Abstract
Nasopharyngeal cancer (NPC) is an uncommon cancer. According to the Global Cancer Observatory, of the 129,000 new diagnoses in 2018, 85% has been made in the Asiatic population. In males the annual age adjusted rate of incidence (per 100,000) dramatically varied between 8 in South-Eastern Asia and <1 in Europe. In Europe (period of diagnosis 1999–2007), the annual incidence rate varied between 0.7 (South of Europe) and 0.2 (North of Europe). Incidence is three time higher in men than women. Elderly are more affected than young people. Five-year survival, from European population based cancer registries was 49% (period 1999–2007), survival was better in younger than in older patients (73% vs. 31%), prognosis was more favorable in women than men (54% vs. 47%). Geographical variation of survival was reported, with poor 5-year in the Eastern European countries (36%).
Incidence and population based survival are crucial for public health and planning clinical study. Lifestyle and environmental factors are responsible of the decreasing trend of incidence in quite all the world countries.
Being one of the rare diseases, NPC need to be centralized for diagnosis and treatment. In Europe, the European Joint Action of Rare Cancers and the European Reference Network for rare disease will play an important role to make progress and reduce geographical disparities.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
Introduction
Nasopharyngeal cancer (NPC) is a rare cancer in the majority of countries, however NPC is endemic in certain regions of southern China, Southeast Asia and Africa. This paper provides descriptive epidemiology of the epithelial malignant nasopharyngeal tumours, showing incidence and survival variation by sex, age, geographic region/population and time trend. The source of data are the major website as given by the International Agency for Research on Cancer (IARC) Global Cancer Observatory [1], and the RARECAREnet European project [2], for Europe.
The differences in incidence and survival will be interpreted according to the literature.
Incidence
In 2018, 129,000 new cases of NPC were diagnosed worldwide with 85% of cases in the Asiatic population. Figure 21.1 shows the estimated number of new cases and the age-standardized incidence rates for the 10 countries in which NPC is diagnosed most common. Actually, in males the annual crude rate of incidence (per 100,000) dramatically varied between 8 in South-Eastern Asia and <1 in the European regions (Table 21.1).
Nasopharyngeal cancer in the ten countries with the highest incidence in 2018. From Global Cancer Observatory [1]
In Europe (EU28) from European population-based cancer registries, 2600 new diagnoses per year (incidence) were made (1999–2007) and 18,200 people were living, in 2008, with a diagnosis of NPC (prevalence) [2]. Tables 21.2 and 21.3 show incidence (numbers and rates) by sex, age, time period and European region. Incidence is higher in men than women with a ratio 3:1 (Table 21.2). The disease is more frequent in the elderly (65 and more years of age): the incidence rate (per 100,000/year) increases with age at diagnosis from <0.1 to 0.9 (Table 21.2).
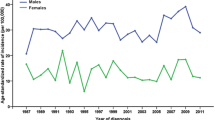
In Europe there is an incidence gradient across countries, with the highest rates in the Southern which are 2/3 times higher than in the Northern countries. The occurrence of NPC remains constant during the period 1995–2007.
Survival
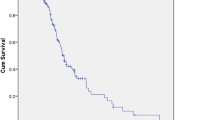
Based on about 7300 cases, survival of European patients with NPC were 76%, 57%, and 49% at 1, 3 and 5 years after diagnosis, respectively (Table 21.4). Prognosis (5-year survival) was better in younger patients, aged 15–24 years, at 73%, and dramatically reduced in the elderly, 65 years and more, at 31%. Females had a significantly better prognosis, 5-year survival, 54% versus 47% (Table 21.4).
Five-year survival was between 51% and 55% in all the European regions, except the Eastern of European countries with 36% (Table 21.5).
During the study period (1995–2007), 5-year survival slightly, but not significantly, improved.
Survival in population based studies was analyzed in terms of relative survival, which is an analogous of cause specific survival usually considered in clinical studies. Relative survival is the ratio between the observed survival of the cohort of patients belonging to a specific population (for example Belgium or Estonia) and the survival of the general population of the same country and with the same age distribution.
Discussion
Incidence of cancers, given by population-based cancer registries, provides the annual number of new cases of a specific cancer in a defined population/region. NPC is a rare cancer, in Europe not more than 3% of all H&N cancers [2]. Incidence together with prevalence are important for public health planning, to organize centralization of the cure and planning of clinical trials. In Europe, the number of annual cases across country ranged between 2 or less (Malta and Iceland) and 454 (Germany) [2]. The geographical variation of the incidence rates gives insight into possible factors or causes of the disease, again relevant to public health to reduce the new number of cases. The incidence variability around the world of NPC is very high and this variation has been explained by diet. According to the World Cancer Research Fund (WCRF) updated review [3], the largest review on diet, nutrition and physical activity, the major risk factors explaining the difference in incidence in populations are the consuming Cantonese style salted fish, meat and preserved non-starchy vegetable; other established causes include smoking, occupational exposure and infectious agents. There is a strong evidence of risk for NPC consuming Cantonese style salted fish and some evidence consuming red meat and processed meat; while the consumption of a greater intake of non-starchy vegetables decreases the risk of NPC. Cantonese-style salted fish contains nitrosamines and nitrosamine precursors which have been shown to induce the development of cancer. Smoking is attributable to 23% of NPC cases [3] and dust and formaldehyde are the major occupational factors associated to NPC [4]. Epstein-Barr virus (EBV) infection is an important player in this disease, but it needs other factors in addition, as only a fraction of the infected population develops NPC [3].
A recent paper, conducted in the Taiwanese population (≈160,000 participants and 115 NPC cases), showed the effect of air pollution as a risk of developing NPC [5]. The study reported a clear dose response relationship: NPC increased with the increase in nitrogen dioxide (NO2) from 1.4 to 2.3 compared to lowest concentration levels. The same was with the fine particulate (PM2.5) with a double risk.
There is a global reducing incidence of NPC as reported by the review by Tang et al. for the period 1970–2007 [6]. The occurrence of NPC significantly decreased in southern and eastern Asia, north America and Nordic countries with average annual percent changes (AAPCs) of −1% to −5%. Decreasing trends in NPC incidence are due to tobacco control, changes in diets and economic development. The ecological study by Lau et al. [7] investigated in some European and Asiatic countries and in the US the relationship between the NPC incidence with the consumption of salted fish, vegetables and tobacco cigarettes, from the Food and Agriculture Organization (FAO) and Census Statistics. They found markedly decreasing trends of NPC in Hong Kong which was correlated with corresponding secular changes in salted fish consumption per capita, tobacco and vegetable consumption per capita. In many countries the tobacco smoking, which is more connected to the keratinizing squamous cell carcinoma and prevalent in the non epidemic area, is reducing [6].
In Europe, NPC 5-year survival was poorer in males, in the elderly and in the Eastern countries. No progress has been observed in the first years of this century. Interestingly, from the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) database (1973–2013) [8], Asians showed a disease specific survival advantage over Caucasians, African Americans and Hispanics, when adjusted for sex, age at diagnosis, grade, TNM staging and treatment strategy. Asians showed a less aggressive disease characterized by non keratinizing lesions, smaller size at diagnosis, well differentiated grading and an earlier TNM stage. However, taking into account these prognostic factors in a multivariate analysis, the advantage persisted suggesting that genetic predispositions, viral agents, occupational exposures, and dietary exposures to chemical carcinogens can be responsible of the aggressiveness of the diseases. However, the African Americans had a higher rate of metastasis at the time of diagnosis and the highest proportion of no treatment with the common therapy of NPC (surgery or radiation). These results may be connected to the fact that certain minorities in the US have less access to or make use of medical care in terms of clinic visits, preventative care and diagnostic testing.
NPC is a rare cancer, therefore the correct and fast diagnosis and treatment can be obtained in high volume hospitals with a good expertise. Diagnosis and treatment in reference centres are expected to be more accurate because they benefit from large numbers of cases, which are often discussed in a multidisciplinary setting involving expert professionals. Within the RARECAREnet project [9] centralization of rare cancer patients was studied in 7 European countries, and for the head and neck group of rare cancers 75% of patients were centralised in two top hospitals in Slovenia (2 million population, 266 treatments per hospital per year), and 12 top hospitals in the Netherlands (17 million population, 201 treatments per hospital per year). The level of centralisation was lower in the other countries such as Finland, Ireland, Bulgaria, Navarra and Belgium. However, the period of study was 1999–2007 and the situation will for sure improve in some countries over time. The European Joint Action on Rare Cancers [10] and the institution of the European Reference Network for rare diseases [11] will continue to play a role in this.
References
WCRF/American Institute for Cancer Research. Diet, Nutrition and Physical Activity and Cancer: a global perspective. Continuous Update Project Expert Report. 2018. Available on https://www.wcrf.org/dietandcancer/nasopharyngeal-cancer
Charbotel B, Fervers B, Droz JP. Occupational exposures in RCs: a critical review of the literature. Crit Rev Oncol Hematol. 2014;90(2):99–134.
Fan H-C, Chen C-Y, Hsu Y-C, Chou R-H, Teng C-LJ, Chiu C-H, et al. Increased risk of incident nasopharyngeal carcinoma with exposure to air pollution. PLoS One. 2018;13(9):e0204568. https://doi.org/10.1371/journal.pone.0204568.
Tang L-L, Chen W-Q, Xue W-Q, He Y-Q, Zheng R-S, Zeng Y-X, Jia W-H. Global trends in incidence and mortality of nasopharyngeal carcinoma. Cancer Lett. 2016;374:22–30.
Lau, et al. Secular trends of salted fish consumption and nasopharyngeal carcinoma: a multi-jurisdiction ecological study in 8 regions from 3 continents. BMC Cancer. 2013;13:298.
Zhou L, Shen N, Li G, Ding J, Liu D, Huang X. The racial disparity of nasopharyngeal carcinoma based on the database analysis. Am J Otolaryngol. 2019;40(6):102288.
Gatta G, Capocaccia R, Botta L, et al. Burden and centralised treatment in Europe of rare tumours: results of RARECAREnet-a population-based study. Lancet Oncol. 2017;18(8):1022e39.
European Parliament and the Council of the European Union. Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients’ rights in cross-border healthcare. Official Journal of the European Union n° L 88/45 of 4.4.2011.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2021 The Author(s)
About this paper
Cite this paper
Gatta, G. (2021). Epidemiological Aspects in Nasopharyngeal Cancer. In: Vermorken, J.B., Budach, V., Leemans, C.R., Machiels, JP., Nicolai, P., O’Sullivan, B. (eds) Critical Issues in Head and Neck Oncology. Springer, Cham. https://doi.org/10.1007/978-3-030-63234-2_21
Download citation
DOI: https://doi.org/10.1007/978-3-030-63234-2_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-63233-5
Online ISBN: 978-3-030-63234-2
eBook Packages: MedicineMedicine (R0)