Abstract
The levator ani muscle is the main muscle of the pelvic floor and consists of:
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Ashton-Miller JA, DeLancey JO. Functional anatomy of the female pelvic floor. Ann N Y Acad Sci. 2007;1101:266–96.
Kearney R, Sawhney R, DeLancey JO. Levator ani muscle anatomy evaluated by origin-insertion pairs. Obstet Gynecol. 2004;104(1):168–73.
Federative Committee on Anatomical Terminology. Terminologia anatomica: international anatomical terminology. Stuttgart: Thieme; 1998.
Kashihara H, Shek KL, Dietz HP. Can we identify the limits of the puborectalis/pubovisceralis muscle on tomographic translabial ultrasound? Ultrasound Obstet Gynecol. 2012;40(2):219–22.
DeLancey JO. Anatomy and biomechanics of genital prolapse. Clin Obstet Gynecol. 1993;36(4):897–909.
DeLancey JO. The anatomy of the pelvic floor. Curr Opin Obstet Gynecol. 1994;6(4):313–6.
Majida M, Braekken IH, Bo K, Benth JS, Engh ME. Validation of three-dimensional perineal ultrasound and magnetic resonance imaging measurements of the pubovisceral muscle at rest. Ultrasound Obstet Gynecol. 2010;35(6):715–22.
Ashton-Miller JA, Delancey JO. On the biomechanics of vaginal birth and common sequelae. Annu Rev Biomed Eng. 2009;11:163–76.
Ashton-Miller JA, Howard D, DeLancey JO. The functional anatomy of the female pelvic floor and stress continence control system. Scand J Urol Nephrol Suppl. 2001;207:1–7; discussion 106-25
Barber MD, Bremer RE, Thor KB, Dolber PC, Kuehl TJ, Coates KW. Innervation of the female levator ani muscles. Am J Obstet Gynecol. 2002;187(1):64–71.
Roshanravan SM, Wieslander CK, Schaffer JI, Corton MM. Neurovascular anatomy of the sacrospinous ligament region in female cadavers: Implications in sacrospinous ligament fixation. Am J Obstet Gynecol. 2007;197(6):660.e1–6.
Guaderrama NM, Liu J, Nager CW, Pretorius DH, Sheean G, Kassab G, et al. Evidence for the innervation of pelvic floor muscles by the pudendal nerve. Obstet Gynecol. 2005;106(4):774–81.
Hsu Y, Summers A, Hussain HK, Guire KE, Delancey JO. Levator plate angle in women with pelvic organ prolapse compared to women with normal support using dynamic MR imaging. Am J Obstet Gynecol. 2006;194:1427–33.
Parks AG, Porter NH, Melzak J. Experimental study of the reflex mechanism controlling the muscle of the pelvic floor. Dis Colon Rectum. 1962;5:407–14.
Taverner D, Smiddy FG. An electromyographic study of the normal function of the external anal sphincter and pelvic diaphragm. Dis Colon Rectum. 1959;2(2):153–60.
Orno AK, Dietz HP. Levator co-activation is a significant confounder of pelvic organ descent on Valsalva maneuver. Ultrasound Obstet Gynecol. 2007;30(3):346–50.
Herschorn S. Female pelvic floor anatomy: the pelvic floor, supporting structures, and pelvic organs. Rev Urol. 2004;6(Suppl 5):S2–s10.
Yiou R, Costa P, Haab F, Delmas V. Functional anatomy of the pelvic floor. Prog Urol. 2009;19:916–25. French
Dietz HP, Eldridge A, Grace M, Clarke B. Does pregnancy affect pelvic organ mobility? Aust N Z J Obstet Gynaecol. 2004;44(6):517–20.
O’Boyle AL, O’Boyle JD, Ricks RE, Patience TH, Calhoun B, Davis G. The natural history of pelvic organ support in pregnancy. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(1):46–9; discussion 9
O’Boyle AL, O’Boyle JD, Calhoun B, Davis GD. Pelvic organ support in pregnancy and postpartum. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(1):69–72; discussion
Shek KL, Kruger J, Dietz HP. The effect of pregnancy on hiatal dimensions and urethral mobility: an observational study. Int Urogynecol J. 2012;23(11):1561–7.
Lowder JL, Debes KM, Moon DK, Howden N, Abramowitch SD, Moalli PA. Biomechanical adaptations of the rat vagina and supportive tissues in pregnancy to accommodate delivery. Obstet Gynecol. 2007;109(1):136–43.
Daucher JA, Clark KA, Stolz DB, Meyn LA, Moalli PA. Adaptations of the rat vagina in pregnancy to accommodate delivery. Obstet Gynecol. 2007;109(1):128–35.
Feola A, Moalli P, Alperin M, Duerr R, Gandley RE, Abramowitch S. Impact of pregnancy and vaginal delivery on the passive and active mechanics of the rat vagina. Ann Biomed Eng. 2011;39(1):549–58.
Harvey MA, Johnston SL, Davies GA. Mid-trimester serum relaxin concentrations and post-partum pelvic floor dysfunction. Acta Obstet Gynecol Scand. 2008;87(12):1315–21.
Sangsawang B. Risk factors for the development of stress urinary incontinence during pregnancy in primigravidae: a review of the literature. Eur J Obstet Gynecol Reprod Biol. 2014;178:27–34.
Sangsawang B, Sangsawang N. Stress urinary incontinence in pregnant women: a review of prevalence, pathophysiology, and treatment. Int Urogynecol J. 2013;24(6):901–12.
Shek KL, Dietz HP. The effect of childbirth on hiatal dimensions. Obstet Gynecol. 2009;113(6):1272–8.
Wijma J, Weis Potters AE, de Wolf BT, Tinga DJ, Aarnoudse JG. Anatomical and functional changes in the lower urinary tract during pregnancy. BJOG. 2001;108(7):726–32.
Villet R, Buzelin JM, Lazorthes F. Female pelvi-perineal disorders. Paris: Vigot; 1995. French
Parente MP, Natal Jorge RM, Mascarenhas T, Fernandes AA, Silva-Filho AL. Computational modeling approach to study the effects of fetal head flexion during vaginal delivery. Am J Obstet Gynecol. 2010;203(3):217 e1–6.
Li X, Kruger JA, Nash MP, Nielsen PM. Anisotropic effects of the levator ani muscle during childbirth. Biomech Model Mechanobiol. 2011;10(4):485–94.
Martins JA, Pato MP, Pires EB, Jorge RM, Parente M, Mascarenhas T. Finite element studies of the deformation of the pelvic floor. Ann N Y Acad Sci. 2007;1101:316–34.
Jing D, Ashton-Miller JA, DeLancey JO. A subject-specific anisotropic viscohyperelastic finite element model of female pelvic floor stress and strain during the second stage of labor. J Biomech. 2012;45(3):455–60.
Hoyte L, Damaser MS, Warfield SK, Chukkapalli G, Majumdar A, Choi DJ, et al. Quantity and distribution of levator ani stretch during simulated vaginal childbirth. Am J Obstet Gynecol. 2008;199(2):198 e1–5.
Ashton-Miller JA, DeLancey JO. Functional anatomy of the female pelvic floor. Ann N Y Acad Sci. 2007;1101:266–96.
Lien KC, Mooney B, DeLancey JO, Ashton-Miller JA. Levator ani muscle stretch induced by simulated vaginal birth. Obstet Gynecol. 2004;103(1):31–40.
Trevathan W. Primate pelvic anatomy and implications for birth. Philos Trans R Soc Lond Ser B Biol Sci. 2015;370(1663):20140065.
Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY, editors. Williams obstetrics. 23rd ed. New York: McGraw-Hill Medical; 2010.
Svabik K, Shek KL, Dietz HP. How much does the levator hiatus have to stretch during childbirth? BJOG. 2009;116(12):1657–62.
DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101(1):46–53.
Dietz HP, Lanzarone V. Levator trauma after vaginal delivery. Obstet Gynecol. 2005;106(4):707–12.
Tunn R, Paris S, Fischer W, Hamm B, Kuchinke J. Static magnetic resonance imaging of the pelvic floor muscle morphology in women with stress urinary incontinence and pelvic prolapse. Neurourol Urodyn. 1998;17:579–89.
Damaser MS, Whitbeck C, Chichester P, Levin RM. Effect of vaginal distension on blood flow and hypoxia of urogenital organs of the female rat. J Appl Physiol (1985). 2005;98(5):1884–90.
Damaser MS, Broxton-King C, Ferguson C, Kim FJ, Kerns JM. Functional and neuroanatomical effects of vaginal distention and pudendal nerve crush in the female rat. J Urol. 2003;170(3):1027–31.
Chaliha C. Postpartum pelvic floor trauma. Curr Opin Obstet Gynecol. 2009;21(6):474–9.
Shek KL, Dietz HP. Intrapartum risk factors for levator trauma. BJOG. 2010;117(12):1485–92.
Dietz HP. Pelvic floor trauma in childbirth. Aust N Z J Obstet Gynaecol. 2013;53(3):220–30.
Valsky DV, Lipschuetz M, Bord A, Eldar I, Messing B, Hochner-Celnikier D, et al. Fetal head circumference and length of second stage of labor are risk factors for levator ani muscle injury, diagnosed by 3-dimensional transperineal ultrasound in primiparous women. Am J Obstet Gynecol. 2009;201(1):91 e1–7.
Dietz HP, Shek KL. Tomographic ultrasound imaging of the pelvic floor: which levels matter most? Ultrasound Obstet Gynecol. 2009;33(6):698–703.
Kearney R, Miller JM, Ashton-Miller JA, DeLancey JO. Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol. 2006;107(1):144–9.
Dietz HP, Simpson JM. Does delayed child-bearing increase the risk of levator injury in labour? Aust N Z J Obstet Gynaecol. 2007;47(6):491–5.
South MM, Stinnett SS, Sanders DB, Weidner AC. Levator ani denervation and reinnervation 6 months after childbirth. Am J Obstet Gynecol. 2009;200(5):519.e1–7.
Handa VL, Danielsen BH, Gilbert WM. Obstetric anal sphincter lacerations. Obstet Gynecol. 2001;98(2):225–30.
Snooks SJ, Swash M, Henry MM, Setchell M. Risk factors in childbirth causing damage to the pelvic floor innervation. Int J Color Dis. 1986;1(1):20–4.
Snooks SJ, Setchell M, Swash M, Henry MM. Injury to innervation of pelvic floor sphincter musculature in childbirth. Lancet. 1984;2(8402):546–50.
Donnelly V, Fynes M, Campbell D, Johnson H, O’Connell PR, O’Herlihy C. Obstetric events leading to anal sphincter damage. Obstet Gynecol. 1998;92(6):955–61.
García-Mejido JA, Gutierrez L, Fernández-Palacin A, Aquise A, Sainz JA. Levator ani muscle injures associated with vaginal vacuum assisted delivery determined by 3/4D transperineal ultrasound. J Matern Fetal Neonatal Med. 2016;21:1–6.
Kruger JA, Heap SW, Murphy BA, Dietz HP. Pelvic floor function in nulliparous women using three-dimensional ultrasound and magnetic resonance imaging. Obstet Gynecol. 2008;111(3):631–8.
Dietz HP, Shek KL, Clarke B. Biometry of the puborectalis muscle and levator hiatus by 3D pelvic floor ultrasound. Ultrasound Obstet Gynecol. 2005;25:580–5.
Dietz HP, Wilson PD. Childbirth and pelvic floor trauma. Best Pract Res Clin Obstet Gynaecol. 2005;19:913–24.
De Leon J, Steensma A, Shek KL, Dietz HP. Ballooning: how to define abnormal distensibility of the levator hiatus. Ultrasound Obstet Gynecol. 2007;30:367–455.
Dietz HP. Ultrasound imaging of the pelvic floor. Part II: three-dimensional or volume imaging. Ultrasound Obstet Gynecol. 2004;23(6):615–25.
Santoro GA, Wieczorek AP, Dietz HP, Mellgren A, Sultan AH, Shobeiri SA, et al. State of the art: an integrated approach to pelvic floor ultrasonography. Ultrasound Obstet Gynecol. 2011;37(4):381–96.
Dietz HP. Pelvic floor ultrasound: a review. Am J Obstet Gynecol. 2010;202(4):321–34.
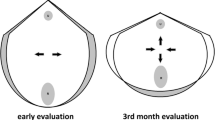
Kamel R, Montaguti E, Nicolaides KH, et al. Contraction of the levator ani muscle during Valsalva maneuver (coactivation) is associated with a longer active second stage of labor in nulliparous women undergoing induction of labor. Am J Obstet Gynecol. 2019;220:189.e1–8.
Dietz HP. Pelvic floor ultrasound in prolapse: what’s in it for the surgeon? Int Urogynecol J. 2011;22(10):1221–32.
Dietz HP, Hoyte L, Steensma AB. Atlas of pelvic floor ultrasound. Dordrecht: Springer; 2008.
Dietz HP, Bernardo MJ, Kirby A, Shek KL. Minimal criteria for the diagnosis of avulsion of the puborectalis muscle by tomographic ultrasound. Int Urogynecol J. 2011;22(6):699–704.
Blasi I, Fuchs I, D’Amico R, Vinci V, La Sala GB, Mazza V, et al. Intrapartum translabial three- dimensional ultrasound visualization of levator trauma. Ultrasound Obstet Gynecol. 2011;37:88–92.
Fuchs I, Tutschek B, Henrich W. Visualization of the fetal fontanels and skull sutures by three-dimensional translabial ultrasound during the second stage of labor. Ultrasound Obstet Gynecol. 2008;31:484–6.
García Mejido JA, Suárez Serrano CM, Fernéndez Palacín A, Aquise Pino A, Bonomi Barby MJ, Sainz Bueno JA. Evaluation of levator ani muscle throughout the different stages of labor by transperineal 3D ultrasound. Neurourol Urodyn. 2017;36:1776–81.
Cleary-Goldman J, Robinson JN. The role of episiotomy in current obstetric practice. Semin Perinatol. 2003;27(1):3–12.
Lede RL, Belizan JM, Carroli G. Is routine use of episiotomy justified? Am J Obstet Gynecol. 1996;174(5):1399–402.
Donald I. Practical obstetric problems. London: Lloyd-Luke; 1979.
Flood C. The real reason for performing episiotomies. World Med. 1982;17:51.
Greenshields W, Ulme HH. The perineum in childbirth: a survey of women’s experiences and midwifery practices. London: National Childbirth Trust; 1993.
Kitzinger S, Walters R. Some women’s experience of episiotomy. London: National Childbirth Trust; 1981.
Carroli G, Belizan J. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2000;1:CD000081.
Espuna-Pons M, Solans-Domenech M, Sanchez E, On Behalf of the Pelvic Floor Research Group (GRESP). Double incontinence in a cohort of nulliparous pregnant women. Neurourol Urodyn. 2012;31:1236–41.
Dietz HP, Shek KL, Chantarasorn V, et al. Do women notice the effect of childbirth-related pelvic floor trauma? Aust N Z J Obstet Gynaecol. 2012;52:277–81.
Handa VL, Blomquist JL, McDermott KC, et al. Pelvic floor disorders after vaginal birth: effect of episiotomy, perineal laceration, and operative birth. Obstet Gynecol. 2012;119:233–9.
Bø K, Hilde G, Tennfjord MK, Engh ME. Does episiotomy influence vaginal resting pressure, pelvic floor muscle strength and endurance, and prevalence of urinary incontinence 6 weeks postpartum? Neurourol Urodyn. 2017;36:716–21.
Cam C, Asoglu MR, Selcuk S, et al. Does mediolateral episiotomy decrease central defects of the anterior vaginal wall? Arch Gynecol Obstet. 2012;285:411–5.
Cassado J, et al. Does episiotomy protect against injury of the levator ani muscle in normal vaginal delivery? Neurourol Urodyn. 2014;33:1212–6.
Fitzgerald MP, Weber AM, Howden N, Cundiff GW, Brown MB. Risk factors for anal sphincter tear during vaginal delivery. Obstet Gynecol. 2007;109(1):29–34.
Dandolu V, Chatwani A, Harmanli O, Floro C, Gaughan JP, Hernandez E. Risk factors for obstetrical anal sphincter lacerations. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(4):304–7.
Coats PM, Chan KK, Wilkins M, Beard RJ. A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol. 1980;87(5):408–12.
Shiono P, Klebanoff MA, Carey JC. Midline episiotomies: more harm than good? Obstet Gynecol. 1990;75(5):765–70.
Revicky V, Nirmal D, Mukhopadhyay S, Morris EP, Nieto JJ. Could a mediolateral episiotomy prevent obstetric anal sphincter injury? Eur J Obstet Gynecol Reprod Biol. 2010;150(2):142–6.
Andrews V, Sultan AH, Thakar R, Jones PW. Risk factors for obstetric anal sphincter injury: a prospective study. Birth. 2006;33(2):117–22.
Sheiner E, Levy A, Walfisch A, Hallak M, Mazor M. Third degree perineal tears in a university medical center where midline episiotomies are not performed. Arch Gynecol Obstet. 2005;271(4):307–10.
de Leeuw JW, de Wit C, Kuijken JP, Bruinse HW. Mediolateral episiotomy reduces the risk for anal sphincter injury during operative vaginal delivery. BJOG. 2008;115(1):104–8.
Kalis V, Landsmanova J, Bednarova B, Karbanova J, Laine K, Rokyta Z. Evaluation of the incision angle of mediolateral episiotomy at 60 degrees. Int J Gynaecol Obstet. 2011;112(3):220–4.
Eogan M, Daly L, O’Connell PR, O’Herlihy C. Does the angle of episiotomy affect the incidence of anal sphincter injury? BJOG. 2006;113(2):190–4.
Aytan H, Tapisiz OL, Tuncay G, Avsar FA. Severe perineal lacerations in nulliparous women and episiotomy type. Eur J Obstet Gynecol Reprod Biol. 2005;121(1):46–50.
Aytan H, Tok EC, Ertunc D, Yasa O. The effect of episiotomy on pelvic organ prolapse assessed by pelvic organ prolapse quantification system. Eur J Obstet Gynecol Reprod Biol. 2014;173:34–7.
Beatty TE. Contributions to medicine and midwifery. Dublin: Fannin and Co; 1866. p. 567.
Black JW. Selected obstetrical & gynaecological works of Sir James Y. Simpson, Bart. Edinburgh: Adam and Charles Black; 1871. p. 65.
Fleming N. Comparison of women with different perineal conditions after childbirth. Ann Arbor: UMI; 1987.
Fleming N. Can the suturing method make a difference in postpartum perineal pain? J Nurse-Midwifery. 1990;35(1):19–25.
Floud E. Protecting the perineum in childbirth 1: a retrospective view. Br J Midwifery. 1994;2(6):258–63.
Verheijen EC, Raven JH, Hofmeyr GJ. Fundal pressure during the second stage of labor. Cochrane Database Syst Rev. 2009;4:CD006067. https://doi.org/10.1002/14651858.CD006067.pub2.
Kline-Kaye V, Miller-Slade D. The use of fundal pressure during the second stage of labor. J Obstet Gynecol Neonatal Nurs. 1990;19(6):511–7. https://doi.org/10.1111/j.1552-6909.1990.tb01670.x.
Merhi ZO, Awonuga AO. The role of uterine fundal pressure in the management of the second stage of labor: a reappraisal. Obstet Gynecol Surv. 2005;60:599–603. https://doi.org/10.1097/01.ogx.0000175804.68946.ac.
Matsuo K, Shiki Y, Yamasaki M, Shimoya K. Use of uterine fundal pressure maneuver at vaginal delivery and risk of severe perineal laceration. Arch Gynecol Obstet. 2009;280:781.
Api O, Balcin ME, Ugurel V, Api M, Turan C, Unal O. The effect of uterine fundal pressure on the duration of the second stage of labor: a randomized controlled trial. Acta Obstet Gynecol Scand. 2009;88(3):320–4. https://doi.org/10.1080/00016340902730326.
Sartore A, et al. The effects of uterine fundal pressure (Kristeller maneuver) on pelvic floor function after vaginal delivery. Arch Gynecol Obstet. 2012;286(5):1135–9.
Cosner KR. Use of fundal pressure during second stage of labor. A pilot study. J Nurse Midwifery. 1996;41(4):334–7.
Zetterstrom J, Lopez A, Anzen B, Norman M, Holmstrom B, Mellgren A. Anal sphincter tears at vaginal delivery: risk factors and clinical outcome of primary repair. Obstet Gynecol. 1999;94(1):21–8.
de Tayrac R, et al. Anatomy and physiology of the pelvic floor. In: Ismail K, editor. Perineal trauma at childbirth. Cham: Springer; 2016.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kamel, R. (2021). Intrapartum Ultrasound and Levator Ani Modifications in Normal and Dystocic Labor. In: Malvasi, A. (eds) Intrapartum Ultrasonography for Labor Management. Springer, Cham. https://doi.org/10.1007/978-3-030-57595-3_35
Download citation
DOI: https://doi.org/10.1007/978-3-030-57595-3_35
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-57594-6
Online ISBN: 978-3-030-57595-3
eBook Packages: MedicineMedicine (R0)