Abstract
In the western world, the risk of cardiovascular diseases (CVDs) in pregnancy has increased due to increasing age at first pregnancy frequently associated with an increasing prevalence of cardiovascular risk factors, especially diabetes, hypertension, and obesity. Additionally, an increasing number of women with congenital heart disease reach childbearing age. In western countries, maternal heart disease is the major cause of maternal death during pregnancy, and peripartum intensive care unit admissions are increasing in frequency. Knowledge of the risks associated with CVDs during pregnancy and their management in pregnant women is of pivotal importance for advising patients before pregnancy. Several risk scores have been developed to risk-stratify women with heart disease desiring pregnancy. The risk estimation needs to be re-evaluated during each prepregnancy visit, because the risk of complications may change over time. The last ESC guidelines for the management of cardiovascular diseases during pregnancy enforce WHO classification of maternal risk and introduce the “pregnancy heart team” a multidisciplinary team that includes cardiologists, anesthesiologists, and obstetricians with expertise in caring for women with heart disease for achieving optimal outcomes.
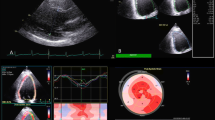
The use of Doppler cardiac output measurement techniques has greatly increased our understanding of the magnitude and timing of cardiac changes during pregnancy. It is important to develop uniformity in echocardiographic methodology, gestational age, ethnicity, prepregnancy body mass index, and equipment and data collection when evaluating serial changes in echo Doppler parameters during each trimester of pregnancy.
Transthoracic echocardiography is the preferred imaging method in pregnancy. Echocardiography provides information about disease etiology, accurate and noninvasive assessment of severity, and means of monitoring progression. Transesophageal echocardiography is relatively safe; however, the risk of vomiting/aspiration and sudden increases in intra-abdominal pressure should be considered, and fetal monitoring performed. Doppler and qualitative color Doppler are useful to clarify the pathophysiology of the hemodynamic consequences of structural valve defects during pregnancy with respect to the transient nature of gradients resulting from variable loading overload of pregnancy.
Congenital heart disease (CHD) is the most common birth defect, and just under 1% of newborns have congenital heart disease. Advances in diagnostic, medical, and surgical management options have improved the long-term survival of patients with CHD. Thus, most women born with CHD will reach reproductive age. While many women with CHD tolerate the hemodynamic changes of pregnancy, others may face significant immediate or late risks of pregnancy including volume overload, arrhythmias, progressive cardiac dysfunction, thrombosis, and death. Fortunately, most of these complications could be managed.
The risks associated with pregnancy in women with congenital heart disease depend on the underlying heart defect as well as on additional factors such as ventricular function, functional class, and cyanosis. The risk of pregnancy includes adverse maternal and fetal outcomes.
The issues surrounding this growing selected population of women will increase in importance in the future as more women with greater age than in the past and with other comorbidities will became pregnant. An echocardiogram taken before the pregnancy is useful in establishing the baseline status and may be repeated safely throughout pregnancy.
Patients with complex cardiac diseases should be informed about maternal and fetal risks related to pregnancy and managed and delivered at a regional or tertiary center where a multidisciplinary team with knowledge and experience in cardiac diseases is available.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
The International Society of Gender Medicine (IGM), the German Institute of Gender in Medicine (DGesGM), the European Society of Anaesthesiology (ESA), the European Society of Gynecology (ESG) Authors/Task Force Members: Vera Regitz-Zagrosek (Chairperson) (Germany), JolienW. Roos-Hesselink (Co-Chairperson) (The Netherlands), Johann Bauersachs (Germany), Carina Blomström-Lundqvist (Sweden), Renata Cífková (Czech Republic), Michele De Bonis (Italy), Bernard Iung (France), Mark Richard Johnson (UK), Ulrich Kintscher (Germany), Peter Kranke (Germany), Irene Marthe Lang (Austria), Joao Morais (Portugal), Petronella G. Pieper (The Netherlands), Patrizia Presbitero (Italy), Susanna Price (UK), Giuseppe M. C. Rosano (UK/Italy), Ute Seeland (Germany), Tommaso Simoncini (Italy), Lorna Swan (UK), Carole A. Warnes (USA). 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy The Task Force for the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:3165–241.
Elkayam U, Goland S, Pieper PG, Silverside CK. High-risk cardiac disease in pregnancy: part i. J Am Coll Cardiol. 2016;68:396–410.
Cantwell R, Clutton-Brock T, Cooper G, Dawson A, Drife J, Garrod D, Harper A, Hulbert D, Lucas S, McClure J, Millward-Sadler H, Neilson J, Nelson-Piercy C, Norman J, O’Herlihy C, Oates M, Shakespeare J, de Swiet M, Williamson C, Beale V, Knight M, Lennox C, Miller A, Parmar D, Rogers J, Springett A. Saving mothers’ lives: reviewing maternal deaths to make motherhood safer: 2006-2008. The eighth report of the confidential enquiries into maternal deaths in the United Kingdom. BJOG. 2011;118:1–203.
Malvasi A, Giacci F, Gustapane S, Di Tizio L, Boscia F, Trojano G, Tinelli A. Puerperal complications. In: Malvasi A, Di Renzo GC, editors. Management and therapy of late pregnancy complications: third trimester and puerperium. Cham: Springer; 2017. p. 369–85.
Farr A, Lenz-Gebhart A, Einig S, Ortner C, Holzer I, Elhenicky M, Husslein PW, Lehner R. Outcomes and trends of peripartum maternal admission to the intensive care unit. Wien Klin Wochenschr. 2017;129:605–11.
Balint OH, Siu SC, Mason J, et al. Cardiac outcomes after pregnancy in women with congenital heart disease. Heart. 2010;96:1656–61.
Roos-Hesselink JW, Ruys TPE, Stein JI, et al. Outcome of pregnancy in patients with structural or ischaemic heart disease: results of a registry of the European Society of Cardiology. Eur Heart J. 2013;34:657–65.
Egidy Assenza G, Cassater D, Landzberg M, et al. The effects of pregnancy on right ventricular remodeling in women with repaired tetralogy of Fallot. Int J Cardiol. 2013;168:1847–52.
Siu SC, Sermer M, Colman JM, et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation. 2001;104:515–21.
Greutmann M, Von Klemperer K, Brooks R, et al. Pregnancy outcome in women with congenital heart disease and residual haemodynamic lesions of the right ventricular outflow tract. Eur Heart J. 2010;31:1764–70.
Gill HK, Splitt M, Sharland GK, et al. Patterns of recurrence of congenital heart disease: an analysis of 6,640 consecutive pregnancies evaluated by detailed fetal echocardiography. J Am Coll Cardiol. 2003;42:923–9.
Lui GK, Silversides CK, Khairy P, et al. Heart rate response during exercise and pregnancy outcome in women with congenital heart disease. Circulation. 2011;123:242–8.
Van Hagen IM, Roos-Hesselink JW, Ruys TPE, et al. Pregnancy in women with a mechanical heart valve: data of the European Society of Cardiology Registry of Pregnancy and Cardiac Disease (ROPAC). Circulation. 2015;132:132–42.
Drenthen W, Pieper PG, Roos-Hesselink JW, et al. Outcome of pregnancy in women with congenital heart disease: a literature review. J Am Coll Cardiol. 2007;49:2303–11.
Pedersen LM, Pedersen TAL, Ravn HB, et al. Outcomes of pregnancy in women with tetralogy of Fallot. Cardiol Young. 2008;18:423–9.
Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM, Crumb SR, Dearani JA, Fuller S, Gurvitz M, Khairy P, Landzberg MJ, Saidi A, Valente AM, Van Hare GF. 2018 AHA/ACC guideline for the management of adults with congenital heart diseases: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(14):e637–97.
Bamfo FE, Kametas NA, Nicolaides KH, Chambers JB. Reference ranges for tissue Doppler measures of maternal systolic and diastolic left ventricular function. Ultrasound Obstet Gynecol. 2007;29:414–20.
Bamfo FE, Kametas NA, Nicolaides KH, Chambers JB. Maternal left ventricular diastolic and systolic long-axis function during normal pregnancy. Eur J Echocardiogr. 2007;8:360–8.
Siu SC, Colman J. Congenital heart disease. Heart disease and pregnancy. Heart. 2001;85:710–5.
Adeyeye VO, Balogun MO, Adebayo RA, Makinde ON, Akinwusi PO, Ajayi EA, Ogunyemi SA, Akintomide AO, Ajayi EO, Adeyeye AG, Ojo TO, Abiodun OO. Echocardiographic assessment of cardiac changes during normal pregnancy among Nigerians. Clin Med Insights Cardiol. 2016;10:157–62.
Keser N. Echocardiography in pregnant women. Anadolu Kardiyol Derg. 2006;6(2):169–73.
Cornette J, Ruys TP, Rossi A, Rizopoulos D, Takkenberg JJ, Karamermer Y, Opic P, Van den Bosch AE, Geleijnse ML, Duvekot JJ, Steegers EA, Roos-Hesselink JW. Hemodynamic adaptation to pregnancy in women with structural heart disease. Int J Cardiol. 2013;168:825–31.
Cornette J, Ruys TP, Roos-Hesselink JW. Assessment of the right ventricle in pregnant women with and without structural heart disease. Int J Cardiol. 2013;168:3087.
Kametas NA, McAuliffe F, Hancock J, Chambers J, Nicolaides KH. Maternal left ventricular mass and diastolic function during pregnancy. Ultrasound Obstet Gynecol. 2001;18:460–6.
Schannwell CM, Schoebel FC, Zimmermann T, Marx R, Plehn G, Leschke M, et al. Left ventricular diastolic function in normal pregnancy. A prospective study using M-mode echocardiography and Doppler echocardiography. Dtsch Med Wochenschr. 2000;125:1069–73.
Trappe HJ. Cardiac arrhythmias during pregnancy—what to do? Herz. 2003;28:216–26.
Rychik J, Ayres N, Cuneo B, Gotteiner N, Hornberger L, Spevak PJ, et al. American society of echocardiography guidelines and standards for performance of the fetal echocardiogram. J Am Soc Echocardiogr. 2004;17:803–10.
Antonelli D, Bloch L, Rosenfeld T. Implantation of permanent dual chamber pacemaker in a pregnant woman by transesophageal echocardiographic guidance. Pacing Clin Electrophysiol. 1999;22:534.
Ray P, Murphy GJ, Shutt LE. Recognition and management of maternal cardiac disease in pregnancy. Br J Anaesth. 2004;93:428–39.
Funakoshi Y, Kato M, Kuratani T. Successful treatment of massive pulmonary embolism in the 38th week of pregnancy. Ann Thorac Surg. 2004;77:694–5.
Khanom M, Hossain A. Valvular heart disease in pregnancy: a review. J Indian Coll Cardiol. 2015;5(3):177–82.
Barlow J, Bosman C. Aneurysmal protrusion of the posterior leaflet of the mitral valve: an auscultatory-electrocardiographic syndrome. Am Heart J. 1966;71(2):166–78.
Tsiaras S, Poppas A. Mitral valve disease in pregnancy: outcomes and management. Obstet Med. 2009;2(1):6–10.
Safi LM, Tsiaras SV. Update on valvular heart disease in pregnancy. Curr Treat Options Cardiovasc Med. 2017;19(9):70. Review.
Samiei N, Amirsardari M, Rezaei Y, Parsaee M, Kashfi F, Hantoosh Zadeh S, Beikmohamadi S, Fouladi M, Hosseini S, Peighambari MM, Mohebbi A. Echocardiographic evaluation of hemodynamic changes in left-sided heart valves in pregnant women with valvular heart disease. Am J Cardiol. 2016;118:1046–52.
Hameed A, Karaalp IS, Tummala PP, Wani OR, Canetti M, Akhter MW, Goodwin I, Zapadinsky N, Elkayam U. The effect of valvular heart disease on maternal and fetal outcome of pregnancy. J Am Coll Cardiol. 2001;37:893–9.
Drenthen W, Boersma E, Balci A, Moons P, Roos-Hesselink JW, Mulder BJ, Vliegen HW, van Dijk AP, Voors AA, Yap SC, van Veldhuisen DJ, Pieper PG. Predictors of pregnancy complications in women with congenital heart disease. Eur Heart J. 2010;31:2124–32.
van Hagen IM, Thorne SA, Taha N, Youssef G, Elnagar A, Gabriel H, ElRakshy Y, Iung B, Johnson MR, Hall R, Roos-Hesselink JW, ROPAC Investigators, EORP Team. Pregnancy outcomes in women with rheumatic mitral valve disease: results from the registry of pregnancy and cardiac disease. Circulation. 2018;137:806–16.
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Munoz D, Rosenhek R, Sjogren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739–91.
Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP, Iung B, Otto CM, Pellikka PA, Quinones M. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. Eur J Echocardiogr. 2009;10:1–25.
Braverman AC, Thomas JD, Lee RT. Doppler echocardiographic estimation of mitral valve area during changing hemodynamic conditions. Am J Cardiol. 1991;68:1485–90.
Iung B, Cormier B, Elias J, Michel P-L, Nallet O, Porte J-M, et al. Usefulness of percutaneous balloon commissurotomy for mitral stenosis during pregnancy. Am J Cardiol. 1994;73(5):398–400.
Routray S, Mishra T, Swain S, Patnaik U, Behera M. Balloon mitral valvuloplasty during pregnancy. Int J Gynecol Obstet. 2004;85(1):18–23.
de Souza JA, Martinez EE Jr, Ambrose JA, Alves CM, Born D, Buffolo E, Carvalho AC. Percutaneous balloon mitral valvuloplasty in comparison with open mitral valve commissurotomy for mitral stenosis during pregnancy. J Am Coll Cardiol. 2001;37:900–3.
Esteves CA, Munoz JS, Braga S, Andrade J, Meneghelo Z, Gomes N, Maldonado M, Esteves V, Sepetiba R, Sousa JE, Palacios IF. Immediate and long-term follow-up of percutaneous balloon mitral valvuloplasty in pregnant patients with rheumatic mitral stenosis. Am J Cardiol. 2006;98:812–6.
Diao M, Kane A, Ndiaye MB, Mbaye A, Bodian M, Dia MM, Sarr M, Kane A, Monsuez JJ, Ba SA. Pregnancy in women with heart disease in sub-Saharan Africa. Arch Cardiovasc Dis. 2011;104:370–4.
Avila WS, Rossi EG, Ramires JA, Grinberg M, Bortolotto MR, Zugaib M, da Luz PL. Pregnancy in patients with heart disease: experience with 1,000 cases. Clin Cardiol. 2003;26:135–42.
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population based study. Lancet. 2006;368(9540):1005–11.
Orwat S, Diller GP, van Hagen IM, Schmidt R, Tobler D, Greutmann M, Jonkaitiene R, Elnagar A, Johnson MR, Hall R, Roos-Hesselink JW, Baumgartner H. Risk of pregnancy in moderate and severe aortic stenosis: from the multinational ROPAC registry. J Am Coll Cardiol. 2016;68:1727–37.
Baumgartner H, Bonhoeffer P, De Groot N, de Haan F, Deanfield J, Galie N, et al. Association for European Paediatric Cardiology (AEPC); ESC Committee for Practice Guidelines (CPG). ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J. 2010;31(23):2915–57.
Nanna M, Stergiopoulos K. Pregnancy complicated by valvular heart disease: an update. J Am Heart Assoc. 2014;3(3):e000712.
Myerson S, Mitchell A, Ormerod O, Banning A. What is the role of balloon dilatation for severe aortic stenosis during pregnancy? J Heart Valve Dis. 2005;14(2):147–50.
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP III, Guyton RA, O’Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM III, Thomas JD. 2014 AHA/ACC guideline for the management of patients with valvular heart disease. J Am Coll Cardiol. 2014;63:e57–e185.
Yuan S-M, Yan S-L. Mitral valve prolapse in pregnancy. Braz J Cardiovasc Surg. 2016;31(2):158–62.
Gelson E, Johnson M, Gatzoulis M, Abselm U. Cardiac disease in pregnancy. Part 2: acquired heart disease. Obstet Gynaecol. 2007;9(2):83–7.
Roos-Hesselink JW, Ruys TP, Stein JI, Thilen U, Webb GD, Niwa K, Kaemmerer H, Baumgartner H, Budts W, Maggioni AP, Tavazzi L, Taha N, Johnson MR, Hall R. Outcome of pregnancy in patients with structural or ischaemic heart disease: results of a registry of the European Society of Cardiology. Eur Heart J. 2013;34:657–65.
Ballo P, Motto A, De Viti D, Mondillo S. Images in cardiology. M-mode Doppler pattern of severe functional mitral regurgitation in the presence of high left ventricular filling pressures: the sign of the galloping coloured horse. Can J Cardiol. 2009;25(2):79–80.
Hayek E, Gring CN, Griffin BP. Mitral valve prolapse. Lancet. 2005;365(9458):507–18.
Roeder HA, Kuller JA, Barker PC, James AH. Maternal valvular heart disease in pregnancy. Obstet Gynecol Surv. 2011;66(9):561–71.
Lesniak-Sobelga A, Tracz W, KostKiewicz M, Podolec P, Pasowicz M. Clinical and echocardiographic assessment of pregnant women with valvular heart diseases–maternal and fetal outcome. Int J Cardiol. 2004;94:15–23.
Jana N, Vasishta K, Khunnu B, Dhall GI, Grover A. Pregnancy in association with mitral valve prolapse. Asia Oceania J Obstet Gynaecol. 1993;19(1):61–5.
Marijon E, Mirabel M, Celermajer DS, Jouven X. Rheumatic heart disease. Lancet. 2012;379(9819):953–64.
Elkayam U, Bitar F. Valvular heart disease and pregnancy part I: native valves. J Am Coll Cardiol. 2005;46:223–30.
Lind J, Wallenburg HC. The Marfan syndrome and pregnancy: a retrospective study in a Dutch population. Eur J Obstet Gynecol Reprod Biol. 2001;98:28–35.
Windram JD, Colman JM, Wald RM, Udell JA, Siu SC, Silversides CK. Valvular heart disease in pregnancy. Best Pract Res Clin Obstet Gynaecol. 2014;28(4):507–18.
Donnelly JE, Brown JM, Radford DJ. Pregnancy outcome and Ebstein’s anomaly. Br Heart J. 1991;66:368–71.
Khairy P, Ouyang DW, Fernandes SM, Lee-Parritz A, Economy KE, Landzberg MJ. Pregnancy outcomes in women with congenital heart disease. Circulation. 2006;113:517–24.
van der Linde D, Konings EE, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJ, Roos-Hesselink JW. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;58:2241–7.
Marelli AJ, Ionescu-Ittu R, Mackie AS, Guo L, Dendukuri N, Kaouache M. Lifetime prevalence of congenital heart disease in the general population from 2000 to 2010. Circulation. 2014;130:749–56.
Stout K. Pregnancy in women with congenital heart disease: the importance of evaluation and counselling. Heart. 2005;91(6):713–4.
Mandalenakis Z, Rosengren A, Skoglund K, Lappas G, Eriksson P, Dellborg M. Survivorship in children and young adults with congenital heart disease in Sweden. JAMA Intern Med. 2017;177:224–30.
Sliwa K, van Hagen IM, Budts W, Swan L, Sinagra G, Caruana M, Blanco MV, Wagenaar LJ, Johnson MR, Webb G, Hall R, Roos-Hesselink JW. Pulmonary hypertension and pregnancy outcomes: data from the registry of pregnancy and cardiac disease (ROPAC) of the European Society of Cardiology. Eur J Heart Fail. 2016;18:1119–28.
Knight M, Nair M, Tuffnell D, Kenyon S, Shakespeare J, Brocklehurst P, Kurinczuk JJ, editors. On behalf of MBRRACE-UK. Saving lives, improving mothers’ care—surveillance of maternal deaths in the UK 2012–14 and lessons learned to inform maternity care from the UK and Ireland confidential enquiries into maternal deaths and morbidity 2009–14. Oxford: National Perinatal Epidemiology Unit, University of Oxford; 2016.
Shime J, Mocarski EJ, Hastings D, Webb GD, McLaughlin PR. Congenital heart disease in pregnancy: short- and long-term implications. Am J Obstet Gynecol. 1987;156:313–22.
Daliento L, Somerville J, Presbitero P, Menti L, Brach-Prever S, Rizzoli G, Stone S. Eisenmenger syndrome: factors relating to deterioration and death. Eur Heart J. 1998;19:1845–55.
Presbitero P, Somerville J, Stone S, Aruta E, Spiegelhalter D, Rabajoli F. Pregnancy in cyanotic congenital heart disease: outcome of mother and fetus. Circulation. 1994;89:2673–6.
Siu SC, Sermer M, Colman JM, Alvarez AN, Mercier LA, Morton BC, Kells CM, Bergin ML, Kiess MC, Marcotte F, Taylor DA, Gordon EP, Spears JC, Tam JW, Amankwah KS, Smallhorn JF, Farine D, Sorensen S. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation. 2001;104:515–21.
Opotowsky AR, Siddiqi OK, D’Souza B, Webb GD, Fernandes SM, Landzberg MJ. Maternal cardiovascular events during childbirth among women with congenital heart disease. Heart. 2012;98:145–51.
Drenthen W, Pieper PG, Roos-Hesselink JW, van Lottum WA, Voors AA, Mulder BJ, van Dijk AP, Vliegen HW, Yap SC, Moons P, Ebels T, Van Veldhuisen DJ, ZAHARA Investigators. Outcome of pregnancy in women with congenital heart disease: a literature review. J Am Coll Cardiol. 2007;49:2303–11.
Balint OH, Siu SC, Mason J, Grewal J, Wald R, Oechslin EN, Kovacs B, Sermer M, Colman JM, Silversides CK. Cardiac outcomes after pregnancy in women with congenital heart disease. Heart. 2010;96:1656–61.
van der Bom T, Bouma BJ, Meijboom FJ, et al. The prevalence of adult congenital heart disease, results from a systematic review and evidence based calculation. Am Heart J. 2012;164:568–75.
Yap SC, Drenthen W, Meijboom FJ, Moons P, Mulder BJ, Vliegen HW, van Dijk AP, Jaddoe VW, Steegers EA, Roos-Hesselink JW, Pieper PG. Comparison of pregnancy outcomes in women with repaired versus unrepaired atrial septal defect. BJOG. 2009;116:1593–601.
Rosas M, Attie F, Sandoval J, et al. Atrial septal defect in adults > or =40 years old: negative impact of low arterial oxygen saturation. Int J Cardiol. 2004;93:145–55.
Bannan A, Shen R, Silvestry FE, et al. Characteristics of adult patients with atrial septal defects presenting with paradoxical embolism. Catheter Cardiovasc Interv. 2009;74:1066–9.
Toglia MR, Weg JG. Venous thromboembolism during pregnancy. N Engl J Med. 1996;335:108–14.
Rigatelli G, Dell’avvocata F, Tarantini G, et al. Clinical, hemodynamic, and intracardiac echocardiographic characteristics of secundum atrial septal defects-related paradoxical embolism in adulthood. J Interv Cardiol. 2014;27:542–7.
Zuber M, Gautschi N, Oechslin E, et al. Outcome of pregnancy in women with congenital shunt lesions. Heart. 1999;81:271–5.
Engelfriet P, Meijboom F, Boersma E, et al. Repaired and open atrial septal defects type II in adulthood: an epidemiological study of a large European cohort. Int J Cardiol. 2008;126:379–85.
Gabriels C, De Meester P, Pasquet A, et al. A different view on predictors of pulmonary hypertension in secundum atrial septal defect. Int J Cardiol. 2014;176:833–40.
Vogel M, Berger F, Kramer A, et al. Incidence of secondary pulmonary hypertension in adults with atrial septal or sinus venosus defects. Heart. 1999;82:30–3.
Yong G, Khairy P, De Guise P, et al. Pulmonary arterial hypertension in patients with transcatheter closure of secundum atrial septal defects: a longitudinal study. Circ Cardiovasc Interv. 2009;2:455–62.
Engelfriet PM, Duffels MG, Moller T, et al. Pulmonary arterial hypertension in adults born with a heart septal defect: the Euro Heart Survey on adult congenital heart disease. Heart. 2007;93:682–7.
Diller GP, Gatzoulis MA. Pulmonary vascular disease in adults with congenital heart disease. Circulation. 2007;115:1039–50.
Vaideeswar P, Mishra P, Nimbalkar M. Infective endocarditis of the Dacron patch-a report of 13 cases at autopsy. Cardiovasc Pathol. 2011;20:e169–75.
Zahr F, Katz WE, Toyoda Y, et al. Late bacterial endocarditis of an amplatzer atrial septal defect occluder device. Am J Cardiol. 2010;105:279–80.
Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC guidelines for the management of infective endocarditis: the task force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36:3075–128.
Drenthen W, Boersma E, Balci A, et al. Predictors of pregnancy complications in women with congenital heart disease. Eur Heart J. 2010;31:2124–32.
Minette MS, Sahn DJ. Ventricular septal defects. Circulation. 2006;114:2190–7.
Warnes CA, Liberthson R, Danielson GK, Dore A, Harris L, Hoffman JI, et al. Task force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol. 2001;37:1170–5.
Kidd L, Driscoll DJ, Gersony WM, Hayes CJ, Keane JF, O’Fallon WM, et al. Second natural history study of congenital heart defects. Results of treatment of patients with ventricular septal defects. Circulation. 1993;87:I38–51.
Roos-Hesselink JW, Meijboom FJ, Spitaels SE, Van Domburg R, Van Rijen EH, Utens EM, et al. Outcome of patients after surgical closure of ventricular septal defect at young age: longitudinal follow-up of 22–34 years. Eur Heart J. 2004;25:1057–62.
Tatsuno K, Ando M, Takao A, Hatsune K, Konno S. Diagnostic importance of aortography in conal ventricular-septal defect. Am Heart J. 1975;89:171–7.
Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease). Circulation. 2008;118:e714–833.
Zuber M, Gautschi N, Oechslin E, Widmer V, Kiowski W, Jenni R. Outcome of pregnancy in women with congenital shunt lesions. Heart. 1999;81:271–5.
Veldtman GR, Connolly HM, Grogan M, Ammash NM, Warnes CA. Outcomes of pregnancy in women with tetralogy of Fallot. J Am Coll Cardiol. 2004;44(1):174–80.
Anderson RH, Allwork SP, Ho SY, Lenox CC, Zuberbuhler JR. Surgical anatomy of tetralogy of Fallot. J Thorac Cardiovasc Surg. 1981;81:887–96.
Lillehei CW, Varco RL, Cohen M, et al. The first open heart corrections of tetralogy of Fallot: a 26 to 31 year follow-up of 106 patients. Ann Surg. 1986;204:490–502.
Greutmann M, Von Klemperer K, Brooks R, Peebles D, O’Brien P, Walker F. Pregnancy outcome in women with congenital heart disease and residual haemodynamic lesions of the right ventricular outflow tract. Eur Heart J. 2010;31:1764–70.
Balci A, Drenthen W, Mulder BJ, Roos-Hesselink JW, Voors AA, Vliegen HW, Moons P, Sollie KM, van Dijk AP, van Veldhuisen DJ, Pieper PG. Pregnancy in women with corrected tetralogy of fallot: occurrence and predictors of adverse events. Am Heart J. 2011;161:307–13.
Akagi T. Pregnancy related cardiovascular complications in women with post operative tetralogy of Fallot: multiinstitutional survey in Japan. Circulation. 2005;108:682.
Connolly HM, Warnes CA. Ebstein’s anomaly: outcome of pregnancy. J Am Coll Cardiol. 1994;23:1194–8.
Niwa K. Adult congenital heart disease with pregnancy. Korean Circ J. 2018;48(4):251–76.
Beckman RH III. Coarctation of the aorta. In: Allen HD, Gutgesell HP, Clark EB, Driscoll DJ, editors. Moss and Adams’ heart disease in infants, children and adolescents: including the fetus and young adult, vol. 2. 6th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2001. p. 988–1010.
Strafford MA, Griffiths SP, Gersony WM. Coarctation of the aorta: a study in delayed detection. Pediatrics. 1982;69:159–63.
Rosenthal L. Coarctation of the aorta and pregnancy: report of five cases. BMJ. 1955;1:16–8.
Beauchesne LM, Connolly HM, Ammash NM, Warnes CA. Coarctation of the aorta: outcome of pregnancy. J Am Coll Cardiol. 2001;38(6):1728–33.
Niwa K, Perloff JK, Bhuta SM, et al. Structural abnormalities of great arterial walls in congenital heart disease: light and electron microscopic analyses. Circulation. 2001;103:393–400.
Niwa K, Siu SC, Webb GD, Gatzoulis MA. Progressive aortic root dilatation in adults late after repair of tetralogy of fallot. Circulation. 2002;106:1374–8.
Sorrell VL, Panczyk E, Alpert JS. A new disease: bicuspid aortic valve aortopathy syndrome. Am J Med. 2012;125:322–3.
Smith K, Gros B. Pregnancy-related acute aortic dissection in Marfan syndrome: a review of the literature. Congenit Heart Dis. 2017;12:251–60.
Pyeritz RE. Maternal and fetal complications of pregnancy in the Marfan syndrome. Am J Med. 1981;71:784–90.
Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, Eagle KA, Hermann LK, Isselbacher EM, Kazerooni EA, Kouchoukos NT, Lytle BW, Milewicz DM, Reich DL, Sen S, Shinn JA, Svensson LG, Williams DM, American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, Society for Vascular Medicine. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeones, and Society for Vascular Medicine. Circulation. 2010;121:e266–369.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/ AAPA/ABC/ACPM/AGS/APHA/aASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Cinical Practice Guidelines. Hypertension. 2018;71:e13–e115.
Guédès A, Mercier LA, Leduc L, Bérubé L, Marcotte F, Dore A. Impact of pregnancy on the systemic right ventricle after a mustard operation for transposition of the great arteries. J Am Coll Cardiol. 2004;44:433–7.
Canobbio MM, Mair DD, van der Velde M, Koos BJ. Pregnancy outcomes after the Fontan repair. J Am Coll Cardiol. 1996;28:763–7.
Drenthen W, Pieper PG, Roos-Hesselink JW, et al. Pregnancy and delivery in women after Fontan palliation. Heart. 2006;92:1290–4.
Canobbio MM, Warnes CA, Aboulhosn J, Connolly HM, Khanna A, Koos BJ, Mital S, Rose C, Silversides C, Stout K. Management of pregnancy in patients with complex congenital heart disease: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2017;135(8):e50–87.
De Viti D, Santoro F, Raimondo P, Brunetti ND, Memmola C. Congenital Aorto-right ventricular fistula associated with pulmonary hypertension in an old female patient. J Cardiovasc Echogr. 2018;28(2):141–2.
Peacock AJ, Murphy NF, McMurray JJ, Caballero L, Stewart S. An epidemiological study of pulmonary arterial hypertension. Eur Respir J. 2007;30:104–9.
Jais X, Olsson KM, Barbera JA, Blanco I, Torbicki A, Peacock A, Vizza CD, Macdonald P, Humbert M, Hoeper MM. Pregnancy outcomes in pulmonary arterial hypertension in the modern management era. Eur Respir J. 2012;40:881–5.
Sliwa K, Hilfiker-Kleiner D, Petrie MC, Mebazaa A, Pieske B, Buchmann E, Regitz-Zagrosek V, Schaufelberger M, Tavazzi L, van Veldhuisen DJ, Watkins H, Shah AJ, Seferovic PM, Elkayam U, Pankuweit S, Papp Z, Mouquet F, McMurray JJ. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy. Eur J Heart Fail. 2010;12:767–78.
Hilfiker-Kleiner D, Sliwa K. Pathophysiology and epidemiology of peripartum cardiomyopathy. Nat Rev Cardiol. 2014;11:364–70.
McNamara DM, Elkayam U, Alharethi R, Damp J, Hsich E, Ewald G, Modi K, Alexis JD, Ramani GV, Semigran MJ, Haythe J, Markham DW, Marek J, Gorcsan J III, Wu WC, Lin Y, Halder I, Pisarcik J, Cooper LT, Fett JD. Clinical outcomes for peripartum cardiomyopathy in North America: results of the IPAC study (investigations of pregnancy-associated cardiomyopathy). J Am Coll Cardiol. 2015;66:905–14.
Metra M. September 2016 at a glance: pregnancy, hypertrophic cardiomyopathy, epidemiology, medical treatment. Eur J Heart Fail. 2016;18:1091–2.
Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, Dubourg O, Kühl U, Maisch B, McKenna WJ, Monserrat L, Pankuweit S, Rapezzi C, Seferovic P, Tavazzi L, Keren A. Classification of the cardiomyopathies: a position statement from the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2008;29(2):270–6.
Christiaans I, Birnie E, Bonsel GJ, et al. Manifest disease, risk factors for sudden cardiac death, and cardiac events in a large nationwide cohort of predictively tested hypertrophic cardiomyopathy mutation carriers: determining the best cardiological screening strategy. Eur Heart J. 2011;32:1161–70.
Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C, et al. ESC guidelines on the management of cardiovascular diseases during pregnancy of the European Society of Cardiology. Eur Heart J. 2011;32:3147–97.
Sbarouni E, Oakley C. Outcome of pregnancy in women with valve prostheses. Br Heart J. 1994;71(2):196–201.
Sadler L, McCowan L, White H, Stewart A, Bracken M, North R. Pregnancy outcomes and cardiac complications in women with mechanical, bioprosthetic and homograft valves. BJOG. 2000;107(2):245–53.
Warnes CA. Prosthetic heart valves. In: Steer PJ, Gatzoulis MA, Baker P, editors. Heart disease and pregnancy. London: RCOG Press; 2006. p. 157–68.
Vitale N, De Feo M, De Santo LS, Pollice A, Tedesco N, Cotrufo M. Dose dependent fetal complications of warfarin in pregnant women with mechanical heart valves. J Am Coll Cardiol. 1999;33(6):1637–41.
Hall JG. Embryopathy associated with oral anticoagulant therapy. Birth Defects. 1965;12:133–40.
Sahul WL, Emery H, Hall JG. Chondrodysplasia punctata and maternal warfarin use during pregnancy. Am J Dis Child. 1975;129:360–2.
Trojano G, Malvasi A, Casavola VC, Marinelli E, Tinelli A, Resta L, Cicinelli E. Chapter 22 Outpatient hysteroscopy in recurrent pregnancy loss. In: Tinelli A, editor. Hysteroscopy. Cham: Springer; 2018. https://doi.org/10.1007/978-3-319-57559-9.
Parazzini F, Cipriani S, Noli S, Baini I, Mauri PA, Busacca M, Vignali M, Trojano G. Centiles of weight of spontaneous and medically induced preterm births in Lombardy. Ital J Gynaecol Obstet. 2016;28:41–4. https://doi.org/10.14660/2385-0868-53.
Parazzini F, Cipriani S, Bulfoni G, Mauri PA, Carraro G, Mastrolia SA, Busacca M, Trojano G. Centiles of weight at term birth according to maternal nationality in a northern Italian region. Ital J Gynaecol Obstet. 2016;28 https://doi.org/10.14660/2385-0868-44.
Xu Z, Fan J, Luo X, Zhang WB, Ma J, Lin YB, Ma SH, Chen X, Wang ZP, Ou JS, Zhang X. Anticoagulation regimens during pregnancy in patients with mechanical heart valves: a systematic review and meta-analysis. Can J Cardiol. 2016;32:1248.E1–9.
Natrella M, Di Naro E, Loverro M, Benshalom-Tirosh N, Trojano G, Tirosh D, Besser L, Loverro MT, Mastrolia SA. The more you lose the more you miss: accuracy of postpartum blood loss visual estimation. A systematic review of the literature. J Matern Fetal Neonatal Med. 2017;12:1–13. https://doi.org/10.1080/14767058.2016.1274302.
De Viti D, Malvasi A, Busardò F, Beck R, Zaami S, Marinelli E. Cardiovascular outcomes in advanced maternal age delivering women. Clinical review and medico-legal issues. Medicina (Kaunas). 2019;55(10):658.
Trojano G, Vignali M, Busacca M, Cipriani S, Esposito G, Bulfoni C, Parazzini F. The timing of elective caesarean delivery at term in lombardy: a comparison of 2010 and 2014. Ital J Gynaecol Obstet. 2016;28 https://doi.org/10.14660/2385-0868-43.
Trojano G, Damiani GR, Olivieri C, Villa M, Malvasi A, Alfonso R, Loverro M, Cicinelli E. VBAC: antenatal predictors of success. Acta Biomed. 2019;90(3):300–9. https://doi.org/10.23750/Abm.V90i3.7623.
Cacciottola L, Solima E, Trojano G, Montesano M, Busacca M, Vignali M. Management of adnexal masses during the third trimester of pregnancy: a case report in twin-pregnancy and review of the literature. Ital J Gynaecol Obstet. 2016;28 https://doi.org/10.14660/2385-0868-40.
Trojano G, Colafiglio G, Saliani N, Lanzillotti G, Cicinelli E. Successful management of a cervical twin pregnancy: neo-adjuvant systemic methotrexate and prophylactic high cervical cerclage before curettage. a case report. Fertil Steril. 2009;91(3):935.E17–9. https://doi.org/10.1016/J.Fertnstert.2008.11.009.
Mastrolia S, Baumfeld Y, Hershkovitz R, Yohay D, Trojano G, Weintraub AY. Independent association between uterine malformations and cervical insufficiency: a retrospective population-based cohort study. Arch Gynecol Obstet. 2018;297:919. https://doi.org/10.1007/S00404-018-4663-2. [Epub Ahead Of Print].
Bianchi C, Battini L, Aragona M, Lencioni C, Ottanelli S, Romano M, Calabrese M, Cuccuru I, De Bellis A, Ml M, Leopardi A, Sabbatini G, Bottone P, Miccoli R, Trojano G, Salerno MG, Del Prato S, Bertolotto A, On Behalf of Tuscany Working Group On “Diabetes, Pregnancy And Exercise”. Prescribing exercise for prevention and treatment of gestational diabetes: review of suggested recommendations. Gynecol Endocrinol. 2017:1–7. https://doi.org/10.1080/09513590.2016.1266474.
Bianchi C, Aragona M, Bertolotto A, Bottone P, Calabrese M, Cuccuru I, De Bellis A, Leopardi A, Lencioni C, Miccoli R, Mori M, Ottanelli S, Romano M, Sabbatini G, Salerno MG, Trojano G, Del Prato S, Battini L, On Behalf of Tuscany Working Group on “Diabetes, Pregnancy And Exercise”. Improving prescription of physical exercise in prophylaxis/therapy of gestational diabetes: a survey from evidence to current recommendations. Ital J Gynaecol Obstet. 2016;28 https://doi.org/10.14660/2385-0868-49.
Malvasi A, Trojano G, Tinelli A, Marinelli E, Zaami S. Episiotomy: an informed consent proposal. J Matern Fetal Neonatal Med. 2019:1–4. https://doi.org/10.1080/14767058.2019.1622677.
Trojano G, Battini L, Bottone P, Tosi V, Nanini C, Carmignani A, Salerno MG. Duodenal atresia and sudden fetal death. running head: prenatal diagnosis of fetal duodenal atresia and risk of fetal adverse outcome. Ital J Gynaecol Obstet. 2014;26:41–2. https://doi.org/10.14660/2385-0868-011.
Malvasi A, Zaami S, Tinelli A, Trojano G, Vergallo GM, Marinelli E. Kristeller maneuvers or fundal pressure and maternal/neonatal morbidity: obstetric and judicial literature review. J Matern Fetal Neonatal Med. 2018;21:1–10. https://doi.org/10.1080/14767058.2018.1441278. Epub Ahead of Print.
Baldini D, Beck R, Negro F, De Viti D. Assisted reproductive technologies and metabolic syndrome complications: medico-legal reappraisal. Clin Ter. 2019;170(5):e364–7. https://doi.org/10.7417/CT.2019.2161.
Beck R, Brizzi A, Cinnella G, Raimondo P, Kuczkowski KM. Anesthesia and analgesia for women undergoing oocyte retrieval. In: Malvasi A, Baldini D, editors. Pick up and oocyte management. Cham: Springer; 2020. p. 99–119.
Pargianas M, Salta S, Fiorentzis S, Kalampoki LG, Beck R, Vizziello D, Kosmas I. Complications in oocyte retrieval. In: Malvasi A, Baldini D, editors. Pick up and oocyte management. Cham: Springer; 2020. p. 305–37.
D’Ambrosio A, Cotoia A, Beck R, Salatto P, Zibar L, Cinnella G. Impedance cardiography as tool for continuous hemodynamic monitoring during cesarean section: randomized, prospective double blind study. BMC Anesthesiol. 2018;18(1):32. https://doi.org/10.1186/s12871-018-0498-4.
Kuczkowski KM, Beck R. Anesthesia in labor and delivery. In: Di Renzo GC, Berghella V, Malvasi A, editors. Good practice and malpractice in labor and delivery. Milan: EDRA; 2019. p. 379–92.
Kuczkowsky KM, Beck R. Labor analgesia. In: Di Renzo GC, Bergella V, Malvasi A, editors. Good practice and malpractice in labor and delivery. Milan: EDRA; 2019. p. 361–72.
Chifenti B, Locci M, Trojano G, Lenzi P, Maria E, Filice ME, Bottone P, Salerno MG, Battini L. Hla-G intracellular expression in decidua trophoblasts in a normal term placenta: a confocal and transmission electron microscopy study. Ital J Gynaecol Obstet. 2016;28 https://doi.org/10.14660/2385-0868-33.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
De Viti, D., Beck, R., Izzo, P., Malvasi, A., Paparella, D., Speziale, G. (2021). Peripartum Echocardiographic Assessment of Women with Cardiovascular Diseases. In: Malvasi, A. (eds) Intrapartum Ultrasonography for Labor Management. Springer, Cham. https://doi.org/10.1007/978-3-030-57595-3_47
Download citation
DOI: https://doi.org/10.1007/978-3-030-57595-3_47
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-57594-6
Online ISBN: 978-3-030-57595-3
eBook Packages: MedicineMedicine (R0)