Abstract
At a fundamental level, smoke from wildland fire is of scientific concern because of its potential adverse effects on human health and social well-being. Although many impacts (e.g., evacuations, property loss) occur primarily in proximity to the actual fire, smoke can end up having a significant social impact far from the source. This dynamic, combined with lengthening fire seasons, suggests that understanding how wildland fire smoke affects diverse social values will be increasingly critical. This chapter reviews the existing scientific knowledge related to wildland fire smoke with respect to four topic areas: human health, economics, social acceptability, and risk communication. The broadest existing knowledge base, regarding the health effects attributed to wildland fire smoke exposure, stems from decades of research on the health effects of exposures to ambient fine particulate matter (PM2.5). Despite the potential consequences, scientific knowledge about chronic health effects, economic impacts, and effectiveness of protective actions in response to wildfire smoke risk communication is fairly limited. The chapter concludes with identification of (1) key areas where the need for more empirical information is most critical, and (2) challenges that inhibit an improved scientific understanding.
The views and opinions expressed in this article are those of the individual authors, and do not necessarily reflect the views and opinions of the co-authors or the official policies and positions of the U.S. Government, the Department of Health and Human Services (CDC/ATSDR), the U.S. Forest Service, the U.S. Environmental Protection Agency, or other participating institutions.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
7.1 Introduction
At a fundamental level, smoke from wildland fire is of scientific concern because of its potential adverse effects on an array of social values (e.g., health, economic, cultural). Compared to impacts that tend to occur in proximity to the actual fire, such as evacuations and property loss, smoke can have a significant social impact far from the source. In the fall of 2019, smoke from Australian bushfires greatly affected New Zealand air quality, and across the USA wildland fire smoke has been observed to account for a disproportionate number of poor air quality days (Liu et al. 2015; Larsen et al. 2018). As wildland fire seasons grow longer (Jolly et al. 2015) and wildfires have greater air quality impacts (McClure and Jaffe 2018; O’Dell et al. 2019), understanding potential social impacts from wildland fire smoke becomes increasingly critical. Despite this need, research on the social impacts of smoke is limited compared to other areas of smoke science.
This chapter reviews existing scientific knowledge related to the effects of wildland fire smoke on different social values. The first section summarizes research studies which focus on acute health effects of smoke, including occupational exposure. The remaining sections discuss what is known regarding economic impacts, social acceptance, and risk communication specific to wildland fire smoke. The chapter ends with a summary of key findings and research needs.
7.2 Health Effects Attributed to Wildland Fire Smoke
Scientific evidence examining health effects attributed to wildland fire smoke exposure has grown significantly in the last decade in response to the increased frequency of large fires, the need to understand their public health impacts, and the desire to develop effective response plans. The growth in research efforts is reflected in the increasing number of systematic and critical reviews identifying the potential health effects of smoke exposure (Naeher et al. 2007; Youssouf et al. 2014; Liu et al. 2015; Adetona et al. 2016; Reid et al. 2016a; Black et al. 2017; Cascio 2018; Kondo et al. 2019). In addition, collaborations among federal, state, tribal, local, and territorial governments, as well as nongovernmental organizations have led to development of guidance documents and training materials to inform public health officials, medical professionals, and fire managers of the potential health risks of wildland fire smoke exposure.
In this section, we provide background information on air pollutants in wildland fire smoke and summarize the current scientific evidence on health effects and risk factors that may increase the likelihood of experiencing adverse health effects. The information draws heavily on published documents that have culminated from several interagency collaborations, including “Wildfire Smoke: A Guide for Public Health Officials” (USEPA 2019c) and the continuing medical education course Wildfire Smoke and Your Patients’ Health (USEPA 2019b), and review articles (Naeher et al. 2007; Youssouf et al. 2014; Liu et al. 2015; Adetona et al. 2016; Reid et al. 2016a; Black et al. 2017; Cascio 2018; Kondo et al. 2019). The evidence presented within this section is a broad overview of the current state of science with respect to health effects attributed to wildland fire smoke exposure and is not intended to be a comprehensive systematic review.
7.2.1 Wildland Fire Smoke Exposure
Wildland fire smoke contains a number of air pollutants that are known to be harmful to health, including particulate matter (PM), nitrogen oxides, carbon dioxide, carbon monoxide (CO), hydrocarbons, and other organic chemicals. Of these, particulate matter (PM) is the most significant concern to public health due to widespread exposure and known health effects. PM is largely a by-product of combustion, with the fuel and conditions of combustion being important predictors of the size of particles produced (Chap. 2). Particle pollution is categorized most often by size fraction. Particles that are ≤2.5 µm in aerodynamic diameter (PM2.5, fine particles) comprise >90% of total particle mass emitted from wildland fires (Groß et al. 2013) and are of primary interest when considering health impacts based on scientific evidence from short- and long-term ambient PM2.5 exposures.
Although particles having an aerodynamic diameter of ≤10 µm (PM10) are able to enter the respiratory tract (Fig. 7.1), PM2.5 particles are of the greatest risk to health and are associated with both less severe (e.g., eye and respiratory tract irritation, wheezing, difficult breathing, persistent coughing, excessive phlegm) and more serious health effects (e.g., exacerbation of asthma and heart failure, premature death) (Box 7.1). Therefore, the focus of the health effects discussion in this section is based mostly on PM2.5; potential effects of exposure to other pollutants found in wildland fire smoke are discussed in Sect. 7.2.3.
Size fraction of particulate matter. From https://www.epa.gov/pmcourse/what-particle-pollution
Once inhaled, PM2.5 can cause serious health effects because of its ability to pass through the nose and throat and enter the lungs, thus affecting the lungs and heart. Inhaled particles cause systemic inflammation and oxidative stress that can exacerbate respiratory and cardiovascular disease. Particles can also lead to autonomic dysfunction and central nervous system activation, increasing heart rate, blood pressure, coagulation, restriction of blood vessels, and heart rhythm abnormalities leading to adverse cardiovascular outcomes. Some smaller particles (e.g., particles with an aerodynamic diameter <0.1 µm) may be able to translocate from the lung to the circulatory system, contributing to effects in other organ systems (Brook et al. 2010; USEPA 2019a).
Box 7.1 Prominent Impacts of Wildland Fire Smoke on Human Health
Asthma is a common chronic respiratory disease that affects all age and sociodemographic groups. It is characterized by chronic inflammation of the bronchi and smaller airways, with intermittent airway constriction, causing shortness of breath, wheezing, chest tightness, and coughing, sometimes accompanied by excess mucus production. During an asthma attack, the muscles tighten around the airways, and the lining of the airways become inflamed and swollen, constricting the flow of air. Symptoms are commonly triggered by exposure to air pollution or allergens and are usually worse at night and in the early morning. Physical exertion and cold air also trigger asthma symptoms.
A significant fraction of the population may have airway hyperresponsiveness; an exaggerated tendency of the large and small airways (bronchi and bronchioles, respectively) to constrict in response to respiratory irritants including cold air, dry air, and other stimuli, as well as wildfire smoke. Although airway hyperresponsiveness is considered a hallmark of asthma, this tendency may also be found in individuals without asthma, for example, during and following a lower respiratory tract infection. In such individuals, smoke exposure may cause asthma-like symptoms and bronchitis.
Chronic obstructive pulmonary disease (COPD), which is generally considered to encompass emphysema and chronic bronchitis, is a chronic respiratory disease characterized by irreversible breathing problems and restricted air flow (USEPA 2019a). COPD is also related to presence of other respiratory and heart conditions including heart failure, leading to highly compromised lung and heart capacity. In addition, COPD patients often may experience asthma-like symptoms. However, because their lung capacity has typically been seriously compromised, additional constriction of the airways in individuals with COPD may result in symptoms requiring medical attention. In addition, cigarette smoke is the primary cause COPD and individuals with this condition may also have heart and vascular disease and are potentially at risk of health effects due to smoke exposure from both conditions (General 2014; Morgan et al. 2018).
Cardiovascular diseases are the leading cause of mortality in the USA, comprising 30–40% of all deaths each year (NHBLI 2012). Most of these deaths occur in people over 65 years of age. Diseases of the circulatory system include high blood pressure, heart failure, vascular diseases such as coronary artery disease, and cerebrovascular conditions. These chronic conditions can render individuals susceptible to attacks triggered by air pollutants, such as wildfire smoke, including angina pectoris (transient chest pain), heart attacks, and sudden death due to cardiac arrhythmia, heart failure, or stroke.
In response to exposure to particulate matter, people with chronic heart disease may experience one or more of the following symptoms: shortness of breath; chest tightness; pain in the chest, neck, shoulder or arm; palpitations; or unusual fatigue or lightheadedness. Chemical messengers released into the blood because of particle-related lung inflammation may increase the risk of blood clot formation, angina episodes, heart attacks, and strokes.
PM may also contribute to respiratory infections by impairing physiological processes that remove inhaled viruses and bacteria and prevent them from entering the lungs and circulation. Even in healthy people, exposures to PM2.5 can lead to respiratory effects, including reduced lung function and pulmonary inflammation, but these effects generally are considered transient. A review of biological mechanisms by which PM found in smoke can affect the human body is found in Neaher et al. (2007) and Adetona et al. (2016). Additional resources are in Brook et al. (2010) and “Integrated Science Assessment for Particulate Matter” (USEPA 2019b).
Coarse particles, also referred to as PM10-2.5 (i.e., particles ≥2.5 µm to <10 µm in aerodynamic diameter), are generated primarily from mechanical operations rather than directly from wildland fires or formed downwind. Larger particles (aerodynamic diameter >10 µm) are generally of less concern because they usually do not enter the lower respiratory tract; however, they can irritate the eyes, nose, and throat.
The chemical composition of particles, particularly PM2.5, in smoke can vary geographically (Chap. 5), and multiple toxicological studies have shown that some individual components (e.g., black carbon, metals) within the PM2.5 mixture may be more toxic than others. As a result, research efforts have attempted to identify whether health effects are more consistently attributed to individual components or specific sources of PM2.5. Evaluation of this evidence has found that, although many components and sources have been linked with health effects, the evidence does not indicate that any specific individual component or source is related more strongly to health effects than PM2.5 (USEPA 2019a). More recent epidemiologic studies focusing on the health effects of wildland fire-specific PM2.5 support this conclusion by reporting associations similar in magnitude between cardiovascular effects and PM2.5 generated on days affected by smoke and days not affected by smoke (DeFlorio-Barker et al. 2019). However, some recent studies indicate that associations between respiratory effects, including asthma exacerbations, and wildfire-specific PM2.5 may be larger in magnitude compared to associations reported in studies of ambient PM2.5, creating a need for additional exploration into these potential differences (Borchers Arriagada et al. 2019; Kiser et al. 2020; DeFlorio-Barker et al. 2019).
7.2.2 Epidemiologic Evidence—Wildfire Smoke and PM2.5
The primary body of evidence that forms the basis of the understanding about the health effects of wildland fire smoke stems from decades of research on the health effects of ambient particle pollution, specifically PM2.5, conducted primarily in urban settings. Those research efforts, which have generally supported a linear concentration-response relationship, provide extensive information on health risks and biological mechanisms by which exposure to particle pollution can lead to health effects. Based on a comprehensive evaluation of the scientific evidence in support of National Ambient Air Quality Standards (NAAQS), the U.S. Environmental Protection Agency (USEPA) has concluded that, for both short- (days to weeks) and long-term (months to years) PM2.5 exposure, there is a “causal relationship” for cardiovascular effects and mortality and “likely to be a causal relationship” for respiratory effects (USEPA 2019a).
In recent years, the number of studies examining the health effects specifically of wildfire smoke exposure has grown as well. However, many of these studies are conducted in different geographic locations and use various exposure metrics (e.g., monitoring data or modeled estimates of PM2.5 or PM10, smoke versus no-smoke days), which complicates the quantitative comparison of risk estimates across studies. There have been recent advancements in approaches used to estimate smoke exposure by blending chemical transport model predictions and satellite data with ground-based measurements through machine learning and data fusion methods. These new methods have the potential to reduce uncertainty and facilitate future quantitative comparisons of health effects across studies.
Some studies are beginning to assess whether there are differences in health effects between smoke from prescribed fire and wildfire. For example, a recent study by Prunicki et al. (2019) provided initial evidence of differences in markers of immune function, DNA methylation, and worsened respiratory outcomes in school-aged children exposed to wildfire smoke compared to prescribed fire smoke. However, it is unclear if these differences are primarily due to the difference in smoke concentrations between prescribed fires and wildfires.
Although the biological mechanisms that can lead to adverse health outcomes are similar between particles emitted from different sources, there are several considerations when generalizing health effects from ambient air pollution to effects from wildland fires. During wildfire events, populations are exposed to a complex mixture as with ambient air pollution, but at much higher concentrations of particles and gases that may have different effects (e.g., synergistic or additive effects) not present during exposure to non-wildfire ambient air pollution. And although much is known about the shape of the PM2.5 concentration response function in ambient settings, less is known about how the response function may differ at hazardous smoke exposure levels, at repeated exposure to hazardous levels, or at peak exposures at the sub-daily level. Some wildfires burn infrastructure in addition to vegetation, likely shifting the mixture from those created solely through the combustion of natural fuels to emissions from the burning of often more toxic, man-made materials (Chap. 6). Finally, population exposure patterns and behavior modification patterns, as well as health impacts during lower intensity events such as prescribed burning, are largely unknown. The following sections characterize the current state of science with respect to health effects of wildland smoke exposure by integrating evidence from studies of ambient PM2.5 and smoke exposure, specifically from wildfires spanning a variety of exposure assignment approaches. Except with firefighters, epidemiologic studies have largely not focused on the population-level health effects from exposure to prescribed fire smoke.
7.2.2.1 Health Outcomes
Respiratory Morbidity
Short-term exposure to PM2.5 during smoke episodes can lead to breathing difficulties, especially for people with chronic lung diseases, such as asthma, chronic obstructive pulmonary disease (COPD), and other reactive airway diseases (Box 7.1). More than 24 million people in the USA, including more than 5 million children, experience chronic asthma, and 16 million experience COPD (CDC 2017, 2019). Epidemiologic studies on exposure to PM2.5 demonstrate increased risk of emergency department visits and hospital admissions related to these outcomes (USEPA 2019a).
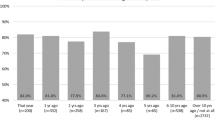
During smoke episodes, increased rates of respiratory-related physician visits (Mott et al. 2002; Moore et al. 2006; Lee et al. 2009; Henderson et al. 2011), emergency department (ED) visits (Tham et al. 2009; Rappold et al. 2011; Thelen et al. 2013; Johnston et al. 2014), and hospitalizations (Mott et al. 2005; Cançado et al. 2006; Chen et al. 2006; Delfino et al. 2009; Ignotti et al. 2010; Morgan et al. 2010; Henderson et al. 2011; Martin et al. 2013; DeFlorio-Barker et al., 2019) are reported with consistency. Among these, asthma- and COPD-related exacerbations and increased use of related medications are among the most commonly reported outcomes (Liu et al. 2015; Adetona et al. 2016; Reid et al. 2016a; Black et al. 2017; Cascio 2018; Gan et al. 2020). An analysis of asthma healthcare utilizations during the 2013 wildfire season in Oregon (Fig. 7.2) found a positive association between wildfire smoke PM2.5 and various asthma morbidity measures, including ED visits, ambulatory care provided in an office setting, outpatient hospital visits, and asthma-rescue-inhaler medication prescriptions filled (Short Acting Beta-2 Agonists [SABA]) (Gan et al. 2020). This suggests that, in communities impacted by smoke, asthma-related healthcare utilizations could increase significantly by people seeking medical countermeasures and treatment in diverse health care facilities (e.g., primary care physician office, clinics, emergency rooms, hospitals).
Association between a 10 μg m−3 increase in wildland fire smoke-related PM2.5 concentration and risk for asthma-related healthcare utilization events (Gan et al. 2020). Asthma-related health risks differed across subpopulations by age and gender, although those differences were not statistically significant for the 2013 wildfire season in Oregon. SABA stands for short acting beta-2 agonists, an asthma-rescue-inhaler medication
Cardiovascular Morbidity
Epidemiologic and experimental studies have linked PM2.5 exposure to increased risks of heart attacks, heart failure, cardiac arrhythmias, and other adverse effects in those with cardiovascular disease (USEPA 2019a). As a result, PM2.5 is a concern for those with chronic heart diseases. Although fewer studies have examined the relationship between smoke exposure and cardiovascular outcomes, evidence is increasing concurrently with the increased frequency of large wildfires (Delfino et al. 2009; Henderson et al. 2011; Rappold et al. 2011, 2012; Dennekamp et al. 2015; Gan et al. 2017; Wettstein et al. 2018; DeFlorio-Barker et al. 2019; Yao et al. 2020). At the time of the last critical review of this literature completed in August 2015, the evidence of a relationship between smoke exposure and cardiovascular outcomes was considered less consistent compared with studies examining ambient PM2.5 exposure (Reid et al. 2016a). However, several recent studies have reported elevated risks of specific cardiovascular outcomes—such as ischemic heart disease, heart failure, and dysrhythmia (Dennekamp et al. 2015; Yao et al. 2016; Wettstein et al. 2018; DeFlorio-Barker et al. 2019; Jones et al. 2020)—with the magnitude of association consistent with those previously reported in studies of ambient PM exposure (USEPA 2019a).
A number of factors may explain the inconsistent results reported in earlier reviews of evidence related to wildland fire smoke exposure and cardiovascular outcomes as compared to those examining ambient PM2.5 effects. These factors include differences in the exposure metric used across studies (e.g., PM10 versus PM2.5 and smoke day versus no-smoke day) and differences in the ability to accurately assess exposure to ambient PM2.5 versus exposure to wildland fire smoke (Liu et al. 2015; Fann et al. 2018). In addition, it has been hypothesized that the difference in results for cardiovascular effects could reflect individuals taking protective action to address acute respiratory effects, which may reduce the risk of other severe outcomes, including cardiovascular, that might result in hospitalizations (DeFlorio-Barker et al. 2019).
Mortality
Extensive epidemiologic evidence from studies conducted across the USA and elsewhere has demonstrated a relationship between short-term PM2.5 exposure and mortality (USEPA 2019a). The limited number of studies examining wildland fire smoke exposure and mortality provide evidence consistent with the larger body of evidence examining ambient PM2.5 exposure (Morgan et al. 2010; Johnston et al. 2011; Analitis et al. 2012; Faustini et al. 2015; Linares et al. 2015, 2018; Kollanus et al. 2016; Yao et al. 2019; Doubleday et al. 2020).
Epidemiologic studies examining cause-specific mortality and wildland fire smoke exposure are limited in number and have only reported evidence of positive associations with cardiovascular-related mortality, although there is extensive evidence indicating a relationship between short-term ambient PM2.5 exposure and respiratory- and cardiovascular-related mortality (Johnston et al. 2011; Analitis et al. 2012; Faustini et al. 2015; Kollanus et al. 2016). This difference in results between wildfire smoke and ambient PM2.5 exposure could be attributed to a number of factors including that cardiovascular mortality accounts for a larger fraction of total non-accidental mortality (~33%) in comparison with respiratory mortality (~7%); in combination with wildland fire events being of short duration (a few days to a few months), the statistical power of a study to observe an association is reduced. Although it is worthwhile to speculate on why there is a difference in results between studies examining mortality associated with short-term wildland fire smoke exposures compared to ambient PM2.5 exposures, it is important to reiterate the extensive evidence demonstrating positive associations between short-term PM2.5 exposure and mortality in studies conducted using different exposure assessment methodologies, in different geographic locations, and in populations with different demographic characteristics (USEPA 2019a).
Other Health Outcomes
In addition to respiratory and cardiovascular effects and mortality, new evidence exists on other potential health effects from both short- and long-term PM2.5 exposure, including metabolic effects and effects on the nervous systems, which may also occur in response to wildland fire smoke exposure. There is some evidence indicating that short-term ambient PM2.5 exposure may lead to altered metabolic function, such as changes in glucose and insulin homeostasis, whereas long-term ambient PM2.5 exposures may lead to the development of metabolic syndrome and diabetes (USEPA 2019a). One study has reported that short-term exposure to wildfire PM2.5 was associated with calls related to diabetes in ambulance dispatches and physician’s assessments but not hospital diagnosis in British Columbia (Yao et al. 2020). Recent studies of ambient PM2.5 exposures also provide evidence of relationships between long-term exposure and nervous system effects in adults, including cognitive declines and altered brain volume (USEPA 2019a). Evidence is more limited for associations between PM2.5 exposures and other outcomes, such as developmental effects, including autism spectrum disorder and cognitive development (USEPA 2019a). Evidence is also limited for nervous system effects in relation to short-term PM2.5 exposures (USEPA 2019a). Overall, there is limited research on the effects of short-term wildfire smoke exposure on metabolic effects and the effects on the nervous system.
Smoke also may have substantial effects on the mental health and emotional stress of communities. Although mental health effects have been studied to a limited degree for general wildfire contexts, the literature on mental health impacts from smoke exposure is even more sparse. When individuals in communities in the Northwest Territories (Canada) were told to stay indoors for most of the summer of 2014 because of prolonged air pollution from nearby wildfires, residents reported decreased physical activity and community engagement, both of which were associated with adverse mental health impacts (Dodd et al. 2018).
7.2.2.2 Life Stages and Populations Potentially at Risk of Smoke-Related Health Effects
Most healthy adults and children may experience transient health effects from smoke exposure without long-term consequences. However, some individuals may experience more severe effects. Although our understanding of the long-term health implications of wildfire smoke exposure is minimal, there is extensive evidence indicating that long-term exposure to ambient PM2.5 can lead to a range of health effects (USEPA 2019a). The concentration and duration of exposure, individual susceptibility (including the presence of preexisting lung [e.g., asthma, COPD] or heart disease), and other factors play significant roles in determining whether someone will experience smoke-related health effects. Beyond those with preexisting health conditions, specific life stages and populations potentially at greater risk of experiencing an adverse health outcome include children under 18 years of age, pregnant people, developing fetuses, older adults, those of lower socioeconomic position (SEP), and outdoor workers.
Evidence of the particular life stages and populations potentially at increased risk of health effects from wildland fire smoke exposure stems from the large number of epidemiologic studies examining PM2.5 in urban settings, which indicate that the risk of health effects attributed to PM2.5 exposures differs based on life stage (children, older adults), health status, and SEP. Risk factors that influence whether a population or individual is at increased risk of health effects from smoke are similar to those for ambient PM2.5 (Naeher et al. 2007; Liu et al. 2015; Adetona et al., 2016; Reid et al. 2016a).
Children
All children are considered at risk for experiencing a health effect because of air pollution and wildland fire smoke, regardless of whether they have a preexisting health condition. Compared with adults, children inhale more air per kilogram of body weight, spend more time outside, and may engage in more vigorous activity, all of which can contribute to increased exposure to PM2.5, and ultimately, affect developing lungs (Sacks et al. 2011).
Short-term exposure to PM2.5 can lead to increased respiratory symptoms, asthma exacerbations, and decreased lung function in children (USEPA 2019a). Similar respiratory effects have been reported in studies of smoke exposure on children, which have demonstrated increased coughing, wheezing, difficulty breathing, and chest tightness, resulting in school absences and declines in lung function (Jacobson et al. 2012, 2014). In addition, an experimental study conducted in infant monkeys has provided initial evidence indicating that smoke exposure during infancy may lead to altered lung and immune function in adolescence (Black et al. 2017).
In the USA, more than 6 million children have chronic lung diseases, such as asthma (CDC 2017, 2019). Higher rates of asthma ED visits and hospital admissions for children, especially infants and very young children, have been observed during and after wildland fires (Hutchinson et al. 2018). However, children without asthma can also experience respiratory symptoms in response to smoke exposure (Jalaludin et al. 2000; Jacobson et al. 2012, 2014), resulting in school absences and other limitations of normal childhood activities.
Although respiratory effects represent the primary adverse health outcome in children in response to smoke exposure, children also may be more likely to be exposed to ash from the fire itself, by engaging in outdoor activities and cleanup after a wildfire, or simply by their proximity to the ground. Fire ash can contain high concentrations of chemicals harmful to health.
Pregnant People and Fetuses
Individuals who are pregnant may be at increased risk of adverse health effects from wildland fire smoke because of the numerous physiologic changes that occur during pregnancy, such as increased blood and plasma volumes and increased respiratory rates, all of which can increase vulnerability to environmental exposures (USEPA 2019c). Developing fetuses also may be at risk when mothers are exposed to smoke during critical phases of human development. For example, Miller et al. (2019) showed that pregnant monkeys exposed to wildfire smoke could pass immune dysregulation on to the next generation.
Although only a few studies have examined the health effects of smoke exposure on pregnancy outcomes, studies on other combustion-related air pollutants have provided some evidence of adverse health effects. Specifically, there is substantial evidence of low birth weight caused by repeated exposures to cigarette smoke, including both active smoking and passive exposure (Martin and Bracken 1986; Windham et al. 2000; Wang et al. 2002).
Studies examining chronic maternal exposure to PM2.5 (USEPA 2019a; DiCicca et al. 2020 Inoue et al. 2020; Li et al. 2021;) and indoor biomass smoke from wood-fire home heating devices have provided some evidence of adverse birth and obstetrical outcomes (e.g., decreased infant birth weight, preterm birth, birth defects) and perinatal mortality (Lakshmi et al. 2013; Amegah et al. 2014; Gehring et al. 2014; Weber et al. 2020). Smoke may also affect the developing fetus, resulting in lower birth weight in children that were in utero when wildland fire smoke was present (Holstius et al. 2012; Candido da Silva et al. 2014). For example, lower birth weight and preterm birth were found to be associated with wildfire smoke exposure in a study conducted across the state of Colorado (Abdo et al. 2019). In addition, there is some evidence for an increase in risk of congenital heart birth defects (atrial and ventricular septal defects) in relation to PM2.5 exposure (Hu et al. 2020). Results from studies examining birth outcomes and smoke exposure are similar to the large number of studies examining PM2.5 exposure and birth outcomes in terms of inconsistency in results. Some studies provide evidence of an association and others do not, potentially a result of inconsistencies in the exposure window (i.e., exposure over the entire pregnancy or specific trimesters) in which associations are observed (USEPA 2019a).
Older Adults
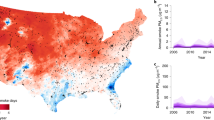
Epidemiologic studies of smoke exposure have demonstrated increased risk of health effects in older populations (often defined as people > 65 years of age). This is of particular concern because the number of US adults 65 years of age and older is expected to double by 2030 (Ortman et al. 2014). Older adults often are at increased risk because of higher prevalence of preexisting lung and heart diseases, reduced lung capacity, and a decline in physiologic processes (e.g., defense mechanisms) that occur with age (Sacks et al. 2011). Wettstein et al. (2018) reported a positive association between wildland fire smoke PM2.5 density and ED visits for cardiovascular, cerebrovascular, and respiratory disease, with the greatest impact observed among adults 65 years and older, in contrast to no change in risk for those under 65 (Fig. 7.3). However, other studies examining smoke exposure did not find evidence that adults over 65 years of age are at increased risk; in fact, some studies have found higher risk for working-age adults (Henderson et al. 2011; Reid et al. 2016b), and others have found no clear differences by age category (Alman et al. 2016). Differences in findings across studies could result from examining different health endpoints, different exposure assessment methods (Gan et al. 2017), or different underlying health of the population.

From Wettstein et al. (2018)
Relative risk and 95% confidence intervals for all-cause cardiovascular outcomes relative to smoke-free days. Data are cumulative 0–4 days following exposure (lag days 0 to lag days 4), by age groups for eight California Air Basins (1 May–30 September 30 2015).
Low Socioeconomic Position (SEP)
Metrics of SEP are used to characterize access to resources, both social and economic (Duncan et al. 2002; Galobardes et al. 2006). These indicators, which include education, employment, income, access to health care, and housing, may be considered at different scales, including individual, family, or community levels. SEP is associated with differential exposures to air pollution; individuals who have lower SEP or live in communities with lower SEP profiles are often exposed to higher concentrations of ambient air pollutants (USEPA 2019c). However, a recent study found that the non-Hispanic white populations in the USA, on average, live in communities with higher wildfire smoke exposure (Burke et al. 2021). When considering exposures to wildland fire smoke, individuals of lower SEP may have limited access to exposure-reducing resources, such as in-home filtration or portable air purifiers, as well as healthcare (USEPA 2019c).
Epidemiologic studies examining short-term PM2.5 exposure demonstrate increased risk of health effects for individuals with lower SEP profiles. However, different studies use different metrics to represent low SEP (e.g., educational attainment, percent below poverty line). The few studies that have examined smoke and the role of SEP as a modifier of risk have similar results. Reid et al. (2016b) reported an inverse relationship between ZIP code-level higher median income and the risk of asthma, COPD, pneumonia, and all-cause respiratory ED visits during a wildland fire event (Fig. 7.4). Rappold et al. (2012) reported higher rates of ED visits in counties with lower SEP status compared with those with higher SEP status during smoke events. Conversely, Liu et al. (2017) found no difference in the likelihood of respiratory hospital admissions by educational attainment in an elderly cohort during periods more affected by smoke.
7.2.3 Other Smoke Pollutants Associated with Health Risks
Although particle pollution is of greatest concern to public health, wildland fire smoke is a complex mixture of pollutants that, individually on their own, also have been associated with health effects. Other pollutants found in smoke that are related to various health effects include tropospheric ozone, CO, and hazardous air pollutants (HAP).
7.2.3.1 Ozone
Ground-level or tropospheric ozone is a widespread pollutant formed by the photochemical reaction of volatile organic compounds and nitrogen oxides in the presence of sunlight (Chaps. 5 and 6). Wildland fires emit large quantities of volatile organic compounds that can be transported in the atmosphere over large distances and enhance ozone production downwind, particularly over urban areas rich in nitrogen oxides from other sources (Brey and Fischer 2016; Larsen et al. 2018). Both epidemiologic and experimental studies have demonstrated that ground-level ozone exposure can result in adverse health effects, such as reduced lung function, inflammation of the airways, chest pain, coughing, wheezing, and shortness of breath—even in healthy people. These effects can be more serious in people with asthma and other lung diseases (USEPA 2020). Respiratory effects attributed to ozone exposure may lead to increased use of medication, school absences, respiratory-related hospital admissions, and ED visits for asthma and COPD. Evidence is more limited for the effects of ozone exposure on the cardiovascular system. However, short-term ozone exposures may lead to premature mortality (USEPA 2020).
Few studies have examined the role of ozone during wildland fire events on health outcomes. Reid et al. (2019) found that ozone downwind during a fire was associated with increased ED visits for respiratory symptoms, but that the associations were not apparent when the analysis was adjusted for PM2.5, which was more strongly associated with respiratory health endpoints than was ozone. However, the study investigated only one fire and, given variability in the timing and location of impacts of wildland fire plumes on ozone production (Buysse et al. 2019), more research is needed on the health impacts of ozone during fire events.
7.2.3.2 Carbon Monoxide
CO is a highly toxic and odorless gas that impairs delivery of oxygen to the body’s organs. Wildland fire smoke can contain high CO concentrations, but this generally does not pose a significant risk except for nearby at-risk populations or individuals (e.g., firefighting personnel). Exposure to CO poisoning is dangerous to all individuals, but people with cardiovascular disease may experience health effects, such as chest pain or cardiac arrhythmias, at lower levels of CO than do healthy people. At higher levels (such as those that occur in major structural fires), CO exposure can cause headache, weakness, dizziness, confusion, nausea, disorientation, visual impairment, coma, and death, even in otherwise healthy individuals (USEPA 2010).
7.2.3.3 Hazardous Air Pollutants
In addition to PM2.5, ozone, and CO, wildland fire smoke also contains additional pollutants characterized as HAPs or toxic air contaminants (Reinhardt and Ottmar 2004). In the extensive list of HAPs, acetaldehyde, acrolein, formaldehyde, and benzene are among those of greatest concern (Chap. 6). These pollutants can be harmful to infants, children, pregnant people and their fetuses, older adults, persons engaging in physical activity, and those with existing lung, heart, or liver diseases. More information on concerns related to HAP exposures can be found in the publication “Wildfire Smoke: A Guide for Public Health Officials” (USEPA 2019c). However, not many epidemiologic studies examine these pollutants because they are not widely measured. Truly understanding the health effects of other pollutants from wildfire smoke would require more monitoring, especially in non-urban areas. Fully assessing population exposures to these additional pollutants is growing in importance as the number of structures burned during wildfire events increases.
7.2.4 Occupational/Cumulative and Chronic Exposures
Although workers in a range of outdoor occupations (e.g., agriculture, construction, landscaping, utility work) can be exposed to smoke, to date the only occupational smoke exposure research has been on wildland firefighters, and this work is relatively limited. Research on wildland firefighters is also the main source of the limited data related to the health effects of cumulative or chronic smoke exposure. While these findings provide insight into potential occupational health effects, caution should be used in applying them broadly as firefighters perform a variety of tasks, whether suppressing wildfires or implementing a prescribed burn, that can have different levels of smoke exposure (Box 7.2).
Box 7.2 Potential Smoke Exposure Incurred by Wildland Firefighters and Other Occupations
During the peak of the 2018 wildfire season, approximately 30,000 wildland firefighters were mobilized across the USA to suppress wildfires. When working on a large wildfire, firefighters sleep and eat at a base camp (incident command post) that is often near the fire, experiencing exposure to smoke, emissions from vehicles and generators (diesel exhaust), and road dust. Firefighters also perform a variety of tasks—operating a fire engine, constructing fireline, holding, mop up, and firing operations—all of which can have distinct smoke exposure.
Engine operators work as a part of an engine crew, operating diesel pumps that provide water to crews working near the fire. Fireline construction involves clearing vegetation and digging or scraping down to mineral soil with hand tools to create a break in burnable vegetation to stop the spread of a fire. Holding refers to activities in which firefighters engage to ensure that the active fire has not crossed the fireline. After the fire has been controlled, crews mop up the area by extinguishing any burning material by digging out the material or applying water to stop smoldering material from re-igniting a fire. Firing operations involve setting an intentional fire, typically using torches filled with a 3:2 diesel/unleaded gasoline mixture, to reduce the available flammable material for the wildfire to consume.
Workers who have outdoor occupations, such as agriculture, construction, landscaping, utility operations, and maintenance can also be exposed to wildfire smoke. There is little research measuring smoke exposure and associated adverse health effects for outdoor workers. In 2020, California adopted an emergency regulation (Regulation 5141.1, Protection from Wildfire Smoke under the California Code of Regulations, Title 8, Division 1, Chapter 4, of the General Industry Safety Orders) to protect outdoor workers from wildfire smoke, using PM2.5 as an indicator for exposure to smoke. The regulation requires employers to determine the Air Quality Index (AQI) for PM2.5 throughout a work shift, communicate and train employees about the hazards of smoke, and reduce exposures when AQI >151 for PM2.5 (0.055 mg m−3).
To reduce exposures at AQI <151, employers can implement engineering or administrative controls, such as providing enclosed spaces with filtered air, changing work schedules, reducing work intensity, or providing more rest breaks. At AQI values between 151 and 500, the regulation requires that respirators (approved by the National Institute for Occupational Safety and Health) be provided to employees for voluntary use, which does not require fit testing or medical evaluations. If AQI >500, employers are required to provide respirators and follow requirements under the respiratory protection regulation, reducing worker exposure to PM2.5 <0.055 mg m−3.
7.2.4.1 Acute Occupational/Firefighter Exposure
Assessments of the health effects of smoke exposure in wildland firefighters have focused mainly on acute effects across individual shifts and entire fire seasons. Wildland firefighters suppressing fires work long hours performing physically demanding work and can be exposed to high levels of smoke. Measuring exposures to smoke can be challenging because of the extreme environment in which wildland firefighters operate. Currently, wildland firefighters do not have respiratory protection available that both meets the demands of the arduous work performed and protects against all potentially hazardous exposures (Domitrovich et al. 2017). In addition, according to the National Wildfire Coordinating Group, only respirators approved by the National Institute for Occupational Safety and Health (NIOSH) shall be used on the fireline. While respiratory-type products (such as bandanas) are marketed to wildland firefighters, they are not NIOSH-approved (NIFC 2020).
Although smoke exposure in firefighters has been studied for decades (e.g., Reinhardt and Ottmar 2000), recent studies have focused primarily on exposure to CO, PM2.5, and PM4 (Navarro 2020). The permissible occupational exposure limit (OEL) standard set by the Occupational Safety and Health Administration (OSHA) for CO is 35 ppm, and 5 mg m−3 for respirable particles not otherwise regulated (PM4) (OSHA 2017). Although field studies have measured different size fractions of PM, the particle size of combustion-generated particles for wood smoke is within a similar size range, which makes PM2.5 and PM4 comparable across wildfire smoke studies (Navarro et al. 2019). Across all field studies conducted since 2009, no measured exposure exceeded the OSHA OELs for CO or PM4. However, these exposure limits do not consider the extended hours that wildland firefighters often work, nor does the PM4 OEL account for the toxicity of wildland fire smoke from various compounds that make up or adsorb to the airborne particulates from smoke. In addition, most field studies collect data only at specific fire incidents, which makes their measurements limited to certain fire conditions and fuel types.
Reinhardt and Broyles (2019) collected field data across many prescribed fires and wildfires in the continental USA, providing smoke data that captures the variability of exposures at different fires. They reported that 22% (at wildfires) and 20% (at prescribed fires) of the measured PM4 exceeded OELs that had been derived specifically for wildland firefighters to account for longer work shift, arduous work demands, and the exposure to multiple chemicals in smoke. They also examined factors in the wildfire environment that may predict exposures, finding that work task, time spent performing the work task, wind position, and type of wildfire crew contributed to exposure. Using the same data as Reinhardt and Broyles, Henn et al. (2019) found that fuel quantity, relative humidity, type of suppression strategy, and wind speed were significantly associated with elevated levels of CO exposure.
Recent field studies measuring smoke exposure found higher concentrations of PM and CO at prescribed fires compared with wildfires. This exposure difference could be due to the job tasks performed on prescribed fires. Past field studies report that wildland firefighters performing holding and firing, the two main job tasks performed on prescribed fires, can be exposed to higher concentrations of PM (Adetona et al. 2017; Reinhardt and Broyles 2019). At prescribed fires, Neitzel et al. (2009) reported the highest mean concentration for PM2.5 (1.2 mg m−3), and Reinhardt and Broyles (2019) reported the highest mean concentration for CO (4.4 ppm). At wildfires, the highest concentrations of measured PM4 (0.51 mg m−3) and CO (1.93 ppm) were reported for wildland firefighters performing mop up and fireline construction (Box 7.2), respectively (Gaughan et al. 2014). Highlighting the complexity of assessing smoke impacts, when looking across different smoke studies in the USA and Australia the highest firefighter exposures to PM2.5 and CO were seen on prescribed fires in the southeast USA and wildfires in Colorado (Navarro 2020).
In addition to examining lung function, certain biomarkers have been measured in wildland firefighters to understand systemic inflammation (Swiston et al. 2008; Adetona et al. 2011a, b; Hejl et al. 2013). Gaughan et al. (2014) reported that wildland firefighters had a significant decline in lung function associated with high exposure to levoglucosan (a tracer for wood smoke) across work shifts. Adetona et al. (2017) demonstrated that, during a prescribed burn operation, firefighters engaged in lighting operations had elevated measurements for C-reactive protein, serum amyloid, and interleukin-8 compared with firefighters involved in holding activities (Box 7.2), an often smoky task where firefighters ensure that the fire does not cross control lines. The researchers hypothesized that in addition to smoke, exposure to combustion of diesel and gasoline during lighting operations could have led to this increase in inflammatory markers. Such elevated measures can be a sign of increased inflammation throughout the body, which can be associated with cardiovascular and other chronic diseases, and possibly the development of cancer. The same researchers reported positive association between creatinine-adjusted urinary mutagenicity and measures of exposure (polycyclic aromatic hydrocarbon metabolites, malondialdehyde, and light-absorbing carbon) across a work shift (Adetona et al. 2019). Results from this study indicate that exposure to smoke may include mutagens that can alter DNA and may cause cancer.
7.2.4.2 Chronic Exposure
While short-term smoke exposure is measured over days to weeks, cumulative or chronic exposures need to be examined over weeks to months, or even across multiple fire seasons. Extensive evidence among the general population indicates relationships between long-term PM2.5 exposure and human health, including respiratory effects (e.g., changes in lung function), cardiovascular effects (e.g., development of atherosclerosis), and premature mortality (USEPA 2019a). However, evidence of health effects from chronic or long-term exposures specific to wildland fire smoke is limited, in part due to significant methodological challenges, such as identifying populations that experience wildfire smoke exposures over many years. The limited research on this topic to date has focused on wildland firefighters; caution should be used in comparing their occupational exposure and health effects to those experienced by the general population (Adetona et al. 2016).
Initial evidence from studies of wildland firefighters indicates that continuous occupational smoke exposure over multiple days or multiple consecutive fire seasons may have a cumulative effect on lung function, with some studies observing a progressive decline in lung function during burn seasons (Liu et al 1992; Gaughan et al. 2014). However, it is unclear if this decline persists across multiple fire seasons or if lung function is recovered in the winter off-season. A survey of firefighters found an association between the duration of their careers and self-reported health outcomes, including associations between ever being diagnosed with two cardiovascular measures (hypertension and/or heart arrhythmia) and the number of years worked as a firefighter (Semmens et al. 2016). Another study estimated that firefighters could have an increased risk of lung cancer (8–43% excess risk) and cardiovascular disease (16 to 30% excess risk) mortality over careers that ranged from 5 to 25 years (Navarro et al. 2019). Although this study was unable to adjust for individual factors (i.e., smoking, diet), the researchers used field measurements of PM4 and heart rate (to calculate breathing rate) collected on wildfires across the USA in a dose–response model to estimate these risks.
7.3 Economic Costs and Losses from Smoke
Smoke from both wildfires and prescribed fires can affect local economies by altering production and consumption of economic goods and services, including transportation, manufacturing, agriculture, health services, recreation, and tourism. These impacts will differ by distance from the fire, and over time as the fire produces different quantities of smoke at different times.
This section assesses the state of science in measuring the economic impacts of smoke from wildland fires. Because research on economic impacts specific to smoke is limited, this section begins with an overview of potential ways that smoke may affect economies and discusses impacts that could result.
7.3.1 Theoretical Costs and Losses
Economists measure the costs and losses of a natural hazard (such as smoke production from a wildfire) or from an externality (such as smoke production from a prescribed fire) as changes in economic welfare, which includes gains and losses to both producers and consumers in each market, as well as true losses to the economy. Losses can be both direct and indirect. For wildfire, loss of life from smoke-induced illnesses or traffic fatalities due to decreased visibility are both direct losses. Indirect losses related to wildfire and smoke can include (1) business losses because of damage to capital, labor, and supply chains; (2) premature mortality resulting from damage to human health caused by wildfire emissions (Rittmaster et al. 2006; Fann et al. 2018; Borgschulte et al. 2019); and (3) losses due to altered perception of a community that might lead to changes in trade and investment (OECD 2016; World Bank 2016; Wouter Botzen 2019).
Economic costs can also result from actions taken to avoid or mitigate impact, also known as “averting behavior” (e.g., recreation shifts, evacuation, smoke avoidance) (Kochi et al. 2010). Averting behaviors, along with redirecting of recreation, tourism, investment, and trade, create losses in the affected area but may create gains elsewhere. Although there is no empirical evidence that intermittent smoke events have affected air quality sufficiently to alter investments or migration, economic theory would imply that changes in air quality would affect long-term investments and migration, potentially resulting in either spatial or temporal shifts in behavior. An overview of the costs of wildfires in Oregon noted the possibility of investment and migration losses, but did not attempt to quantify such losses (Lehner 2018). Box 7.3 summarizes the types of economic losses that could be enumerated from a smoke event.
Few studies have examined how wildland fire smoke affects any of the above potential economic losses. This is likely due, in part, to challenges in distinguishing between smoke-specific losses versus losses from the fire more broadly, although some work has addressed valuation of economic losses by measuring willingness to pay for a smoke-free day (World Bank 2016). Fann et al. (2018) applied the fire-attributable PM effects from Delfino (2009) in a national assessment of health-related economic losses associated with wildfire smoke using BenMAP-CE (USEPA 2014). However, the potential smoke-related costs and losses described in Box 7.3 have not been comprehensively assessed in any empirical studies. The following sections discuss three areas where limited research is available: (1) direct and indirect health costs and losses, (2) evacuation as an averting behavior, and (3) displaced recreation/tourism.
Box 7.3 Classification of Potential Damages, Costs, and Losses Caused by Wildland Fire Smoke
Direct (occurs during the smoke event) |
• Damage to productive capital and inventories |
• Damage to housing stock |
• Damage to infrastructure |
• Damage to human capital—includes direct fatalities and injuries from smoke, and fatalities and injuries from traffic accidents due to reduced visibility during the event |
Indirect (can be during or after the smoke event) |
• Damage to human capital (manifested after the event, including premature mortality and long-term morbidity) |
• Business losses because of supply shifts resulting from |
– Damage to capital (human, infrastructure, manufacturing and business, agricultural) |
– Disruption to supply chains (including transportation disruption) |
• Business losses because of demand shifts resulting from |
– Averting behaviors affecting consumption (recreation, evacuation, and transportation) |
– Increased health expenditures that reduce expenditures on other things |
• Losses because of perceptions |
– Trade: shutdowns, cancellations, and transportation difficulties can make trade partners less confident, reducing trade in the short and long run—will trade elsewhere |
– Investment: averting behavior—will invest elsewhere |
7.3.2 Health Costs and Losses
A smoke event, whether from wildfire or prescribed fire, can lead to direct welfare losses through damage to human capital (fatalities and injuries), and indirect welfare losses from longer-term impacts on human health. Except in rare conditions, air pollution has not tended to result in hazardous visibility conditions (see 1952 London fog for a counter example; Wang et al. 2016). However, recent years have seen growing concern about smoke impacts on transportation, particularly in relation to formation of superfog (see Chap. 4). Here, we assess what is known about economic costs and losses resulting from wildland fire smoke.
Similar to health effects research, studies on the economic impacts of air pollution focus on the role of PM2.5. Two main methods have been used to value morbidity impacts: (1) cost of illness (COI), and (2) contingent valuation-based willingness to pay (WTP). The two methods would be expected to generate different values, because the WTP measures also might include consideration of averting costs incurred by victims, as well as the direct costs of suffering an air-quality-based illness.
The economic value of disease varies by type of illness. Kochi et al. (2010) found that the ratio of WTP to COI is 1.3–2.4 for asthma, cataracts, and angina symptoms, with typical ratios ranging from 1.5 to 2.0. They also report that the USEPA estimates that WTP of each case during a wildfire smoke event ranges from $8 (2007 dollars) to avoid shortness of breath, to $10,971 to avoid respiratory hospital admissions, and $15,105 for a cardiovascular hospital admission. Nationwide annual hospital admissions that could be attributed to wildfire smoke from 2008 to 2012 ranged from 3900 to 8500 respiratory admissions and 1700–2800 cardiovascular admissions (Fann et al. 2018). Based on the economic value of those admissions, annual nationwide costs would be $43–93 million for respiratory illness and $26–42 million for cardiovascular illnesses caused by wildfires.
Annual economic losses from mortality effects of wildfire smoke have been estimated as nearly 1000 times higher than the economic losses attributed to morbidity from wildfire smoke in the USA. Kochi et al. (2010) identified a range of $2–14 million annually for economic loss per human life lost, conceived as the value of statistical life (VSL). A central estimate was established as $7.6 million (in 2007 dollars), which is the figure used by the USEPA in its impact assessments for air quality, and by Fann et al. (2018) in their nationwide assessment of the economic impacts of wildfire smoke emissions in the USA. Fann et al. (2018) summarized economic losses based on VSL for mortality from wildfire smoke events from 2008 to 2012, finding a median estimate of $11–20 billion per year for short-term exposures and hospital admissions and $76–130 billion per year for long-term effects of smoke exposure and respiratory hospital admissions. Therefore, the total value of the lives lost ranged from $88 billion in 2009 to $142 billion in 2008, with interannual variation depending on the area burned and location of fires relative to human populations. Overall, for the five years of the study, losses from premature mortality and hospital visits related to smoke averaged $103 billion per year in the USA.
7.3.3 Evacuation as an Averting Behavior
Evacuation is an economically disruptive activity, resulting in time off work, longer commutes, increased expenditures on housing and food, loss of social networks, stress, and discomfort. However, evacuation specifically because of smoke is not recommended; rather, sheltering in place is generally the preferred public health and safety redress (CARPA 2014; USEPA 2019c). A number of recommended public health actions can result in additional expenditures for residents and homeowners (e.g., creating a “clean room” at home, or missing work).
The accepted “correct” methodology for evaluating averting costs and losses resulting from a smoke event is to query residents on their willingness to pay to avoid a smoky day. A recent study found that residents were willing to pay an average of $129 per person per day to avoid a smoky day (Jones 2018). The author suggested this amount might account for the costs of averting behaviors, including evacuation and the need to clean indoor air or filter outdoor air. It may reflect expected expenditures on hospital visits to the extent that the residents surveyed had experienced these expenditures and were aware of the costs imposed by the smoke event. However, more than a single survey is needed to assess the value of an individual day of smoke avoidance.
7.3.4 Displaced Recreation and Tourism
In economic studies, it is assumed that a specific recreation choice provides the greatest benefit to the consumer and that being required, or choosing, to recreate in a different place or at a different time period to avoid smoke will result in a loss to the consumer and possibly result in increased costs (e.g., if the distance traveled must be increased). Although there is evidence that tourism and travel expenditures are affected by wildfires, these effects have not been isolated specifically for smoke (Butry et al. 2001; Rahn 2009; Kootenay Rockies Tourism Association 2018), although we can assume that at least some of the impacts are due to smoke. Other summaries have noted the costs of event cancellations from smoke, particularly when events are scheduled outdoors (e.g., outdoor theaters and raceways) (Lehner 2018).
7.4 Social Acceptance and Risk Communication
7.4.1 Social Acceptability
Research specific to public perspectives and response to wildland fire smoke is limited, with most relevant findings emerging from specific questions in studies that were focused broadly on social acceptance of prescribed fire. This research has consistently found that approximately 30% of survey respondents indicate someone in their household has a health issue affected by smoke. For these individuals and households, smoke tends to be a particularly salient topic. However, for most individuals, smoke is less critical in shaping acceptance of prescribed burning. Instead, understanding the beneficial ecological effects of fire and trust in those who are implementing the prescribed burn are more critical. Research also has shown that concerns about prescribed fire smoke tend to decrease with greater understanding of the ecological benefits of fire (McCaffrey and Olsen 2012).
Two recent studies (Blades et al. 2014; Olsen et al. 2014) did focus on public perceptions and preferences around smoke. This work included populations in both rural and urban areas of different regions in the USA and found that the majority of respondents were tolerant of all types of wildland fire smoke, with the highest tolerance for smoke from wildfires that were being actively suppressed. Slightly lower tolerance levels were found for smoke from prescribed fires and managed naturally-ignited fires. However, tolerance for smoke from both types of fire was significantly higher when forest health objectives were mentioned. Overall, the two studies found that human health status was the strongest predictor of smoke tolerance, with those who had experienced personal health effects from wildfire smoke being less tolerant. No significant differences between rural and urban residents were found in the two studies, and the few differences between regions were attributed to specific local context (Engebretson et al. 2016). One of the studies conducted a conjoint analysis in which the relative importance of advance warning was consistently found to be (slightly) higher than negative health effects or smoke duration as an influence on smoke tolerance levels. This highlights the importance of the communication process in allowing people to mitigate or avoid potential smoke impacts (Blades et al. 2014).
7.4.2 Risk Communication
Risk communication focuses on identifying the most effective means of providing information about a potential risk or threat to the health and safety of people or the environment and in a way that encourages appropriate protective actions (Reynolds and Seeger 2005; Steelman and McCaffrey 2013). Effective risk communication ensures that information is timely, accurate, and credible. To date, most research at the intersection of risk communication and wildland fire has focused on communication about a specific fire event (e.g., Steelman and McCaffrey 2013). However, interest in research on risk communication about the public health impacts of smoke events is growing (Olsen et al. 2014).
Deploying risk communication messaging during a wildfire smoke event is an essential strategy for protecting public health (Hano et al. 2020a). The messaging is designed to increase awareness of the issue among at-risk populations and the general public in an effort to support individual decisions that can mitigate or minimize exposure to smoke (Elliott 2014; Fish et al. 2017). During a smoke event, the type of information provided to affected populations may include status of the wildfire, wildfire smoke forecasts, and what actions people can take to protect themselves. Depending on factors such as air quality levels and the populations most at risk, specific public health recommendations regarding actions to reduce smoke exposure may differ but generally include: stay indoors, reduce outdoor physical activity, wear a properly fitted particulate-filtering respirator, develop and activate an asthma/COPD action plan, and create an at-home clean air room (Elliott 2014; USEPA 2019c; Joseph et al 2020). Recommendations and alerts may be deployed using television, radio, community meetings, newspapers, social media, and mobile applications. The source of information can include trusted news outlets, public health professionals, governmental agencies, medical providers, and fire response teams.
Investigating the effectiveness of risk communication for encouraging the adoption of specific recommended behaviors in the context of wildland fire is a growing area of research. Models of health behavior provide some guidance for structuring and deploying risk communication messaging. Recent research suggests that, similar to other public health domains, an individual’s attitudes and risk perception may influence individual decision-making regarding exposure-reducing behaviors (Hano et al. 2020b). Findings and recommendations from the few studies that have examined risk communication during smoke events are similar to those found in the broader literature on health-risk communication.
7.4.2.1 Protective Actions
Minimal research has examined the effectiveness of wildfire smoke-related public health messages in leading to appropriate protective action. Most studies are retrospective and observational, limiting the ability to infer causation (Fish et al. 2017). Initial evidence indicates that messages that use plain language and are non-technical—such as “stay indoors” and “reduce outdoor physical activity”—are more commonly recalled and understood, and have a higher compliance rate (Sugerman et al. 2012; Dix-Cooper 2014; Fish et al. 2017). A study conducted in New South Wales, Australia, found that 42.5% of respondents reported a behavior change due to hearing a public health message, with staying indoors and reducing outdoor activity being the most common actions (Burns et al. 2010).
There is some evidence that certain groups are more likely to follow recommended public health actions including: those with chronic respiratory disease or high socioeconomic status, young or middle-aged adults, parents with young children, and native or primary English speakers (Dix-Cooper 2014; Fish et al. 2017). Although initial evidence shows the most common action taken was to stay indoors, it is difficult to infer from current studies if this action would have been taken by the population regardless of advisories (Fish et al. 2017). Limited information is available on adoption of other recommended protective actions, such as use of high-efficiency particulate air (HEPA) filters, and no information is available on compliance with public health messages or recommendations related to the duration of a smoke event, frequency of messages released, or length of time a message has been issued (Fish et al. 2017).
Few studies have evaluated how effective different recommended protective actions are in decreasing health impacts from smoke. However, there is growing evidence that demonstrates the effectiveness of filtration devices and behavioral modifications for reducing exposure to PM2.5 (Rajagopalan et al. 2020). There is some evidence that air cleaners with HEPA filters can decrease exposures to smoke (Barn et al. 2016) and reduce the odds of experiencing adverse health effects associated with exposure (Mott et al. 2002).
Occupational studies have also shown that properly fitted N95 masks can substantially reduce particle exposure, although limited data are available on the benefits of using N95 masks by individuals who do not have access to fit testing for masks. There is growing evidence that demonstrates individual behaviors, such as avoiding air pollution by staying indoors, closing windows, and modifying exercise and outdoor activities, are effective strategies to reduce exposure to PM2.5 (Rajagopalan et al. 2020).
Finally, although individuals are generally advised to stay indoors, evidence is limited on the degree, and duration, that air quality is better indoors as compared to outdoors (Chap. 6), making it unclear when it is appropriate to provide guidance on sheltering people in locations without good ventilation systems (Shrestha et al. 2019). As wildfire seasons increase in length and more fires cause higher air pollution levels, it also will be important to know if recommending sheltering in place for extended periods offsets other public health concerns (e.g., mental health considerations).
7.4.2.2 Communication Channels and Timing
Risk communication literature suggests conventional mass communication channels tend to be the primary mechanisms for conveying health-risk communication during emergency response situations. Wolkin et al. (2019) recently analyzed a set of Community Assessments for Public Health Emergency Response conducted from 2014 to 2017 for chemical spill, harmful algal bloom, hurricane, and flood emergencies. Their study found that television was the main information source for most individuals, followed by social media, and word of mouth. The assessment concluded that using multiple communication methods increases the likelihood of reaching a large portion of the population, and that the use of social media and word of mouth can increase the timeliness of messaging and provide message confirmation from sources that communities trust.
A review of the limited literature examining smoke communication (Fish et al. 2017) found a wide range of communication channels were used for smoke health messages, including mass media, road signage, face-to-face communication, hotlines, and the Internet. The few studies focused on risk communication during wildfire smoke events support the wider literature with respect to public reliance on mass communication channels. Two studies (Kolbe and Gilchrist 2009; Sugerman et al.2012) found that television was the primary source for smoke information, whereas another found a preference for smoke information from local papers as well as from television (for those under 40) and government-funded radio (for those over 40) (Burns et al. 2010). One US study did find a preference for receiving smoke warnings via a phone call rather than mass media (Blades et al. 2014).
The limited evidence about which communication channels are most effective in reaching at-risk populations indicates that certain groups are less likely to receive smoke warnings, including those with lower income or education levels, individuals for whom English is a second language, and the elderly (Dix-Cooper 2014; Fish et al. 2017). Finally, there is a lack of studies investigating effective communication for reaching culturally and linguistically diverse communities (Fish et al. 2017).
Evidence on the use of social media is limited, although there are some indications that mobile applications (apps) and Twitter data may be useful means of monitoring real-time air quality (Fish et al. 2017; Sachdeva et al. 2018). A number of apps have been developed specific to national air quality and health including: AirRater (Australia; https://airrater.org), AQHI Canada (Canada; https://open.alberta.ca/interact/aqhi-canada), AirNow (USEPA; www.airnow.gov/airnow-mobile-app), and Smoke Sense (USEPA; www.epa.gov/air-research/smoke-sense-study-citizen-science-project-using-mobile-app). Early research related to these apps has focused on understanding users’ exposures to adverse air quality conditions and concurrent health symptoms (Johnston et al. 2018; Rappold et al. 2019), and preliminary evaluations of the effectiveness of mobile apps for mitigating adverse health impacts related to air quality (Rappold et al 2019; Campbell et al. 2020; Hatch 2020).
Trust in both the source and channel is a critical component of risk communication, influencing the saliency of messaging for the intended audience (Reynolds and Seeger 2005; Fish et al. 2017). General wildfire studies have found that trust in those providing information or implementing a practice is associated with a more positive public response to a practice (McCaffrey and Olsen 2012). No studies to date have specifically assessed trustworthy sources specific to smoke messages, but research about trusted information sources during a fire event found that information from fire officials and, to a lesser degree, friends and family were found to be trustworthy by a high portion of respondents; few found information from mass or social media to be trustworthy information sources (Steelman et al. 2015). Timing may also influence the saliency of health-risk communication. Mott et al. (2002) found that timely messaging about reducing wildfire smoke exposure using multiple channels (e.g., health care providers, radio broadcasts, and telephone messages) was associated with fewer reported respiratory symptoms among the general population.
7.5 Key Findings
Specific to social and societal implications of wildland fire smoke, the broadest body of research to date has focused on health effects of short-term PM2.5 exposures. Much of this understanding is derived from broader air pollution studies, with a growing body of research specific to smoke from wildland fires that generally has congruent findings.
-
Current understanding of the health effects of wildland fire smoke is rooted in decades of research examining the health effects of ambient air pollution, specifically PM2.5, with the strongest evidence for effects on the respiratory and cardiovascular systems, as well as mortality.
-
Studies of wildland fire smoke report consistent evidence of a positive association with respiratory effects such as asthma and COPD exacerbations, and related increases in medication usage and physician visits.
-
A growing body of research is providing consistent evidence of links between wildfire smoke, specifically wildfire-specific PM2.5 exposure and adverse cardiovascular impacts, including ischemic heart disease, cardiac arrhythmia, and heart failure.
-
-
Although wildland fire smoke exposure has the potential to elicit adverse health effects among the general population, some populations and life stages are potentially at greater risk. Health effects from smoke are more common for individuals with preexisting cardiovascular or respiratory disease, older adults, children, pregnant people, outdoor workers, and possibly for those of lower SEP.
-
Although a complete characterization of economic costs of wildland fire smoke is unavailable, limited economic research suggests that health costs and losses could be considerable. Economic losses associated with the health impacts of wildfire smoke are estimated to range from $88 billion to $142 billion per year, with the majority of those losses arising from premature human mortality.
-
There is initial evidence that smoke from wildland fires can have a number of significant economic impacts, including those occurring due to temporary disruptions to lives and businesses, visibility problems resulting in transportation issues, alteration of recreation and tourism destinations or timing, and business losses through inventory damages and supply chain disruption.
-
There is good evidence that, for most individuals, smoke is not a critical concern in determining acceptance of prescribed fire, instead this acceptance is based primarily on understanding of associated ecological benefits and trust in those who are implementing a prescribed burn. However, for households with health issues, smoke is a significant influence on prescribed fire acceptance. In addition, those who have recently experienced personal health effects from smoke are less tolerant of smoke in general. There is limited evidence that most individuals are receiving smoke messages and following advice to stay indoors.
7.6 Key Information Needs
Broadly speaking, a number of data gaps and challenges affect our ability to routinely conduct health-risk assessments and risk communication activities, and also limit assessments of economic effects of smoke, in relation to both short-term and long-term exposure. There are four general areas for which more information, both observational and experimental, is needed:
7.6.1 Understudied Health Effects
-
More research is needed to better understand the health effects attributed to high smoke exposures (i.e., high PM2.5 concentrations) during wildland fire events, specifically the effect of smoke exposure on cardiovascular and reproductive outcomes, as well as fetal development (which could potentially affect future chronic disease development and have intergenerational impacts), and the identification of populations at increased risk of smoke-related health effects.
-
Improved understanding of the impact of repeated exposures to high concentrations of wildfire smoke and long-term chronic exposures over multiple fire seasons is critical, as this can inform studies of health impacts due to both short-term and long-term exposures. Currently, there are significant challenges in our ability to develop robust study designs and access historical health and smoke concentration data at appropriate spatiotemporal scales. The development of an occupational health surveillance system for wildland firefighter may provide information on the long-term effects of exposure to smoke for both workers and the general public.
-
To fully understand the health burden of wildland fire smoke exposure, it will be important to consider both physical and mental health effects resulting from fire events. Therefore, we need to improve our knowledge of mental health impacts of smoke, particularly in relation to long-duration events.
-
An emerging issue is the need to understand how wildfires that burn human infrastructure may adversely affect the mixture of air pollutants (Chaps. 5 and 6) and potential health effects.
7.6.2 Health Benefits and Trade-Offs of Public Health Interventions
-
A better understanding is needed of which protective actions individuals are taking in response to smoke, whether the actions taken are appropriate given an individual’s health status (e.g., being classified as “at-risk”), and barriers to taking protective actions to mitigate adverse health impacts.
-
Experimental research is needed to assess the effectiveness of various risk communication messages and strategies (including best management practices) around smoke, particularly for at-risk groups.
-
A better understanding is needed of effective risk communication strategies when high smoke concentrations coincide with other environmental hazards (e.g., high smoke PM levels during a heat wave). An assessment is needed of the effects of public-safety power-shutoff procedures on public health, especially should that coincide with an extreme heat event.
7.6.3 Economic Impacts
Additional research is needed to validate estimates of the values of human mortality, the economic impacts of evacuations specifically attributable to smoke on local economies, and the economic impacts of smoke on transportation networks and local businesses.
7.6.4 Central Repository of Standards and Actions
A central repository with data collection standards for smoke predictions would provide much needed information to accurately and consistently characterize population-level exposures. The public health community typically relies on exposure models, using data derived from various environmental data sources, including air quality measurements from monitors, chemical transport models, and remotely sensed information. Although such smoke exposure modeling efforts are feasible, they are resource intensive. The paucity of literature on effective solutions suggests that more research is needed to gain insight on health consequences of smoke exposure.
7.7 Conclusions
More empirical information on the acute and chronic health effects and economic impacts of wildland fire smoke exposures, as well as the protective actions that are taken in response to smoke risk communication, will be critical to improving future outcomes and effectively building on current biophysical research efforts. However, despite the large and potentially growing societal impacts of wildland fire smoke on a range of values, only a limited amount of scientific data are available that are useful for assessing these impacts. In particular, there are two hurdles specific to social research that present challenges to an improved understanding.
First, it is difficult to attribute a given health or economic outcome to one or more high pollution-exposure events or to measure the impacts of exposure on specific human or societal outcomes. Scientific studies of the effects of smoke on humans and society are observational; identifying the effects of specific interventions requires accounting for the influences of correlated and potentially confounding environmental and human factors. Furthermore, such science is complicated by the need to measure smoke transport across large distances, quantify human exposures to smoke, and model how humans respond to smoke with mitigating and averting behaviors.
Second, micro-level studies on how humans are affected by smoke are constrained by controls on personal health information, including health histories, which may be critical to obtaining a comprehensive and accurate assessment of the impacts of smoke on people. Economic studies of the effects of smoke are similarly inhibited by the limited availability of high-frequency economic time-series data, which could accurately reveal the timing and magnitudes of responses to evacuation orders or mitigating actions by individuals and businesses in affected locations.
Although these hurdles are significant, many can be addressed but would require research efforts similar to those that have contributed to the current understanding of the biophysical and chemical aspects of smoke.
References
Abdo M, Ward I, O’Dell K et al (2019) Impact of wildfire smoke on adverse pregnancy outcomes in Colorado, 2007–2015. Int J Environ Res Public Health 16:3720
Achtemeier GL (2008) Effects of moisture released during forest burning on fog formation and implications for visibility. J Appl Meteorol Climatol 47:1287–1296
Adetona AM, Adetona O, Gogal RM et al (2017) Impact of work task-related acute occupational smoke exposures on select proinflammatory immune parameters in wildland firefighters. J Occup Environ Med 59:679–690
Adetona O, Dunn K, Hall DB et al (2011a) Personal PM(2.5) exposure among wildland firefighters working at prescribed forest burns in Southeastern United States. J Occup Environ Hyg 8:503–511
Adetona O, Hall DB, Naeher LP (2011b) Lung function changes in wildland firefighters working at prescribed burns. Inhalation Toxicol 23:835–841
Adetona AM, Martin WK, Warren SH et al (2019) Urinary mutagenicity and other biomarkers of occupational smoke exposure of wildland firefighters and oxidative stress. Inhalation Toxicol 31:73–87
Adetona O, Reinhardt TE, Domitrovich J et al (2016) Review of the health effects of wildland fire smoke on wildland firefighters and the public. Inhalation Toxicol 28:95–139
Adetona O, Simpson CD, Onstad G, Naeher LP (2013) Exposure of wildland firefighters to carbon monoxide, fine particles, and levoglucosan. Ann Occup Hyg 57:979–991
Alman BL, Pfister G, Hao H et al (2016) The association of wildfire smoke with respiratory and cardiovascular emergency department visits in Colorado in 2012: a case crossover study. Environ Health 15:64
Amegah AK, Quansah R, Jaakkola JJ (2014) Household air pollution from solid fuel use and risk of adverse pregnancy outcomes: a systematic review and meta-analysis of the empirical evidence. PloS One 9:e113920
Analitis A, Georgiadis I, Katsouyanni K (2012) Forest fires are associated with elevated mortality in a dense urban setting. Occup Environ Med 69:158–162
Barn PK, Elliott CT, Allen RW et al (2016) Portable air cleaners should be at the forefront of the public health response to landscape fire smoke. Environ Health 15:116
Black C, Tesfaigzi Y, Bassein JA, Miller LA (2017) Wildfire smoke exposure and human health: significant gaps in research for a growing public health issue. Environ Toxicol Pharmacol 55:186–195
Blades JJ, Shook SR, Hall TE (2014) Smoke management of wildland and prescribed fire: understanding public preferences and trade-offs. Can J for Res 44:1344–1355
Borchers AN, Horsley JA, Palmer AJ et al (2019) Association between fire smoke fine particulate matter and asthma-related outcomes: systematic review and meta-analysis. Environ Res 179:108777
Borgschulte M, Molitor D, Zou EY (2019) Air pollution and the labor market: evidence from wildfire smoke. Online working paper. https://www.aeaweb.org/conference/2020/preliminary/paper/YYnFtk9N#:~:text=We%20calculate%20that%2017.7%20days,%24147%20billion%20in%202018%20dollars. Accessed 6 Jan 2021
Brey SJ, Fischer EV (2016) Smoke in the city: how often and where does smoke impact summertime ozone in the United States? Environ Sci Technol 50:1288–1294
Brook RD, Rajagopalan S, Pope CA III et al (2010) Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 121:2331–2378
Burke M, Driscoll A, Heft-Neal S et al (2021) The changing risk and burden of wildfire in the United States. In: Proceedings of the national academies of sciences, USA, vol 118, p e2011048118
Burns R, Robinson P, Smith P (2010) From hypothetical scenario to tragic reality: a salutary lesson in risk communication and the Victorian 2009 bushfires. Aust N Z J Public Health 34:24–31
Butry DT, Mercer DE, Prestemon JP et al (2001) What is the price of catastrophic wildfire? J Forest 99:9–17
Buysse CE, Kaulfus A, Nair U, Jaffe DA (2019) Relationships between particulate matter, ozone, and nitrogen oxides during urban smoke events in the Western US. Environ Sci Technol 53:12519–12528
California Air Response Planning Alliance (CARPA) (2014) Wildfire smoke response coordination—best practices being implemented by agencies in California, Working draft. https://ww3.arb.ca.gov/smp/progdev/iasc/wildfireresponse.pdf. Accessed 18 June 2020
Campbell SL, Jones PJ, Williamson GJ et al (2020) Using digital technology to protect health in prolonged poor air quality episodes: a case study of the AirRater App during the Australian 2019–20 Fires. Fire 2020:40
Cançado JE, Saldiva PH, Pereira LA et al (2006) The impact of sugar cane–burning emissions on the respiratory system of children and the elderly. Environ Health Perspect 114:725–729
Candido da Silva AM, Moi GP, Mattos IE, de Souza Hacon S (2014) Low birth weight at term and the presence of fine particulate matter and carbon monoxide in the Brazilian Amazon: a population-based retrospective cohort study. BMC Pregnancy Childbirth 14:309
Cascio WE (2018) Wildland fire smoke and human health. Sci Total Environ 624:586–595
Centers for Disease Control and Prevention (CDC) (2017) Fast Stats: Asthma. https://www.cdc.gov/nchs/fastats/asthma.htm. Accessed 18 June 2020
Centers for Disease Control and Prevention (CDC) (2019) Basics about COPD. https://www.cdc.gov/copd/basics-about.html. Accessed 18 June 2020
Chen L, Verrall K, Tong S (2006) Air particulate pollution due to bushfires and respiratory hospital admissions in Brisbane, Australia. Int J Environ Health Res 16:181–191
DeCicca P, Malak N (2020) When good fences aren’t enough: the impact of neighboring air pollution on infant health. J Environ Econ Manage 102:102324
DeFlorio-Barker S, Crooks J, Reyes J, Rappold AG (2019) Cardiopulmonary effects of fine particulate matter exposure among older adults, during wildfire and non-wildfire periods, in the United States 2008–2010. Environ Health Perspect 127:037006
Delfino RJ, Brummel S, Wu J et al (2009) The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occup Environ Med 66:189–197
Dennekamp M, Straney LD, Erbas B et al (2015) Forest fire smoke exposures and out-of-hospital cardiac arrests in Melbourne, Australia: a case-crossover study. Environ Health Perspect 123:959–964
Dix-Cooper L (2014) Evidence review: reducing time outdoors during wildfire smoke events. BC Centre for Disease Control, Vancouver, British Columbia. http://www.bccdc.ca/resourcegallery/Documents/Guidelines%20and%20Forms/Guidelines%20and%20Manuals/HealthEnvironment/WFSG_EvidenceReview_ReducingTimeOutdoors_FINAL_v6trs.pdf. Accessed 1 July 2020
Dodd W, Scott P, Howard C et al (2018) Lived experience of a record wildfire season in the Northwest Territories, Canada. Can J Public Health 109:327–337
Domitrovich J, Broyles G, Ottmar RD et al (2017) Wildland fire smoke health effects on wildland firefighters and the public. U.S. Forest Service, Pacific Northwest Research Station, Final Report, JFSP13-1-02-14. https://www.firescience.gov/projects/13-1-02-14/project/13-1-02-14_final_report.pdf. Accessed 18 June 2020
Doubleday A, Schulte J, Sheppard L et al (2020) Mortality associated with wildfire smoke exposure in Washington state, 2006–2017: a case-crossover study. Environ Health 19:1–10
Duncan GJ, Daly MC, McDonough P, Williams DR (2002) Optimal indicators of socioeconomic status for health research. Am J Public Health 92:1151–1157
Elliott CT (2014) Guidance for BC public health decisions makers during wildfire smoke events. BC Centre for Disease Control, Vancouver, British Columbia. http://www.bccdc.ca/resourcegallery/Documents/Guidelines%20and%20Forms/Guidelines%20and%20Manuals/Health-Environment/WFSG_BC_guidance_2014_09_03trs.pdf. Accessed 1 July 2020.
Engebretson JM, Hall TE, Blades JJ et al (2016) Characterizing public tolerance of smoke from wildland fires in communities across the United States. J Forest 114:601–609
Fann N, Alman B, Broome RA et al (2018) The health impacts and economic value of wildland fire episodes in the US: 2008–2012. Sci Total Environ 610:802–809
Faustini A, Alessandrini ER, Pey J et al (2015) Short-term effects of particulate matter on mortality during forest fires in Southern Europe: results of the MED-PARTICLES Project. Occup Environ Med 72:323–329
Fish J, Peters M, Ramsey I et al (2017) Effectiveness of public health messaging and communication channels during smoke events: a rapid systematic review. J Environ Manage 193:247–256
Galobardes B, Shaw M, Lawlor DA et al (2006) Indicators of socioeconomic position (part 1). J Epidemiol Community Health 60:7–12
Gan RW, Ford B, Lassman W et al (2017) Comparison of wildfire smoke estimation methods and associations with cardiopulmonary-related hospital admissions. GeoHealth 1:122–136
Gan RW, Liu JC, Ford B et al (2020) The association between wildfire smoke exposure and asthma-specific medical care utilization in Oregon during the 2013 wildfire season. J Eposure Sci Environ Epidemiol 1:11
Gaughan DM, Piacitelli CA, Chen BT et al (2014) Exposures and cross-shift lung function declines in wildland firefighters. J Occup Environ Hyg 11:591–603
Gehring U, Tamburic L, Sbihi H et al (2014) Impact of noise and air pollution on pregnancy outcomes. Epidemiology 25:351–358
General S (2014) The health consequences of smoking—50 years of progress: a report of the surgeon general. US Department of Health and Human Services
Groß S, Esselborn M, Weinzierl B et al (2013) Aerosol classification by airborne high spectral resolution lidar observations. Atmos Chem Phys 13:2487–2505
Hano MC, Prince SE, Wei L et al (2020) Knowing your audience: a typology of smoke sense participants to inform wildland fire smoke health risk communication. Front Public Health 8:143
Hano MC, Wei L, Hubbell B, Rappold AG (2020) Scaling up: citizen science engagement and impacts beyond the individual. Citizen Sci Theory Pract 5:1
Hatch A (2020) WSU study will use phone app to help people with asthma during wildfire season. WSU Insider, 12 August. Washington State University, Pullman. https://news.wsu.edu/2020/08/12/wsu-study-will-use-phone-app-help-people-asthma-wildfire-season. Accessed 28 Jan 2021
Hejl AM, Adetona O, Diaz-Sanchez D et al (2013) Inflammatory effects of woodsmoke exposure among wildland firefighters working at prescribed burns at the Savannah River Site, SC. J Occup Environ Hyg 10:173–180
Henderson SB, Brauer M, MacNab YC, Kennedy SM (2011) Three measures of forest fire smoke exposure and their associations with respiratory and cardiovascular health outcomes in a population-based cohort. Environ Health Perspect 119:1266–1271
Henn SA, Butler C, Li J et al (2019) Carbon monoxide exposures among U.S. wildland firefighters by work, fire, and environmental characteristic and conditions. J Occup Environ Hyg 16:793–803
Holstius DM, Reid CE, Jesdale BM, Morello-Frosch R (2012) Birth weight following pregnancy during the 2003 Southern California wildfires. Environ Health Perspect 120:1340–1345
Hu CY, Huang K, Fang Y et al (2020) Maternal air pollution exposure and congenital heart defects in offspring: a systematic review and meta-analysis. Chemosphere 253:126668
Hutchinson JA, Vargo J, Milet M et al (2018) The San Diego 2007 wildfires and medi-cal emergency department presentations, inpatient hospitalizations, and outpatient visits: an observational study of smoke exposure periods and a bidirectional case-crossover analysis. PLoS Med 15:e1002601
Inouea T, Nunokawab N, Kurisub D, Ogasawara K (2020) Particulate air pollution, birth outcomes, and infant mortality: evidence from Japan's automobile emission control law of 1992. SSM Popul Health 11:100590
Ignotti E, Hacon SdeS, Junger WL et al (2010) Air pollution and hospital admissions for respiratory diseases in the subequatorial Amazon: a time series approach. Cadernos de Saude Publica 26:747–761
Jacobson LdaS, Hacon SdeS, Castro HA et al (2012) Association between fine particulate matter and the peak expiratory flow of schoolchildren in the Brazilian subequatorial Amazon: a panel study. Environ Res 117:27–35
Jacobson LdaS, Hacon SdeS, Castro HA et al (2014) Acute effects of particulate matter and black carbon from seasonal fires on peak expiratory flow of schoolchildren in the Brazilian Amazon. PloS One 9:e104177
Jalaludin B, Smith M, O’Toole B, Leeder S (2000) Acute effects of bushfires on peak expiratory flow rates in children with wheeze: a time series analysis. Aust N Z J Public Health 24:174–177
Johnston F, Hanigan I, Henderson S et al (2011) Extreme air pollution events from bushfires and dust storms and their association with mortality in Sydney, Australia 1994–2007. Environ Res 111:811–816
Johnston F, Purdie S, Jalaludin B et al (2014) Air pollution events from forest fires and emergency department attendances in Sydney, Australia 1996–2007: a case-crossover analysis. Environ Health 13:105
Johnston FH, Wheeler AJ, Williamson GJ et al (2018) Airrater Tasmania: using smartphone technology to understand local environmental drivers of symptoms in people with asthma and allergic rhinitis. J Allergy Clin Immunol 141:AB84
Jolly WM, Cochrane MA, Freeborn PH et al (2015) Climate-induced variations in global wildfire danger from 1979 to 2013. Nat Commun 6:7537
Jones BA (2018) Willingness to pay estimates for wildfire smoke health impacts in the US using the life satisfaction approach. J Environ Econ Policy 7:403–419
Jones CG, Rappold AG, Vargo J et al (2020) Out‐of‐hospital cardiac arrests and wildfire‐related particulate matter during 2015–2017 California wildfires. J Am Heart Assoc 9:e014125
Joseph G, Schramm PJ, Vaidyanathan A, Breysse P, Goodwin B (2020) Evidence on the use of indoor air filtration as an intervention for wildfire smoke pollutant exposure. United States Centers for Disease Control and Prevention, Atlanta, GA. https://www.cdc.gov/air/wildfire-smoke/socialmedia/Wildfire-Air-Filtration-508.pdf. Accessed July 2020
Kiser D, Metcalf WJ, Elhanan G et al (2020) Particulate matter and emergency visits for asthma: a time-series study of their association in the presence and absence of wildfire smoke in Reno, Nevada, 2013–2018. Environ Health 19:92
Kochi I, Donovan GH, Champ PA, Loomis JB (2010) The economic cost of adverse health effects from wildfire-smoke exposure: a review. Int J Wildland Fire 19:803–817
Kolbe A, Gilchrist KL (2009) An extreme bushfire smoke pollution event: health impacts and public health challenges. NWS Public Health Bulletin 20:19–23
Kollanus V, Prank M, Gens A et al (2016) Mortality due to vegetation fire-originated PM2. 5 exposure in Europe-assessment for the years 2005 and 2008. Environ Health Perspect 125:30–37
Kondo MC, De Roos AJ, White LS et al (2019) Meta-analysis of heterogeneity in the effects of wildfire smoke exposure on respiratory health in North America. Int J Environ Res Public Health 16:960
Kootenay Rockies Tourism Association. (2018) Economic impact of 2017 wildfires on tourism in the Kootenay Rockies tourism region (final). Kootenay Rockies Tourism Association, Kimberley, British Columbia. https://www.krtourism.ca/wp-content/uploads/2018/10/Wildfire-Recovery-Survey-2018.pdf. Accessed 22 June 2020
Lakshmi P, Virdi NK, Sharma A et al (2013) Household air pollution and stillbirths in India: analysis of the DLHS-II National Survey. Environ Res 121:17–22
Larsen AE, Reich BJ, Ruminski M, Rappold AG (2018) Impacts of fire smoke plumes on regional air quality, 2006–2013. J Eposure Sci Environ Epidemiol 28:319
Lee T-S, Falter K, Meyer P et al (2009) Risk factors associated with clinic visits during the 1999 forest fires near the Hoopa Valley Indian Reservation, California, USA. Int J Environ Health Res 19:315–327
Lehner J (2018) Wildfires: a preliminary economic assessment. Oregon Office of Economic Analysis, August 8. https://oregoneconomicanalysis.com/2018/08/08/wildfires-a-preliminary-economic-assessment. Accessed 2 Oct 2019
Li G, Li L, Liu D et al (2021) Effect of PM2.5 pollution on perinatal mortality in China. Sci Rep 11, 7596
Linares C, Carmona R, Salvador P, Díaz J (2018) Impact on mortality of biomass combustion from wildfires in Spain: a regional analysis. Sci Total Environ 622:547–555
Linares C, Carmona R, Tobías A et al (2015) Influence of advections of particulate matter from biomass combustion on specific-cause mortality in Madrid in the period 2004–2009. Environ Sci Pollut Res 22:7012–7019
Liu D, Tager IB, Balmes JR, Harrison RJ (1992) The effect of smoke inhalation on lung function and airway responsiveness in wildland fire fighters. Am Rev Respir Dis 146:1469–1473
Liu JC, Pereira G, Uhl SA et al (2015) A systematic review of the physical health impacts from non-occupational exposure to wildfire smoke. Environ Res 136:120–132
Liu JC, Wilson A, Mickley LJ et al (2017) Who among the elderly is most vulnerable to exposure to and health risks of fine particulate matter from wildfire smoke? Am Epidemiol 186:730–735
Martin KL, Hanigan IC, Morgan GG et al (2013) Air pollution from bushfires and their association with hospital admissions in Sydney, Newcastle and Wollongong, Australia 1994–2007. Aust N Z J Public Health 37:238–243
Martin TR, Bracken MB (1986) Association of low birth weight with passive smoke exposure in pregnancy. Am J Epidemiol 124:633–642
McCaffrey SM, Olsen CS (2012) Research perspectives on the public and fire management: a synthesis of current social science on eight essential questions. (General Technical Report NRS-GTR-104). U.S. Forest Service, Northern Research Station, Newtown Square
McClure CD, Jaffe DA (2018) US particulate matter air quality improves except in wildfire-prone areas. Proc Nat Acad Sci USA 115:7901–7906
Miller LA (2019) Are adverse health effects from air pollution exposure passed on from mother to child? (Final report CN 15-303, California Air Resources Board). Regents of the University of California, Davis. https://ww2.arb.ca.gov/sites/default/files/classic/research/apr/past/15-303.pdf. Accessed 5 Feb 2021
Miranda AI, Martins V, Cascão P et al (2010) Monitoring of firefighters exposure to smoke during fire experiments in Portugal. Environ Int 36:736–745
Moore D, Copes R, Fisk R et al (2006) Population health effects of air quality changes due to forest fires in British Columbia in 2003. Can J Public Health 97:105–108
Morgan AD, Zakeri R, Quint JK (2018) Defining the relationship between COPD and CVD: what are the implications for clinical practice? Ther Adv Respir Dis 12:1753465817750524
Morgan G, Sheppeard V, Khalaj B et al (2010) Effects of bushfire smoke on daily mortality and hospital admissions in Sydney, Australia. Epidemiology 47–55
Mott JA, Mannino DM, Alverson CJ et al (2005) Cardiorespiratory hospitalizations associated with smoke exposure during the 1997 Southeast Asian forest fires. Int J Hyg Environ Health 208:75–85
Mott JA, Meyer P, Mannino D et al (2002) Wildland forest fire smoke: health effects and intervention evaluation, Hoopa, California, 1999. West J Med 176:157–162
Naeher LP, Brauer M, Lipsett M et al (2007) Woodsmoke health effects: a review. Inhalation Toxicol 19:67–106
National Heart, Lung, and Blood Institute (NHBLI) (2012) NHLBI FY 2012 Fact Book. U.S. National Institutes of Health, Dept. of Health and Human Services, Chap. 4. https://www.nhlbi.nih.gov/files/docs/factbook/FactBook2012.pdf. Accessed 11 Feb 2021
National Interagency Fire Center (NIFC) (2020) Interagency standards for fire and fire aviation operations (NFES 2724). Interagency Standards for Fire and Fire Aviation Operations Group, Boise.https://www.nifc.gov/PUBLICATIONS/redbook/2020/RedBookAll.pdf. Accessed 5 Feb 2021
Navarro K (2020) Working in smoke: Wildfire impacts on the health of firefighters and outdoor workers and mitigation strategies. Clin Chest Med 41:763–769
Navarro KM, Kleinman MT, Mackay CE et al (2019) Wildland firefighter smoke exposure and risk of lung cancer and cardiovascular disease mortality. Environ Res 173:462–468
Neitzel R, Naeher L, Paulsen M et al (2009) Biological monitoring of smoke exposure among wildland firefighters: a pilot study comparing urinary methoxyphenols with personal exposures to carbon monoxide, particular matter, and levoglucosan. J Eposure Sci Environ Epidemiol 19:349–358
O’Dell K, Ford B, Fischer EV, Pierce JR (2019) Contribution of wildland-fire smoke to us PM2.5 and its influence on recent trends. Environ Sci Technol 53:1797–1804
Occupational Safety and Health Administration (OSHA) (2017) Permissible Exposure Limits, 2017; Vol. 29 CFR 1910.1000.
Olsen C, Mazzotta D, Toman E, Fischer A (2014) Communicating about smoke from wildland fire: challenges and opportunities for managers. Environ Manage 54:571–582
Organisation for Economic Co-operation and Development (OECD) (2016) The economic consequences of outdoor air pollution: Policy highlights. OECD Policy Highlights, June. www.oecd.org.environment/the-economic-consequences-of-outdoor-air-pollution-9789264257474-en.htm. Accessed 22 June 2020
Ortman JM, Velkoff VA, Hogan H (2014) An aging nation: the older population in the United States (Report P25-1140 May). United States Census Bureau, Economics and Statistics Administration, Washington, DC. https://www.census.gov/prod/2014pubs/p25-1140.pdf. Accessed 22 June 2020
Permissible Exposure Limits, 29 CFR 1910.1000 C.F.R. § Table Z-1-A (2017)
Prunicki M, Kelsey R, Lee J et al (2019) The impact of prescribed fire versus wildfire on the immune and cardiovascular systems of children. Allergy 74:1989–1991
Rahn M (2009) Wildfire impact analysis. San Diego State University, San Diego, CA. http://universe.sdsu.edu/sdsu_newscenter/images/rahn2009fireanalysis.pdf. Accessed 22 June 2020
Rajagopalan S, Brauer M, Bhatnagar A et al (2020) Personal-level protective actions against particulate matter air pollution exposure: a scientific statement from the American Heart Association. Circulation 142:e411–e431, e448
Rappold AG, Cascio WE, Kilaru VJ et al (2012) Cardio-respiratory outcomes associated with exposure to wildfire smoke are modified by measures of community health. Environ Health 11:71
Rappold AG, Hano MC, Prince S et al (2019) Smoke Sense initiative leverages citizen science to address the growing wildfire-related public health problem. GeoHealth 3:443–457
Rappold AG, Stone SL, Cascio WE et al (2011) Peat bog wildfire smoke exposure in rural North Carolina is associated with cardiopulmonary emergency department visits assessed through syndromic surveillance. Environ Health Perspect 119:1415–1420
Reid CE, Brauer M, Johnston FH et al (2016) Critical review of health impacts of wildfire smoke exposure. Environ Health Perspect 124:1334–1343
Reid CE, Considine EM, Watson GL et al (2019) Associations between respiratory health and ozone and fine particulate matter during a wildfire event. Environ Int 129:291–298
Reid CE, Jerrett M, Tager IB et al (2016) Differential respiratory health effects from the 2008 northern California wildfires: a spatiotemporal approach. Environ Res 150:227–235
Reinhardt TE, Broyles G (2019) Factors affecting smoke and crystalline silica exposure among wildland firefighters. J Occup Environ Hyg 16:151–164
Reinhardt TE, Ottmar RD (2000) Smoke exposure at western wildfires. (Research Paper PNW-RP-525). U.S. Forest Service, Pacific Northwest Research Station, Portland
Reinhardt TE, Ottmar RD (2004) Baseline measurements of smoke exposure among wildland firefighters. J Occup Environ Hyg 1:593–606
Reisen F, Brown SK (2009) Australian firefighters’ exposure to air toxics during bushfire burns of autumn 2005 and 2006. Environ Int 35:342–352
Reisen F, Hansen D, Meyer CP (2011) Exposure to bushfire smoke during prescribed burns and wildfires: firefighters’ exposure risks and options. Environ Int 37:314–321
Reynolds B, Seeger M (2005) Crisis and emergency risk communication as an integrative model. J Health Commun 10:43–55
Rittmaster R, Adamowicz WL, Amiro B, Pelletier RT (2006) Economic analysis of health effects from forest fires. Can J for Res 36:868–877
Sachdeva S, McCaffrey S (2018) Using social media to predict air pollution during California wildfires. In: Proceedings of the international conference on social media and society, July 18–20; SM Society, Copenhagen
Sacks JD, Stanek LW, Luben TJ et al (2011) Particulate matter–induced health effects: who is susceptible? Environ Health Perspect 119:446–454
Semmens EO, Domitrovich J, Conway K, Noonan CW (2016) A cross-sectional survey of occupational history as a wildland firefighter and health. Am J Ind Med 59:330–335
Shrestha PM, Humphrey JL, Carlton EJ et al (2019) Impact of outdoor air pollution on indoor air quality in low-income homes during wildfire seasons. Int J Environ Res Public Health 16:3535
Steelman TA, McCaffrey S (2013) Best practices in risk and crisis communication: Implications for natural hazards management. Nat Hazards 65:683–705
Steelman TA, McCaffrey SK, Velez A-L, Briefel JA (2015) What information do people use, trust, and find useful during a disaster? Evidence from five large wildfires. Nat Hazards 76:615–634
Sugerman D, Keir J, Dee D et al (2012) Emergency health risk communication during the 2007 San Diego Wildfires: comprehension, compliance, and recall. J Health Commun 17:678–712
Swiston JR, Davidson W, Attridge S et al (2008) Wood smoke exposure induces a pulmonary and systemic inflammatory response in firefighters. Eur Respir J 32:129–138
Tham R, Erbas B, Akram M et al (2009) The impact of smoke on respiratory hospital outcomes during the 2002–2003 bushfire season, Victoria, Australia. Respirology 14:69–75
Thelen B, French NH, Koziol BW et al (2013) Modeling acute respiratory illness during the 2007 San Diego wildland fires using a coupled emissions-transport system and generalized additive modeling. Environ Health 12:94
U.S. Environment Protection Agency (USEPA) (2010) Integrated science assessment (ISA) for carbon monoxide (Final Report, Jan 2010). U.S. Environmental Protection Agency (EPA/600/R-09/019F). Washington, DC 2010. https://cfpub.epa.gov/ncea/isa/recordisplay.cfm?deid=218686
U.S. Environmental Protection Agency (USEPA) (2013) Integrated science assessment (ISA) for ozone and related photochemical oxidants (EPA 600/R-10/076F). Washington, DC
U.S. Environmental Protection Agency (USEPA) (2014) Environmental benefits mapping and analysis program—community edition (BenMAP-CE). https://www.epa.gov/benmap. Accessed 24 Sept 2019
U.S. Environmental Protection Agency (USEPA) (2019a) Integrated science assessment (ISA) for particulate matter (EPA/600/R-19/188). Washington, DC
U.S. Environmental Protection Agency (USEPA) (2019b) Wildfire smoke and your patients’ health. Washington, DC. https://www.epa.gov/wildfire-smoke-course. Accessed 14 July 2020
U.S. Environmental Protection Agency (USEPA) (2019c) Wildfire smoke: a guide for public health officials (EPA-452/R-19-901). Washington, DC. https://www3.epa.gov/airnow/wildfire-smoke/wildfire-smoke-guide-revised-2019.pdf. Accessed 14 July 2020
U.S. Environmental Protection Agency (USEPA) (2020) Integrated science assessment (ISA) for ozone and related photochemical oxidants (EPA/600/R-20/012). Washington, DC. https://cfpub.epa.gov/ncea/isa/recordisplay.cfm?deid=348522. Accessed 5 Feb 2021
Wang X, Zuckerman B, Pearson C et al (2002) Maternal cigarette smoking, metabolic gene polymorphism, and infant birth weight. JAMA 287:195–202
Wang G, Zhang R, Gomez ME et al (2016) Persistent sulfate formation from London Fog to Chinese haze. Proc Nat Acad Sci USA 113:13630–13635
Weber E, Adu-Bonsaffoh K, Vermeulen R et al (2020) Household fuel use and adverse pregnancy outcomes in a Ghanaian cohort study. Reprod Health 17:29
Wettstein ZS, Hoshiko S, Fahimi J et al (2018) Cardiovascular and cerebrovascular emergency department visits associated with wildfire smoke exposure in California in 2015. J Am Heart Assoc 7:e007492
Windham GC, Hopkins B, Fenster L, Swan SH (2000) Prenatal active or passive tobacco smoke exposure and the risk of preterm delivery or low birth weight. Epidemiology 11:427–433
Wolkin A, Schnall A, Nakata N, Ellis E (2019) Getting the message out: Social media and word-of-mouth as effective communication methods during emergencies. Prehosp Disaster Med 34:89–94
World Bank (2016) The cost of air pollution: strengthening the economic case for action. International Bank for Reconstruction and Development, The World Bank, Washington, DC. http://documents.worldbank.org/curated/en/781521473177013155/pdf/108141-REVISED-Cost-of-PollutionWebCORRECTEDfile.pdf. Accessed 1 July 2020
Wouter Botzen WJ, Deschenes O, Sanders M (2019) The economic impacts of natural disasters: a review of models and empirical studies. Rev Environ Econ Pol 13:167–188
Yao J, Eyamie J, Henderson SB (2016) Evaluation of a spatially resolved forest fire smoke model for population-based epidemiologic exposure assessment. J Eposure Sci Environ Epidemiol 26:233
Yao J, Stieb DM, Taylor E, Henderson SB (2019) Assessment of the air quality health index (AQHI) and four alternate AQHI-Plus amendments for wildfire seasons in British Columbia. Can J Public Health 111:96–106
Yao J, Brauer M, Wei J et al(2020). Sub-daily exposure to fine particulate matter and ambulance dispatches during wildfire seasons: a case-crossover study in British Columbia, Canada. Environ Health Perspect 128:067006
Youssouf H, Liousse C, Roblou L et al (2014) Non-accidental health impacts of wildfire smoke. Int J Environ Res Public Health 11:11772–11804
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 This is a U.S. government work and not under copyright protection in the U.S.; foreign copyright protection may apply
About this chapter
Cite this chapter
McCaffrey, S.M. et al. (2022). Social Considerations: Health, Economics, and Risk Communication. In: Peterson, D.L., McCaffrey, S.M., Patel-Weynand, T. (eds) Wildland Fire Smoke in the United States. Springer, Cham. https://doi.org/10.1007/978-3-030-87045-4_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-87045-4_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-87044-7
Online ISBN: 978-3-030-87045-4
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)