Abstract
This chapter provides an overview of the evidence linking mobility to quality of life (QoL). The findings showed that the operationalization of QoL varied across studies covering measures of physical or mental health, general health perception, life satisfaction, participation, illness intrusiveness, health-related QoL (HRQL) and global quality of life. These outcomes are sometimes single items or uni-dimensional constructs and sometimes profile measures, rendering the interpretation of findings in our context difficult. This complexity led to a revelation that one could think of QOL of the person differently from the QoL of the body. QoL of the person is best reflected through global QOL measures including those of life satisfaction whereas QoL of the body is reflected in outcomes related to aspects of function including physical, emotional, or psychological impairments, activity limitations and participation restrictions. This chapter will focus on the general construct of mobility, which is considered an activity limitation, and on the causes of limited mobility, impairments of structures and functions needed for mobility. A distinction is made between the between the person’s QoL and the body’s QoL. While the person’s QOL is best self-expressed, the body’s QOL could be monitored in real-time with the assistance of a growing portfolio of personal, wearable technologies. The chapter ends with thoughts about how QoL of the body, and especially mobility, could be monitored and what that future may look like.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
What Is Mobility?
According to Merriam-Webster’s Dictionary mobility is the “ability or capacity to move”.Footnote 1
In the scientific community mobility has been defined “as the ability to move oneself (either independently or by using assistive devices or transportation) within environments that expand from one’s home to the neighborhood and to regions beyond” [1]. The life-space within a person can move has also been recognized as ranging from the person’s room, home, outdoors, and neighborhood to the service community of shops, banks, healthcare facilities etc., surrounding area within person’s own country, and the world. This mobility is recognized to be constrained or influenced by financial, environmental, and psychosocial conditions as well as physical and cognitive capabilities. Gender, culture, and the person’s life-experience also affect mobility. In order to conceptualize mobility more coherently, Webber et al. [1] proposed a framework that links factors relevant to walking, wheeling, driving, and taking alternate forms of transportation within different life-spaces.
In the context of global and public health, mobility has been defined within the World Health Organization’s International Classification of Function, Disability and Health (ICF) [2] according to the components of: changing and maintaining body position (d410-d429); carrying, moving and handling objects (d430-d449); walking and moving (d450-d469);moving around using transportation (d470-d489). Table 5.1 lists these components that are based on the person doing the movement. What is immediately obvious from the definition using the ICF is, that mobility is a necessary (but not sufficient) capacity required for many other activities such as basic activities of daily living, more complex activities required for maintain self and living space, work, and recreation and leisure including sports. These downstream activities that depend on some degree of mobility are themselves important contributor to QOL [3].
The ICF definition of mobility also includes two other very important qualifying constructs: capacity, what the person can do usually in a test situation; and performance, what the person actually does [4]. Capacity and performance constructs have important implications for measuring mobility. In the ICF, capacity refers to the person’s ability to execute a task in a standard environment. This tends to refer to clinical testing. Whereas Webber et al. [1] also include capacity as a factor in their mobility model but refers to having the biological capability such as having sufficient joint mobility or strength to make mobility possible, areas that fall under the body structure and function component of the ICF.
In the ICF context, performance is poorly described. In another view, Loechte et al. [5] considered mobility in relationship to movement away from the home and other parameters related to what the person is doing. Action range is quantified as to how far a person moves outside their house. Distance is a parameter that can be measured independently from the home reference point such as distance covered per unit time such as per minutes (Six Minute Walk Test (6MWT) [6], per hour, per day. Other mobility parameters are duration (how long someone is mobile), pace (how many steps per minute, e.g. 100 steps per minute), and frequency of mobility events (how many 10 minute bouts of walking). There are important mobility parameters that are related to physical activity guidelines [7]. Mobility can also be characterized qualitatively, without measurement units such as time-of-day, alone or accompanied, and places. For example, places people move to more than 5 minutes can be captured and qualified by location (parks, malls, cafes, museums), activity (socializing, exercising), environment (noisy), or either usual or novel location. As an example, consider two different people.
Mark leaves the house at the same time every day, rides his bicycle 4 km to work taking the same route, and comes home. On the weekend he goes to the gym and does family-related errands and activities.
Eleanor, works from home and regularly exercises by walking, biking, or swimming at her community pool; she sometimes calls up a friend to go with her. These activities are done at different times during the day depending on her work schedule. Sometimes she works in cafes and makes a point of going to different ones. On the weekend, she likes to explore different parts of the city or take small trips out of the city. These are done alone or sometimes with a friend.
In each case, Mark and Eleanor would be classified with the same mobility capacity and performance indicators on the ICF, and they would have the same “action distance” values, but their mobility is realized through very different patterns. The richness of this mobility variety is not easy to capture without technology. Mark may accurately self-report because of the routine nature of his mobility but Eleanor would not be able to provide an average mobility rating for the past week or past month owing to her mobility variation.
While capacity ICF indicators are necessary in the context of a person with a health conditions, they are not sufficient for tracking mobility in healthy populations where performance in the real world is the relevant QOL indicator.
What Is QOL?
The Dictionary of Quality of Life and Health Outcomes Measurement [8] has this to say about QoL:
QOL is a term often used erroneously to refer to health-related quality of life or health status, but is broader than just health and includes components of material comforts, health and personal safety, relationships, learning, creative expression, opportunity to help and encourage others, participation in public affairs, socializing, and leisure [9]. The World Health Organization (WHO) has defined quality of life as “individuals’ perception of their position in life in the context of the culture in which they live and in relation to their goals, expectations, standards and concerns”. In the context of health research, quality of life goes beyond a description of health status, but rather is a reflection of the way that people perceive and react to their health status and to other, nonmedical aspects of their lives. According to Aristotle, quality of life would be the best kind of life, the happiest life [10].
Clearly measuring this happiest of lives is a challenge. QoL is not the same as health as health is only one of many QoL components [9]. Three approaches have been taken to measure QoL. QoL profiles are derived from measures that are made up of multi-item domains that produce domain scores and a total score. The WHOQOL-100 [11] (100 items; six domains: physical health, psychological, level of independence, social relationships, environment, spirituality, plus two single indicators of general health and global QoL) and WHOQOL-Bref [12] (26 items; four domains: physical health, psychological, social relationships, environment and the same two single indicators), are examples of profile QoL measures where the domains are physical health (including mobility), psychological health, social relationships and the environment. The CASP-19 is a quality-of-life measure comprising four domains, control, autonomy, pleasure and self-realization [13]. QoL has also been measured using health indices such as the EQ-5D from the EUROQOL Group [14] or the Health Utilities Index [15] but these measures do not cover many, if any, domains beyond health [16]. The advantage of indices is that they comprise multiple dimensions (usually with one item per each dimension) and a single score is derived by weights related to how much a typical citizen is willing to trade off years of life for these dimensions health. The third way in which QoL is measured is by a single item rated on an ordinal scale (e.g. Excellent, Very good, Good, Fair, Poor) or a visual analogue scale (from worst, 0, to best, 10).Only the person can assess their QoL using these methods and, other than the single-item method, only periodic assessments are possible [17].
Instead of relying on people to periodically sample and report on their QoL, Wac [18] proposes a new way of measuring QOL, using technologies. Quality of Life Technologies (QoLT) refers any technologies that can be used for assessment or improvement of the individual’s QoL. QoLT will be the way of the future owing to the increasing availability of miniaturized computing, storage, and communication capacity that are now embedded within various personal devices and made available through smartphones and wearables.
How much can we infer about QoL by quantifying domains related to QoL? This chapter addresses this novel way of thinking about QoL. Here we address one of these quantifiable domains, namely individual’s (body) mobility, a construct that lends itself well to being quantified by harnessing the power of these existing and emerging technologies.
Is Mobility Important for QoL?
Now that mobility has been described in terms of capacity and performance, and QoL has been defined as “the happiest kind of life” , we discuss if mobility is important to QoL and, if so, what aspects of mobility are important. The answer to this question needs to consider who is being asked and how it is asked. For mostly healthy members of the general population, mobility, particularly walking, is the most important of five key HRQL items. A well known and widely used measure of HRQL is the EQ-5D from the EUROQOL [14] group. The weight, in terms of degree of detraction from perfect health, that members of the general population (from the United States) put on having no mobility as represented by being unable to walk about, is −0.558 (on a scale from 0 to 1; where ‘0’ is the worst possible health state and ‘1’ is perfect health). In contrast, the detracting effect of extreme problems in self-care (−0.471), usual activities (−0.374), pain (−0.537) and mood (−0.450). This translates to be willing to trade off nearly 6 years of life in order to live with no problems with walking about. Research on the effect of mobility limitations on risk of death shows that people, again from the general population of the United States, who walk very slowly have a risk of death 1.89 times higher (95% CI: 1.46–2.46), in comparison to the fastest walkers Liu [19].
In the EQ-5D classification system , the walking component of mobility is one of five HRQL areas clearly underlining its importance. One way of knowing if mobility is important to QoL is to identify how often and how comprehensively mobility is included in recognized QoL or health-related QoL measures. Mayo et al. [16] found that in generic QoL or HRQL measures, mobility was represented in 1/8 items in the HUI [20]; 10/36 items in the SF-36 (1/12 in SF-12) [21, 22]; 2/35 items or 1/8 dimensions of the AQOL [23], 1/26 items in the WHOQOL-BREF [12], and 9/71 items of the QWB [24].
Mobility is clearly important for people with health conditions. Almost every health condition can have an effect on mobility, permanent or transient. There are ICF core sets for some 30 health conditions and all except mental health conditions included one or more aspects of mobility.Footnote 2, Footnote 3 Mobility is more important to QoL once it is limited. People tend to take mobility for granted until the limitations set in, but when asked how they would imaging their life without mobility, they imagine it poorer than with other health challenges. This is one of the reasons why, when valuing health for the purposes of allocation of scarce resources or evaluation of cost-effectiveness of medical interventions, those with the health condition under consideration are not asked to provide a valuation from their point of view as this valuation is considered to be too influenced by their current health state [25,26,27].
The importance of mobility to QoL has been investigated extensively using many different methods, quantitative and qualitative, and in many different health conditions.
What Do People Say?
One of the best ways of answering the question about how mobility relates to QoL is to ask people directly. This is made possible through a synthesis of the qualitative literature or when people are asked open-ended questions.
A synthesis of 11 qualitative studies on QoL after hip fracture [28] identified mobility as a key contributor. Limited mobility affected this population’s opportunities to make free choices about their activities and social interactions, impacted on independence, and was a threat to preservation of self-image. Thirteen qualitative studies from people with leg ulcers also confirmed the importance of mobility to QoL [29].
In a systematic review of 20 papers using an individualized approach to identifying areas important for QoL in people with cancer, Aburub et al. [30] found that in 11 or the 20 papers, mobility/physical activity was listed a one of the top 10 areas. In a review of the 10 most important areas of QoL across four health conditions, Mayo et al. [31] reported that for people with stroke, mobility was the number one area of importance; for people with Multiple Sclerosis mobility was number 6, and for people with cancer and HIV mobility was also selected as important to QoL.
What Do the Data Say about the QoL of the Body
The quantitative investigation of the importance of mobility to QoL is challenging because, as conceptualized using the ICF model [2], mobility limitations are caused by impairments of body structure and function and also act to limit other important activities and restrict participation in key personal, family, and societal roles that have a more direct influence on QoL. Figure 5.1 show these theoretical influences by combining the ICF model with the Wilson-Cleary model [32]. The ICF focuses on the observable manifestations of disability, while the Wilson-Cleary model goes beyond these to consider the effects on health perception and QOL, considered by the ICF model to reflect satisfaction with the observable manifestations and akin to well-being.
Having established that mobility is definitely important for QOL, other questions arise. Is mobility more, less, or as important as other health, social, and environmental domains? What are the best methods of partitioning out the role of mobility in quality of life? If we were to use mobility to quantify QOL, how much will we under or overestimate QOL and in whom and under what circumstances?
In order to sort out the relative importance of mobility and other factors to QOL it is necessary to have a strong theoretical model linking both the capacity and performance aspects of mobility to QOL. One such model is the Wilson-Cleary model [32] that has been shown in Fig. 5.1. The Wilson-Cleary model shows the links between biological and physiological measures taken on the body, symptoms reported by the person (pain, fatigue, mood), function (what the person can do physically and mentally), health perception (how the person actually feels) and QOL and also shows that these links are affected by factors related to the person (age and sex but also beyond these to include lifestyle and preferences), and their environment.
This complexity requires that mobility be considered in a multi-factorial framework and Structural Equation Modeling (SEM) [33] is an ideal statistical method for carrying out a fair assessment of the impact of mobility. However, it is important when using SEM that the outcome is a QOL measure and not a composite measure that includes the constructs under investigation. For example, the WHOQOL-Bref includes a domain for physical health and this includes items about mobility. A selection of 18 relevant papers from a structured review are summarized in Table 5.2.
A feature of these papers is that the impact of mobility is evaluated in the context of other variables including personal factors, environmental factors, symptoms, and other activities. However, a limitation of these studies is there is no universally accepted measure of QoL and the outcomes modeled covered domains that are part of, but not, QoL such as physical health (often the PCS from the SF-36), general health, mental health, participation, illness intrusiveness, or generic or condition specific profile measures of HRQL. Two constructs closer to QoL were life-satisfaction and well being. Only two of the 18 studies measured of QoL, one with a QoL measure, CASP-19 (Study #16, and one with a single item (Study # 17 from Table 5.2). The studies are ordered according to the rank of mobility in explain QoL outcomes.
In these studies, mobility was measured in two ways, through self-reported limitations or difficulties with mobility related activities and through tests of physical capacity. For the latter, these measures included impairments affecting mobility such as strength, balance, and aerobic capacity and performance tests of mobility such as gait speed, Timed-up-and-Go, and 6MWT.
The first seven studies had at least one component of the mobility variable as the most important. Of these seven studies, four were from general population samples or older persons (Study # 1,3,4,5) and three were from clinical populations (Study # 2,6,7). Five studies had mobility as the second most important variable (Study # 8–12) and these were all of clinical populations.
The two studies (Study # 17,18) where mobility variables were not related to QoL were the same two studies that used actual QoL measures rather than measures of related constructs. These measures relate to QoL of the person. Study #17 used the CASP-19 which measures the extent to which the older person feels control, autonomy, pleasure and self-realization. Study #18 used a single QoL item in men living with HIV, a condition that does not affect mobility primarily. The outcomes in many of the other studies included aspects of the body’s QoL for which mobility would have a stronger influence.
This new distinction between QoL of the person and QoL of the body is important because health care targets the body. Monitoring the body’s QoL could be a valuable way for people to know about their body and to reduce the impact of illness and life’s stresses on the body. Monitoring the body’s QoL could also be an effective health care surveillance strategy particularly if it can be done unobtrusively and in real-time.
QoL of the person is best reflected through global QoL measures including those of life satisfaction, whereas QoL of the body is reflected in outcomes related to in health, participation, and illness’ intrusiveness, by, for example impairing mobility. The importance of this distinction could be profound, as the person, with assistance for a growing portfolio of technologies, is better placed to monitor the QoL of their body in real time and react or adjust accordingly. Also, it is recognized that QoL of the person has a profound effect on the body through stress reaction or, in general, behaviors aimed at managing negative emotions [52], that the person could be made aware of through monitoring QoL of the body.
Using Mobility to Quantify QoL
If we were to use mobility to quantify QoL, how much will we under or overestimate QoL and in whom and under what circumstances? While the WHO provides a definition of QoL, in 1978, Flanagan [9] identified 15 components of QoL which are listed in Fig. 5.2.
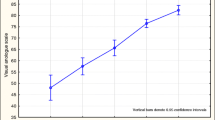
Based on the literature [36, 53, 54] and the clinical and research experience of the authors, an estimated 1/3 of QoL of the person would be explained by mobility, with helping others and active recreation most affected and learning, understanding self, and creativity the least affected (see Fig. 5.3).
What Mobility Parameters Can Be Monitored Via Technologies?
Table 5.2 provides a list of mobility parameters that people have linked to QoL. Starting at the most global is life-space mobility [55], which relates to how far from home a person moves and has been shown to be associated with social support, capacity to drive, and gait speed [56]. One can tell a lot about a person through this one measure, which can be monitored through Global Positioning System (GPS) technology (or some combination of Cell-IDs [57]) that comes with most smart phones or smart wearables. Second on the list, and also very telling about the body’s QoL is the amount of vigorous activities carried out which can be monitored using heart rate and physical accelerations. Increased heart rate without movement would indicate stress (physical or emotional), fear, or cardiac pathology. Amount of time spent in activity would be another very important indicator of the body’s QoL and this is easily monitored using simple wearable devices that monitor accelerations. A common metric is sedentary time [58], which is known to be detrimental to health. Wearable accelerometers also provide information on speed of movement such as step cadence and duration of activity bouts. Canadian Physical Activity Guideline [7] for adults advocate a minimum of 150 minutes of moderate activity accumulated over a week in bouts of 10 minutes; walking at a cadence of 100 steps a minute would meet this recommendation [59].
Higher levels of physical activity such as is achieved through climbing stairs can also be tracked on many smart phone/watch applications. For example a 4 hour game of golf on a hilly golf course that the senior author (NM) regularly walks accumulates 20,000 steps and the equivalent of 38 flights of stairs.
Gait speed while considered the sixth vital sign [60] is actually less important than cadence and more difficult to track as it requires a measure of distance not just stepping frequency. Gait speed is easier to measure clinically where a fixed course can be walked and timed, raising its importance as a clinical indicator because of ease of measurement. The importance of gait speed for safety cannot be disputed as people who cannot walk a speeds of greater than 0.5 m/sec (i.e., in terms of their capacity) are at risk of falls and benchmarks of >0.7 m/sec and > 1.0 m/sec indicate safety risk when crossing 2- and 4-lane streets [61]. However, the frequency at which people walk at different cadence bands a more relevant indicator of how the body is doing in everyday life. Tudor-Locke [59] showed that despite having capacity to walk at a health promoting pace when tested clinically, it is rare for the North American senior to do this in the real world for more than a few minutes a day. Mate et al. [62] showed the same was true for people with Multiple Sclerosis in that they do not reproduce what they are capable of doing on a clinical test in their real world environment, except of course if they lack capacity.
Another clinical test that shows importance for QoL is the Timed-Up-and-Go (TUG) test [63]. This test is indicative of mobility as it requires standing up from a chair, walking 3 meters, turning around, and return to sit back down on the chair. Again, this test is easily done in the clinic, as it requires only a standard chair and 3 meters of walking space. In the real world, the number of transitions from sitting to standing can be captured, as it is another metric available on standard accelerometers.
These mobility measures relate to activity but it is also possible to track motor impairments that lead to mobility limitations such as slowness of movements that can result from stiff joints, resting and intention tremors, poor posture, balance, and poor gait quality. Monitoring these impairments would require different technologies distributed to different parts of the body, but all are possible. There are apps for tremor and balance that require the person hold a smart phone. Posture, balance and gait quality can be measured using inertial devices attached to the back [64] or to the shoe [65,66,67,68]. A selection of wearable devices for mobility and health are shown below (Table 5.3).
How do these measurements relate to QoL of the body? Research show that slowness of movement, poor and irregular gait, poor posture, lack of activity can indicate states of pain, fatigue, low mood, apathy, or anxiety [69,70,71,72,73].
Mapping the Future
We are at the cusp of changing the way we think about monitoring and remediating [74] and technology is poised to empower people to take charge of their own QoL, including, or starting from, their body’s QoL. Given the emergence of today’s and tomorrow’s personalized and miniaturized technologies, the future of monitoring the QoL of the body is inevitable [18]. We envision that the individuals will wear an accurate, well designed smartwatch that monitors activity, heart rate, oxygen saturation, and tremor, amongst other variables. For people with specific health challenges, their posture, stability, and gait quality would be also monitored by small unobtrusive sticky devices placed on their spine, shoulder, ankle or shoe. They also would receive updates on how they are doing, as their devices are continually connected to their smartphone. They will be able to see how their body reacts to internal and external stimulae and learn how to respond to signs of threat [18]. They will also be able to program these devices to provide engaging and effective feedback for optimal performance, literally stamping in good mobility habits, and influencing positively their QoL in the long term.
References
Webber SC, Porter MM, Menec VH. Mobility in older adults: a comprehensive framework. Gerontologist. 2010 Aug;50(4):443–50.
WHO. World Health Organization. International classification of functioning, disability and health. 2nd ed. Geneva; 2001.
Mayo NE, Wood-Dauphinee S, Cote R, Durcan L, Carlton J. Activity, participation, and quality of life six months post-stroke. Arch Phys Med Rehab. 2002;83:1035–42.
Mate KK, Kuspinar A, Ahmed S, Mayo NE. Comparison between common performance-based tests and self-reports of physical function in people with multiple sclerosis: does sex or gender matter? Arch Phys Med Rehabil. 2019 May;100(5):865–73.
Loechte N, Von BT, Haux R. Mobility parameters in health applications–a literature review. Stud Health Technol Inform. 2014;205:523–7.
Crapo RO, Casaburi R, Coates AL, Enright PL, MacIntyre NR, Mckay RT, et al. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002 Jul 1;166(1):111–7.
Canadian Physical Activity Guideline for Older Adults. http://www.csep.ca/CMFiles/Guidelines/CSEP_PAGuidelines_older-adults_en.pdf. 2015.
Mayo NE. Dictionary of quality of life and health outcomes measurement. 1st ed. International Society for Quality of Life; 2015.
Flanagan JC. A research approach to improving our quality of life. Am Psychol. 1978;33:138–47.
McKeon R. Aristotle. Nicomachean Ethics. Introduction to Aristotle. New York: Modern Library; 1947.
The WHOQOL Group. The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995 Nov;41(10):1403–9.
Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL group. Psychol Med. 1998 May;28(3):551–8.
Sim J, Bartlam B, Bernard M. The CASP-19 as a measure of quality of life in old age: evaluation of its use in a retirement community. Qual Life Res. 2011 Sep;20(7):997–1004.
EuroQol Group. EQ-5D. http://www.euroqol.org/. 2016.
Feeny D, Torrance G, Furlong W. Health utilities index. In: Spilker B, editor. Quality of life and Pharmacoeconmics in clinical trials. 2nd ed. Philadelphia: Lippincott-Raven; 1996. p. 239–52.
Mayo NE, Moriello C, Asano M, van der Spuy S, Finch L. The extent to which common health-related quality of life indices capture constructs beyond symptoms and function. Qual Life Res. 2011 Jun;20(5):621–7.
Wac K. Quality of life technologies. In: Gellman M, editor. Encyclopedia of behavioral medicine. New York: Springer; 2020.
Wac K. From quantified self to quality of life. Digital health. Springer; 2008. p. 83–108. https://link.springer.com/chapter/10.1007/978-3-319-61446-5_7
Liu B, Hu X, Zhang Q, Fan Y, Li J, Zou R, et al. Usual walking speed and all-cause mortality risk in older people: a systematic review and meta-analysis. Gait Posture. 2016 Feb;44:172–7.
Feeny D, Furlong W, Boyle M, Torrance GW. Multi-attribute health status classification systems–health utilities index. Pharmaco Economics. 1995;7(6):490–502.
Ware J Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. conceptual framework and item selection. Med Care. 1992;30(6):473–81.
Richardson J, Iezzi A, Khan MA, Maxwell A. Validity and reliability of the assessment of quality of life (AQoL)-8D multi-attribute utility instrument. Patient. 2014;7(1):85–96.
Kaplan RM. The quality of Well-being index. Quality of life and Pharmacoeconomics in clinical trials. 2nd ed. Philadelphia: Lippincott-Raven; 1996.
McPherson K, Myers J, Taylor WJ, McNaughton HK, Weatherall M. Self-valuation and societal valuations of health state differ with disease severity in chronic and disabling conditions. Med Care. 2004 Nov;42(11):1143–51.
Insinga RP, Fryback DG. Understanding differences between self-ratings and population ratings for health in the EuroQOL. Qual Life Res. 2003 Sep;12(6):611–9.
Brazier J, Akehurst R, Brennan A, Dolan P, Claxton K, McCabe C, et al. Should patients have a greater role in valuing health states? Appl Health Econ Health Policy. 2005;4(4):201–8.
Ehlers MM, Nielsen CV, Bjerrum MB. Experiences of older adults after hip fracture: an integrative review. Rehabil Nurs. 2018 Sep;43(5):255–66.
Phillips P, Lumley E, Duncan R, Aber A, Woods HB, Jones GL, et al. A systematic review of qualitative research into people's experiences of living with venous leg ulcers. J Adv Nurs. 2018 Mar;74(3):550–63.
Aburub AS, Mayo NE. A review of the application, feasibility, and the psychometric properties of the individualized measures in cancer. Qual Life Res. 2017 May;26(5):1091–104.
Mayo NE, Aburub A, Brouillette MJ, Kuspinar A, Moriello C, Rodriguez AM, et al. In support of an individualized approach to assessing quality of life: comparison between patient generated index and standardized measures across four health conditions. Qual Life Res. 2017 Mar;26(3):601–9.
Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. J Am Med Assoc. 1995 Jan 4;273(1):59–65.
Kline RB. Principles and practice of structural equation modeling. 1st ed. Guilford Press; 1998.
Li L, Loo BP. Mobility impairment, social engagement, and life satisfaction among the older population in China: a structural equation modeling analysis. Qual Life Res. 2017 May;26(5):1273–82.
Shahrbanian S, Duquette P, Ahmed S, Mayo NE. Pain acts through fatigue to affect participation in individuals with multiple sclerosis. Qual Life Res. 2016 Feb;25(2):477–91.
Alonso J, Vilagut G, Adroher ND, Chatterji S, He Y, Andrade LH, et al. Disability mediates the impact of common conditions on perceived health. PLoS One. 2013;8(6):e65858.
Lampinen P, Heikkinen RL, Kauppinen M, Heikkinen E. Activity as a predictor of mental Well-being among older adults. Aging Ment Health. 2006 Sep;10(5):454–66.
Bentley JP, Brown CJ, McGwin G Jr, Sawyer P, Allman RM, Roth DL. Functional status, life-space mobility, and quality of life: a longitudinal mediation analysis. Qual Life Res. 2013 Sep;22(7):1621–32.
Huang CY, Liao LC, Tong KM, Lai HL, Chen WK, Chen CI, et al. Mediating effects on health-related quality of life in adults with osteoporosis: a structural equation modeling. Osteoporos Int. 2015 Mar;26(3):875–83.
Lee J, Choi M, Jung D, Sohn YH, Hong J. A structural model of health-related quality of life in Parkinson's disease patients. West J Nurs Res. 2015 Aug;37(8):1062–80.
Tannenbaum C, Ahmed S, Mayo N. What drives older women's perceptions of health-related quality of life? Qual Life Res. 2007 May;16(4):593–605.
Kalpinski RJ, Williamson ML, Elliott TR, Berry JW, Underhill AT, Fine PR. Modeling the prospective relationships of impairment, injury severity, and participation to quality of life following traumatic brain injury. Biomed Res Int. 2013;2013:102570.
Shim EJ, Hahm BJ, Go DJ, Lee KM, Noh HL, Park SH, et al. Modeling quality of life in patients with rheumatic diseases: the role of pain catastrophizing, fear-avoidance beliefs, physical disability, and depression. Disabil Rehabil. 2018 Jun;40(13):1509–16.
Barclay R, Ripat J, Mayo N. Factors describing community ambulation after stroke: a mixed-methods study. Clin Rehabil. 2015 Aug;29(29):509–21.
Bouchard V, Duquette P, Mayo NE. Path to illness intrusiveness: what symptoms impact the life of people living with multiple sclerosis? Arch Phys Med Rehabil. 2017 Apr 15;98(7):1357–65.
Perruccio AV, Davis AM, Hogg-Johnson S, Badley EM. Importance of self-rated health and mental Well-being in predicting health outcomes following total joint replacement surgery for osteoarthritis. Arthritis Care Res (Hoboken). 2011 Jul;63(7):973–81.
Aree-Ue S, Kongsombun U, Roopsawang I, Youngcharoen P. Path model of factors influencing health-related quality of life among older people with knee osteoarthritis. Nurs Health Sci. 2019 Sep;21(3):345–51.
Mayo NE, Scott SC, Bayley M, Cheung A, Garland J, Jutai J, et al. Modeling health-related quality of life in people recovering from stroke. Qual Life Res. 2015 Jan;1:41–53.
Soh SE, McGinley JL, Watts JJ, Iansek R, Murphy AT, Menz HB, et al. Determinants of health-related quality of life in people with Parkinson's disease: a path analysis. Qual Life Res. 2013 Sep;22(7):1543–53.
Bielderman A, de Greef MH, Krijnen WP, van der Schans CP. Relationship between socioeconomic status and quality of life in older adults: a path analysis. Qual Life Res. 2015 Jul;24(7):1697–705.
Mayo NE, Brouillette MJ, Scott SC, Harris M, Smaill F, Smith G, et al. Relationships between cognition, function, and quality of life among HIV+ Canadian men. Qual Life Res. 2019 Sep 9;
Nanni MG, Caruso R, Sabato S, Grassi L. Demoralization and embitterment. Psychol Trauma. 2018 Jan;10(1):14–21.
Collins JJ, Baase CM, Sharda CE, Ozminkowski RJ, Nicholson S, Billotti GM, et al. The assessment of chronic health conditions on work performance, absence, and total economic impact for employers. J Occup Environ Med. 2005 Jun;47(6):547–57.
Diehr PH, Thielke SM, Newman AB, Hirsch C, Tracy R. Decline in health for older adults: five-year change in 13 key measures of standardized health. J Gerontol A Biol Sci Med Sci. 2013 Sep;68(9):1059–67.
Phillips J, Dal GE, Ritchie C, Abernethy AP, Currow DC. A population-based cross-sectional study that defined normative population data for the life-space mobility assessment-composite score. J Pain Symptom Manag. 2015 May;49(5):885–93.
Kuspinar A, Verschoor CP, Beauchamp MK, Dushoff J, Ma J, Amster E, et al. Modifiable factors related to life-space mobility in community-dwelling older adults: results from the Canadian longitudinal study on aging. BMC Geriatr. 2020 Jan 31;20(1):35.
Fanourakis M, Wac K. ReNLocAn anchor-free localizaiton algorithm for indirect ranging. 6th International Symposium on A World of Wireless, Mobile and Multimedia Networks (WoWMoM); 2015 Jun 15; Institute of Electrical and Electronics Engineers (IEEE}; 2015 p. 1–19.
Benatti FB, Ried-Larsen M. The effects of breaking up prolonged sitting time: a review of experimental studies. Med Sci Sports Exerc. 2015 Oct;47(10):2053–61.
Tudor-Locke C, Camhi SM, Leonardi C, Johnson WD, Katzmarzyk PT, Earnest CP, et al. Patterns of adult stepping cadence in the 2005-2006 NHANES. Prev Med. 2011 Sep;53(3):178–81.
Fritz S, Lusardi M. White paper: “walking speed: the sixth vital sign”. J Geriatr Phys Ther. 2009;32(2):46–9.
Hornyak V, Van Swearingen JM, Brach JS. Measurement of gait speed. Topics in Geriatric Rehabilitation. 2012;28(1):27–32.
Mate K, Mayo NE. Clinically assessed walking capacity does not always reflect real world walking performance: an example from people with multiple sclerosis. International Journal of MS Care. 2020;22(3):147–54.
Podsiadlo D, Richardson S. The timed “up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8.
Collett J, Esser P, Khalil H, Busse M, Quinn L, DeBono K, et al. Insights into gait disorders: walking variability using phase plot analysis, Huntington’s disease. Gait Posture. 2014 Sep;40(4):694–700.
Vadnerkar A, Figueiredo S, Mayo NE, Kearney RE. Design and validation of a biofeedback device to improve heel-to-toe gait in seniors. IEEE J Biomed Health Inform. 2018 Jan;22(1):140–6.
Mate KK, Abou-Sharkh A, Morais JA, Mayo NE. Real-time auditory feedback-induced adaptation to walking among seniors using the Heel2Toe sensor: proof-of-concept study. JMIR Rehabil Assist Technol. 2019 Dec 11;6(2):e13889.
Mate KKV, Abou-Sharkh A, Morais JA, Mayo NE. Putting the best foot forward: relationships between indicators of step quality and cadence in three gait vulnerable populations. NeuroRehabilitation. 2019;44(2):295–301.
Carvalho LP, Mate KKV, Cinar E, Abou-Sharkh A, Lafontaine A, Mayo NE. A new approach toward gait training in patients with Parkinson’s disease. Gait Posture. 2020;81(9):14–20.
Mansoubi M, Weedon BD, Esser P, Mayo N, Fazel M, Wade W, et al. Cognitive performance, quality and quantity of movement reflect psychological symptoms in adolescents. J Sports Sci Med. 2020 Jun;19(2):364–73.
Esser P, Collett J, Maynard K, Steins D, Hillier A, Buckingham J, et al. Single sensor gait analysis to detect diabetic peripheral neuropathy: a proof of principle study. Diabetes Metab J. 2018 Feb;42(1):82–6.
Harvey RH, Peper E, Mason L, Joy M. Effect of posture feedback training on health. Appl Psychophysiol Biofeedback. 2020 Jun;45(2):59–65.
Serrano-Checa R, Hita-Contreras F, Jimenez-Garcia JD, Achalandabaso-Ochoa A, Aibar-Almazan A, Martinez-Amat A. Sleep quality, anxiety, and depression are associated with fall risk factors in older women. Int J Environ Res Public Health. 2020 Jun;5:17(11).
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011 Apr;23(6):42.
Holloway C, Dawes H. Disrupting the world of disability: the next generation of assistive technologies and rehabilitation practices. Healthc Technol Lett. 2016 Dec;3(4):254–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Mayo, N.E., Mate, K.K.V. (2022). Quantifying Mobility in Quality of Life. In: Wac, K., Wulfovich, S. (eds) Quantifying Quality of Life. Health Informatics. Springer, Cham. https://doi.org/10.1007/978-3-030-94212-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-94212-0_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94211-3
Online ISBN: 978-3-030-94212-0
eBook Packages: MedicineMedicine (R0)