in the use of consumer-grade devices for sleep monitoring. IEEE Rev Biomed Eng. 2018;11:53–67.
Liang Z, Ploderer B. How does Fitbit measure brainwaves: a qualitative study into the credibility of sleep-tracking technologies. Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies. 2020;4(1):1–29.
Li I, Dey A, Forlizzi J. A stage-based model of personal informatics systems. In: Proceedings of the SIGCHI conference on human factors in computing systems; 2010. p. 557–66.
Lupton D. Data mattering and self-tracking: what can personal data do? Continuum-Journal of Media & Cultural Studies. 2020;34(1):1–13. https://doi.org/10.1080/10304312.2019.1691149
Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):9–17.
Gillespie T. Designed to ‘effectively frustrate’: copyright, technology, and the agency of users. New Media Soc. 2006;8(4):651–69.
Munson SA. Rethinking assumptions in the design of health and wellness tracking tools. Interactions. 2017;25(1):62–5. https://doi.org/10.1145/3168738.
Liu W, Ploderer B, Hoang T. In bed with technology: challenges and opportunities for sleep tracking. In: Proceedings of the annual meeting of the Australian special interest Group for Computer Human Interaction; 2015. p. 142–51.
Pina LR, Sien S-W, Ward T, Yip JC, Munson SA, Fogarty J, Kientz JA. From personal informatics to family informatics: understanding family practices around health monitoring. Paper presented at the Proceedings of the 2017 ACM Conference on Computer Supported Cooperative Work and Social Computing, Portland, Oregon, USA; 2017. https://doi.org/10.1145/2998181.2998362.
Costa Figueiredo M, Chen Y. Patient-generated health data: dimensions, challenges, and open questions. Foundations and trends®. Human-Computer Interaction. 2020;13(3):165–297. https://doi.org/10.1561/1100000080.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Roomkham, S., Ploderer, B., Smith, S., Perrin, D. (2022). Technologies for Quantifying Sleep: Improved Quality of Life or Overwhelming Gadgets?. In: Wac, K., Wulfovich, S. (eds) Quantifying Quality of Life. Health Informatics. Springer, Cham. https://doi.org/10.1007/978-3-030-94212-0_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-94212-0_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94211-3
Online ISBN: 978-3-030-94212-0
eBook Packages: MedicineMedicine (R0)