Abstract
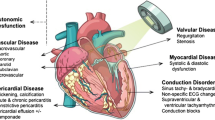
Chest radiation therapy (RT) is an important cause of cardiovascular disease in patients treated for cancers including lung, esophagus, mediastinal tumors, and especially Hodgkin disease and breast cancer.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Jaworski C, Mariani JA, Wheeler G, Kaye DM. Cardiac complications of thoracic irradiation. J Am Coll Cardiol. 2013;61:2319–28.
Aleman BM, van den Belt-Dusebout AW, De Bruin ML, van ’t Veer MB, Baaijens MH, de Boer JP, Hart AA, Klokman WJ, Kuenen MA, Ouwens GM, Bartelink H, van Leeuwen FE. Late cardiotoxicity after treatment for Hodgkin lymphoma. Blood 2007;109:1878–86.
Darby SC, Ewertz M, McGalle P, Bennet AM, Blom-Goldman U, Bronnum D et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368:987–98.
Borkenhagen JF, Bergom C, Rapp CT, et al. Dosimetric predictors of cardiotoxicity in thoracic radiotherapy for lung cancer. Clin Lung Cancer. 2019 Nov;20(6):435–41. doi: https://doi.org/10.1016/j.cllc.2019.05.014.
Taylor CW et al. Cardiac exposures in breast cancer radiotherapy: 1950’s–1990’s. Int J Radiat Oncol Biol Phys. 2007;69:1484–95.
Carver JR, Shapiro CL, Ng A, Jacobs L, Schwartz C, Virgo KS et al., ASCO cancer survivorship expert panel. American society of clinical oncology clinical evidence review on the ongoing care of adult cancer survivors: cardiac and pulmonary late effects. J Clin Oncol. 2007;25:3991–4008.
van Nimwegen FA, Schaapveld M, Janus CP, Krol AD, Petersen EJ, Raemaekers JM, Kok WE, Aleman BM, van Leeuwen FE. Cardiovascular disease after Hodgkin lymphoma treatment: 40-year disease risk. JAMA Intern Med. 2015;175:1007–17.
Meyer R, Gospodarowicz M, Connors J, et al., NCIC clinical trials group, eastern cooperative oncology group. ABVD alone versus radiation-based therapy in limited-stage Hodgkin’s lymphoma. N Engl J Med. 2012;366:399–408.
Stewart F, Hoving S, Russell N. Vascular damage as an underlying mechanism of cardiac and cerebral toxicity in irradiated cancer patients. Radiat Res. 2010;174:865–9.
Yusuf S, Sami S, Daher I. Radiation-induced heart disease: a clinical update. Cardiol Res Pract. 2011;(317659):9. doi: https://doi.org/10.4061/2011/317659.
Lancellotti P, Nkomo VT, Badano LP, et al. Expert consensus for multi-modality imaging evaluation of cardiovascular complications of radiotherapy in adults: a report from the European association of cardiovascular imaging and the American society of echocardiography. Eur Heart J Cardiovasc Imaging. 2013;14:721–40.
Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the task force for the diagnosis and management of pericardial diseases of the European Society of Cardiology (ESC) Eur Heart J. 2015 Nov 7;36(42):2921–64.
George TJ, Arnaoutakis GJ, Beaty CA, et al. Contemporary etioloigies, risk factors, and outcomes after pericardiectomy. Ann Thorac Surg. 2012;94:445–51.
Wethal T, Lund MB, Edvardsen T, et al. Valvular dysfunction and left ventricular changes in Hodgkin’s lymphoma survivors. A Longitudinal Study. Br J Cancer. 2009;101:575–81.
Tsai HR, Gjesdal O, Wethal T, et al. Left ventricular function assessed by two-dimensional speckle tracking echocardiography in long-term survivors of Hodgkin’s lymphoma treated by mediastinal radiotherapy with or without anthracycline therapy. Am J Cardiol. 2011;107:472–7.
Saxena P, Joyce LD, Daly RC, et al. Cardiac transplantation for radiation-induced cardiomyopathy: the Mayo Clinic experience. Ann Thorac Surg. 2014;98(6):2115–21.
Hull MC, Morris CG, Pepine cJ et al. Valviular dysfunction and carotid, subclavian and coronary disease in survivors of Hodgkin lymphoma treated with radiation therapy. JAMA. 2003;290:2831–7.
Donnellan E, Griffin BP, Johnston DR, et al. Rate of progression of aortic stenosis and its impact on outcomes in patients with radiation-associated cardiac disease: a matched cohort study. J Am Coll Cardiol Img. 2018;11:1072–80.
Dolmaci OB, Farag ES, Boekholdt SM, et al. Outcomes of cardiac surgery after mediastinal radiation therapy: a single-center experience. J Card Surg. 2020 Mar;35(3):612–9.
Heidenreich PA, Schnittger I, Strauss HW, et al. Screening for coronary artery disease after mediastinal irradiation for Hodgkin lymphoma. J Clin Oncol. 2007;25:43–9.
Nilsson G, Holmberd L, Gamo H, et al. Distribution of coronary artery stenosis after radiation for breast cancer. J Clin Oncol. 2012;30:380–6.
Iliescu CA, Grines CL, Hermann J, et al. SCAI Expert consensus statement: evaluation, management and special considerations of cardiooncology patients in the cardiac catheterization laboratory (endorsed by the Cardiological Society of India, and Sociedad Latino Americana de Cardiologia Intervencionista). Catheter Cardiovasc Interv. 2016. https://doi.org/10.1002/ccd.26379.
Baumgartner H Chair, Hung J Co-Chair, Bermejo J, Chambers JB, Edvardsen T, Goldstein S, Lancellotti P, LeFevre M, Miller F Jr, Otto CM. Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European association of cardiovascular imaging and the American society of echocardiography. Eur Heart J Cardiovasc Imaging. 2017 Mar 1;18(3):254–75. doi: https://doi.org/10.1093/ehjci/jew335.
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Muñoz D, Rosenhek R, Sjögren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL. ESC scientific document group. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017 Sep 21;38(36):2739–91. doi: https://doi.org/10.1093/eurheartj/ehx391.
Donnellan E, Griffin BP, Johnston DR, et al. Rate of progression of aortic stenosis and its impact on outcomes in patients with radiation-associated cardiac disease: a matched cohort study. J Am Coll Cardiol Img. 2018;11:1072–80.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
23.1 Electronic supplementary material
Below is the link to the electronic supplementary material.
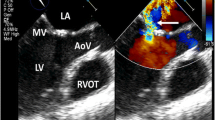
Video 23.1
Echocardiography in 2016 before TAVR. A, Parasternal long axis view showing calcification and thickening of aortic valve cusps (arrow) with severe limitation of their opening. Aortic valve annulus is also calcified. We can see also that LV contractility is low. LV—left ventricle. TAVR—transcatheter aortic valve replacement. B, Short axis view of aortic valve showing markedly limited excursion and calcification of the cusps (PPTX 1953 kb)
Video 23.2
Echocardiography in 2016 before TAVR. A, Moderate aortic regurgitation. B, LV hypokinesis. LVEF estimated at <20%. LV—left ventricle. LVEF—left ventricular ejection fraction TAVR—transcatheter aortic valve replacement (PPTX 1545 kb)
Video 23.3
Coronary angiography. Intact LAD and LCx with late collateral contrast filling of obstructed RCA. LAD—left anterior descending artery. LCx—left circumflex artery. RCA—right coronary artery (PPTX 6842 kb)
Video 23.4
Coronary angiography of left coronary artery at first presentation in 2009. A and B, Two views before stenting showing significant LCx stenosis. C and D, After stent placement in LCx showing good coronary flow. LCx—left circumflex artery (PPTX 4597 kb)
Video 23.5
Left panel: Angiography of the left subclavian artery performed after the onset of arm claudication in 2010 showing severe arterial stenosis. There are no visible branches of the artery due to the markedly reduced blood flow. Right panel: Angiography of the left subclavian artery after stenting. There is normal contrast filling of the subclavian artery and its branches (PPTX 1300 kb)
Video 23.6
Coronary angiography performed in May 2019 when the patient was admitted with worsening heart failure and some chest discomfort not typical for angina (unlike the first presentation in 2009). It shows stenoses at the proximal and the distal ends of the stent in LCx. LAD appears normal. LAD—left anterior descending artery. LCx—left circumflex artery (PPTX 2276 kb)
Video 23.7
Coronary angiography performed in May 2020 at admission with diagnosis of non-ST-elevation myocardial infarction presenting with worsening of heart failure. Shows 2 views of left coronary artery branches revealing subtotal LCx stent stenosis. LAD ostial stenosis was also recognized but it cannot be seen well on these videos. LAD—left anterior descending artery. LCx—left circumflex artery (PPTX 4246 kb)
Video 23.8
Echocardiography after recent coronary intervention in August 2020. A and B, Parasternal long axis view and four-chamber view showing mitral valve with thickening of anterior cusp, shortening of posterior cusp, and calcifications in subvalvular apparatus. Limited opening of mitral valve can be seen also, but mitral stenosis was not confirmed. C, Color Doppler showing high-speed eccentric regurgitant jet at mitral valve. The grade of mitral regurgitation is III (PPTX 1953 kb)
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Poltavskaya, M. (2021). Cardio-Oncologists Perspective on the Cardiac Implications of Radiotherapy: Complex Cases of Radiation-Related Valvular and Vascular Disease. In: Steingart, R.M., Liu, J.E. (eds) Atlas of Imaging in Cardio-Oncology. Springer, Cham. https://doi.org/10.1007/978-3-030-70998-3_23
Download citation
DOI: https://doi.org/10.1007/978-3-030-70998-3_23
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-70997-6
Online ISBN: 978-3-030-70998-3
eBook Packages: MedicineMedicine (R0)