Abstract
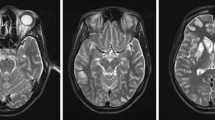
Neurological symptoms described in COVID-19 infected patients can also occur in a more inflammatory related setting as in case of posterior reversible encephalopathy syndrome (PRES) that can be associated with SARS-CoV2 infection due to the massive cytokine storm, damage to endothelium and vasogenic oedema. At brain imaging, quite symmetric bilateral focal or confluent vasogenic oedema with posterior parietal and occipital lobe involvement are found. In severe cases like in COVID-setting, PRES can be complicated by ischemia or haemorrhage: we then describe in the atlas two cases of classic and complicated COVID-related PRES.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Hinchey J, Chaves C, Appignani B, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334(8):494–500. https://doi.org/10.1056/NEJM199602223340803.
Bartynski WS. Posterior reversible encephalopathy syndrome, part 1 and 2: fundamental imaging and clinical features. AJNR Am J Neuroradiol. 2008;29:1036–42. https://doi.org/10.3174/ajnr.A0928.
Bakshi R, Bates VE, Mechtler LL, et al. Occipital lobe seizures as the major clinical manifestation of reversible posterior leukoencephalopathy syndrome: magnetic resonance imaging findings. Epilepsia. 1998;39(3):295–9. https://doi.org/10.1111/j.1528-1157.1998.tb01376.x.
Fugate JE, Claassen DO, Cloft HJ, et al. Posterior reversible encephalopathy syndrome: associated clinical and radiologic findings. Mayo Clin Proc. 2010;85(5):427–32. https://doi.org/10.4065/mcp.2009.0590.
Miller TR, Shivashankar R, Mossa-Basha M, et al. Reversible cerebral vasoconstriction syndrome, part 1: epidemiology, pathogenesis, and clinical course. AJNR Am J Neuroradiol. 2015;36:1392–9. https://doi.org/10.3174/ajnr.A4214.
Schwartz RB, Jones KM, Kalina P, et al. Hypertensive encephalopathy: findings on CT, MR imaging, and SPECT imaging in 14 cases. AJR Am J Roentgenol. 1992;159:379–83. https://doi.org/10.2214/ajr.159.2.1632361.
Calabrese LH, Dodick DW, Schwedt TJ, et al. Narrative review: reversible cerebral vasoconstriction syndromes. Ann Intern Med. 2007;146:34–44. https://doi.org/10.7326/0003-4819-146-1-200701020-00007.
Chen SP, Fuh JL, Wang SJ, et al. Magnetic resonance angiography in reversible cerebral vasoconstriction syndromes. Ann Neurol. 2010;67:648–56. https://doi.org/10.1002/ana.21951.
Aird WC. The role of the endothelium in severe sepsis and multiple organ dysfunction syndrome. Blood. 2003;101:3765–77. https://doi.org/10.1182/blood-2002-06-1887.
Bartynski WS, Tan HP, Boardman JF, et al. Posterior reversible encephalopathy syndrome after solid organ transplantation. AJNR Am J Neuroradiol. 2008;29:924–30. https://doi.org/10.3174/ajnr.A0960.
Gupta S, Kaplan MJ. Pathogenesis of systemic lupus erythematosus. Rheumatology. 7th ed. Philadelphia, PA: Elsevier; 2019. p. 1154–9.
Loscalzo J. Endothelial injury, vasoconstriction, and its prevention. Tex Heart Inst J. 1995;22:180–4.
Sandoo A, van Zanten JJ, Metsios GS, et al. The endothelium and its role in regulating vascular tone. Open Cardiovasc Med J. 2010;4:302–12. https://doi.org/10.2174/1874192401004010302.
Franceschi AM, Ahmed O, Giliberto L, et al. Hemorrhagic posterior reversible encephalopathy syndrome as a manifestation of COVID-19 infection. AJNR Am J Neuroradiol. 2020;41(7):1173–6. https://doi.org/10.3174/ajnr.A6595.
Hernández-Fernández F, Valencia HS, Barbella-Aponte RA, et al. Cerebrovascular disease in patients with COVID-19: neuroimaging, histological and clinical description. Brain. 2020;143:3089. https://doi.org/10.1093/brain/awaa239.
Filatov A, Sharma P, Hindi F, et al. Neurological complications of coronavirus (COVID-19): encephalopathy. Cureus. 2020;12:e7352. https://doi.org/10.7759/cureus.7352.
Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–4. https://doi.org/10.1016/S0140-6736(20)30628-0.
Eltzschig HK, Carmeliet P. Hypoxia and inflammation. N Engl J Med. 2011;364:656–65. https://doi.org/10.1056/NEJMra0910283.
Bartels K, Grenz A, Eltzschig HK. Hypoxia and inflammation are two sides of the same coin. Proc Natl Acad Sci U S A. 2013;110:18351–2. https://doi.org/10.1073/pnas.1318345110.
Rosa Junior M, Borges EI, Fonseca APA, et al. Posterior reversible encephalopathy syndrome during treatment with tocilizumab in juvenile idiopathic arthritis. Arq Neuropsiquiatr. 2018;76:720–1. https://doi.org/10.1590/0004-282X20180093.
Cross SN, Ratner E, Rutherford TJ, et al. Bevacizumab-mediated interference with VEGF signalling is sufficient to induce a preeclampsia-like syndrome in nonpregnant women. Rev Obstet Gynecol. 2012;5:2–8.
McKinney AM, Short J, Truwit CL, et al. Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findings. AJR Am J Roentgenol. 2007;189:904–12. https://doi.org/10.2214/AJR.07.2024.
Levitt M, Zampolin R, Burns J, et al. Posterior reversible encephalopathy syndrome and reversible cerebral vasoconstriction syndrome. Distinct Clinical Entities with Overlapping Pathophysiology. Radiol Clin N Am. 2019;57:1133–46. https://doi.org/10.1016/j.rcl.2019.07.001.
Covarrubias DJ, Luetmer PH, Campeau NG. Posterior reversible encephalopathy syndrome: prognostic utility of quantitative diffusion-weighted MR images. AJNR Am J Neuroradiol. 2002;23:1038–4.
Eichler FS, Wang P, Wityk RJ, et al. Diffuse metabolic abnormalities in reversible posterior leukoencephalopathy syndrome. AJNR Am J Neuroradiol. 2002;23(5):833–7.
Hefzy HM, Bartynski WS, Boardman JF, et al. Hemorrhage in posterior reversible encephalopathy syndrome: imaging and clinical features. AJNR Am J Neuroradiol. 2009;30(7):1371–9. https://doi.org/10.3174/ajnr.A1588.
Cruz-Flores S, de Assis Aquino Gondim F, Leira EC. Brainstem involvement in hypertensive encephalopathy: clinical and radiological findings. Neurology. 2004;62(8):1417–9. https://doi.org/10.1212/01.wnl.0000120668.73677.5f.
Pilato F, Distefano M, Calandrelli R. Posterior reversible encephalopathy syndrome and reversible cerebral vasoconstriction syndrome: clinical and radiological considerations. Front Neurol. 2020;11:34. https://doi.org/10.3389/fneur.2020.00034.
Muttikkal TJ, Wintermark M. MRI patterns of global hypoxic-ischemic injury in adults. J Neuroradiol. 2013;40:164–71. https://doi.org/10.1016/j.neurad.2012.08.002.
Wijdicks EF, Campeau NG, Miller GM. MR imaging in comatose survivors of cardiac resuscitation. AJNR Am J Neuroradiol. 2001;22:1561–5.
Ho ML, Rojas R, Eisenberg RL. Cerebral edema. AJR Am J Roentgenol. 2012;199:W258–73. https://doi.org/10.2214/AJR.11.8081.
Coolen T, Lolli V, Sadeghi N, et al. Early postmortem brain MRI findings in COVID-19 non-survivors. Neurology. 2020;95(14):e2016–27. https://doi.org/10.1212/WNL.0000000000010116.
Anand P, Lau HV, Chung DY, et al. Posterior reversible encephalopathy syndrome in patients with coronavirus disease 2019: two cases and a review of the literature. J Stroke Cerebrovasc Dis. 2020;29(11):105212.
Gaensbauer JT, Press CA, Hollister JR, et al. Procalcitonin: a marker of infection not subverted by treatment with interleukin-6 receptor inhibition. Pediatr Infect Dis J. 2013;32(9):1040. https://doi.org/10.1097/INF.0b013e318295a3d0.
Kotani K, Miyamoto M, Ando H. The effect of treatments for rheumatoid arthritis on endothelial dysfunction evaluated by flow-mediated vasodilation in patients with rheumatoid arthritis. Curr Vasc Pharmacol. 2016;15(1):10–8. https://doi.org/10.2174/1570161114666161013113457.
Vallejo S, Palacios E, Romacho T, et al. The interleukin-1 receptor antagonist anakinra improves endothelial dysfunction in streptozotocin-induced diabetic rats. Cardiovasc Diabetol. 2014;13:158. https://doi.org/10.1186/s12933-014-0158-z.
Ikonomidis I, Lekakis JP, Nikolaou M, et al. Inhibition of interleukin-1 by anakinra improves vascular and left ventricular function in patients with rheumatoid arthritis. Circulation. 2008;117(20):2662–9. https://doi.org/10.1161/CIRCULATIONAHA.107.731877.
Doo FX, Kassim G, Lefton DR, et al. Rare presentations of COVID-19: PRES-like leukoencephalopathy and carotid thrombosis. Clin Imaging. 2020;69:94–101. https://doi.org/10.1016/j.clinimag.2020.07.007.
Rogg J, Baker A, Tung G. Posterior reversible encephalopathy syndrome (PRES): another imaging manifestation of COVID-19. Interdiscip Neurosurg. 2020;22:100808. https://doi.org/10.1016/j.inat.2020.100808.
Jayaraman K, Rangasami R, Chandrasekharan A. Magnetic resonance imaging findings in viral encephalitis: a pictorial essay. J Neurosci Rural Pract. 2018;9(4):556–60. https://doi.org/10.4103/jnrp.jnrp_120_18.
Egdell R, Egdell D, Solomon T. Herpes simplex virus encephalitis. BMJ. 2012;344:e3630. https://doi.org/10.1136/bmj.e3630.
Steiner I, Budka H, Chaudhuri A, et al. Viral meningoencephalitis: a review of diagnostic methods and guidelines for management. Eur J Neurol. 2010;17(8):999–e57. https://doi.org/10.1111/j.1468-1331.2010.02970.x.
Gupta RK, Soni N, Kumar S, et al. Imaging of central nervous system viral diseases. J Magn Reson Imaging. 2012;35(3):477–91. https://doi.org/10.1002/jmri.22830.
Finkenstaedt M, Szudra A, Zerr I, et al. MR imaging of Creutzfeldt-Jakob disease. Radiology. 1996;199(3):793–8. https://doi.org/10.1148/radiology.199.3.8638007.
Becker JT, Maruca V, Kingsley LA, et al. Multicenter AIDS Cohort Study. Factors affecting brain structure in men with HIV disease in the post-HAART era. Neuroradiology. 2011;54(2):113–21. https://doi.org/10.1007/s00234-011-0854-.
Shah R, Bag AK, Chapman PR, et al. Imaging manifestations of progressive multifocal leukoencephalopathy. Clin Radiol. 2010;65(6):431–9. https://doi.org/10.1016/j.crad.2010.03.001.
Misra UK, Kalita J, Phadke RV, et al. Usefulness of various MRI sequences in the diagnosis of viral encephalitis. Acta Trop. 2010;116(3):206–11. https://doi.org/10.1016/j.actatropica.2010.08.007.
Molimard J, Baudou E, Mengelle C, et al. Coxsackie B3-induced rhombencephalitis. Arch Pediatr. 2019;26(4):247–8. https://doi.org/10.1016/j.arcped.2019.02.013.
Asadi-Pooya AA, Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci. 2020;413:116832. https://doi.org/10.1016/j.jns.2020.116832.
Hernandez-Fernandez F, Valencia HS, Barbella-Aponte RA, et al. Cerebrovascular disease in patients with COVID-19: neuroimaging, histological and clinical description. Brain. 2020;143:3089. https://doi.org/10.1093/brain/awaa239.
Mahammedi A, Saba L, Vagal A, et al. Imaging in neurological disease of hospitalized COVID-19 patients: an Italian multicenter retrospective observational study. Radiology. 2020;297:E270. https://doi.org/10.1148/radiol.2020201933.
Merkler AE, Parikh NS, Mir S, et al. Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID-19) vs patients with influenza. JAMA Neurol. 2020;77:1. https://doi.org/10.1001/jamaneurol.2020.2730.
Garg RK, Paliwal VK, Gupta A. Encephalopathy in patients with COVID-19: a review. J Med Virol. 2020:1–17. https://doi.org/10.1002/jmv.26207.
Baig AM, Khaleeq A, Ali U, et al. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11(7):995–8. https://doi.org/10.1021/acschemneuro.0c00174.
Moriguchi T, Harii N, Goto J, et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020;94:55–8. https://doi.org/10.1016/j.ijid.2020.03.062.
Russell B, Moss C, Rigg A, et al. Anosmia and ageusia are emerging as symptoms in patients with COVID-19: what does the current evidence say? Ecancermedicalscience. 2020;14:ed98. https://doi.org/10.3332/ecancer.2020.ed98.
Hamming I, Timens W, Bulthuis M, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–7. https://doi.org/10.1002/path.1570.
Tai W, He L, Zhang X, et al. Characterization of the receptor-binding domain (RBD) of 2019 novel coronavirus: implication for development of RBD protein as a viral attachment inhibitor and vaccine. Cell Mol Immunol. 2020;17:613–20. https://doi.org/10.1038/s41423-020-0400-4.
Lau SK, Woo PC, Yip CC, et al. Coronavirus HKU1 and other coronavirus infections in Hong Kong. J Clin Microbiol. 2006;44(6):2063–71. https://doi.org/10.1128/JCM.02614-05.
MacNamara KC, Chua MM, Phillips JJ, et al. Contributions of the viral genetic background and a single amino acid substitution in an immunodominant CD8+ T-cell epitope to murine coronavirus neurovirulence. J Virol. 2005;79(14):9108–18. https://doi.org/10.1128/JVI.79.14.9108-9118.2005.
Mehta P, McAuley DF, Brown M, et al. HLH Across Speciality Collaboration, UK. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–4. https://doi.org/10.1016/S0140-6736(20)30628-0.
Al-Olama M, Rashid A, Garozzo D. COVID-19-associated meningoencephalitis complicated with intracranial hemorrhage: a case report. Acta Neurochir. 2020;162(7):1495–9. https://doi.org/10.1007/s00701-020-04402-w.
Dogan L, Kaya D, Sarikaya T, et al. Plasmapheresis treatment in COVID-19-related autoimmune meningoencephalitis: case series. Brain Behav Immun. 2020;87:155–8. https://doi.org/10.1016/j.bbi.2020.05.022.
Piechotta V, Chai KL, Valk SJ, et al. Convalescent plasma or hyperimmune immunoglobulin for people with COVID-19: a living systematic review. Cochrane Database Syst Rev. 2020;7(7):CD013600. https://doi.org/10.1002/14651858.CD013600.pub2.
Zambreanu L, Lightbody S, Bhandari M, et al. A case of limbic encephalitis associated with asymptomatic COVID-19 infection. J Neurol Neurosurg Psychiatry. 2020;91:1229. https://doi.org/10.1136/jnnp-2020-323839.
Varatharaj A, Thomas N, Ellul MA, et al. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. 2020;7(10):875–82. https://doi.org/10.1016/S2215-0366(20)30287-X.
Xiong W, Mu J, Guo J, et al. New onset neurologic events in people with COVID-19 in 3 regions in China. Neurology. 2020;95(11):e1479–87. https://doi.org/10.1212/WNL.0000000000010034.
Pons-Escoda A, Naval-Baudín P, Majós C, et al. Neurologic Involvement in COVID-19: cause or coincidence? A neuroimaging perspective. AJNR Am J Neuroradiol. 2020;41(8):1365–9. https://doi.org/10.3174/ajnr.A6627.
Chougar L, Shor N, Weiss N, et al. CoCo Neurosciences study group. Retrospective observational study of brain magnetic resonance imaging findings in patients with acute SARS-CoV-2 infection and neurological manifestations. Radiology. 2020;297:E313. https://doi.org/10.1148/radiol.2020202422.
Montalvan V, Lee J, Bueso T, et al. Neurological manifestations of COVID-19 and other coronavirus infections: a systematic review. Clin Neurol Neurosurg. 2020;194:105921. https://doi.org/10.1016/j.clineuro.2020.105921.
Guilmot A, Maldonado Slootjes S, et al. Immune-mediated neurological syndromes in SARS-CoV-2-infected patients. J Neurol. 2020:1–7. https://doi.org/10.1007/s00415-020-10108-x.
Toscano G, Palmerini F, Ravaglia S, et al. Guillain-Barré syndrome associated with SARS-CoV-2. N Engl J Med. 2020;382(26):2574–6. https://doi.org/10.1056/NEJMc2009191.
Gutiérrez-Ortiz C, Méndez-Guerrero A, Rodrigo-Rey S, et al. Miller Fisher syndrome and polyneuritis cranialis in COVID-19. Neurology. 2020;95(5):e601–5. https://doi.org/10.1212/WNL.0000000000009619.
Pilotto A, Odolini S, Masciocchi S, et al. Steroid-responsive encephalitis in coronavirus disease 2019. Ann Neurol. 2020;88:423. https://doi.org/10.1002/ana.25783.
Scullen T, Keen J, Mathkour M, et al. Coronavirus 2019 (COVID-19)-associated encephalopathies and cerebrovascular disease: the New Orleans experience. World Neurosurg. 2020;141:e437–46. https://doi.org/10.1016/j.wneu.2020.05.192.
Zuhorn F, Omaimen H, Ruprecht B, et al. Parainfectious encephalitis in COVID-19: “The Claustrum Sign”. J Neurol. 2020:1–4. https://doi.org/10.1007/s00415-020-10185-y.
Yoshikawa K, Kuwahara M, Morikawa M, et al. Varied antibody reactivities and clinical relevance in anti-GQ1b antibody-related diseases. Neurol Neuroimmunol Neuroinflamm. 2018;5(6):e501. https://doi.org/10.1212/NXI.0000000000000501.
Chi MS, Ng SH, Chan LY. Asymmetric acute motor axonal neuropathy with unilateral tongue swelling mimicking stroke. Neurologist. 2016;21(6):106–8. https://doi.org/10.1097/NRL.0000000000000102.
Hayashi M, Sahashi Y, Baba Y, et al. COVID-19-associated mild encephalitis/encephalopathy with a reversible splenial lesion. J Neurol Sci. 2020;415:116941. https://doi.org/10.1016/j.jns.2020.116941.
Wong PF, Craik S, Newman P, et al. Lessons of the month 1: a case of rhombencephalitis as a rare complication of acute COVID-19 infection. Clin Med (Lond). 2020;20(3):293–4. https://doi.org/10.7861/clinmed.2020-0182.
Paterson RW, Brown RL, Benjamin L, et al. UCL Queen Square National Hospital for Neurology and Neurosurgery COVID-19 Study Group. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain. 2020;143:3104. https://doi.org/10.1093/brain/awaa240.
Virhammar J, Kumlien E, Fällmar D, et al. Acute necrotizing encephalopathy with SARS-CoV-2 RNA confirmed in cerebrospinal fluid. Neurology. 2020;95(10):445–9. https://doi.org/10.1212/WNL.0000000000010250.
Acknowledgements
Cases 1 and 2 of Sect. 4.1 and Case 2 of Sect. 4.2 courtesy of:
-
E. D’Adda, MD; M.E. Fruguglietti, MD; Neurologist Stroke Unit Cerebrovascular Dept; ASST Crema Hospital
-
M. Borghetti MD, G. Benelli MD; Radiology Unit, Cerebrovascular Dept; ASST Crema Hospital
-
G. Merli MD, G. Lupi MD, Department of Anesthesia and Critical Care Medicine, ASST Crema Hospital
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Manara, O., Pezzetti, G., Gerevini, S. (2021). Posterior Reversible Encephalopathy Syndrome (PRES) and Meningo-Encephalitis in COVID. In: Gerevini M.D., S. (eds) Neuroimaging of Covid-19. First Insights based on Clinical Cases. Springer, Cham. https://doi.org/10.1007/978-3-030-67521-9_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-67521-9_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-67520-2
Online ISBN: 978-3-030-67521-9
eBook Packages: MedicineMedicine (R0)